2016 Vol.28(3)
Display Mode: |
2016, 28(3): 263-274.
doi: 10.21147/j.issn.1000-9604.2016.03.01
Abstract:
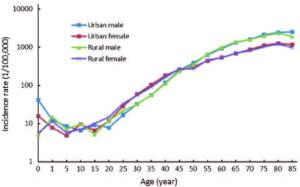
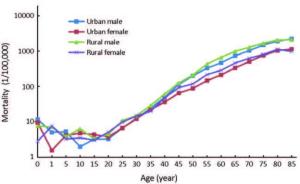
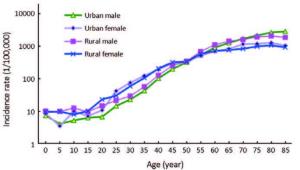
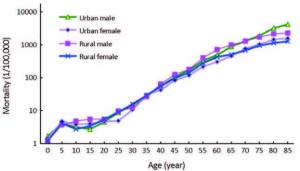
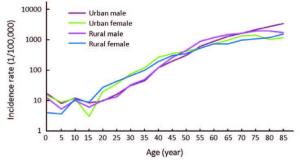
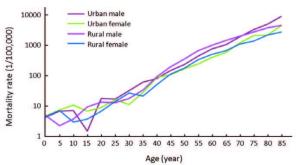
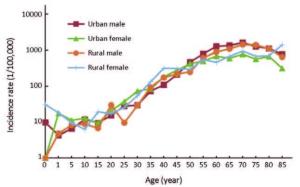
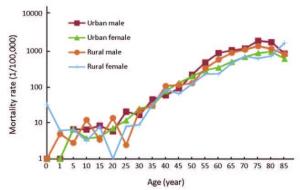
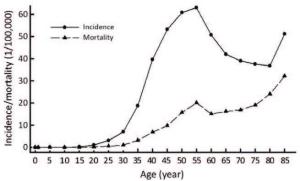
Objective Population-based cancer registration data in 2012 from all available cancer registries in Shandong province were collected by Shandong Center for Disease Control and Prevention (SDCDC). SDCDC estimated the numbers of new cancer cases and cancer deaths in Shandong province with compiled cancer incidence and mortality rates. MethodsIn 2015, there were 21 cancer registries submitted data of cancer incidence and deaths occurred in 2012. All the data were checked and evaluated based on the National Central Cancer Registry (NCCR) criteria of data quality. Qualified data from 15 registries were used for cancer statistics analysis as provincial estimation. The pooled data were stratified by area (urban/rural), gender, age group (0, 1.4, 5.9, 10.14, …, 85+ years) and cancer type. New cancer cases and deaths were estimated using age-specific rates and corresponding provincial population in 2012. The Chinese census data in 2000 and Segi’s population were applied for age-standardized rates. All the rates were expressed per 100,000 person-year. Results Qualified 15 cancer registries (4 urban and 11 rural registries) covered 17,189,988 populations (7,486,039 in urban and 9,703,949 in rural areas). The percentage of cases morphologically verified (MV%) and death certificate-only cases (DCO%) were 66.12% and 2.93%, respectively, and the mortality to incidence rate ratio (M/I) was 0.60. A total of 253,060 new cancer cases and 157,750 cancer deaths were estimated in Shandong province in 2012. The incidence rate was 263.86/100,000 (303.29/100,000 in males, 223.23/100,000 in females), the age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 192.42/100,000 and 189.50/100,000 with the cumulative incidence rate (0.74 years old) of 22.07%. The cancer incidence, ASIRC and ASIRW in urban areas were 267.64/100,000, 195.27/100,000 and 192.02/100,000 compared to 262.32/100,000, 191.26/100,000 and 188.48/100,000 in rural areas, respectively. The cancer mortality was 164.47/100,000 (207.42/100,000 in males, 120.23/100,000 in females), the age-standardized incidence rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 117.54/100,000 and 116.90/100,000, and the cumulative mortality rate (0.74 years old) was 13.53%. The cancer mortality, ASMRC and ASMRW were 141.59/100,000, 101.17/100,000 and 100.33/100,000 in urban areas, and 173.79/100,000, 124.20/100,000 and 123.64/100,000 in rural areas, respectively. Cancers of the lung, stomach, liver, esophagus, colorectum, female breast, brain, leukemia, bladder and pancreas were the most common cancers, accounting for about 82.12% of all cancer new cases. Lung cancer, stomach cancer, liver cancer, esophageal cancer, colorectal cancer, female breast cancer, pancreatic cancer, brain tumor, leukemia and lymphoma were the leading causes of cancer death, accounting for about 89.01% of all cancer deaths. The cancer spectrum showed difference between urban and rural, males and females both in incidence and mortality rates. Conclusions Cancer surveillance information in Shandong province is making great progress with the increasing number of cancer registries, population coverage and the improving data quality. Cancer registration plays a fundamental role in cancer control by providing basic information on population-based cancer incidence, mortality, survival and time trend. The disease burden of cancer is serious in Shandong province, and so cancer prevention and control in Shandong province should be enhanced including health education, health promotion, cancer screening and cancer care services.
