2018 Vol.30(3)
Display Mode: |
2018, 30(3): 291-298.
doi: 10.21147/j.issn.1000-9604.2018.03.01
Abstract:
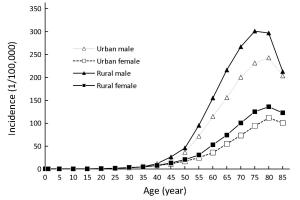
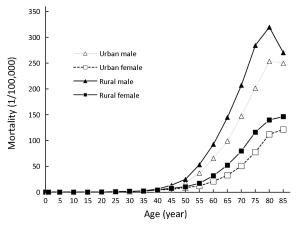
Objective In this study, we aimed to estimate the updated incidence and mortality rate of stomach cancer based on the cancer registration data in 2014, collected by the National Central Cancer Registry of China (NCCRC). Methods In 2017, 339 registries’ data were qualified based on the criteria of data quality control of the NCCRC. Cases of stomach cancer were retrieved from the national database. We estimated numbers of stomach cancer cases and deaths in China using age-specific rates and corresponding national population stratified by area, sex, age-group (0, 1–4, 5–9, 10–14, …, 85+). Chinese standard population in 2000 and Segi’s world population were applied for age-standardized incidence and mortality rates. Results In 2014, 410,400 new stomach cancer cases and 293,800 cancer-associated deaths were estimated to have occurred in China. The crude incidence rate of stomach cancer was 30.00/100,000, age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 19.62/100,000 and 19.51/100,000, respectively. The crude mortality rate of stomach cancer was 21.48/100,000, age-standardized mortality rates by Chinese (ASMRC) and by world standard population (ASMRW) were 13.44/100,000 and 13.30/100,000, respectively. Incidence and mortality rates in rural areas were both higher than that in urban areas. Stomach cancer has a strong relationship with gender and age. The disease has occurred more frequently among men than women with a male to female ratio of 2.4 for ASIRC. After age group of 40−44 years, incidence rates are substantially higher in men than in women, same pattern was seen for age-specific mortality rates. Conclusions There is still a heavy burden of stomach cancer in China. The incidence and mortality patterns of stomach cancer show substantial gender and regional disparities. Great effort is needed to provide more accessible health services, sufficient financial resources, and adequate cancer-care infrastructure for the Chinese population, especially for people living in rural areas.
2018, 30(3): 299-306.
doi: 10.21147/j.issn.1000-9604.2018.03.02
Abstract:
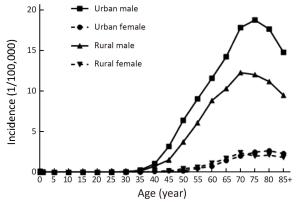
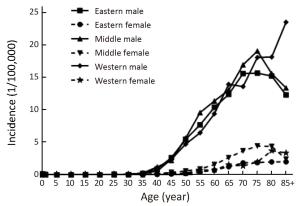
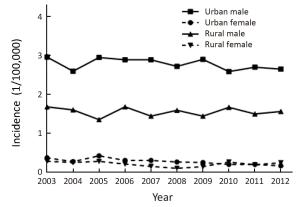
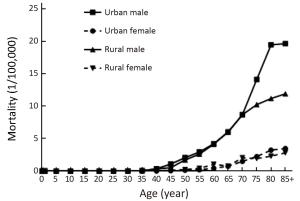
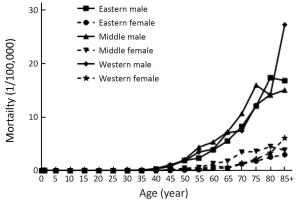
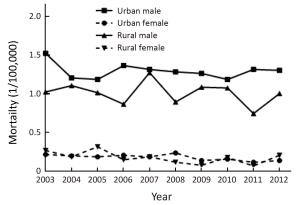
Objective To analyze the incidence and mortality rates of laryngeal cancer in China from 2008 to 2012. Methods Incident and death cases of laryngeal cancer were retrieved from the National Central Cancer Registry (NCCR) database collecting from 135 cancer registries in China during 2008–2012. The crude incidence and mortality rates of laryngeal cancer were calculated by area (urban/rural), region (eastern, middle, western), gender and age group (0, 1–4, 5–9, …, 85+). China census in 2000 and Segi’s world population were applied for age standardized rates. JoinPoint (Version 4.5.0.1) model was used for time trend analysis. Results The crude incidence rate of laryngeal cancer was 1.86/100,000 ranked the 21st in overall cancers. The age-standardized incidence rates by China population (ASIRC) and by World population (ASIRW) were 1.22/100,000 and 1.23/100,000, respectively. The crude mortality of laryngeal cancer in China was 1.01/100,000 and it was the 21st cause of cancer-related death in overall cancers. Both the age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 0.63/100,000. Incidence and mortality rates of laryngeal cancer were higher in males than in females and higher in urban areas than in rural areas. Middle areas had the highest incidence and mortality rates followed by eastern and western areas. Incidence and mortality rates of laryngeal cancer retained low level before age of 40 years old but increased greatly after and peaked in age group of 75. Incidence showed significant down trends in recent 10 years by 1.27% annually [95% confidence interval (95% CI): –2.2%, –0.3%]. Mortality declined in females sharply by 5.18% per year although stable in males and both sexes combined. Conclusions Appropriate targeted prevention, early detection and treatment programs should be carried out to control the local burden of laryngeal cancer.
