2018 Vol.30(6)
Display Mode: |
2018, 30(6): 571-587.
doi: 10.21147/j.issn.1000-9604.2018.06.01
Abstract:
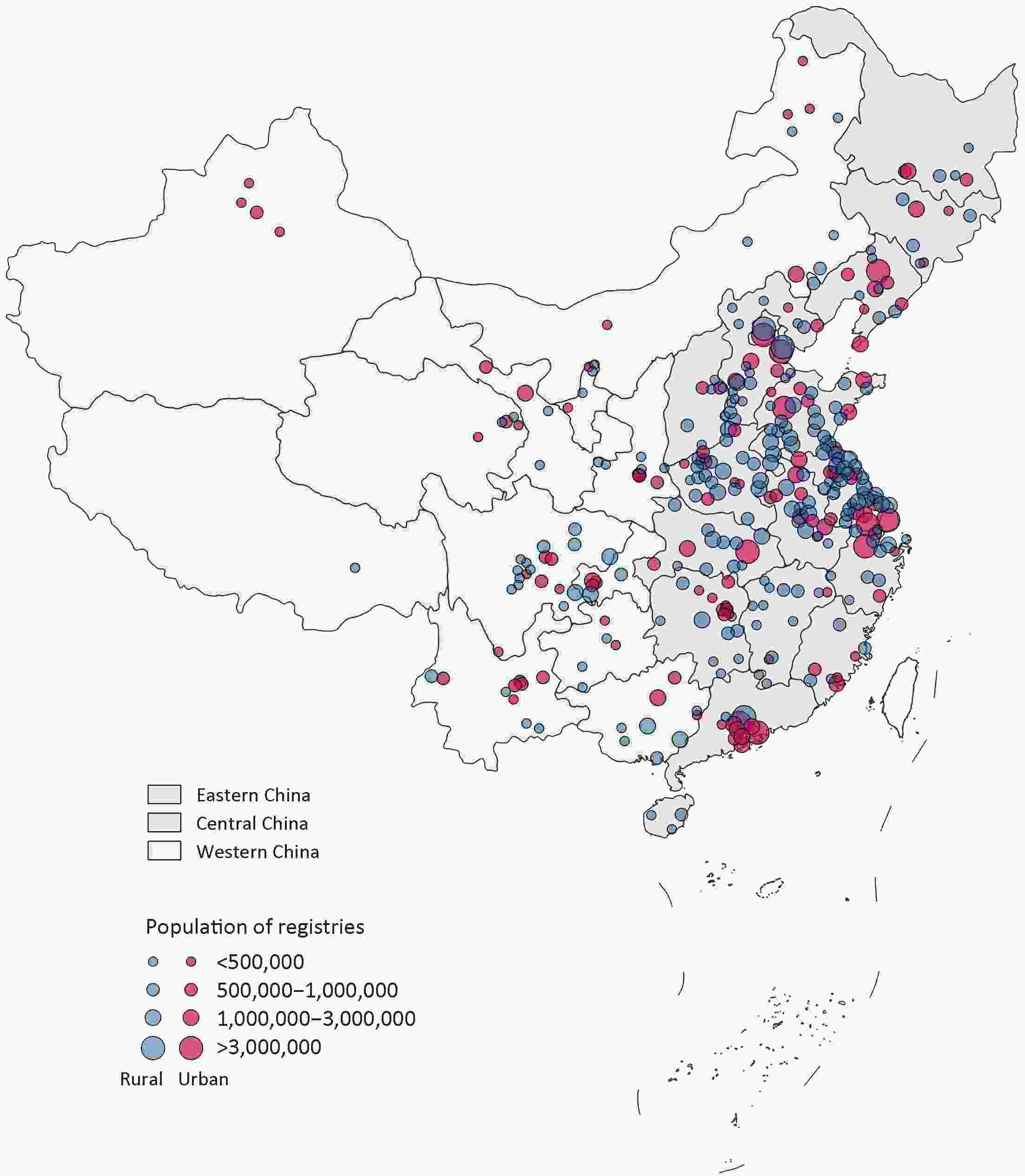
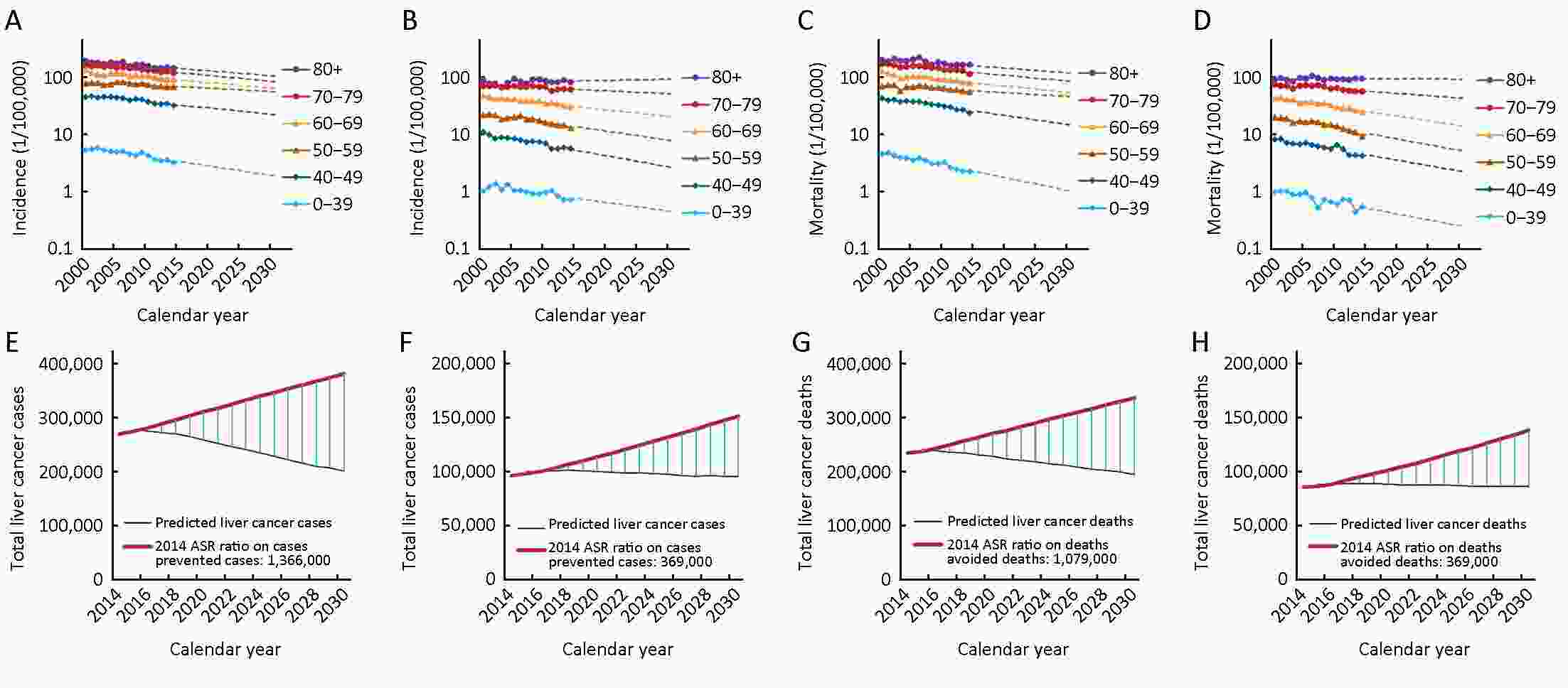
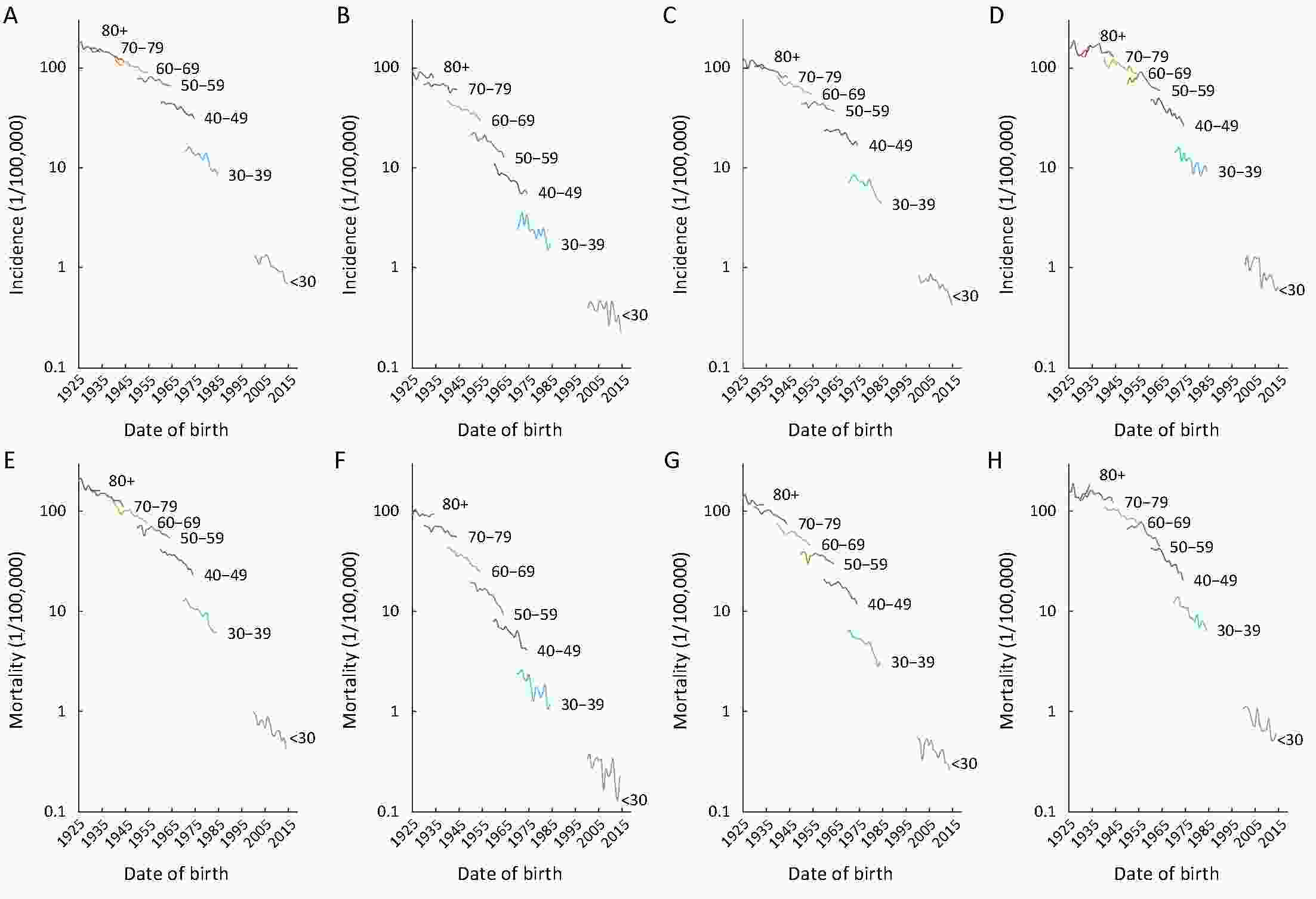
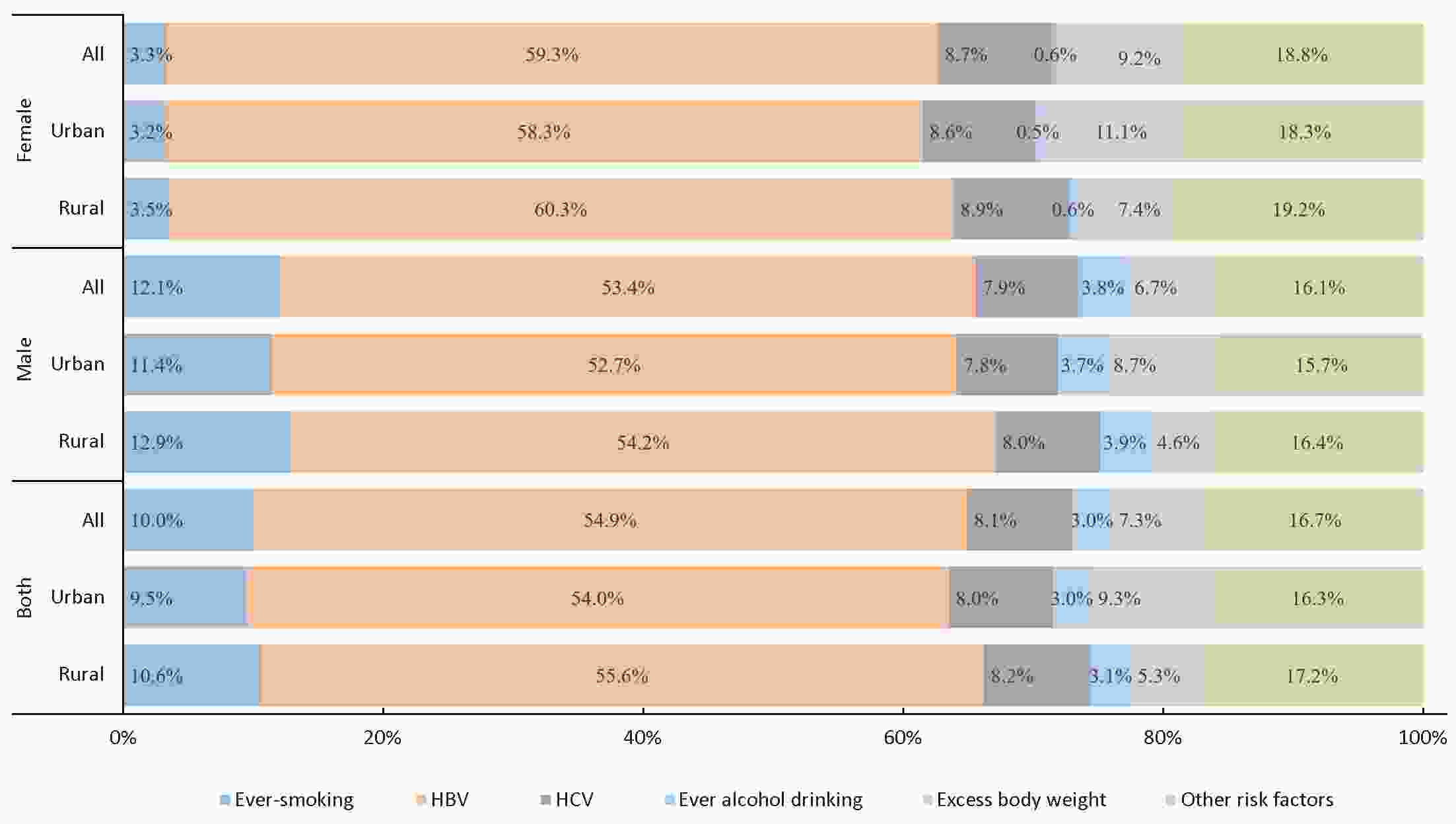
ObjectiveLiver cancer is one of the most common cancers and major cause of cancer deaths in China, which accounts for over 50% of new cases and deaths worldwide. The systematic liver cancer statistics including of projection through 2030 could provide valuable information for prevention and control strategies in China, and experience for other countries. MethodsThe burden of liver cancer in China in 2014 was estimated using 339 cancer registries’ data selected from Chinese National Cancer Center (NCC). Incident cases of 22 cancer registries were applied for temporal trends from 2000 to 2014. The burden of liver cancer through 2030 was projected using age-period-cohort model. ResultsAbout 364,800 new cases of liver cancer (268,900 males and 95,900 females) occurred in China, and about 318,800 liver cancer deaths (233,500 males and 85,300 females) in 2014. Western regions of China had the highest incidence and mortality rates. Incidence and mortality rates decreased by about 2.3% and 2.6% per year during the period of 2000−2014, respectively, and would decrease by more than 44% between 2014 and 2030 in China. The young generation, particularly for those aged under 40 years, showed a faster down trend. ConclusionsBased on the analysis, incidence and mortality rates of liver cancer are expected to decrease through 2030, but the burden of liver cancer is still serious in China, especially in rural and western areas. Most cases of liver cancer in China can be prevented through vaccination and more prevention efforts should be focused on high risk groups.