2016, 28(3): 275-285.
doi: 10.21147/j.issn.1000-9604.2016.03.02
Abstract:
Objective Population-based cancer registration data in 2012 from all available cancer registries in Henan province were collected by Henan Office for Cancer Research and Control. The numbers of new cancer cases and cancer deaths in Henan province with compiled cancer incidence and mortality rates were estimated. Methods In 2015, all registries’ data in Henan province were qualified for the national cancer registry annual report in 2012. The pooled data were stratified by area (urban/rural), gender, age group (0, 1.4, 5.9, 10.14, …, 85+) and cancer type. New cancer cases and deaths were estimated using age-specific rates and corresponding population of Henan province in 2012. The Chinese census data in 2000 and Segi’s population were applied for age-standardized rates. All the rates were expressed per 100,000 person-years. Results Qualified 19 cancer registries (4 urban and 15 rural registries) covered 16,082,688 populations of Henan province in 2012. The percentage of cases with morphologically verified (MV%) and death certificateonly cases (DCO%) were 69.84% and 2.30%, respectively, and the mortality to incidence rate ratio (M/I) was 0.64. It was estimated that there were 248,510 new cancer cases and 158,630 cancer deaths in Henan province in 2012. The incidence rate was 266.17/100,000 (288.61/100,000 in males and 241.86/100,000 in females), the age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 208.95/100,000 and 206.41/100,000 with the cumulative incidence rate (0.74 years old) of 24.30%. The crude incidence rate in urban areas was higher than that in rural areas. However, after adjusted by age, the cancer incidence rate in rural was higher than that in urban areas. The crude mortality of all cancers in Henan province was 169.90/100,000 (201.23/100,000 in males and 135.95/100,000 in females). The age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 131.20/100,000 and 130.80/100,000, respectively. Among the patients aged 0.74 years, the cumulative mortality rate was 15.03%. The crude cancer mortality rate in urban areas was higher than that of rural areas. However, the age-standardized rate in rural areas was higher than that of urban areas. Cancers of lung, stomach, esophagus, liver, female breast, colorectum, cervix, brain, uterus and ovary were the most common cancers, accounting for about 82.80% of all cancer new cases. Lung cancer, stomach cancer, esophageal cancer, liver cancer, colorectal cancer, female breast cancer, brain cancer, leukemia, pancreatic cancer and cervix cancer were the leading causes of cancer deaths, accounting for about 88.50% of all cancer deaths. The burden between urban and rural, males and females were different. Conclusions Registration data of Henan province was qualified to provide basic information on population-based cancer incidence, mortality for cancer prevention and control. The upper digestive tract cancer burden in Henan province, especially for males in rural areas, was higher. The incidence rate of female breast cancer was higher in urban areas. Targeted prevention, early detection and treatment programs should be carried out by health department to control the cancer burden.
2016, 28(3): 286-300.
