2017 Vol.29(6)
Display Mode: |
2017, 29(6): 471-476.
doi: 10.21147/j.issn.1000-9604.2017.06.01
Abstract:
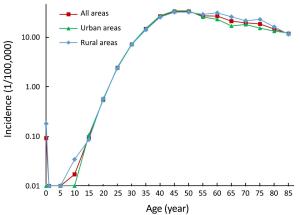
Objective Estimating the incidence and mortality rate of cervical cancer became necessary to establish prevention measures and healthy policies. The aim of this study was to estimate the updated incidence and mortality rate of cervical cancer in 2013 in China. Methods According to the evaluation criteria developed by the National Central Cancer Registry of China, the data submitted from 255 cancer registries met the required standards in 2013. Cervical cancer cases were retrieved from the national database and combined with the 2013 national population data. The age-standardized incidence and mortality rates were based on the demographic structure of the national census 2000 and Segi’s world population. Results In 2013, the estimated number of new cases and deaths from cervical cancer were 100,700 and 26,400, respectively. The crude incidence of cervical cancer was 15.17/100,000. The age-standardized incidence rates based on the Chinese standard population (ASIRC) and the world standard population (ASIRW) were 11.30/100,000 and 10.30/100,000, respectively. The incidence of cervical cancer in urban areas was 15.62/100,000 and the ASIRC was 11.12/100,000. The incidence of cervical cancer in rural areas was 14.65/100,000 and the ASIRC was 11.47/100,000. The mortality rate of cervical cancer was 3.98/100,000. The age-standardized mortality rates based on the Chinese (ASMRC) and world standard populations (ASMRW) were 2.76/100,000 and 2.62/100,000, respectively. The mortality rate of cervical cancer in urban areas was 3.85/100,000 and in rural areas was 4.14/100,000. Cervical cancer incidence and mortality increased with age. Urban areas had a higher incidence of cervical cancer and lower mortality rates when compared with rural areas. Conclusions Dynamic monitoring of cervical cancer incidence and mortality is the fundamental work of cervical cancer prevention and control. Cervical cancer is a serious issue in women’s health, and prevention strategies need to be enhanced, such as human papilloma virus (HPV) vaccination and screening programs.
2017, 29(6): 477-486.
doi: 10.21147/j.issn.1000-9604.2017.06.02
Abstract:
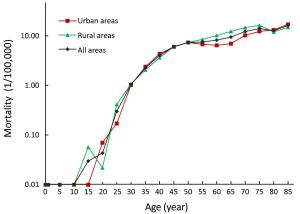
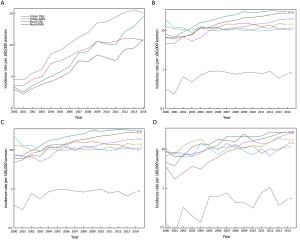
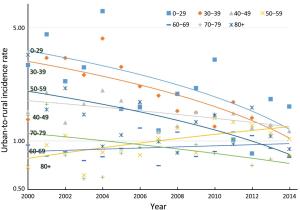
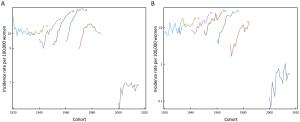
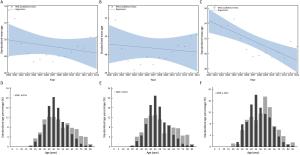
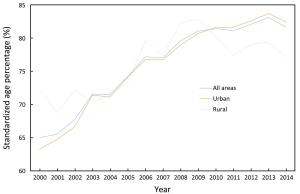
Objective To analyze the trends of incidence rate and age at diagnosis for cervical cancer incidence in China using population-based cancer registration data from 2000 to 2014. Methods Data were from National Central Cancer Registry of China. Crude incidence rates (CIRs), age-specific incidence rate, age-standardized incidence rates (ASIRs), age percentage distribution, standardized age percentage distribution, mean age at diagnosis and standardized mean age at diagnosis for cervical cancer in all areas of China, urban China and rural China were calculated separately. The world Segi’s population was applied to remove the age structure influence. Joinpoint regression was performed to obtain average annual percent change (AAPC) and age-period-cohort analysis was used to examine the incidence trends. Results CIRs and ASIRs for cervical cancer increased in China from 2000 to 2014. The AAPC of ASIRs in China was at 9.2% [95% confidence interval (95% CI): 7.0%–11.5%, P<0.05], and the AAPC in rural areas was relatively high. The age-specific incidence rate in groups aged 0–69 years have significantly increased over time. Groups aged 40–69 years showed the highest incidence risk, and the annual percent changes (APCs) of incidence rate in groups aged 40–59 years in urban China and groups aged 0–49 years in rural China were more than 10%. For each age group, the urban-to-rural incidence rate ratios (IRRs) got close to 1 over time. There were clear birth cohort effects in successive generations born from 1940 to 1970 in China. In rural China, the standardized mean age at diagnosis had significantly declined by 5.18 years. In China, the main peak and secondary peak of standardized age percentages appeared in the groups aged 45–49 and 40–44 years, respectively. In rural China, the main peak of standardized age percentage moved from the group aged 55–59 years to the group aged 45–49 years, and the standardized age percentages of groups aged 25–34 years also increased. In China, the standardized age percentages has significantly increased in groups aged 35–64 and 30–64 years over time, and accounted for about 80% and 85% in 2014, respectively. Conclusions The cervical cancer incidence increased in China and the gap of incidence between urban and rural China was narrowed. The trends of increasing cervical cancer incidence among younger women existed in China, especially in rural China. A more appropriate screening, vaccination and health education strategies should be established.
2017, 29(6): 487-495.
doi: 10.21147/j.issn.1000-9604.2017.06.03
Abstract:
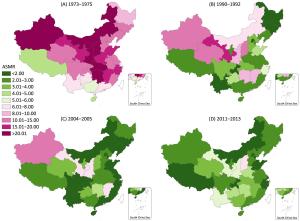
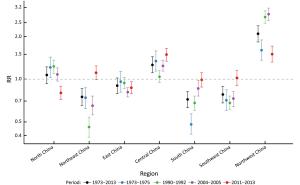
Objective This study was designed to explore the time trends in geographical variations of cervical cancer mortality in mainland China over the period 1973 to 2013, to provide subnational spatio-temporal patterns for targeted promotion of human papillomavirus vaccine in China. Methods Data were extracted from three national retrospective death surveys and cancer registry. The rate ratio (RR) was estimated for the aggregated data for seven geographical regions using generalized linear models to evaluate time trends in geographical disparities of cervical cancer mortality. Results There was a significant decrease in cervical cancer mortality in China from 1973–1975 to 2004–2005, but leveled off thereafter to 2011–2013. Compared to the period 1973–1975 the RR for the three last time periods were 0.33 [95% confidence interval (95% CI): 0.30–0.37] for 1990–1992, 0.21 (95% CI: 0.19–0.24) for 2004–2005 and 0.24 (95% CI: 0.22–0.26) for 2011–2013. Females living in the Northwest China and Central China have a high risk of mortality from cervical cancer compared to the nationwide, with the RR being 2.09 (95% CI: 1.83–2.38) and 1.26 (95% CI: 1.11–1.44) respectively, while the RRs for South China, Northeast China and Southwest China were below 1.00, indicating the lower death risk. Despite the mortality rate had increased slightly from 2004 to 2013, there was an encouraging sign that the geographical disparities in cervical cancer mortality had gradually narrowed over time across China. Conclusions Although cervical cancer mortality in China has reduced to very low levels, the high risk of cervical cancer in Northwest China and Central China is still noteworthy. Public health policies including the promotion of vaccine should be targeted to further reduction of geographical disparities in cervical cancer mortality.