2018, 30(6): 580-587.
doi: 10.21147/j.issn.1000-9604.2018.06.02
Abstract:
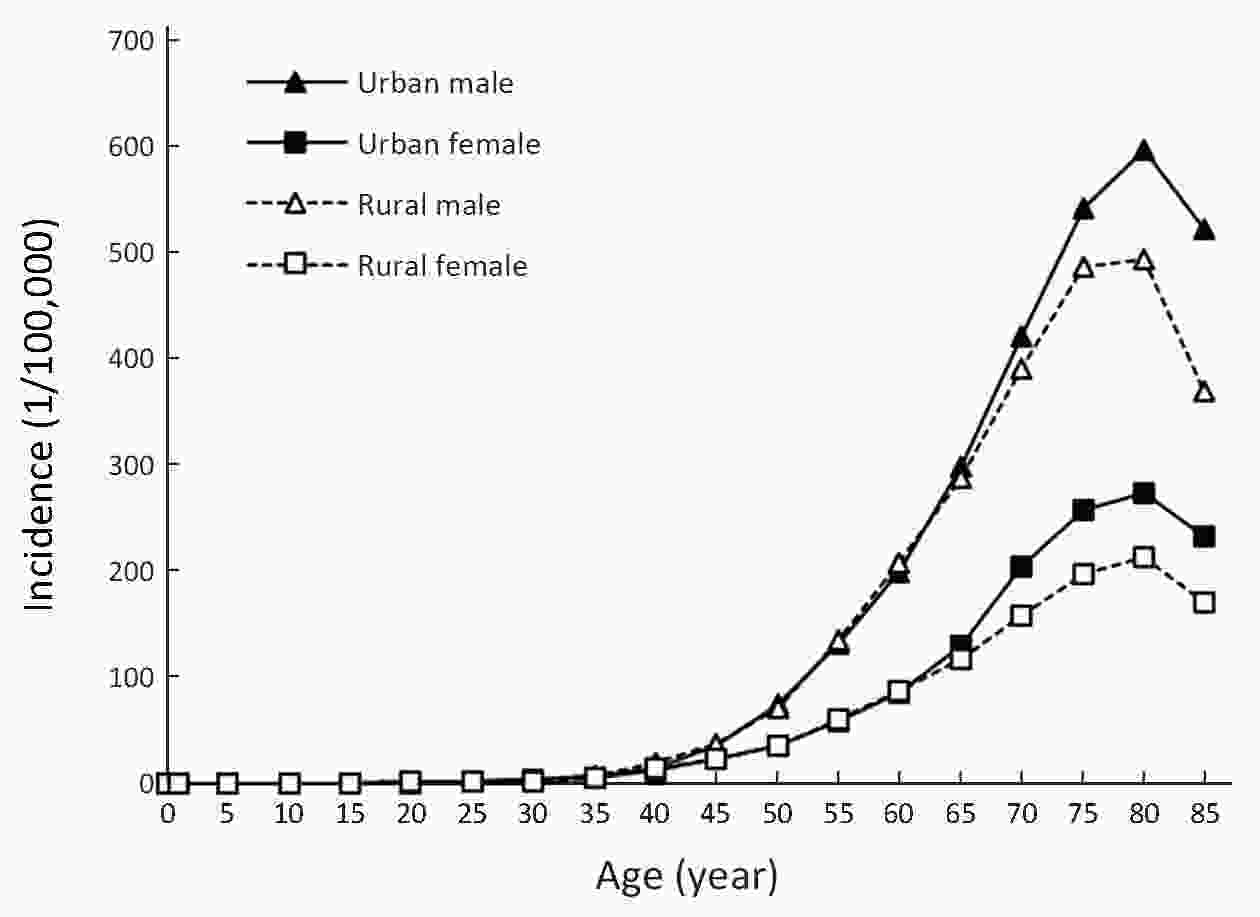
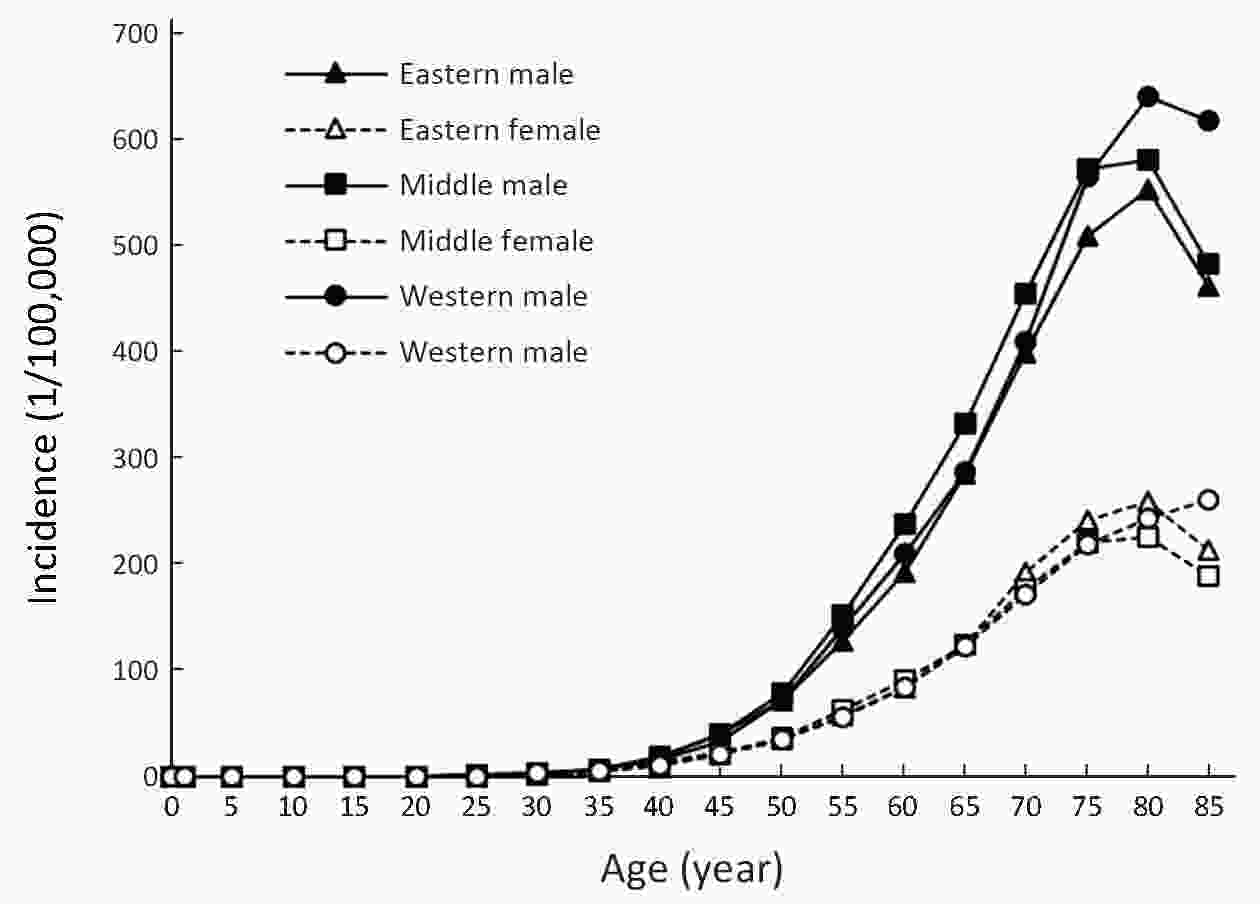
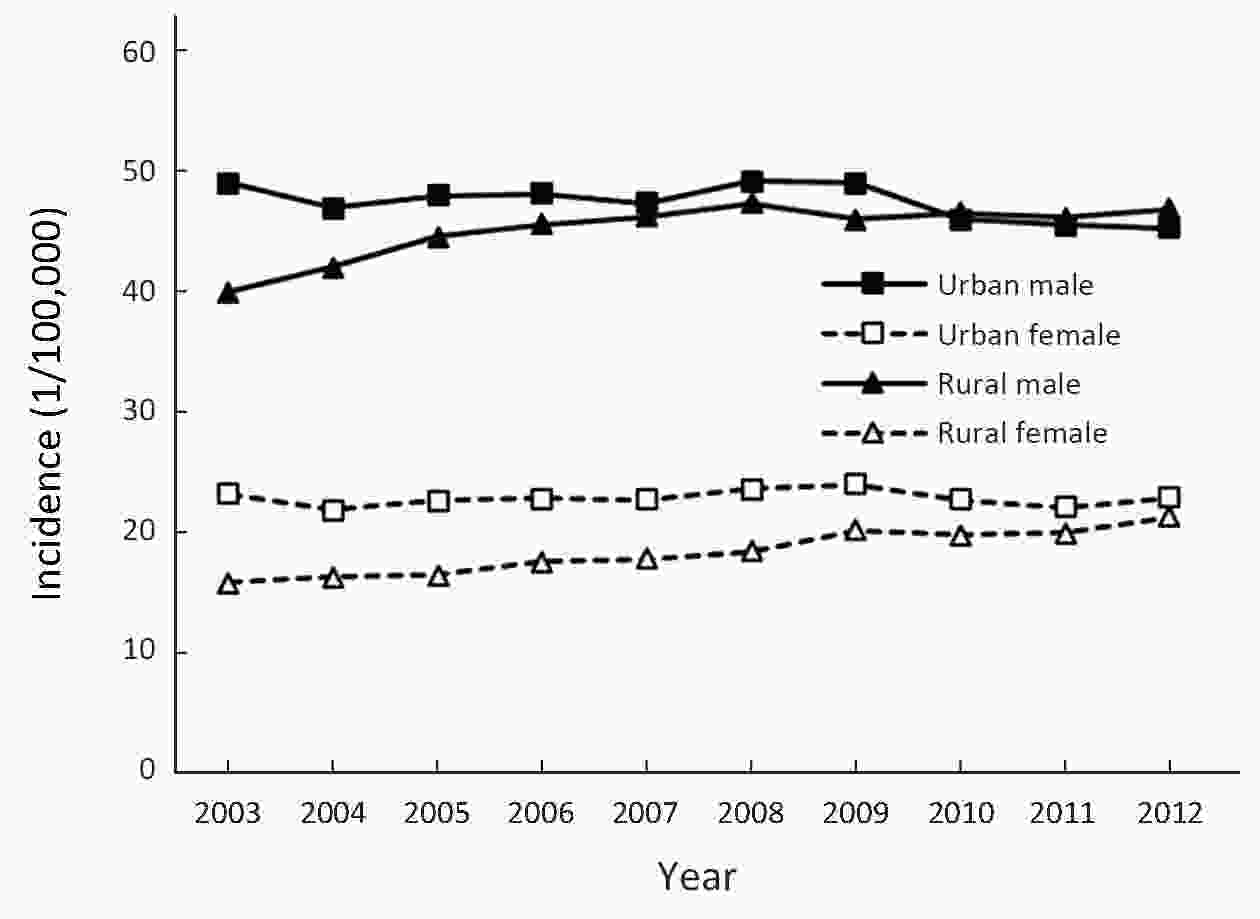
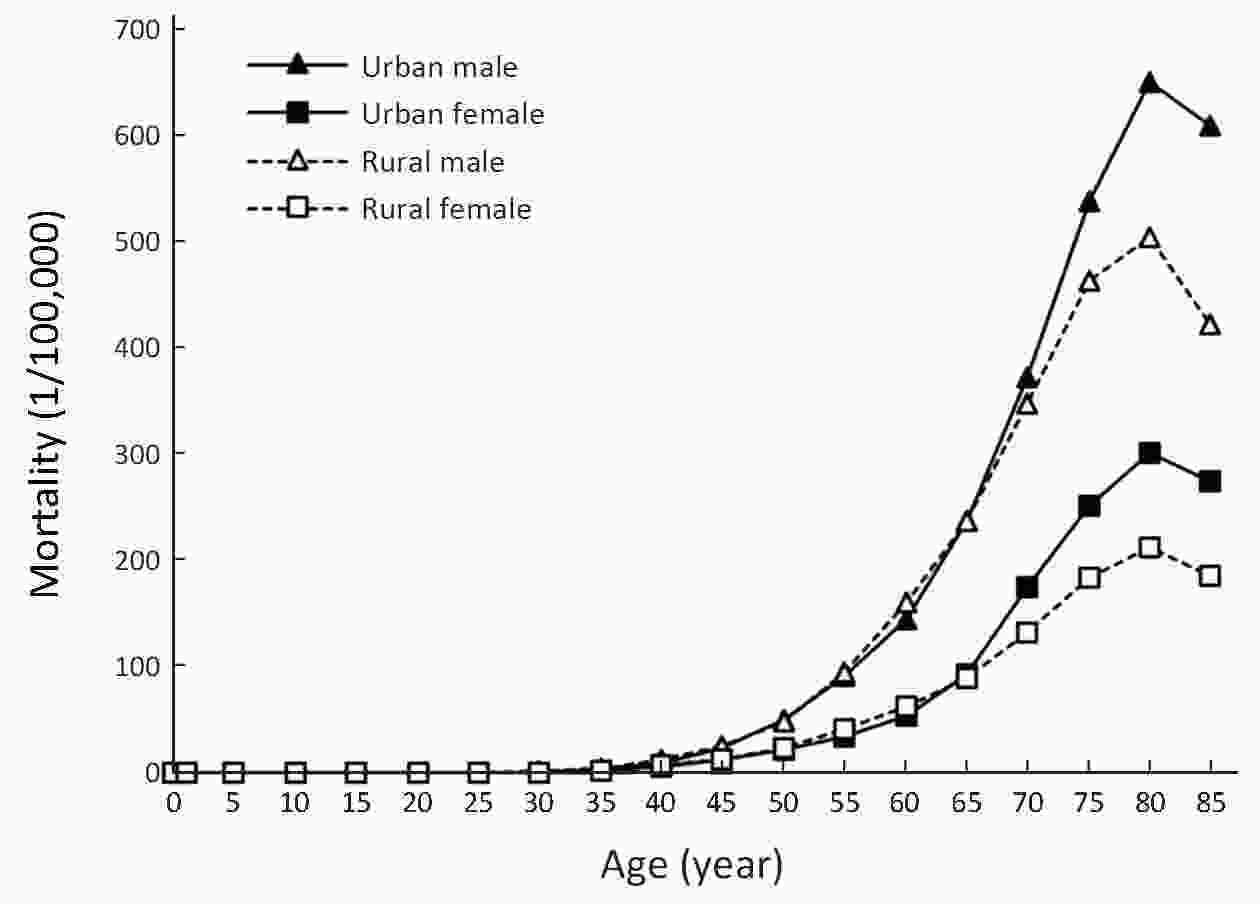
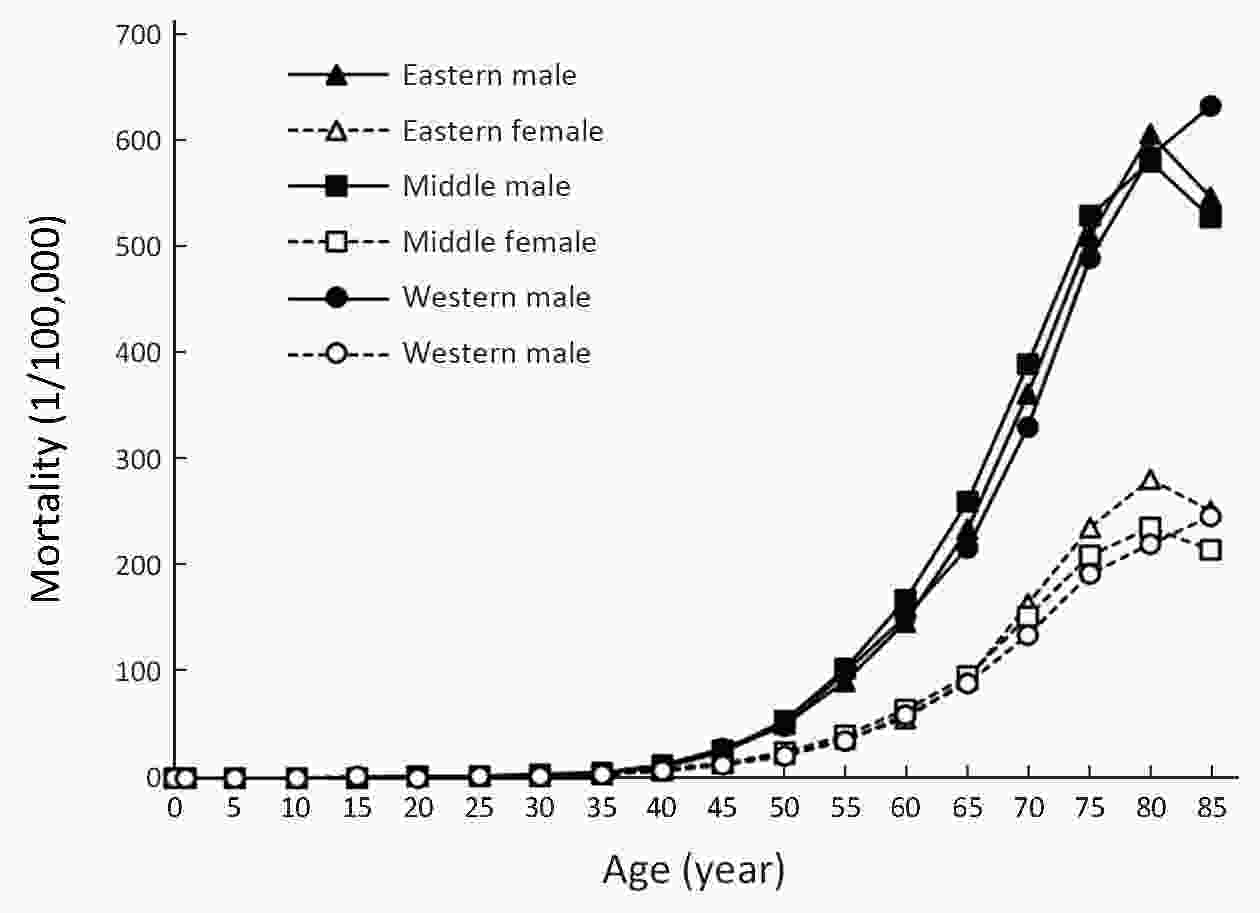
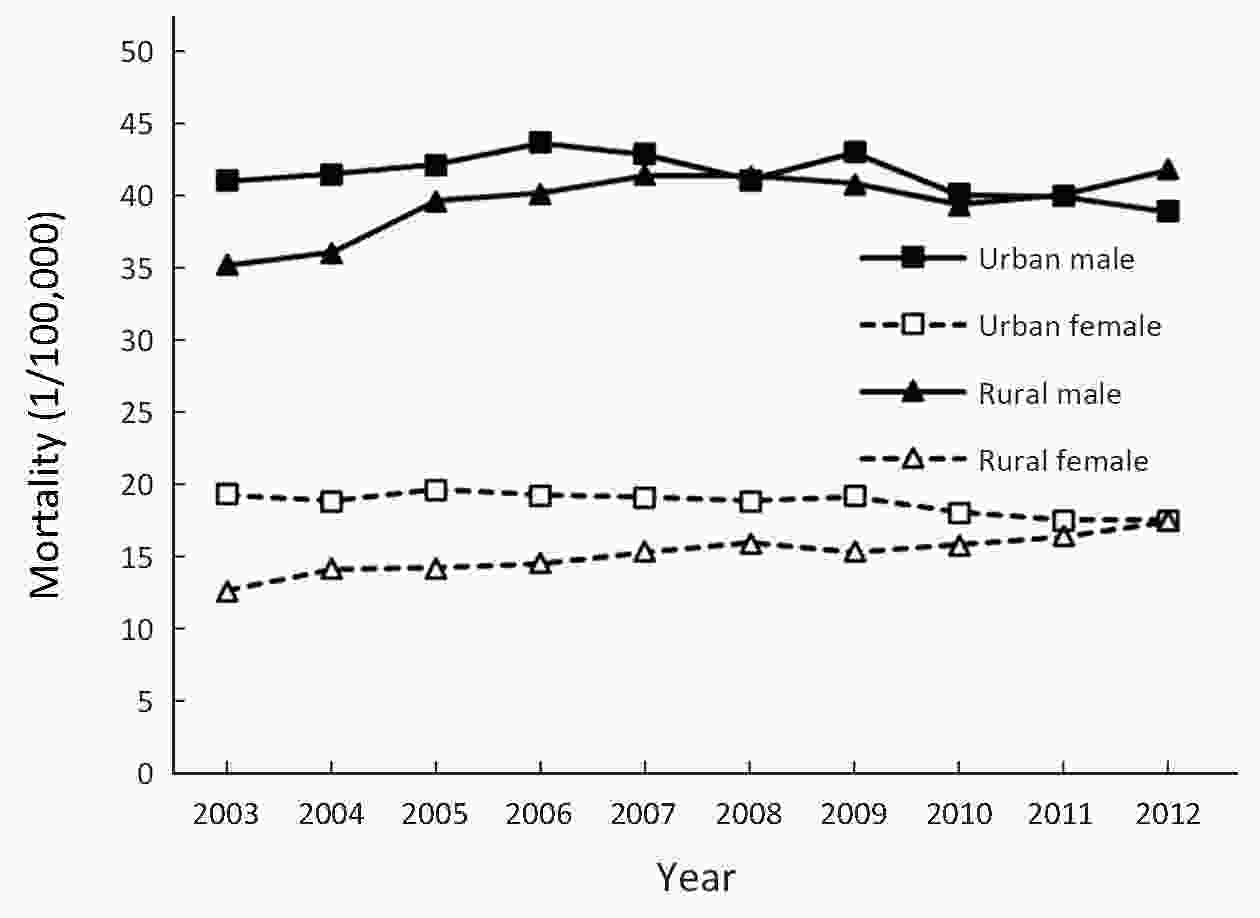
ObjectiveTo analyze the incidence and mortality rates of lung cancer in China from 2008 to 2012. MethodsIncident and death cases of lung cancer were retrieved from the National Central Cancer Registry (NCCR) database collecting from 135 cancer registries in China during 2008−2012. The crude incidence and mortality rates of lung cancer were calculated by area (urban/rural), region (eastern, middle, western), gender and age group (0, 1−4, 5−9, …, 85+). China census in 2000 and Segi’s world