doi: 10.21147/j.issn.1000-9604.2016.03.03
Abstract:
Objective This study estimates the numbers of new cancer cases and cancer deaths in Hebei province using incidence and mortality data from 9 population-based cancer registries in 2012. MethodsThe data of new diagnosed cancer cases and cancer deaths in 2012 were collected from 9 population-based cancer registries of Hebei province in 2015. All the data met the National Central Cancer Registry of China (NCCR) criteria of data quality. The pooled data analysis was stratified by areas (urban/rural), gender, age group (0, 1.4, 5.9, 10.14, …, 85+) and cancer type. New cancer cases and deaths in Hebei province were estimated using age-specific rates and corresponding provincial population in 2012. The 10 most common cancers in different groups and the cumulative rates were calculated. Chinese population census in 2000 and Segi’s population were used for age-standardized incidence/mortality rates. Results All cancer registries covered 4,986,847 populations, 6.84% of Hebei provincial population (2,098,547 in urban and 2,888,300 in rural areas). The percentage of cases morphologically verified (MV%) and death certificate-only cases (DCO%) were 76.40% and 4.72%, respectively. The mortality to incidence rate ratio (M/I) was 0.64. In 2012, it is estimated that there were about 187,900 new diagnosed cancer cases and 119,800 cancer deaths in Hebei province. The incidence rate of cancer was 258.12/100,000 (275.75/100,000 in males, 239.78/100,000 in females), and the age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 210.65/100,000 and 208.50/100,000, with the cumulative incidence rates (0.74 years old) of 24.46%. The cancer incidence and ASIRC were 256.99/100,000 and 211.32/100,000 in urban areas and 258.94/100,000 and 209.99/100,000 in rural areas, respectively. The cancer mortality rate was 164.63/100,000 (201.85/100,000 in males, 125.92/100,000 in females). Agestandardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 137.30/100,000 and 137.39/100,000 with the cumulative mortality rate (0.74 years old) of 14.58%, respectively. The cancer mortality rate in rural areas (167.16/100,000) was higher than that in urban areas (161.16/100,000). The most common cancers were lung cancer, stomach cancer, breast cancer, esophageal cancer, liver cancer and colorectal cancer, which accounted for 72.31% of all cancer cases. Lung cancer, stomach cancer, liver cancer, esophageal cancer and colorectal cancer were the major causes of cancer death in Hebei province, which accounted for 75.24% of all cancer deaths. The cancer spectrum differs between urban and rural, males and females in both incidence and mortality rates. ConclusionsThe most common cancers were lung cancer, stomach cancer, esophageal cancer, breast cancer, liver cancer and colorectal cancer in Hebei province.
2016, 28(3): 301-310.
doi: 10.21147/j.issn.1000-9604.2016.03.04
Abstract:
ObjectivePopulation-based cancer registration data in 2012 from all available cancer registries in Gansu province were collected by the Central Cancer Registry of Gansu. The numbers of new cancer cases and cancer deaths in Gansu province with compiled cancer incidence and mortality rates were estimated. Methods In 2015, data from 7 registries in Gansu province were qualified. The pooled data were stratified by area (urban/rural), gender, age group (0, 1.4, 5.9, 10.14, …, 85+) and cancer type. New cancer cases and deaths were estimated using age-specific rates and corresponding population of Gansu province in 2012. The Chinese census data in 2000 and Segi’s population were applied for age-standardized rates. All the rates were expressed per 100,000 person-years. Results Qualified 7 cancer registries (3 urban and 4 rural registries) covered 2,956,560 populations of Gansu province in 2012. The percentage of cases morphologically verified (MV%) and death certificate-only cases (DCO%) were 72.41% and 1.65%, respectively, and the mortality to incidence rate ratio (M/I) was 0.63. It was estimated that there were 575,600 new cancer cases and 331,300 cancer deaths in Gansu province in 2012. The incidence rate was 223.29/100,000 (244.14/100,000 in males and 201.50/100,000 in females), the age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 208.95/100,000 and 206.41/100,000 with the cumulative incidence rate (0.74 years old) of 22.49%. The crude incidence rate in urban areas was equal to that in rural areas. However, after adjusted by age, the cancer incidence rate in urban was the same as that of rural areas. The crude mortality in Gansu province was 128.54/100,000 (135.04/100,000 in males and 124.43/100,000 in females), the age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 109.54/100,000 and 108.44/100,000, respectively, and the cumulative mortality rate (0.74 years old) was 12.91%. The crude cancer mortality rate in urban areas was higher than that of rural areas. However, the agestandardized rate in urban areas was the same as that of rural areas. Cancers of stomach, liver, lung, esophagus, female breast, colorectum, cervix, brain, pancreas and ovary were the most common cancers, accounting for about 83.56% of all cancer new cases. Stomach cancer, liver cancer, lung cancer, esophageal cancer, female breast cancer, colorectal cancer, brain cancer, lymphoma, pancreatic cancer and cervix cancer were the leading causes of cancer death, accounting for about 85.58% of all cancer deaths. The burden between urban and rural, males and females was different. Conclusions Registration data of Gansu province were qualified to provide basic information on population-based cancer incidence, mortality for cancer prevention and control. The digestive tract cancer burden in Gansu province, especially for males in rural areas, was higher. The incidence rate of female breast cancer was higher in urban areas. Targeted prevention, early detection and treatment programs should be carried out by health department to control the cancer burden.