2018, 30(3): 307-314.
doi: 10.21147/j.issn.1000-9604.2018.03.03
Abstract:
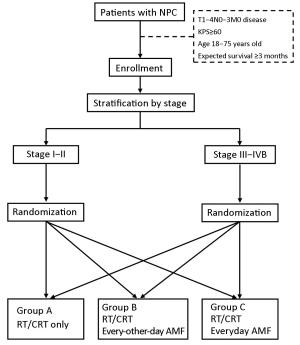
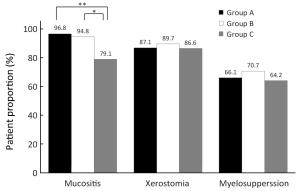
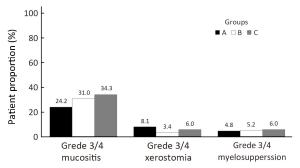
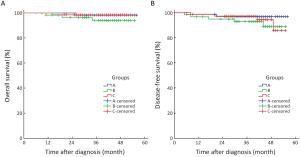
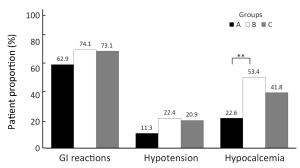
Objective The radioprotective effects of amifostine remain uncertain in patients with nasopharyngeal carcinoma (NPC), and adverse effects and cost limit generalization of its classical everyday regimen. This phase II multicenter randomized controlled trial aimed to explore whether amifostine could ameliorate the toxicities of NPC patients in the era of intensity-modulated radiotherapy (IMRT), and to compare different regimens of amifostine on effectiveness and safety. Methods Patients with stage I–IVB NPC were involved prospectively from January 1st, 2013. All patients received radical treatment based on IMRT. After a randomization stratified by their