2017, 29(6): 496-509.
doi: 10.21147/j.issn.1000-9604.2017.06.04
Abstract:
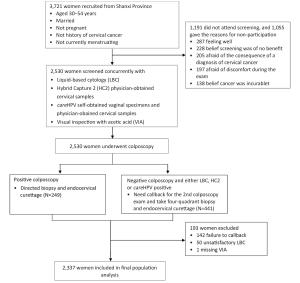
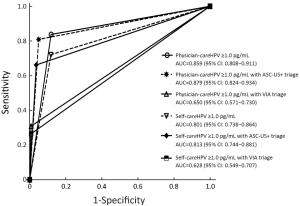
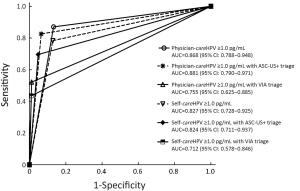
Objective CareHPV is a human papillomavirus (HPV) DNA test for low-resource settings (LRS). This study assesses optimum triage strategies for careHPV-positive women in LRS. Methods A total of 2,530 Chinese women were concurrently screened for cervical cancer with visual inspection with acetic acid (VIA), liquid-based cytology and HPV testing by physician- and self-collected careHPV, and physician-collected Hybrid Capture 2 (HC2). Screen-positive women were referred to colposcopy with biopsy and endocervical curettage as necessary. HPV-positivity was defined as ≥1.0 relative light units/cutoff (RLU/CO) for both careHPV and HC2. Primary physician-HC2, physician-careHPV and self-careHPV and in sequential screening with cytology, VIA, or increased HPV test-positivity performance, stratified by age, were assessed for cervical intraepithelial neoplasia (CIN) grade 2/3 or worse (CIN2/3+) detection. Results The sensitivities and specificities of primary HPV testing for CIN2+ were: 83.8%, 88.1% for physician-careHPV; 72.1%, 88.2% for self-careHPV; and 97.1%, 86.0% for HC2. Physician-careHPV test-positive women with VIA triage had a sensitivity of 30.9% for CIN2+ versus 80.9% with cytology triage. Self-careHPV test-positive women with VIA triage was 26.5% versus 66.2% with cytology triage. The sensitivity of HC2 test-positive women with VIA triage was 38.2% versus 92.6% with cytology triage. The sensitivity of physician-careHPV testing for CIN2+ decreased from 83.8% at ≥1.0 RLU/CO to 72.1% at ≥10.00 RLU/CO, while the sensitivity of self-careHPV testing decreased from 72.1% at ≥1.0 RLU/CO to 32.4% at ≥10.00 RLU/CO; similar trends were seen with age-stratification. Conclusions VIA and cytology triage improved specificity for CIN2/3 than no triage. Sensitivity with VIA triage was unsuitable for a mass-screening program. VIA provider training might improve this strategy. Cytology triage could be feasible where a high-quality cytology program exists. Triage of HPV test-positive women by increased test positivity cutoff adds another LRS triage option.
2017, 29(6): 510-520.
doi: 10.21147/j.issn.1000-9604.2017.06.05
Abstract:
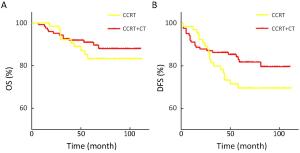
Objective The aim of this study was to investigate the prognostic factors and to evaluate the impact of adjuvant therapy on clinical outcome for early-stage cervical cancer. Methods The clinical-pathological data of all 1,335 patients with the International Federation of Gynecology and Obstetrics (FIGO) Ib–IIa cervical cancer treated with primary radical surgery at the Chinese National Cancer Center between May 2007 and Dec 2013 were retrospectively reviewed. The median follow-up was 70 months. Results Of all the patients, 61.6% of the cases received adjuvant therapy, with 5-year disease-free survival (DFS) of 92.1% and 5-year overall survival (OS) of 95.0%. In multivariate analysis, differentiation of G3 (P<0.05), lymph node metastasis (LNM, P<0.05) and lymphovascular space invasion (LVSI, P<0.05) were independent predictors for OS, while LNM (P<0.05), deep stroma invasion (DSI, P<0.05) and LVSI (P<0.05) were independent factors for DFS. The samples were stratified by histologic type, and cervical squamous cell carcinoma (SCC) was found to share the same independent factors except for differentiation of OS. As to patients with cervical adenocarcinoma/adenosquamous carcinoma (AC/ASC), differentiation was the independent predictor of OS (P<0.05); and LVSI of DFS (P<0.05). Of 236 patients with high-risk factors, there was no significant difference in survival between concurrent chemoradiotherapy (CCRT, n=195), radiotherapy (RT, n=24), and chemotherapy (CT, n=17). Among the 190 patients with LNM who underwent CCRT, 124 cases showed improved DFS after sequential CT (P=0.118), with a recurrence rate decrease of 14%, though the difference was not statistically significant. Patients with single intermediate-risk factors like DSI or LVSI were found to partially benefit from adjuvant therapy, but the difference was not statistically significant. Conclusions LNM, LVSI, DSI and differentiation were found to be independent prognostic factors for operable cervical cancer. Aggressive postoperative adjuvant therapy based on single risk factors in Chinese National Cancer Center could benefit survival. CCRT+CT outperformed CCRT in high-risk patients. For patients with single non-high-risk factor, the role of adjuvant therapy needs to be further discussed.
2017, 29(6): 521-532.
doi: 10.21147/j.issn.1000-9604.2017.06.06
Abstract:
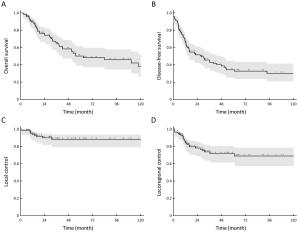
Objective Primary uterine leiomyosarcomas (ULMS) are rare, and the optimal treatment is controversial. We aimed to assess the outcome and prognostic factors in a multicenter population of women treated for primary ULMS. Methods We retrospectively collected data of 110 women treated in 19 institutions of the Rare Cancer Network (RCN). Inclusion criteria consisted of a pathology report confirming the diagnosis of ULMS, aged 18–80 years, complete International Federation of Gynecology and Obstetrics (FIGO) stage information, complete information on treatment, and a minimum follow-up of 6 months. Local control (LC) and locoregional control (LRC), overall survival (OS) and disease-free survival (DFS) rates were computed using the Kaplan-Meier method. Univariate analysis was implemented using the log rank test, and multivariate analysis using the Cox model. Results All patients underwent surgery. Seventy-five patients (68%) received adjuvant radiotherapy (RT), including brachytherapy in 18 (16%). Seventeen patients (15%) received adjuvant chemotherapy. Median follow-up was 58 (range, 6–240) months. Five-year OS and DFS rates were 50% and 34%, and LC and LRC rates were 88% and 72%, respectively. On multivariate analysis, independent favorable prognostic factors were younger age, FIGO stage I, small tumor size, previous uterine disease, and no vascular invasion for OS and DFS. FIGO stage was the only favorable factor influencing LRC. Adjuvant local or systemic treatments did not improve the outcomes. Eight patients treated with RT presented a grade 3 acute toxicity, and only one patient with grade 3 late toxicity. Conclusions In this large population of primary ULMS patients, we found good results in terms of LC and LRC. Nevertheless, OS remains poor, mainly due to the occurrence of distant metastases. An early diagnosis seemed to improve the prognosis of the patients. Adjuvant local or systemic treatments, or more aggressive surgical procedures such as the Wertheim procedure, did not seem to impact the outcome.