2016, 28(3): 311-320.
doi: 10.21147/j.issn.1000-9604.2016.03.05
Abstract:
Objective To estimate the cancer incidence and mortality in 2012 in Guangdong province by analyzing the cancer data of selected population-based cancer registries in Guangdong province in 2012. Methods Eight of nine population-based cancer registries submitted cancer data to the Guangdong Provincial Centre for Disease Control and Prevention (Guangdong CDC), whose data met the data quality criteria were included for analysis. The statistics of selected registries, stratified by areas, gender, age and cancer types, were used to estimate the cancer incidence and mortality in 2012 in Guangdong province according to the population data in Guangdong province. Segi’s population and the national census population in 2000 were used for calculating the age-standardized rates (ASR). ResultsA total of 15,084,942 people, accounted for 17.47% of all population in Guangdong province, were covered in 8 selected population-based cancer registries in 2012. The percentage of cases morphologically verified (MV%) and the percentage of death certificate-only cases (DCO%) were 72.84% and 0.87%, respectively, and the mortality/incidence (M/I) ratio was 0.56. It was estimated that there were 211,300 new cancer cases and 117,300 cancer deaths. The incidence crude rate (CR), the ASR by Chinese standard population (ASRC) and by world standard population (ASRW), and the accumulated rate (AR) (0.74 years)were 250.20/100,000 (265.39/100,000 in males, 234.29/100,000 in females), 207.04/100,000, 201.34/100,000 and 22.91%, respectively, in Guangdong province in 2012. The incidence CR and ASRC were 267.25/100,000 and 221.43/100,000 in urban areas, and 215.51/100,000 and 178.77/100,000 in rural areas, respectively. The death CR, ASRC, ASRW and AR (0.74 years) were 148.44/100,000 (190.95/100,000 in males, 105.06/100,000 in females), 103.73/100,000, 102.44/100,000 and 11.68%, respectively, in Guangdong province in 2012. The death CR and ASRC were 164.57/100,000 and 105.46/100,000 in urban areas, and 124.63/100,000 and 99.97/100,000 in rural areas, respectively. Top 5 cancers were lung cancer, liver cancer, female breast cancer, colon cancer and nasopharyngeal cancers (NPC), and top 5 death cancers were lung cancer, liver cancer, colon cancer, stomach cancer, and NPC in Guangdong province in 2012. Conclusions Lung cancer, liver cancer, female breast cancer, colon cancer and NPC were the major economic cancer burdens and health concerns in Guangdong province in 2012. Early prevention, diagnosis and treatment of different cancers, survival quality improvement and cancer burden reduction, are important issues we faced in cancer control and prevention.
2016, 28(3): 321-329.