stage, these patients were allocated into 3 groups: the group treated without amifostine, the group treated with the everyday regimen of amifostine, and the group treated with the every-other-day regimen. The 3 groups of patients were compared on radiotherapy-related acute toxicities, treatment effects of NPC, and amifostine-related complications. This trial was registered on the clinicaltrials.gov (ID: NCT01762514). Results Until August 31st, 2017, totally 187 patients completed experimental intervention. Only amifostine of everyday regimen appeared to reduce the patient proportion of mucositis (79.1% vs. 96.8%, P=0.002). Hypocalcemia was less common in patients treated without amifostine than in those treated with amifostine (22.6% vs. 53.4% vs. 41.8%, P=0.002). Neither complete remission rates nor the survivals were affected by amifostine. Conclusions Amifostine of everyday regimen could reduce mucositis in NPC patients who received IMRT, though it also had the possibility to cause more hypocalcemia.
2018, 30(3): 315-326.
doi: 10.21147/j.issn.1000-9604.2018.03.04
Abstract:
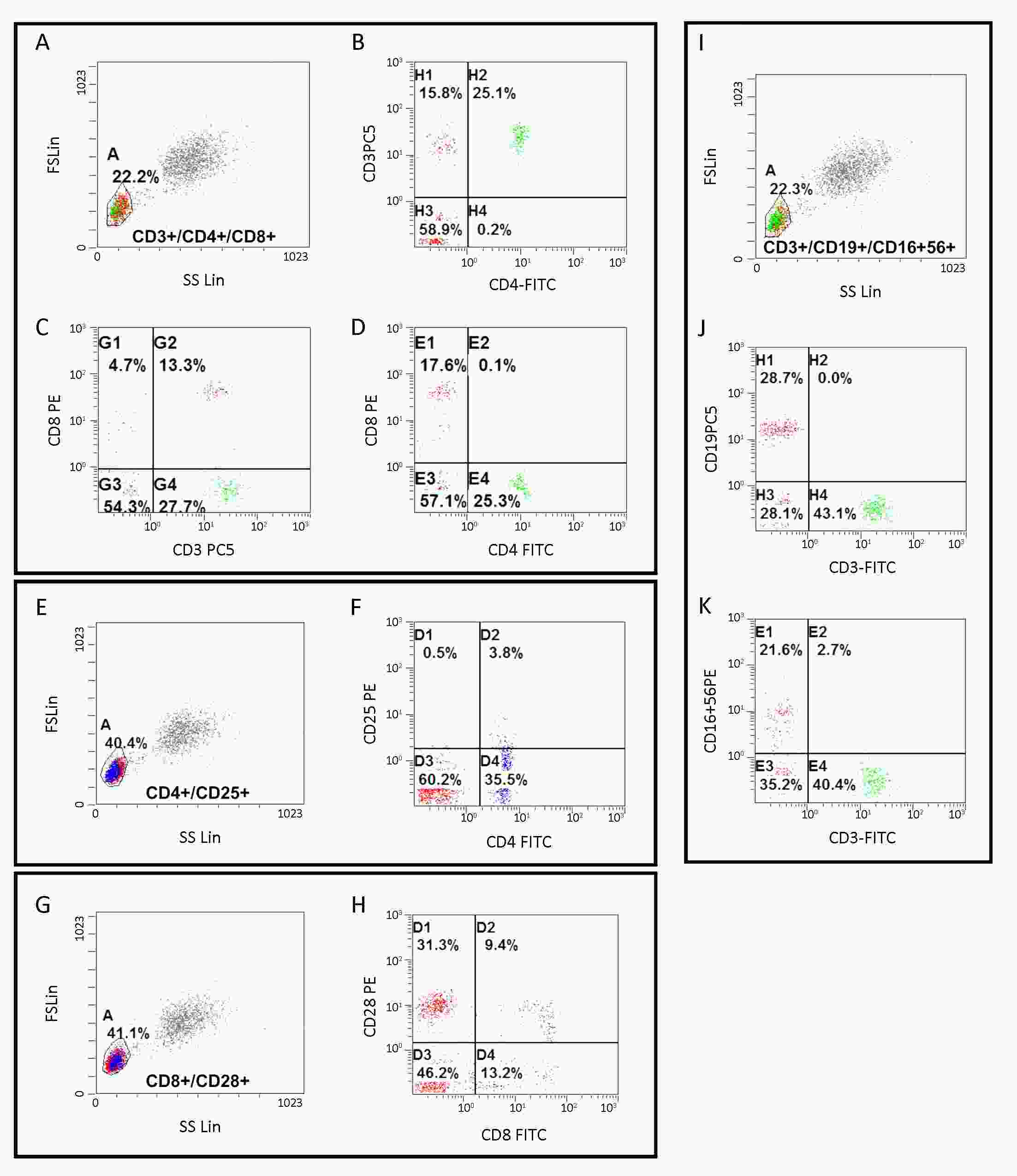
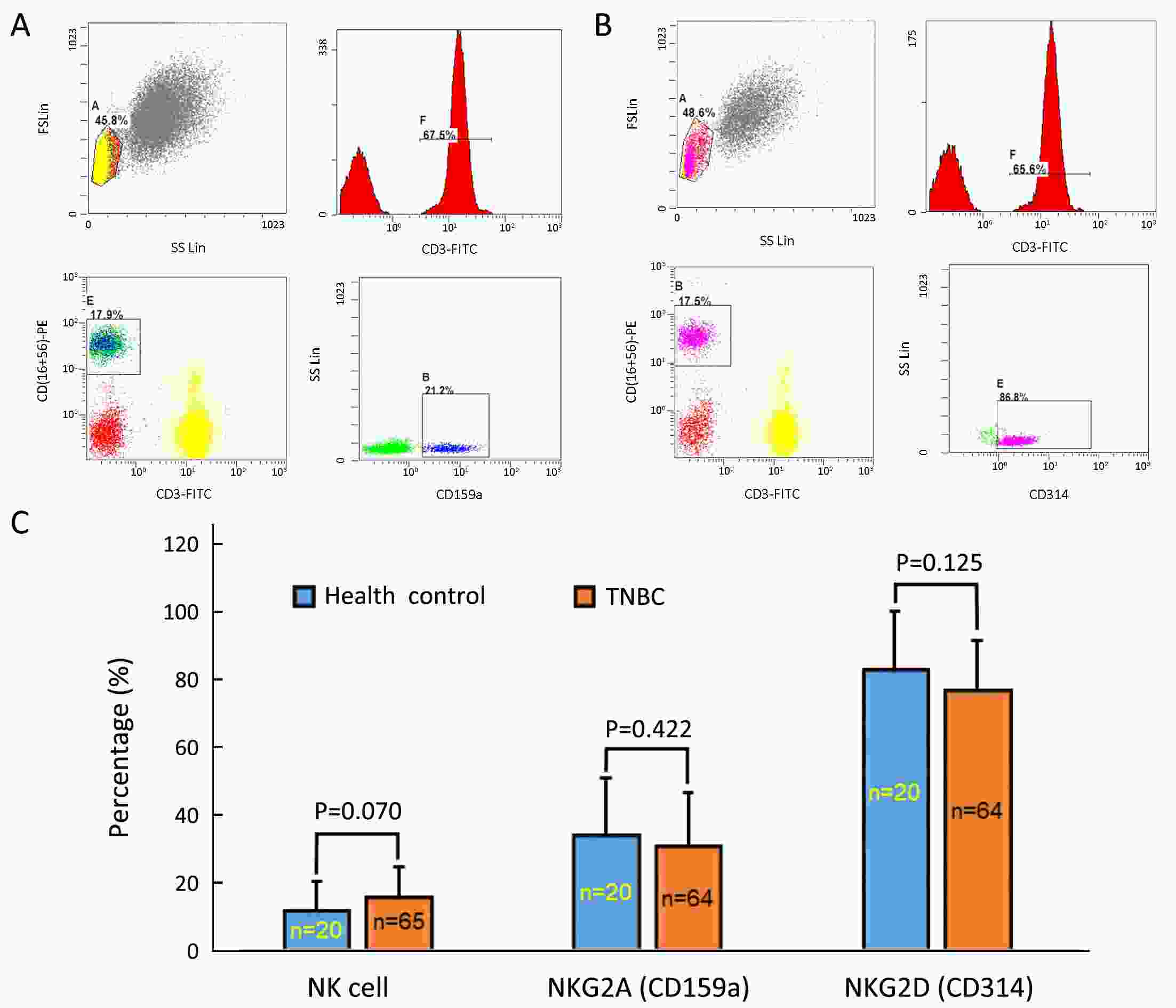
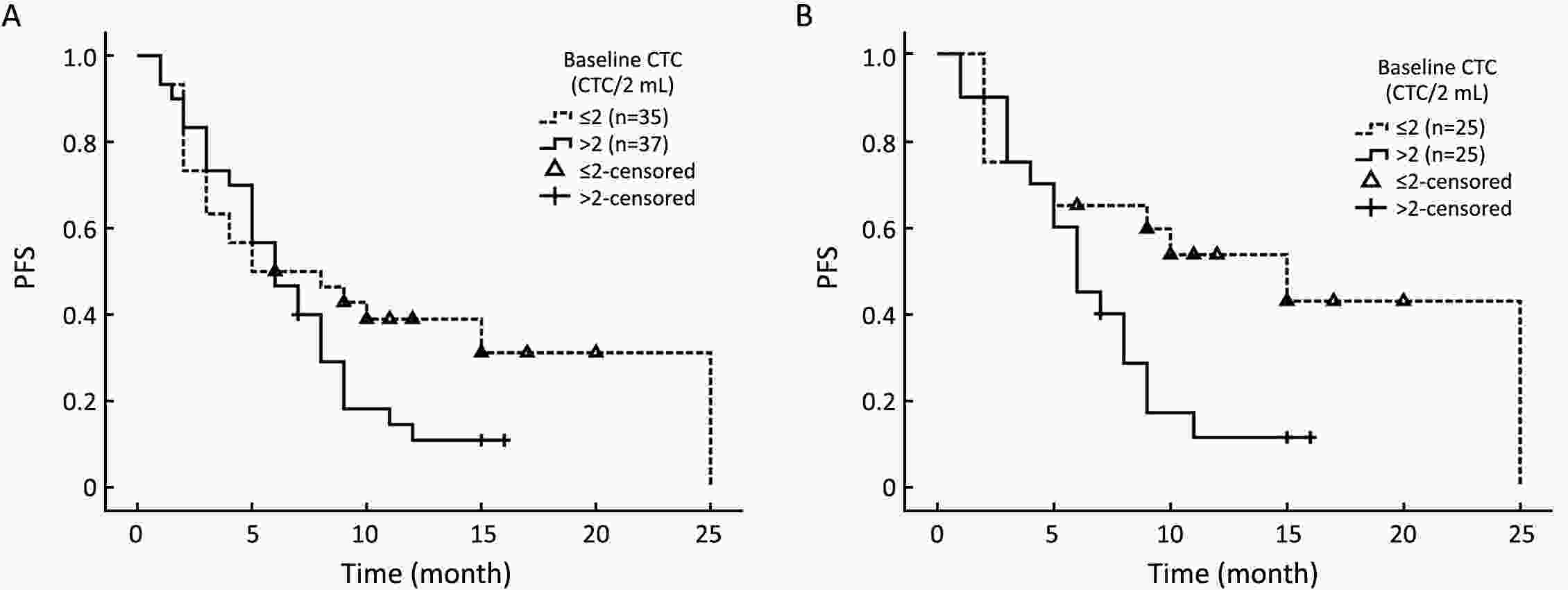
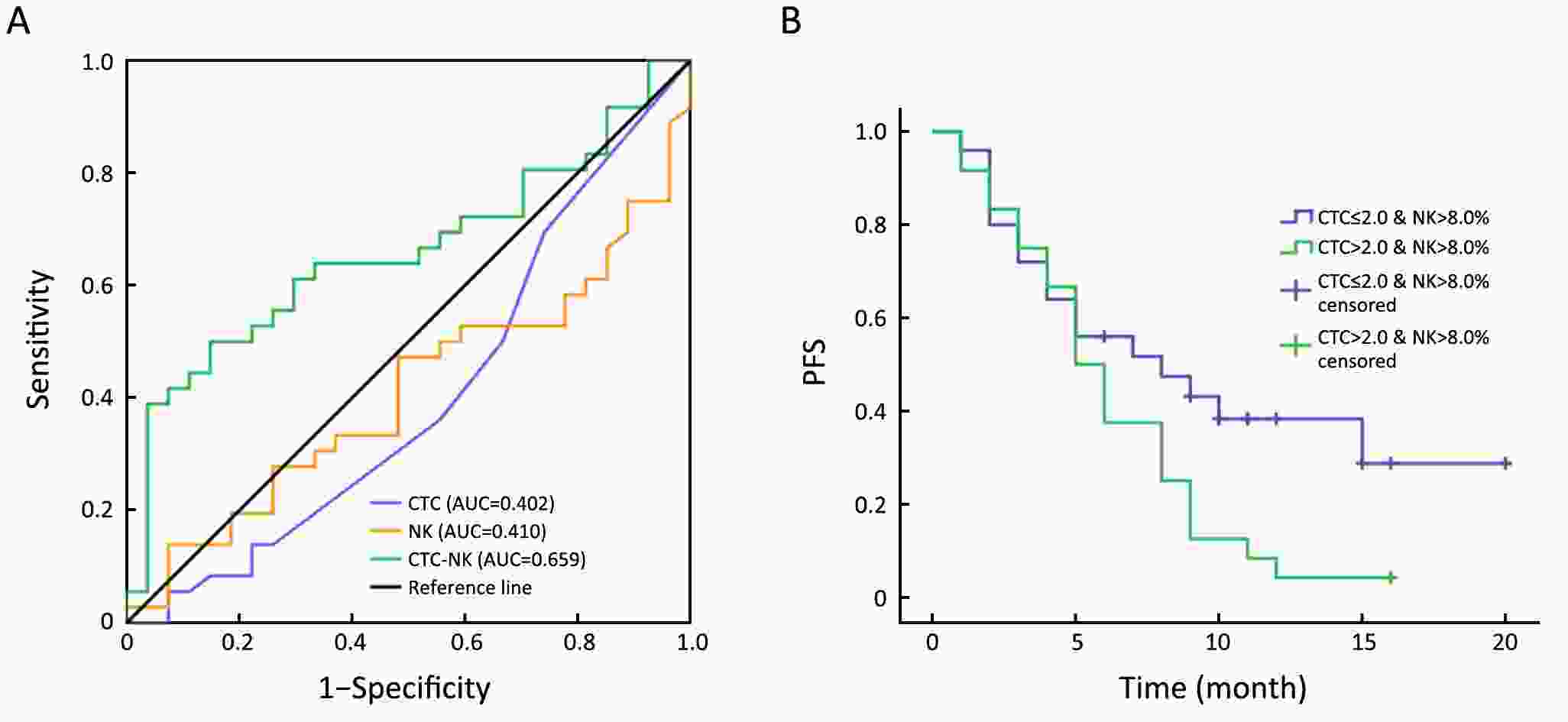
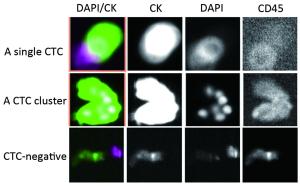
ObjectiveTriple-negative breast cancer (TNBC) is a heterogeneous disease with poor prognosis. Circulating tumor cells (CTCs) are a promising predictor for breast cancer prognoses but their reliability regarding progression-free survival (PFS) is controversial. We aim to verify their predictive value in TNBC. MethodsIn present prospective cohort study, we used the Pep@MNPs method to enumerate CTCs in baseline blood samples from 75 patients with TNBC (taken at inclusion in this study) and analyzed correlations between CTC numbers and outcomes and other clinical parameters. ResultsMedian PFS was 6.0 (range: 1.0–25.0) months for the entire cohort, in whom we found no correlations between baseline CTC status and initial tumor stage (P=0.167), tumor grade (P=0.783) or histological type (P=0.084). However, among those getting first-line treatment, baseline CTC status was positively correlated with ratio of peripheral natural killer (NK) cells (P=0.032), presence of lung metastasis (P=0.034) and number of visceral metastatic site (P=0.037). Baseline CTC status was predictive for PFS in first-line TNBC (P=0.033), but not for the cohort as a whole (P=0.118). This prognostic limitation of CTC could be ameliorated by combining CTC and NK cell enumeration (P=0.049). ConclusionsBaseline CTC status was predictive of lung metastasis, peripheral NK cell ratio and PFS in TNBC patients undergoing first-line treatment. We have developed a combined CTC-NK enumeration strategy that allows us to predict PFS in TNBC without any preconditions.