population were applied for age-standardized rates. JoinPoint (Version 4.5.0.1) model was used for time trend analysis. ResultsThe crude incidence rate of lung cancer was 54.66/100,000 which ranked the first in overall cancers. The age-standardized incidence rates by China population (ASIRC) and by World population (ASIRW) were 35.13/100,000 and 34.86/100,000, respectively. The crude mortality of lung cancer in China was 45.60/100,000 and it was the first cause of cancer-related death in overall cancers. The age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 28.57/100,000 and 28.22/100,000, respectively. Incidence and mortality rates of lung cancer were higher in males than in females and higher in urban areas than in rural areas. Eastern areas had the highest incidence and mortality rates followed by middle and western areas. Incidence and mortality rates of lung cancer retained low level in age groups before 40 years old but increased greatly after and peaked in age group of 80−84. During 2003−2012, the temporal trend of the incidence rate of lung cancer in both sexes in China was general stable (P<0.05). The lung cancer incidence rate increased by 0.71% per year in females (P<0.05) and 2.26% per year in rural areas (P<0.05). The mortality rate of lung cancer decreased slightly annually during 2003−2012 in China (P>0.05). In urban areas, it declined by 0.76% per year (P<0.05), but rose by 2.09% per year (P<0.05) in rural areas. ConclusionsAppropriate targeted prevention, early detection and treatment programs should be carried out to control the local burden of lung cancer.
2018, 30(6): 588-595.