doi: 10.21147/j.issn.1000-9604.2016.03.06
Abstract:
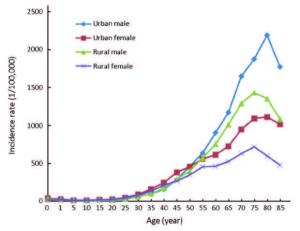
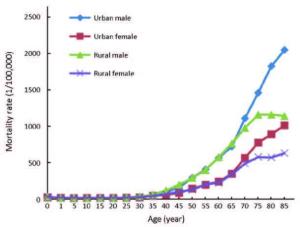
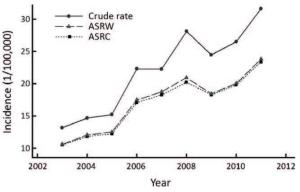
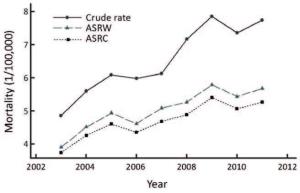
ObjectiveTo assess the incidence, mortality and survival status of female breast cancer in Jiangsu province of China. Methods Population-based cancer registry data in Jiangsu province were collected during 2003-2011. Crude rates, age-specific rates, age-standardized rates and annual percent changes of incidence and mortality were calculated to describe the epidemiologic characteristics and time trends. Patients diagnosed from 2003 to 2005 were chosen for analyzing the survival status of breast cancer. Results From 2003 to 2011, 17,605 females were diagnosed with breast cancer and 4,883 died in selected registry areas in Jiangsu province. The crude incidence rate was 25.18/100,000, and the age-standardized rates by Chinese population (ASRC) and by world population (ASRW) were 19.03/100,000 and 17.92/100,000, respectively. During the same period, the crude mortality rate was 6.98/100,000 and the ASRC and ASRW were 4.93/100,000 and 4.80/100,000, respectively. From 2003 to 2011, the incidence and mortality increased with annual percent change of 11.37% and 5.78%, respectively. For survival analysis, 1,392 patients in 7 areas were identified in 2003-2005 and finished 5 years of follow-up. Survival rates were found to decrease with survival years, the 5-year observed survival rate was 45.9% and the relative survival rate was 52.0%. We also found that the survival rate varied across the province, which was lower in the north and higher in the south of Jiangsu province. Conclusions Breast cancer has become a significant public health problem in Jiangsu province and China. More resources should be invested in primary prevention, earlier diagnosis and better health services in order to increase survival rates among Chinese females.
2016, 28(3): 339-347.
doi: 10.21147/j.issn.1000-9604.2016.03.08
Abstract:
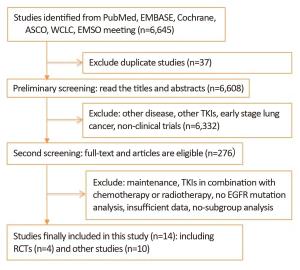
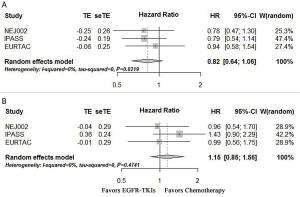
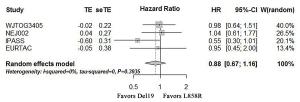
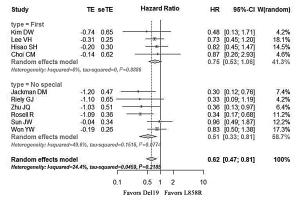
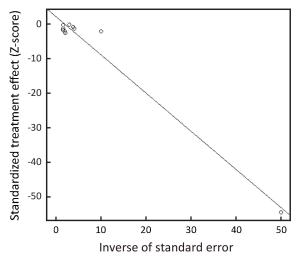
ObjectiveCombined overall survival (OS) analysis of Lux-Lung 3 and Lux-Lung 6 demonstrated that patients with epidermal growth factor receptor (EGFR) exon 19 deletions (Del19) would benefit from first-line second generation EGFR tyrosine kinase inhibitors (TKIs) afatinib but not for those with L858R. This study was to investigate the survival difference between first-line first generation EGFR-TKIs and chemotherapy in patients with either Del19 or L858R, and to directly compare OS in these two mutation groups. MethodsEligibles were all prospective and retrospective studies comparing EGFR-TKIs with conventional chemotherapy or receiving single agent EGFR-TKIs and demonstrating survival analysis based on mutation types. The primary outcome was OS measured as pooled hazard ratios (HRs). All measures were pooled using randomeffects models and 95% confidential interval (95% CI) was calculated. ResultsA total of 14 studies incorporating 1,706 patients with either Del19 or L858R were included. Enrolling patients with Del19 or L858R in randomized controlled trials (RCTs), first-line first generation EGFR-TKIs were associated with no OS benefit, compared with chemotherapy (pooled HRTKI/Chemo for Del19: 0.82, 95% CI: 0.64-1.06, P = 0.14; pooled HRTKI/Chemo for L858R: 1.15, 95% CI: 0.85-1.56, P = 0.38). Direct comparison of Del19 with L858R receiving with first-line first generation EGFR-TKIs demonstrated no significant survival difference (pooled HR19/21: 0.88, 95% CI: 0.67-1.16, P = 0.37). ConclusionsAmong patients with advanced non-small cell lung cancer (NSCLC) harboring Del19 and L858R, first-line first generation EGFR-TKIs demonstrated no survival benefit comparing with chemotherapy. Direct comparison between Del19 and L858R revealed no significant survival difference after first-line first generation EGFR-TKIs.