2018, 30(3): 327-339.
doi: 10.21147/j.issn.1000-9604.2018.03.05
Abstract:
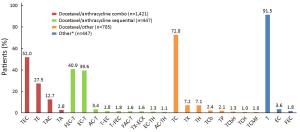
Objective Adjuvant docetaxel-based chemotherapy is frequently used for operable early breast cancer (EBC). This study investigated patterns of use of docetaxel (T) in real-life clinical practice in China. Methods This was a retrospective pooled analysis of the Asia-Pacific Breast Initiatives (APBI) I (2006–2008) and II (2009–2011) registries, and two Chinese observational studies; BC STATE (2011–2014) and BC Local Registry (2007–2010). Female Chinese adults (≥18 years) with operable breast cancer treated with docetaxel-based adjuvant chemotherapy were included in the analysis. Patients with metastatic disease were excluded. The primary endpoint was assessment of treatment patterns and patient profiles. A logistic regression analysis was conducted to identify factors associated with choice of adjuvant chemotherapy regimen. Results Data from 3,020 patients were included. The most frequently used adjuvant regimen was docetaxel/anthracycline combination [n=1,421 (47.1%); of whom 52.0% received T/epirubicin (E)/cyclophosphamide (C)], followed by docetaxel/other [n=705 (23.3%); of whom 72.8% received TC], docetaxel/anthracycline sequential [n=447 (14.8%); of whom 40.9% and 39.6% received 5-Fu/EC-T and EC-T, respectively], and " other” [n=447 (14.8%); of whom 91.5% received T]. A significant association was found between adjuvant therapy with docetaxel/anthracycline combination and patient weight, menopausal status and estrogen receptor status. Conclusions Real-world data revealed that docetaxel/anthracycline combination is the most commonly used category of docetaxel-based adjuvant therapy for patients with operable breast cancer in China; of which TEC is the most frequently used regimen.
2018, 30(3): 340-350.
doi: 10.21147/j.issn.1000-9604.2018.03.06
Abstract:
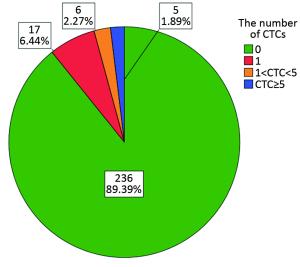
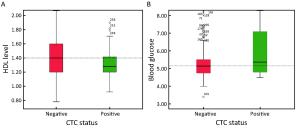
Objective Although circulating tumor cells (CTCs) have been well-established as promising prognostic biomarkers in both early breast cancer and metastatic settings, little is known regarding the prognostic relevance of CTCs in the long-term postoperative monitoring of patients with non-metastatic breast cancer (non-MBC). In this study, we investigated the associations of CTCs with clinicopathological features and metabolic-related variables, such as obesity and hyperglycemia. Methods In this retrospective study, we recruited 264 patients with postoperative stage I–III breast cancer at Guangdong General Hospital from January 2009 to December 2015. The prevalence and number of CTCs were assessed using the CellSearch System at a median time of 19.0 months [interquartile range (IQR), 7.8–33.0] after surgery. The CTC assay results were correlated with the clinicopathological features and metabolic-related variables. A multivariate logistic regression analysis was performed to further determine the independent predictors of CTCs. Results CTCs were detected in 10.6% of all patients. The positive rate of CTCs in patients with infiltrating ductal carcinoma was lower than that in patients with other pathological types (9.0% vs. 28.6%, P=0.020). More importantly, the presence of CTCs was correlated with blood glucose level (P=0.015) and high-density lipoprotein level (P=0.030). The multivariate logistic regression analysis showed that the pathological type [odds ratio (OR): 1.757, 95% CI: 1.021–3.023; P=0.042] and blood glucose level (OR: 1.218, 95% CI: 1.014–1.465; P=0.035) were independent predictors of the presence of CTCs. Conclusions This study revealed potential associations between CTCs and metabolic-related factors in Chinese patients with non-MBC and supports the hypothesis that metabolic dysfunction in breast cancer patients might influence the biological activity of metastatic breast cancer, leading to a higher prevalence of CTCs.