doi: 10.21147/j.issn.1000-9604.2018.06.03
Abstract:
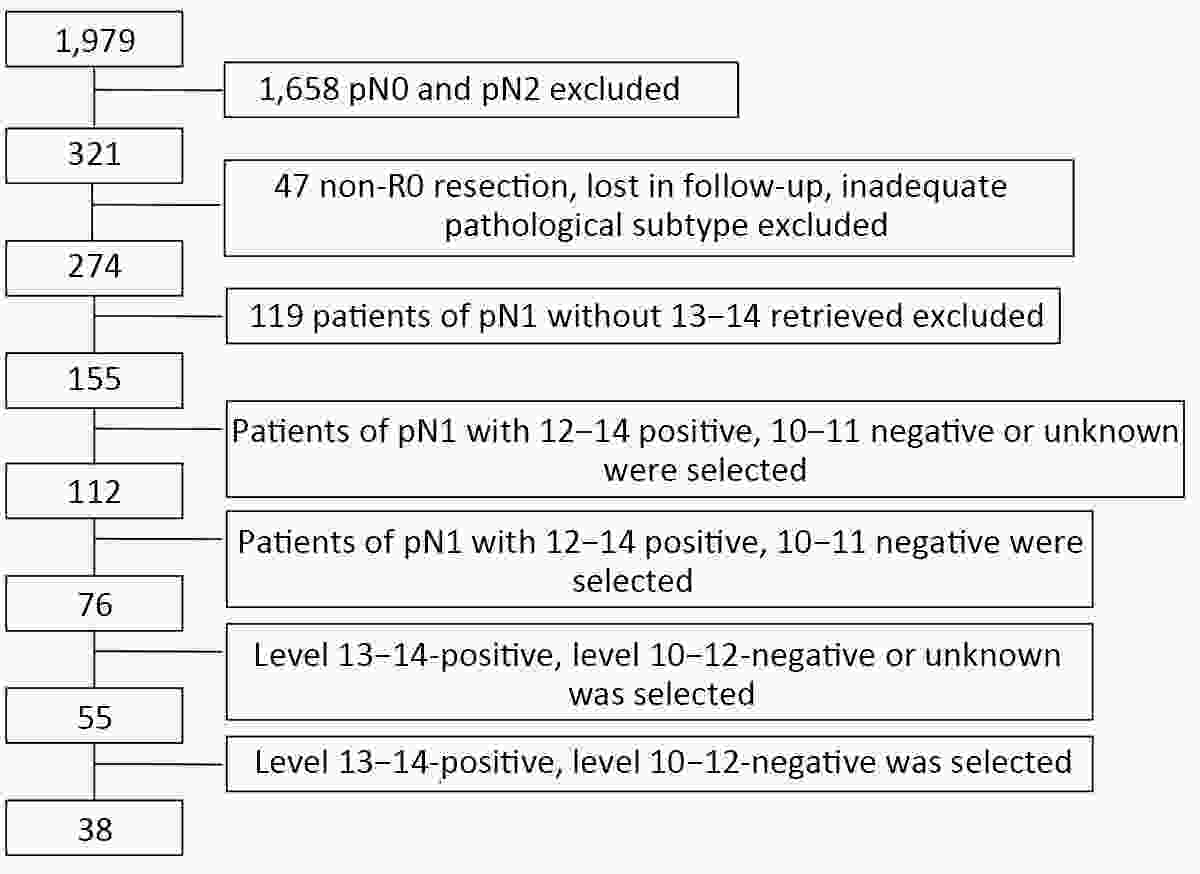
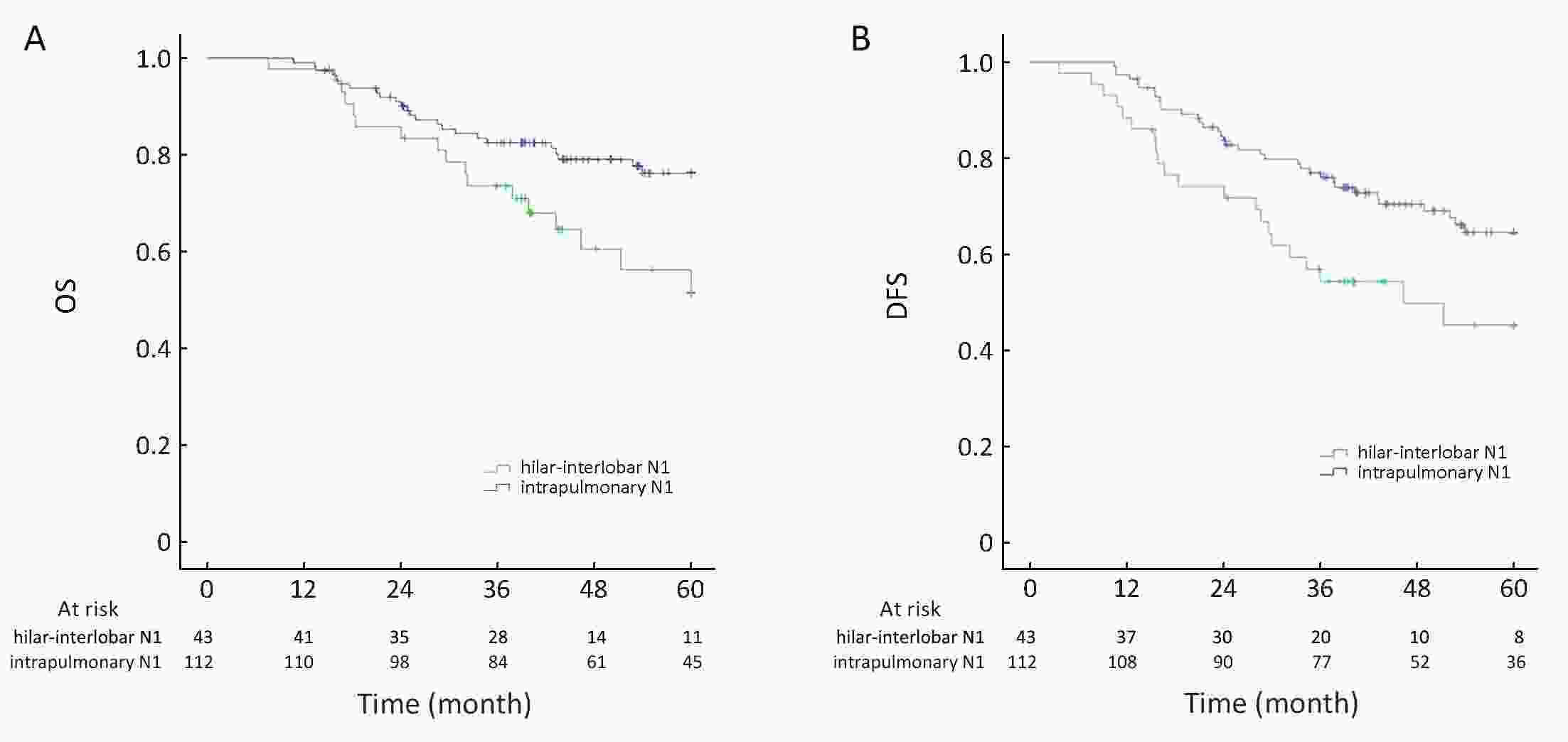
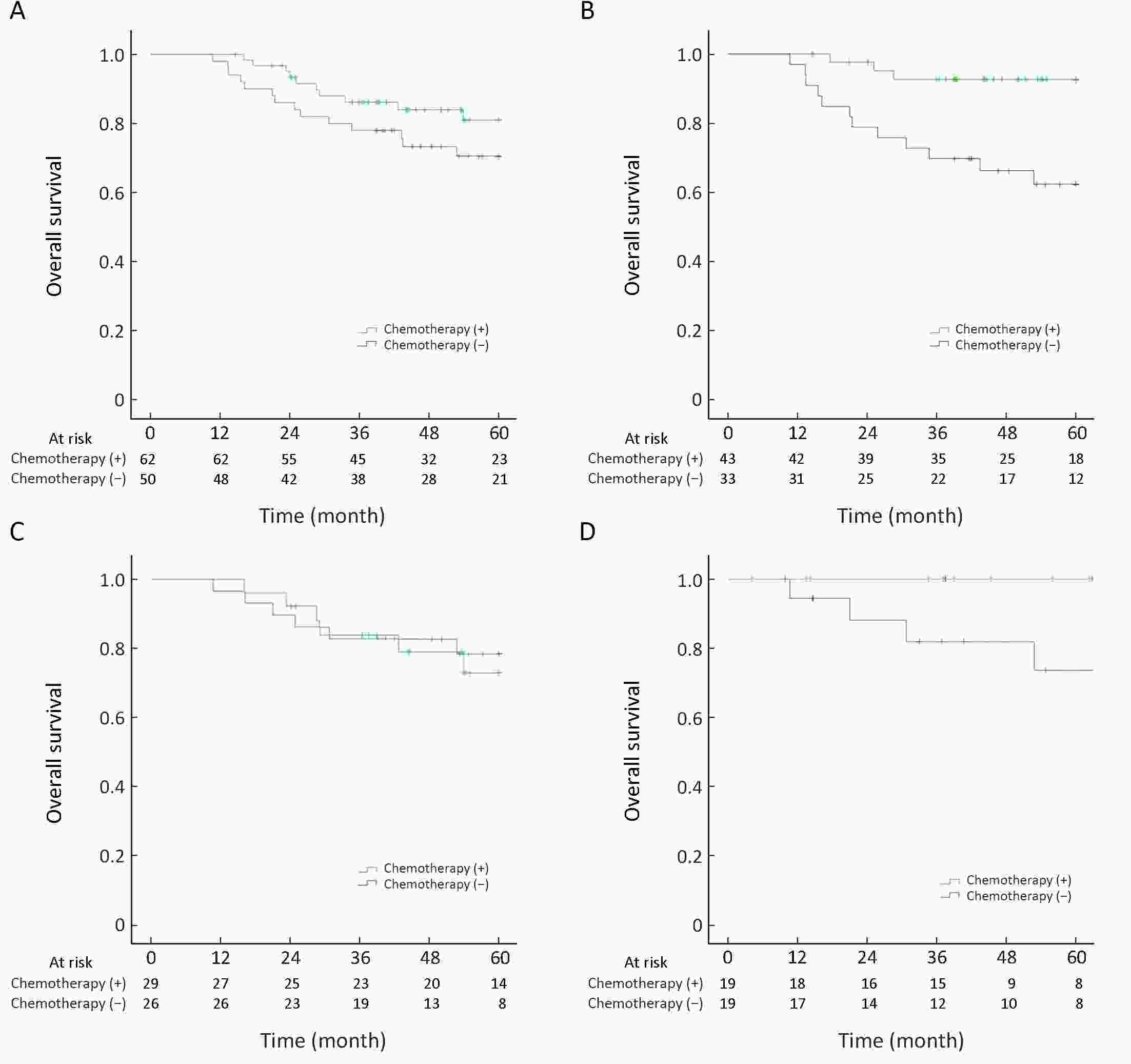
ObjectiveSurvival benefit of adjuvant chemotherapy (AC) of patients with intrapulmonary lymph node (IPLN) metastasis (level 12−14) needs investigation. We evaluated the impact of AC on patients whose metastatic nodes were limited to intrapulmonary levels after systematic dissection of N1 nodes. MethodsFirst, 155 consective cases of lung cancer confirmed as pathologic N1 were collected and evaluated. Patients received systematic dissection of N2 and N1 nodes. For patients with IPLN metastasis, survival outcomes were compared between those receiving AC and those not receiving AC. ResultsIn this group, 112 cases (72.3%) had IPLN metastasis and 55 cases (35.5%) had N1 involvement limited to level 13−14 without further disease spread to higher levels. Patients with IPLN involvement had a better prognosis than that of patients with hilar-interlobar involvement. For the intrapulmonary N1 group (level 12−14-positive, level 10−11-negative or unknown, n=112), no survival benefit was found between the AC group and non-AC group [5-year overall survival (OS): 54.6±1.6 vs. 50.4±2.4 months, P=0.177]. However, 76 of 112 cases for whom harvesting of level-10 and level-11 nodes was done did