2017, 29(6): 543-552.
doi: 10.21147/j.issn.1000-9604.2017.06.09
Abstract:
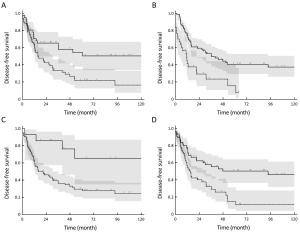
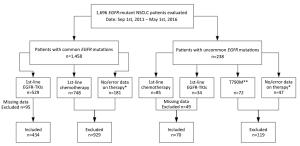
Objective Data on the clinical activity of epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) in patients with non-small-cell lung cancer (NSCLC) and uncommon EGFR mutations remain insufficient. This study aimed to investigate the effect of first-line EGFR-TKIs or platinum-based chemotherapy in NSCLC patients with uncommon EGFR mutations. Methods We retrospectively enrolled 504 patients with EGFR-mutant NSCLC. The clinical characteristics and treatment outcomes were collected and compared between patients with common and uncommon EGFR-mutant NSCLC. Results Seventy patients (13.9%) harboring uncommon EGFR mutations were included. Thirty of these patients received EGFR-TKIs and 40 received platinum-based chemotherapy as first-line therapy. The objective response rate (ORR) and median progression-free survival (mPFS) of patients treated with TKIs in the uncommon mutation group was significantly inferior to that in the common mutation group (ORR: 23.3% vs. 51.8%, P=0.003; mPFS: 7.1 vs. 10.9 months, P<0.001). In the uncommon group, mPFS was similar between first-line EGFR-TKIs treatment and platinum-based chemotherapy (7.1vs. 6.1 months, P=0.893). In patients with EGFR G719X or L861Q mutations, the mPFS was longer in