2018, 30(3): 351-363.
doi: 10.21147/j.issn.1000-9604.2018.03.07
Abstract:
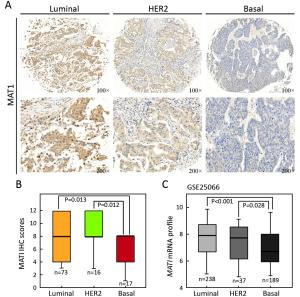
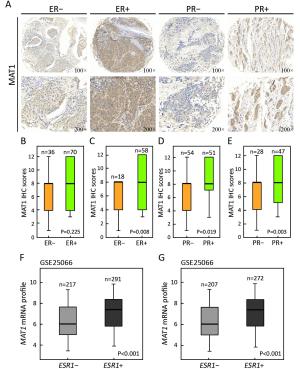
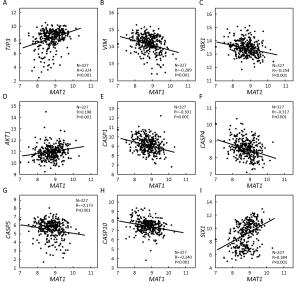
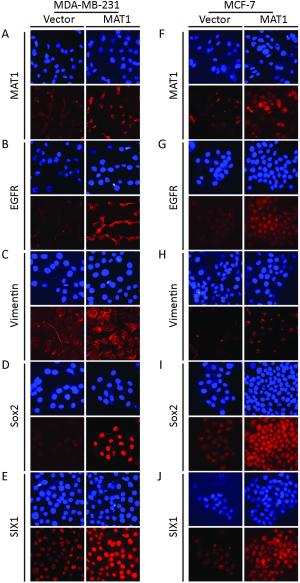
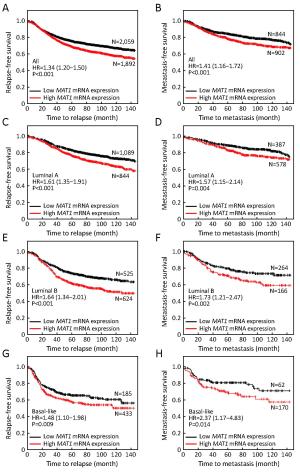
Objective Menage a trois 1 (MAT1) is a targeting subunit of cyclin-dependent kinase-activating kinase and general transcription factor IIH kinase, which modulates cell cycle, transcription and DNA repair. Its dysregulation is responsible for diseases including cancers. To further explore the role of MAT1 in breast cancer, we investigated the pathways in which MAT1 might be involved, the association between MAT1 and molecular subtypes, and the role of MAT1 in clinical outcomes of breast cancer patients. Methods We conducted immunohistochemistry staining on tissue microarray and immunofluorescence staining on sections of MAT1 stable breast cancer cells. Also, we performed Kyoto Encyclopedia of Genes and Genomes pathway analysis, correlation analysis and prognosis analysis on public databases. Results MAT1 was involved in multiple pathways including normal physiology signaling and disease-related signaling. Furthermore, MAT1 positively correlated with the protein status of estrogen receptor and progesterone receptor, and was enriched in luminal-type and human epidermal growth factor receptor 2-enriched breast cancer in comparison with basal-like subtype at both mRNA and protein levels. Correlation analysis revealed significant association between MAT1 mRNA amount and epithelial markers, mesenchymal markers, cancer stem cell markers, apoptosis markers, transcription markers and oncogenes. Consistently, the results of immunofluorescence stain indicated that MAT1 overexpression enhanced the protein abundance of epidermal growth factor receptor, vimentin, sex determining region Y-box 2 and sine oculis homeobox homolog 1. Importantly, Kaplan-Meier Plotter analysis reflected that MAT1 could serve as a prognostic biomarker predicting worse relapse-free survival and metastasis-free survival. Conclusions MAT1 is correlated with molecular subtypes and is associated with unfavorable prognosis for breast cancer patients.
2018, 30(3): 364-372.
doi: 10.21147/j.issn.1000-9604.2018.03.08
Abstract:
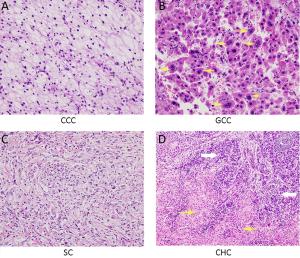
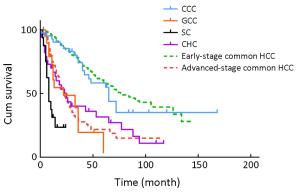
Objective This study aimed to analyze clinicopathological and prognostic features of four rare pathological subtypes of primary liver malignancies to make better understanding of their clinical features. Methods The clinicopathological data of 114 patients who were diagnosed with histologically proven four subtypes: clear cell carcinoma (CCC), giant cell carcinoma (GCC), sarcomatoid carcinoma (SC), and combined hepatocellular-cholangiocarcinoma (CHC) between October 1998 and August 2015 were reviewed. Their survival data were compared with those of 908 patients with histologically proven common hepatocellular carcinoma (HCC) (early- and advanced-stage HCC) during the same period. Results The outcome of the CCC group was better than that of the other three subgroups, and was similar to that of the early-stage HCC group. Also, the smallest tumor size and the highest incidence of pseudocapsule formation were observed in the CCC group. The SC group had the worst outcome among these four subgroups; the prognosis was much poorer than that of any other subgroups, even poorer than that of the advanced-stage common HCC group. No statistical difference was observed between the GCC, CHC and advanced-stage HCC groups on survival analysis. The incidences of tumor vascular emboli, TNM staging and non-radical resection were three risk factors of the prognosis. Conclusions CCC is a low-degree malignancy and relatively favorably prognostic subtype of HCC. However, GCC, SC, and CHC are three rare high-degree malignancy subtypes of HCC with poor prognosis.