not show cancer involvement in pathology reports (level 12−14-positive, level 10−11 both negative), oncologic outcome was better for patients receiving AC than those not receiving AC in this subgroup (5-year OS: 57.3±1.5 vs. 47.1±3.2 months, P=0.002). ConclusionsOncologic outcome may be improved by AC for patients with involvement of N1 nodes limited to intrapulmonary levels after complete examination of N1 nodes.
2018, 30(6): 596-604.
doi: 10.21147/j.issn.1000-9604.2018.06.04
Abstract:
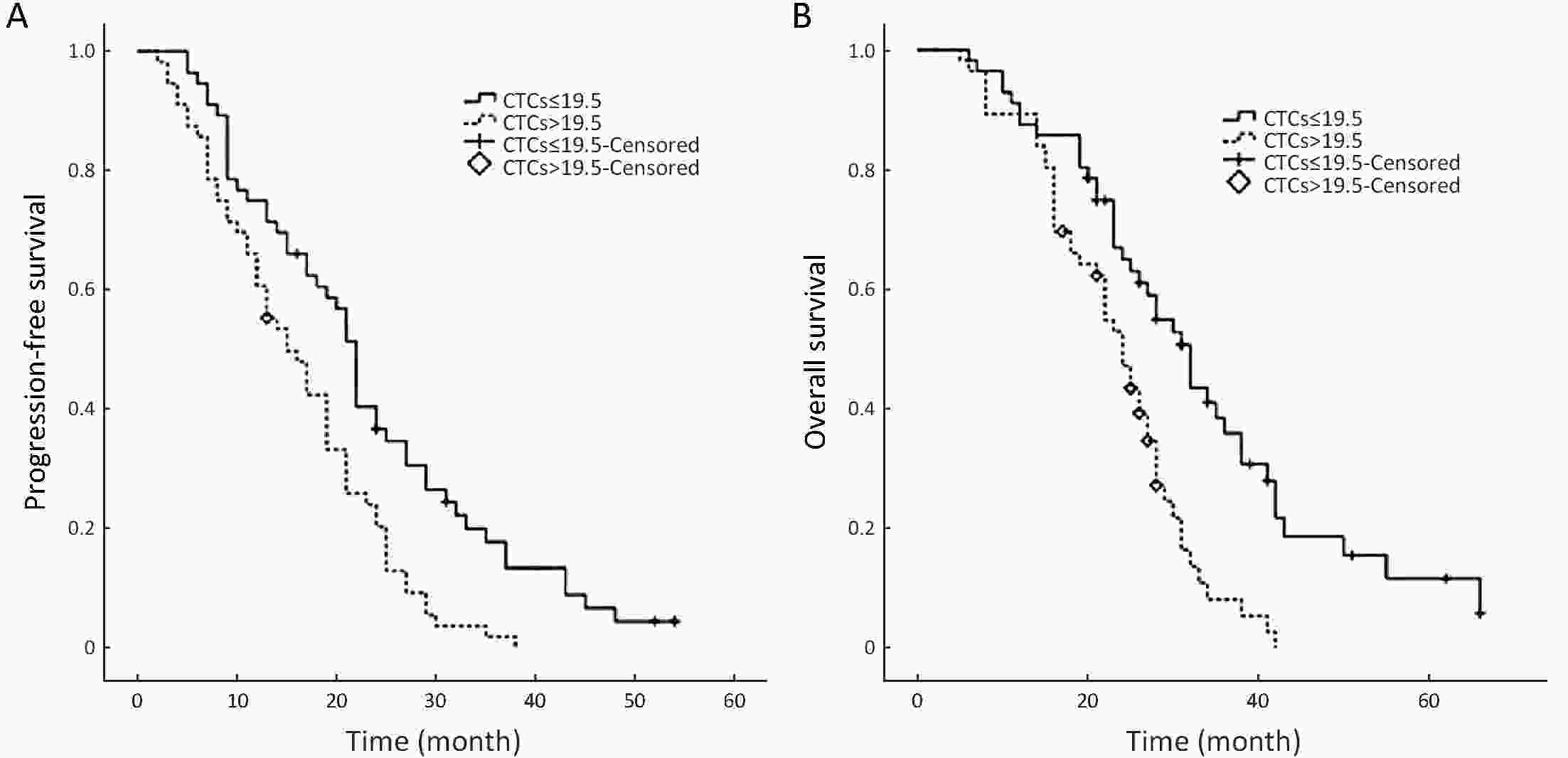
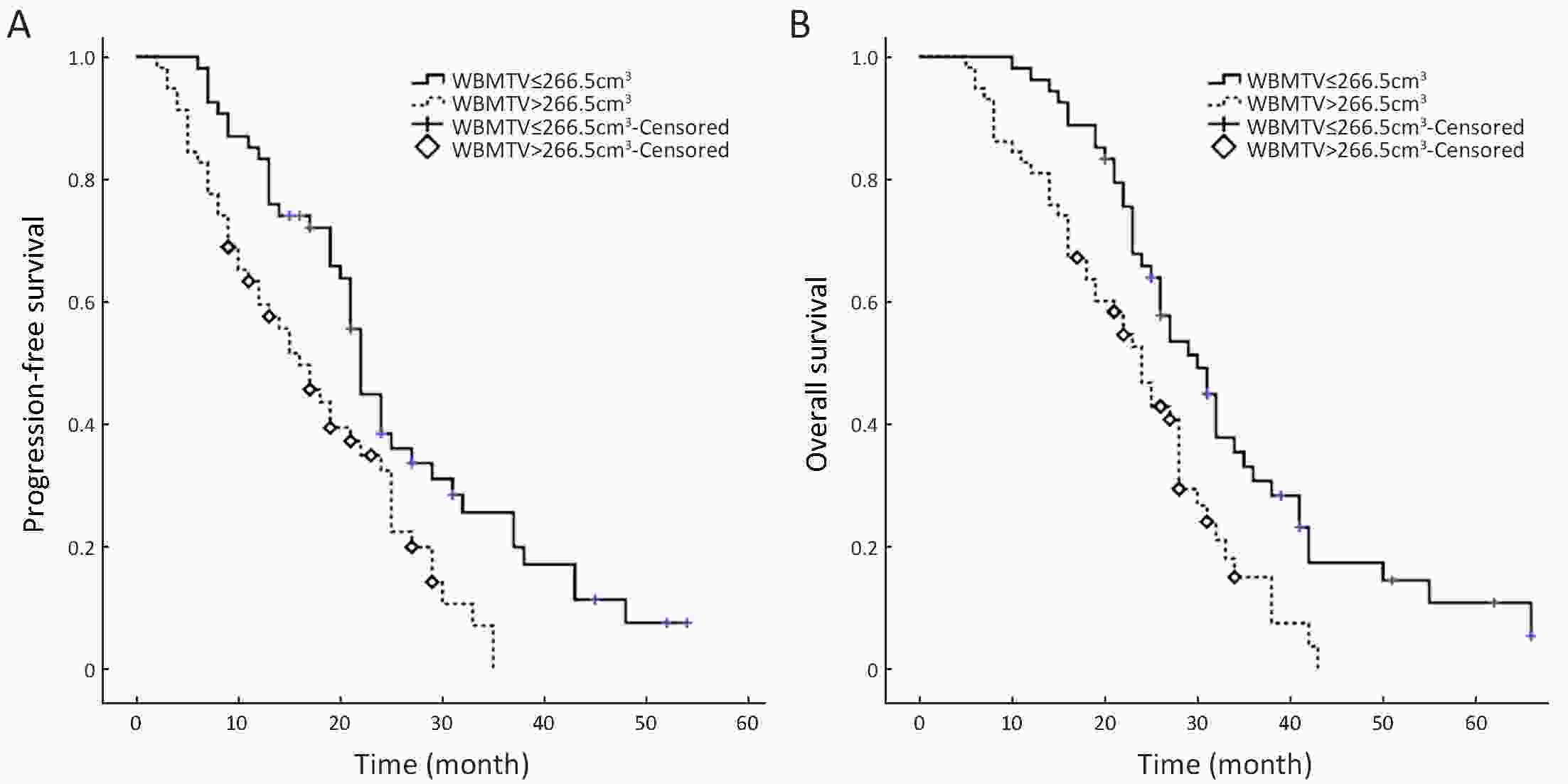
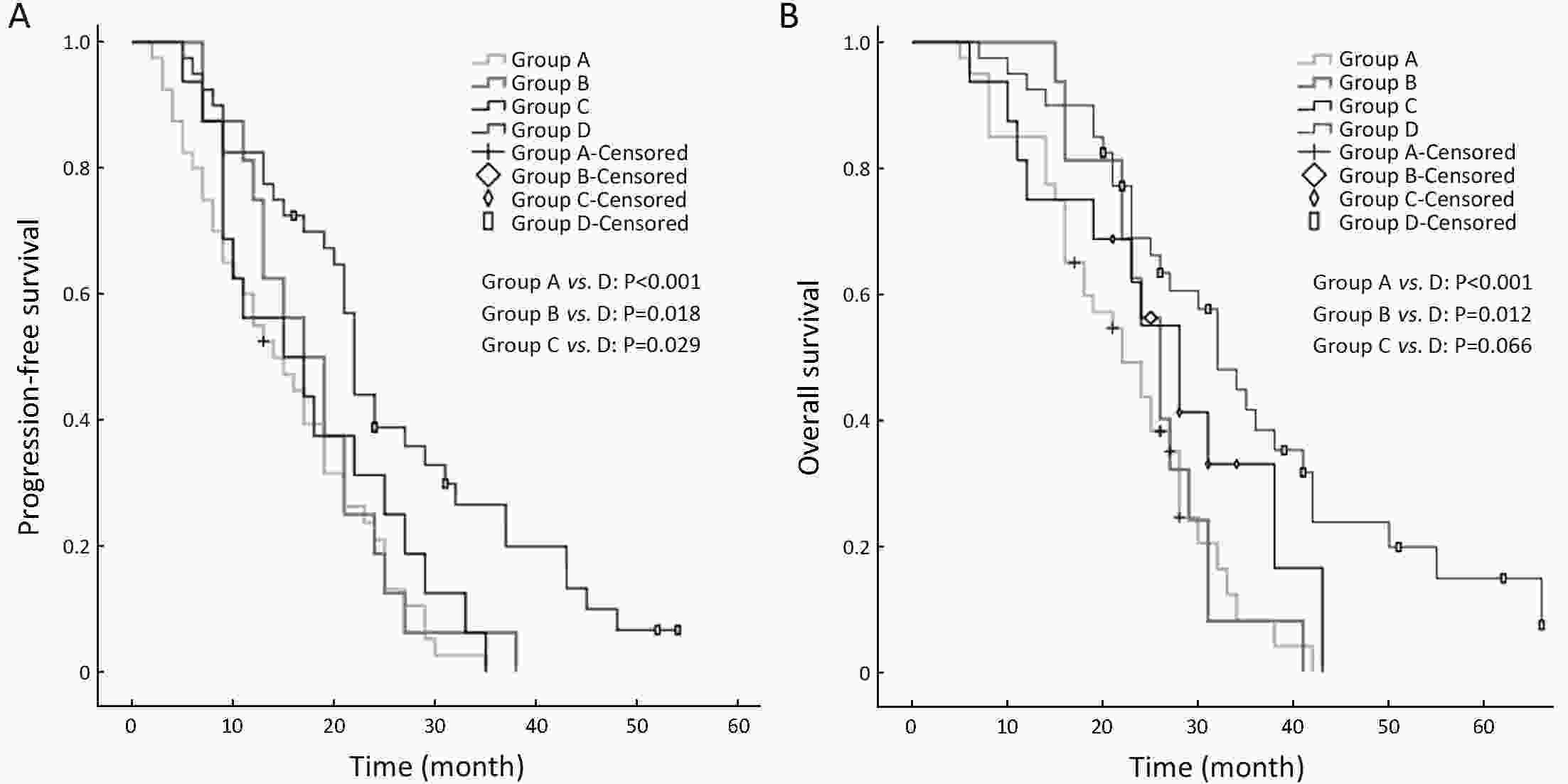
ObjectiveWe investigated the correlation between the number of circulating tumor cells (CTCs) and whole-body metabolic tumor volume (WBMTV) measured by 18F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT). The aim was to evaluate the value of the incorporation of CTC number and WBMTV in the prognostic prediction of stage III small-cell lung cancer (SCLC). MethodsOne hundred and twenty-nine patients were enrolled in this study. All patients were treated with four cycles of a platinum-based regimen and concurrent chest irradiation, followed by prophylactic cranial irradiation. Blood samples for CTC analysis were obtained from 112 patients before the initiation of chemotherapy (as a baseline), after cycle 1 and after cycle 4. CTCs were