the first-line EGFR-TKIs treatment group than in the chemotherapy group, but the difference was not statistically significant (G719X: 8.2 vs. 5.8 months, P=0.061; L861Q: 7.6 vs. 4.1 months, P=0.872). Multivariate analyses identified adenocarcinoma (P=0.003) as the independent predictive factor for PFS in patients with uncommon EGFR mutations who were treated with first-line EGFR-TKIs. Conclusions The current study demonstrated that the effect of first-line EGFR-TKIs was similar to that of platinum-based chemotherapy in patients with uncommon EGFR-mutant NSCLC. Adenocarcinoma was the independent predictive factor for PFS in uncommon EGFR-mutant NSCLC patients treated with first-line EGFR-TKIs.
2017, 29(6): 553-560.
doi: 10.21147/j.issn.1000-9604.2017.06.10
Abstract:
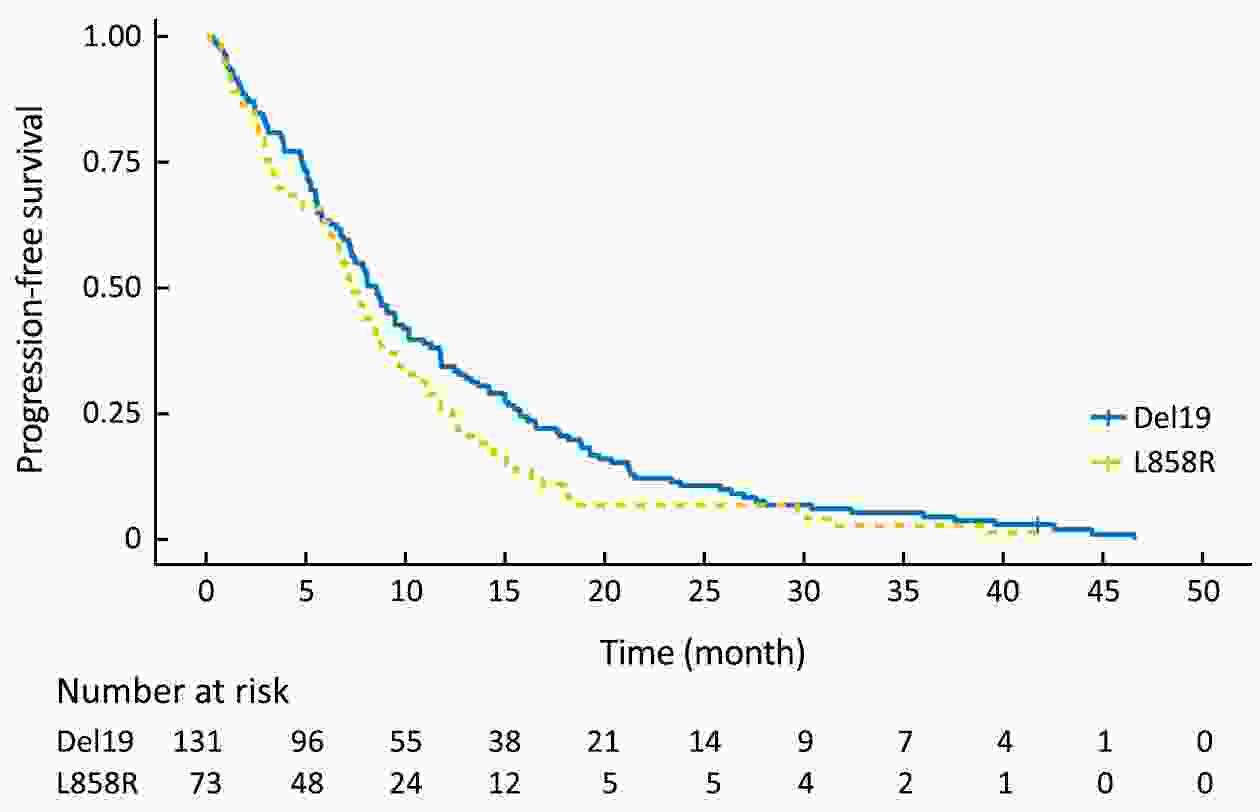
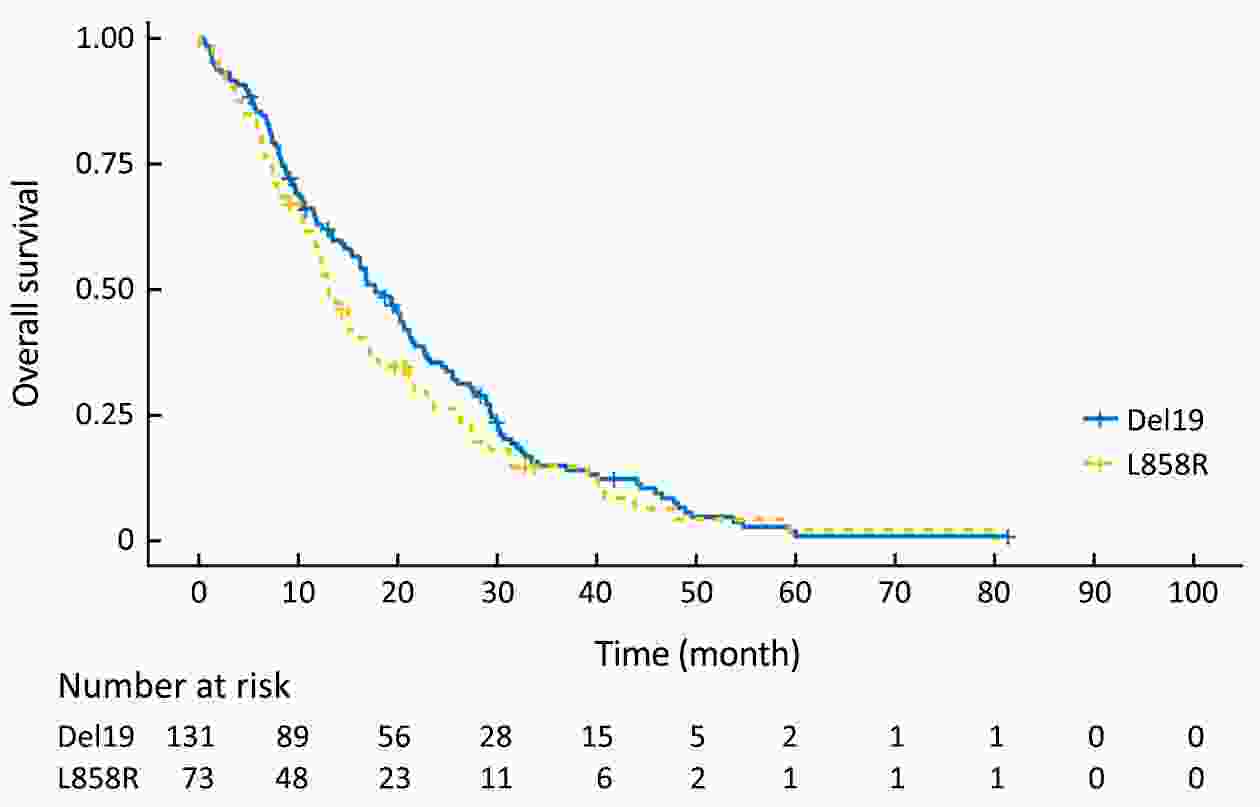
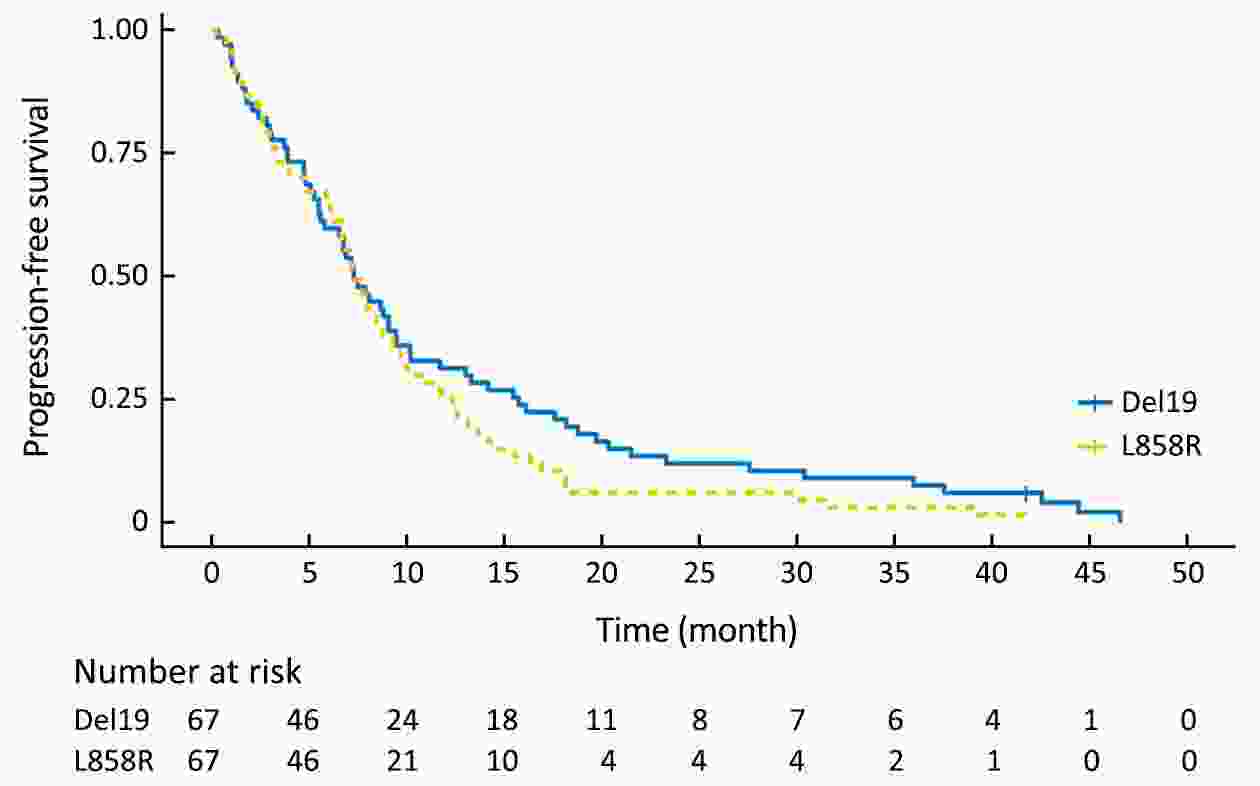
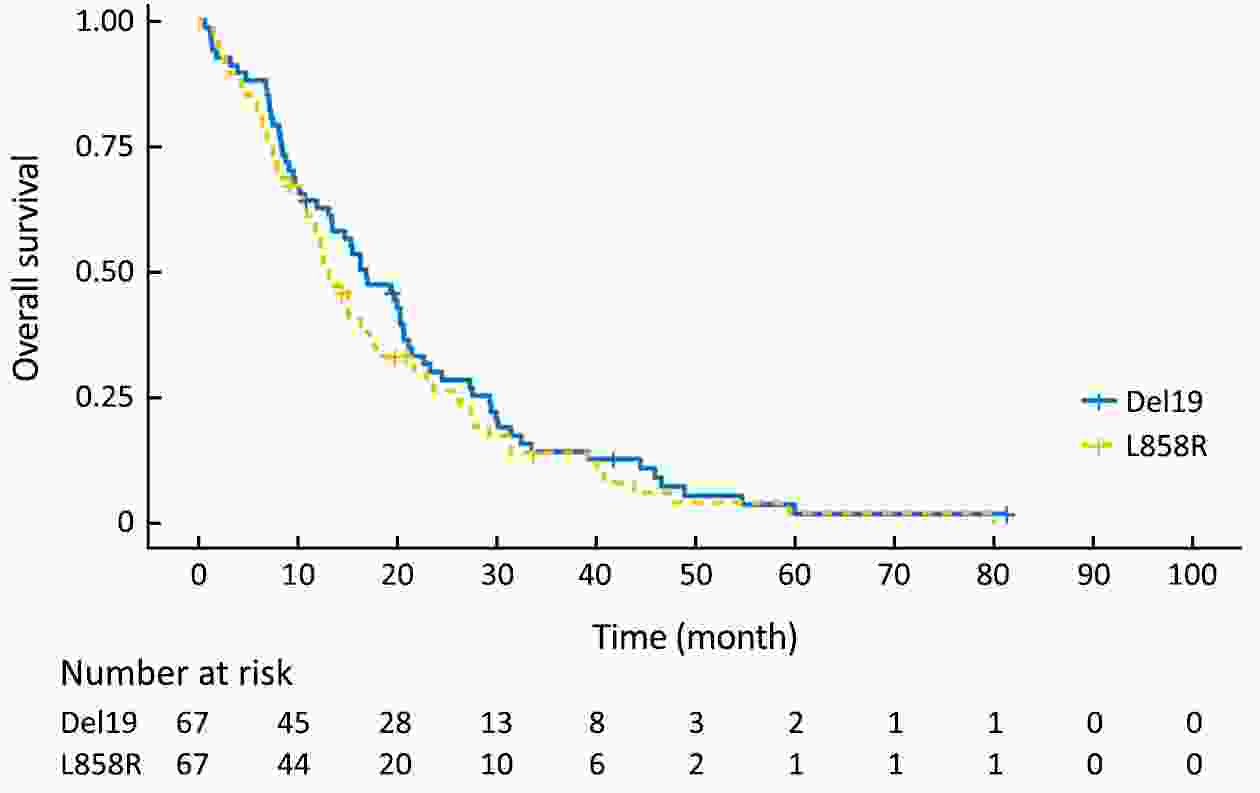
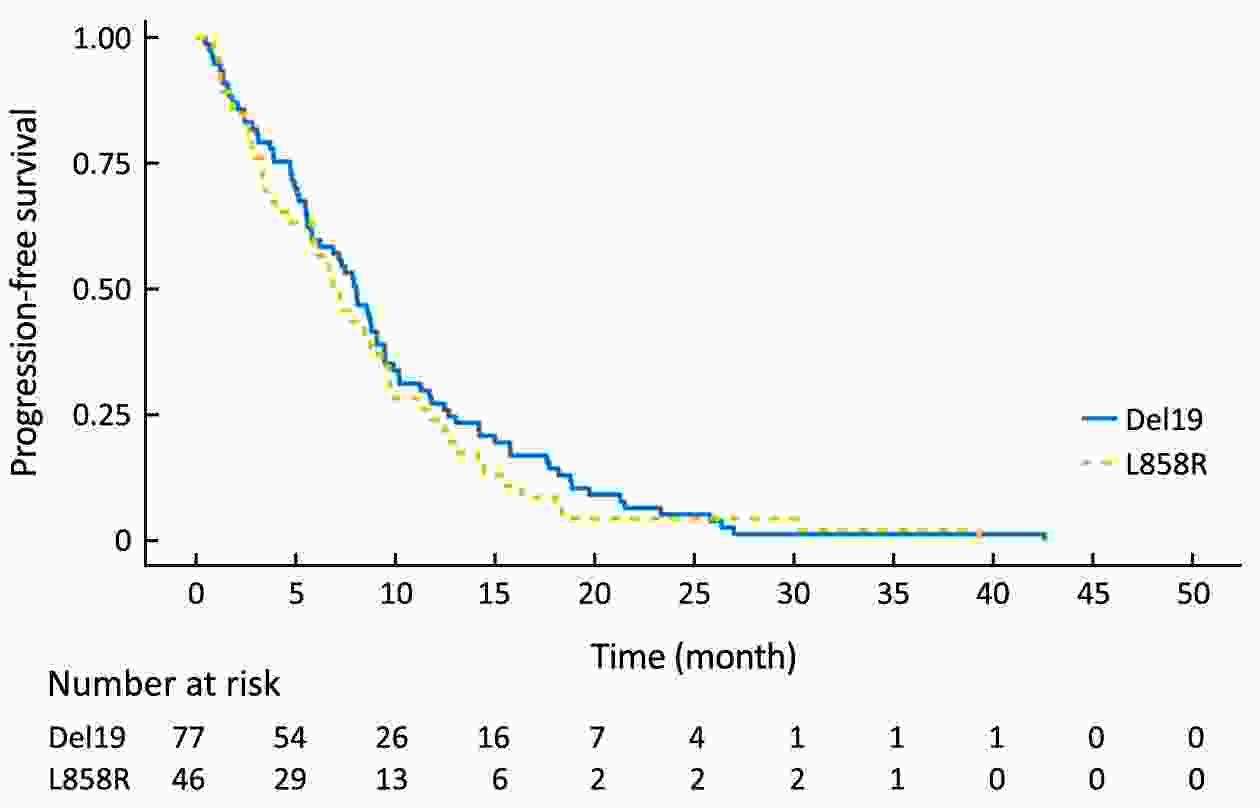
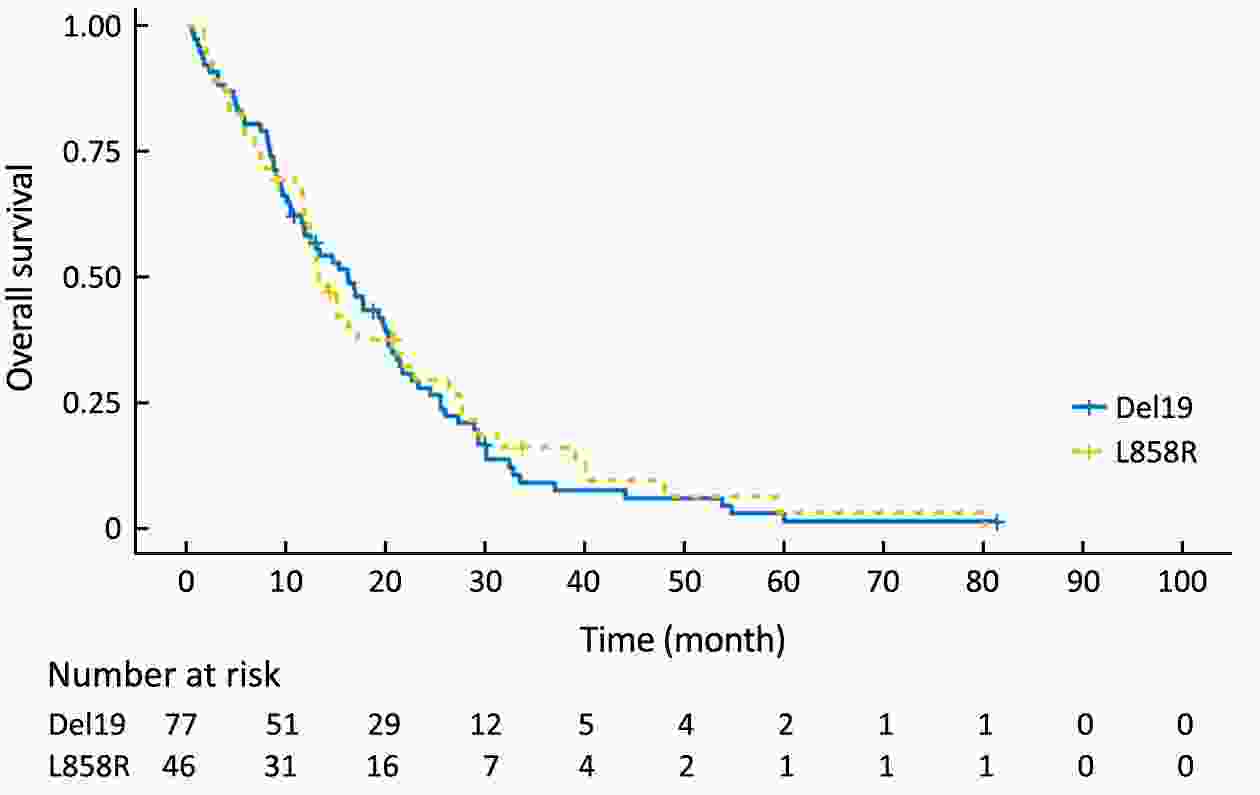
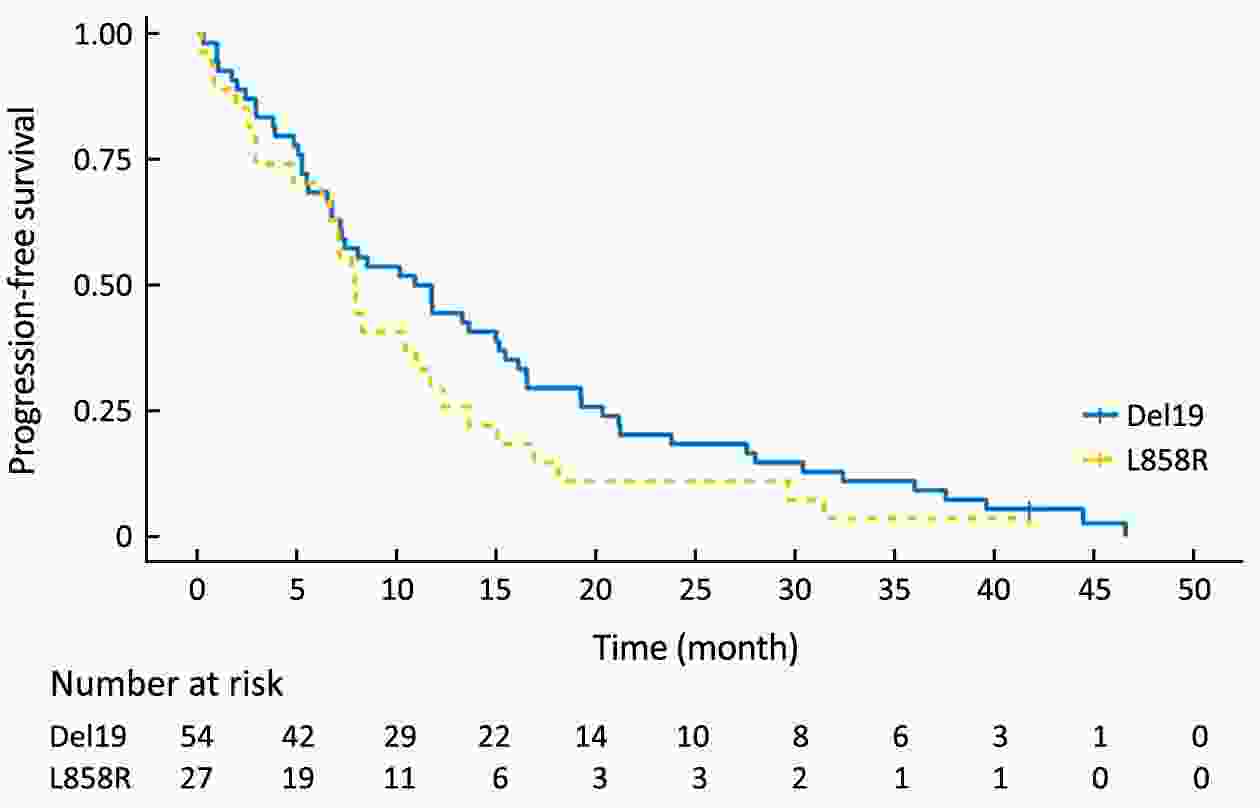
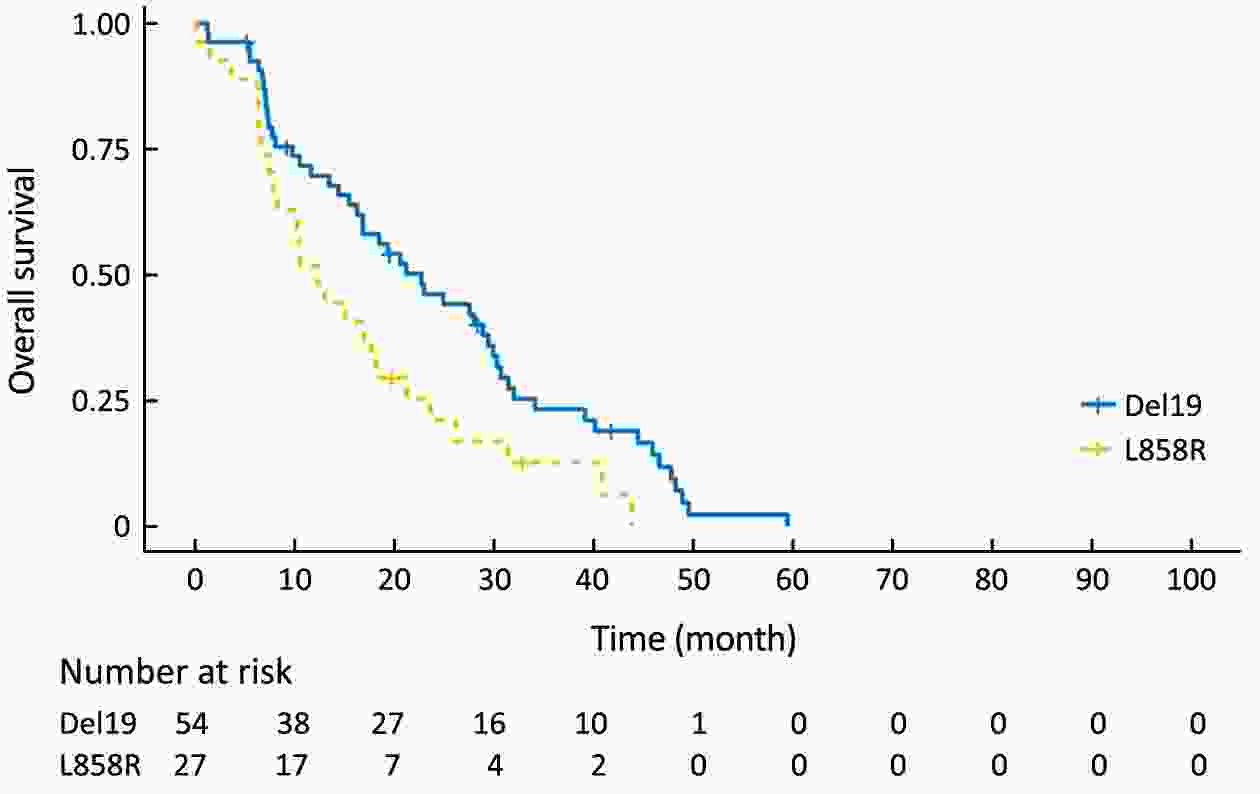
Objective Although superior clinical benefits of epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) in the treatment of advanced non-small-cell lung cancer (NSCLC) had been reported, the survival difference between exon 19 deletion (Del19) and exon 21 Leu858Arg substitution (L858R) remains controversial. The purpose of this study is to investigate the differences in progression-free survival (PFS) and overall survival (OS) between different EGFR mutant subtypes among advanced NSCLC patients receiving gefitinib. Methods There were 204 advanced NSCLC patients with EGFR mutations treated with gefitinib were enrolled in this retrospective cohort study. Patients were divided into the EGFR Del19 group and the L858R mutated group according to their mutant subtype. Propensity score matching (PSM) was conducted by using a nearest-neighbor algorithm (1:1) to adjust for demographical and clinical covariates. Survival curves were constructed with the Kaplan-Meier method and compared by using the log-rank test. Results The PFS in Del19 group was similar to that in the L858R group [before PSM 8.6 vs. 7.2 months, P=0.072; after PSM 7.3 vs. 7.2 months, P=0.155]. No differences were detected in OS between the L858R and the Del19 group (before PSM 17.8 vs. 13.1 months, P=0.253; after PSM 16.9 vs. 13.1 months, P=0.339). The Del19 group was significantly younger compared with the L858R mutation group in age (P=0.015). Conclusions No significant difference was found in the PFS or OS between the Del19 and L858R mutant NSCLC patients receiving gefitinib. The age gap might contribute to the survival differences between Del19 and L858R groups. PSM is of important value to the elimination of potential bias.