2018, 30(3): 373-381.
doi: 10.21147/j.issn.1000-9604.2018.03.09
Abstract:
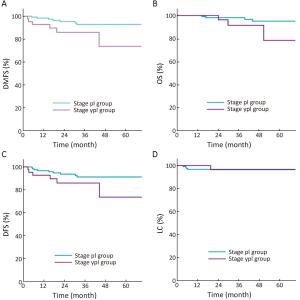
Objective Prognosis of patients with locally advanced rectal cancer (LARC) but achieving ypT1–2N0 stage after neoadjuvant concurrent chemo-radiotherapy (CRT) has been shown to be favorable. This study aims to determine whether the long-term outcome of ypT1–2N0 cases can be comparable to that of pT1–2N0 cohort that received definitive surgery for early disease. Method From January 2008 to December 2013, 449 consecutive patients with rectal cancer were treated and their outcome maintained in a database. Patients with LARC underwent total mesorectal excision (TME) surgery at 4–8 weeks after completion of CRT, and those achieving stage ypI were identified as a group. As a comparison, stage pI group pertains to patients whose initially limited disease was not upstaged after TME surgery alone. After propensity score matching (PSM), comparisons of local regional control (LC), distant metastasis-free survival (DMFS), disease-free survival (DFS) and overall survival (OS) were performed using Kaplan-Meier analysis and log-rank test between ypI and pI groups. Down-staging depth score (DDS), a novel method of evaluating CRT response, was used for subset analysis. Results Of the 449 patients, 168 matched cases were generated for analysis. Five-year LC, DMFS, DFS and OS for stage pI vs. ypI groups were 96.7% vs. 96.4% (P=0.796), 92.7% vs. 73.6% (P=0.025), 91.2% vs. 73.6% (P=0.080) and 93.1% vs. 72.3% (P=0.040), respectively. In the DDS-favorable subset of the ypI group, LC, DMFS, DFS and OS resulted in no significant differences in comparison with the pI group (P=0.384, 0.368, 0.277 and 0.458, respectively). Conclusions LC was comparable in both groups; however, distant metastasis developed more frequently in down-staged LARC than de novo early stage cases, reflecting the need to improve the efficacy of systemic treatment despite excellent pathologic response. DDS can be an indicator to identify a subset of the ypI group whose long-term oncologic outcomes are as good as those of stage pI cohort.
2018, 30(3): 382-394.
doi: 10.21147/j.issn.1000-9604.2018.03.10
Abstract:
Sorafenib, which is a novel targeted agent, plays an important role in treating advanced hepatocellular carcinoma (HCC) through its antiangiogenic and antiproliferative effects. However, conventional morphology-based radiographic evaluation systems may underestimate the efficacy of sorafenib in HCC due to a lack of apparent tumor shrinkage or altered tumor morphology in many cases. This calls for the development of more accurate imaging methods for evaluating sorafenib. The introduction of tumor burden measurements based on viability and other evolving imaging approaches for assessing therapeutic effects are promising for overcoming some of the limitations of the morphology-based criteria. In this review, we summarize various imaging methods that are used to assess treatment responses of advanced HCC to sorafenib. Imaging markers predictive of prognosis in advanced HCC after treatment with sorafenib are also included and discussed.
Sorafenib, which is a novel targeted agent, plays an important role in treating advanced hepatocellular carcinoma (HCC) through its antiangiogenic and antiproliferative effects. However, conventional morphology-based radiographic evaluation systems may underestimate the efficacy of sorafenib in HCC due to a lack of apparent tumor shrinkage or altered tumor morphology in many cases. This calls for the development of more accurate imaging methods for evaluating sorafenib. The introduction of tumor burden measurements based on viability and other evolving imaging approaches for assessing therapeutic effects are promising for overcoming some of the limitations of the morphology-based criteria. In this review, we summarize various imaging methods that are used to assess treatment responses of advanced HCC to sorafenib. Imaging markers predictive of prognosis in advanced HCC after treatment with sorafenib are also included and discussed.

 Abstract
Abstract FullText HTML
FullText HTML PDF 379KB
PDF 379KB