2016, 28(3): 348-354.
doi: 10.21147/j.issn.1000-9604.2016.03.09
Abstract:
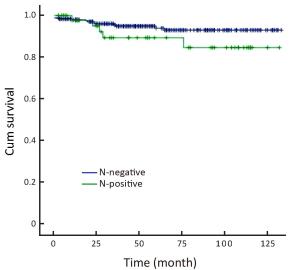
ObjectiveAccurate estimation of lymph node metastasis (LNM) in intramucosal gastric cancer is essential to select less invasive treatment options and even avoid surgery. The aim of this study was to evaluate combined clinicopathological features to predict the presence of LNM. MethodsA retrospective review of data from 386 intramucosal gastric cancer patients who underwent gastrectomy with extended lymphadenectomy from 2003 to 2010 was conducted. The mutual relation between clinicopathological characteristics and LNM was analyzed. ResultsLNM was detected in 40 (10.4%) of the 386 patients. Histological type and vascular or lymphatic invasion presence showed a positive correlation with LNM occurrence by univariate analysis. Multivariate analysis revealed that histological type was the only factor associated with LNM. Combined clinicopathologic characteristics would be more predictable for LNM. We found no LNM when we used combined clinicopathological characteristics conforming to Japanese absolute indications for endoscopic therapy. The LNM rate was as high as 8.7% when Japanese expanded criteria were used. Univariate analysis in cancer conformity to expand endoscopic submucosal dissection (ESD) indication also revealed that the undifferential type was the only significant factor for LNM. ConclusionsIt was possible to predict intramucosal gastric cancer cases without LNM using combined clinicopathological characteristic analysis. Extended indication for ESD should be cautiously used for intramucosal gastric cancer patients.
2016, 28(3): 355-361.
doi: 10.21147/j.issn.1000-9604.2016.03.10
Abstract:
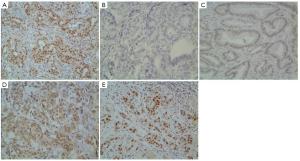
ObjectiveThe aim of this study is to identify the prognostic significance of X-ray cross-complementing gene 1 (XRCC1) in patients with gastric cancer undergoing surgery and platinum-based adjuvant chemotherapy. MethodsImmunohistochemistry (IHC) was used to evaluate XRCC1 protein expression profiles on surgical specimens of 612 gastric cancer patients. The relationship between XRCC1 expression and existing prognostic factors, platinum-based adjuvant chemotherapy, disease-free survival (DFS) and overall survival (OS) were analyzed. ResultsAmong 612 patients staged Ⅱ/Ⅲ in our study, 182 (29.74%) were evaluated as XRCC1 IHC positive. XRCC1 expression was not significantly related to OS (P = 0.347) or DFS (P = 0.297). Compared with surgery only, platinum-based adjuvant chemotherapy significantly improved the OS (P = 0.031). And the patients with negative XRCC1 expression benefited more from platinum-based adjuvant chemotherapy (P = 0.049). Multivariate analysis demonstrated that tumor size, T category, N category, vascular or nerve invasion and platinum-based chemotherapy were good prognostic factors for OS (P < 0.05). Though XRCC1 plays an important role in DNA repair pathways, no significant relationship is found in XRCC1 expression and OS among gastric cancer in our study. ConclusionsXRCC1 might be an alternative prognostic marker for the patients of gastric cancer after radical resection. The patients with negative XRCC1 expression can benefit more from platinum-based adjuvant chemotherapy.
2016, 28(3): 362-369.