2017, 29(6): 561-571.
doi: 10.21147/j.issn.1000-9604.2017.06.11
Abstract:
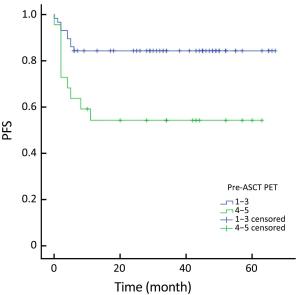
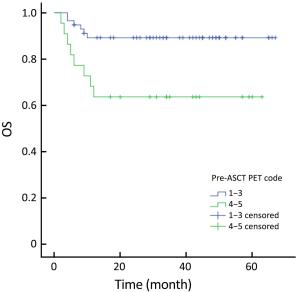
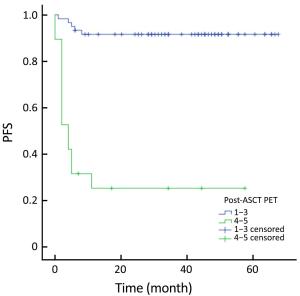
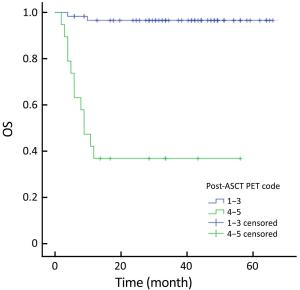
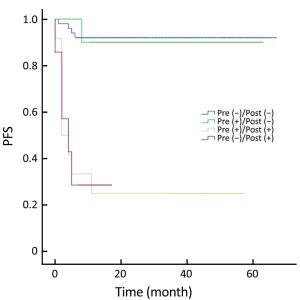
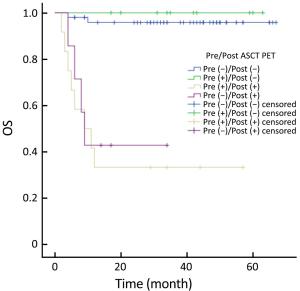
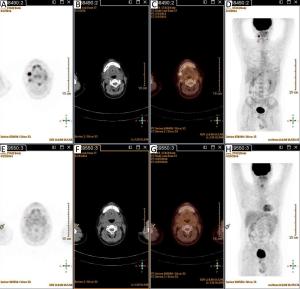
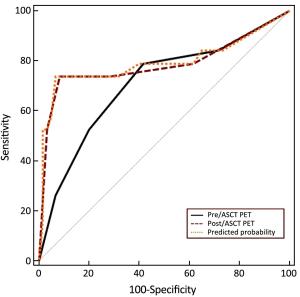
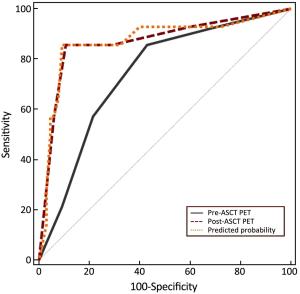
Objective High-dose chemotherapy (HDC) followed by autologous stem cell transplantation (ASCT) is the standard of care in the upfront or relapsed/refractory setting in some patients with non-Hodgkin lymphoma (NHL). However, a proportion of patients do not respond to ASCT. 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) has been widely used for staging, response evaluation, and prognosis prediction. Here, we investigated the prognostic role of PET/CT in NHL patients before and after ASCT. Methods A retrospective study was conducted at Peking University Cancer Hospital. All NHL patients who underwent ASCT between March 2010 and July 2016 were identified. Patients who had PET/CT scan before and after ASCT were included. Deauville criteria (5-point scale) were used to interpret PET scans. Univariate and multivariate survival analyses were performed using Cox regression. The predictive value of PET scanning was estimated by comparing the area under the receiver operating characteristic (ROC) curve. Results In total, 79 patients were enrolled in this study. In univariate analysis, pre- and post-ASCT PET result was identified as prognostic factors for 3-year progression-free survival (PFS) and overall survival (OS). Patients with negative pre-ASCT PET result demonstrated significantly better PFS (84.2% vs. 54.2%) and OS (89.2% vs. 63.6%) than patients with positive pre-ASCT PET result. PFS (91.6% vs. 25.3%) and OS (96.5% vs. 36.8%) were also significantly different between patients with negative and positive post-ASCT PET result. Multivariate analysis also showed a significant association between survival and post-ASCT PET result. ROC analysis revealed that the predictive value of post-ASCT PET result was superior to that of pre-ASCT PET result alone. Combined pre- and post-ASCT PET result is better for predicting outcomes in patients with NHL receiving transplantation. Deauville criteria score >3 was identified as the best cutoff value for post-ASCT PET. Conclusions Post-ASCT PET result was more important than pre-ASCT PET result in predicting outcomes for NHL patients who underwent ASCT. The prognostic significance can be improved when combining pre-ASCT PET result with post-ASCT PET result. Deauville criteria can be used for interpreting PET scans in this scenario.
2017, 29(6): 572-580.
doi: 10.21147/j.issn.1000-9604.2017.06.12
Abstract:
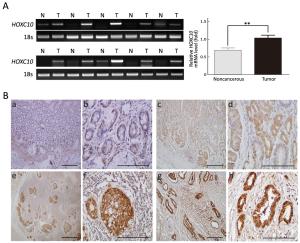
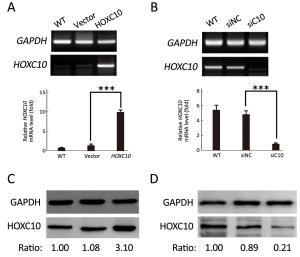
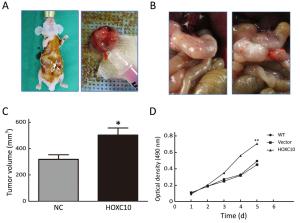
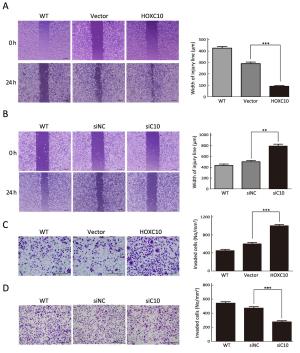
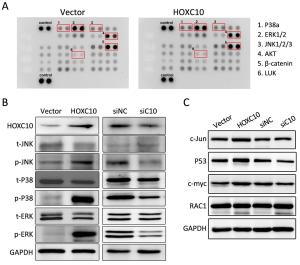
Objective As an important regulator of embryonic morphogenesis, homeodomain-containing gene 10 (HOXC10) has been found to promote progression of human cancers and its expression indicates poor survival outcome. However, very few studies are available on the role of HOXC10 in gastric carcinoma. Therefore, the aim of this study was to determine the role of HOXC10 in gastric cancer and the potential mechanism underlying its function for cancer biology. Methods A primary gastric cancer mouse model was obtained via intra-gastric wall injection of gastric cancer cells and was used to evaluate the function of HOXC10 during gastric cancer progression in vivo. Immunohistochemistry was performed to visualize and measure HOXC10 protein expression in gastric cancer tissue. Cells were transfected with plasmids to increase the expression of HOXC10, and siRNA transfection was performed to suppress HOXC10 expression. Reverse transcription polymerase chain reaction (RT-PCR) and western blotting were utilized to measure mRNA and protein expression, respectively. Proliferation, migration, and invasion were investigated using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, wound healing assay, and matrigel invasion assay in vitro, respectively. Results HOXC10 expression was significantly increased in gastric cancer tissues compared to matched normal tissues. HOXC10 up-regulation significantly increased tumor volumes in nude mice. Plasmid transfection significantly increased HOXC10 protein and mRNA expressions and effectively promoted cell proliferation. Moreover, HOXC10 up-regulation significantly promoted migration and invasion of gastric cancer cells. Mechanistic investigation showed that HOXC10 up-regulation significantly increased mRNA and protein expression of mitogen-activated protein kinase (MAPK) signaling related genes, including c-myc, c-jun and p53, while also modulating the phosphorylation of c-Jun N-terminal kinase (JNK), extracellular signal-regulated kinase (ERK) and P38 but not their total protein levels. Conclusions This study demonstrated the tight link between HOXC10 and gastric cancer cell proliferation and metastasis via involvement of the MAPK pathway.
2017, 29(6): 581-586.
doi: 10.21147/j.issn.1000-9604.2017.06.13
Abstract:
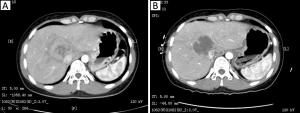
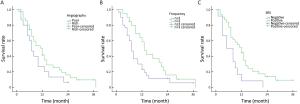
Objective To analyze the angiography appearance of liver metastases from gastroenteropancreatic neuroendocrine tumors (GEP-NETs), and evaluate the clinical efficacy and prognostic factors of interventional treatment for hepatic metastases. Methods Fifty GEP-NETs patients with hepatic metastases were treated from January 2012 to December 2016, and received transarterial embolization (TAE) in the hepatic tumor or hepatic arterial infusion chemotherapy (HAIC). All patients received 179 times of the intervention therapy in total. Results Blood supplies were identified in the 50 cases with angiography, which showed that 35 cases had abundant vessels, while 15 cases had poor blood supply. Twenty-two cases were found either collateral blood supply, or portal vein invasion or arterial-portal vein fistula. The best curative efficacy was complete remission (CR) in 4 cases, partial remission (PR) in 28 cases and stable disease (SD) in 18 cases during the process of treatment. The angiography (P=0.047) and the frequency of intervention (P=0.037) showed significantly statistical difference with Kaplan-Meier analysis. The Cox analysis showed that more than 3 times of interventional therapy was an independent prognostic factor. Conclusions Interventional treatment is safe and effective for GEP-NETs, and is beneficial to patients with main hepatic metastases after endocrine therapy.
2017, 29(6): 533-534.
doi: 10.21147/j.issn.1000-9604.2017.06.07
Abstract:
2017, 29(6): 587-588.
doi: 10.21147/j.issn.1000-9604.2017.06.14
Abstract:
2017, 29(6): 535-542.
doi: 10.21147/j.issn.1000-9604.2017.06.08
Abstract:
Leptomeningeal metastasis is an uncommon but serious complication in patients with advanced cancers. Leptomeningeal metastasis is diagnosed in approximately 5% of the patients, most commonly among patients with cancers of breast and lung, melanoma, and gastrointestinal malignancies. Treatment goal is to improve survival and quality of the patients. Use of targeted therapies and immunotherapy has led to improved survival of patients with non-small cell lung cancer (NSCLC). In this article, we review emerging data on use of mutation-specific agents and immunotherapy in the treatment of leptomeningeal metastasis among patients with NSCLC.
Leptomeningeal metastasis is an uncommon but serious complication in patients with advanced cancers. Leptomeningeal metastasis is diagnosed in approximately 5% of the patients, most commonly among patients with cancers of breast and lung, melanoma, and gastrointestinal malignancies. Treatment goal is to improve survival and quality of the patients. Use of targeted therapies and immunotherapy has led to improved survival of patients with non-small cell lung cancer (NSCLC). In this article, we review emerging data on use of mutation-specific agents and immunotherapy in the treatment of leptomeningeal metastasis among patients with NSCLC.

 Abstract
Abstract FullText HTML
FullText HTML PDF 331KB
PDF 331KB