doi: 10.21147/j.issn.1000-9604.2016.03.11
Abstract:
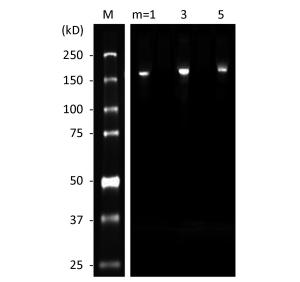
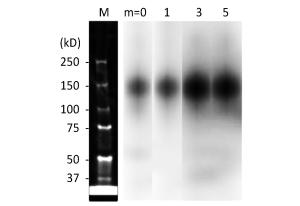
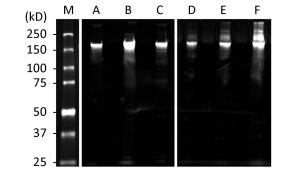
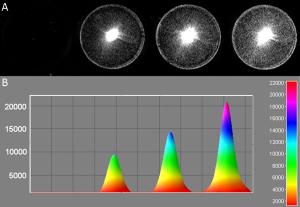
ObjectiveTo investigate the effect of fluorescent dye labeling on the targeting capabilities of 111In-(DTPA)n-trastuzumab-(IRDye 800)m. MethodsTrastuzumab-based conjugates were synthesized and conjugated with diethylenetriaminepentaacetic acid (DTPA) at molar ratios of 1, 2, 3 and 5 and with a fluorescent dye (IRDye 800CW) at molar ratios of 1, 3 and 5. Immunoreactivity and internalization were assessed on SKBR-3 cells, overexpressing human epidermal growth factor receptor 2. The stability in human serum and phosphate-buffered saline (PBS) was evaluated. The biodistribution of dual-labeled conjugates was compared with that of 111In-(DTPA)2-trastuzumab in a SKBR-3 xenograft model to evaluate the effect of dye-to-protein ratio. ResultsAll trastuzumab-based conjugates exhibited a high level of chemical and optical purity. Flow cytometry results showed that increasing dye-to-protein ratios were associated with decreased immunoreactivity. Stability studies revealed that the conjugate was stable in PBS, while in human serum, increased degradation and protein precipitation were observed with increasing dye-to-protein ratios. At 4 h, the percentages of internalization of dual-labeled conjugates normalized by dye-to-protein ratio (m) were 24.88%±2.10%, 19.99%±0.59%, and 17.47%±1.26% for "m" equal to 1, 3, and 5, respectively. A biodistribution study revealed a progressive decrease in tumor uptake with an increase in the dye-to-protein ratios. The liver, spleen and kidney showed a marked uptake with increased dye-to-protein ratios, particularly in the latter. ConclusionsWith non-specific-site conjugation of the fluorescent dye with a protein based on imaging agent, the increase in dye-to-protein ratios negatively impacted the immunoreactivity and stability, indicating a reduced tumor uptake.
2016, 28(3): 370-376.
doi: 10.21147/j.issn.1000-9604.2016.03.12
Abstract:
Sentinel lymph node biopsy (SLNB) is a new surgical technique for local axillary lymph nodes (ALNs) of breast cancer. Large-scale clinical trials have confirmed that undergoing SLNB and ALN dissection (ALND) showed no significant difference for sentinel lymph node (SLN)-negative patients in terms of disease-free survival, overall survival and recurrence-free survival. However, false-negative results are still the main concern of physicians as well as patients who undergo SLNB instead of ALND. The American Society of Breast Surgeons established a task force to suggest acceptable standards for SLNB. In 2000, the task force recommended that the identification rate for SLNB be 85% or higher and the false-negative rate be 5% or lower. This review focuses on clinical factors (tumor volume, multifocal/multi-center cancers, neoadjuvant chemotherapy and skip metastasis), tracer techniques and pathological factors affecting SLNB and explores methods for reducing the false-negative rate
Sentinel lymph node biopsy (SLNB) is a new surgical technique for local axillary lymph nodes (ALNs) of breast cancer. Large-scale clinical trials have confirmed that undergoing SLNB and ALN dissection (ALND) showed no significant difference for sentinel lymph node (SLN)-negative patients in terms of disease-free survival, overall survival and recurrence-free survival. However, false-negative results are still the main concern of physicians as well as patients who undergo SLNB instead of ALND. The American Society of Breast Surgeons established a task force to suggest acceptable standards for SLNB. In 2000, the task force recommended that the identification rate for SLNB be 85% or higher and the false-negative rate be 5% or lower. This review focuses on clinical factors (tumor volume, multifocal/multi-center cancers, neoadjuvant chemotherapy and skip metastasis), tracer techniques and pathological factors affecting SLNB and explores methods for reducing the false-negative rate
2016, 28(3): 377-379.
doi: 10.21147/j.issn.1000-9604.2016.03.13
Abstract:

 Abstract
Abstract FullText HTML
FullText HTML PDF 854KB
PDF 854KB