measured using the CELLSEARCH® system. The patients underwent pretreatment FDG PET/CT WBMTV, which included all malignant lesions. The Spearman rank test was used to determine the correlation among CTC counts, WBMTV and disease stage. Overall survival (OS) and progression-free survival (PFS) curves were produced using the Kaplan-Meier method, and survival differences between groups were assessed by the log-rank test. ResultsThe number of CTCs at baseline did not correlate with WBMTV before the initiation of therapy (P=0.241). The number of CTCs at baseline and the WBMTV before the initiation of therapy were independent relevant factors for PFS and OS. The subgroup analysis (Group A: CTC count >19.5 and a WBMTV >266.5 cm3; Group B: CTC count >19.5 and a WBMTV ≤266.5 cm3; Group C: CTC count ≤19.5 and a WBMTV >266.5 cm3; Group D: CTC count ≤19.5 and a WBMTV ≤266.5 cm3) showed that the differences were statistically significant in the median PFS (Group A vs. D, P<0.001; Group B vs. D, P=0.018; Group C vs. D, P=0.029) and in the median OS (Group A vs. D, P<0.001; Group B vs. D, P=0.012). ConclusionsCTC number and WBMTV are related to progression and death in patients with SCLC. The incorporation of CTC number and WBMTV scans can provide a detailed prognostic prediction for SCLC.
2018, 30(6): 605-612.
doi: 10.21147/j.issn.1000-9604.2018.06.05
Abstract:
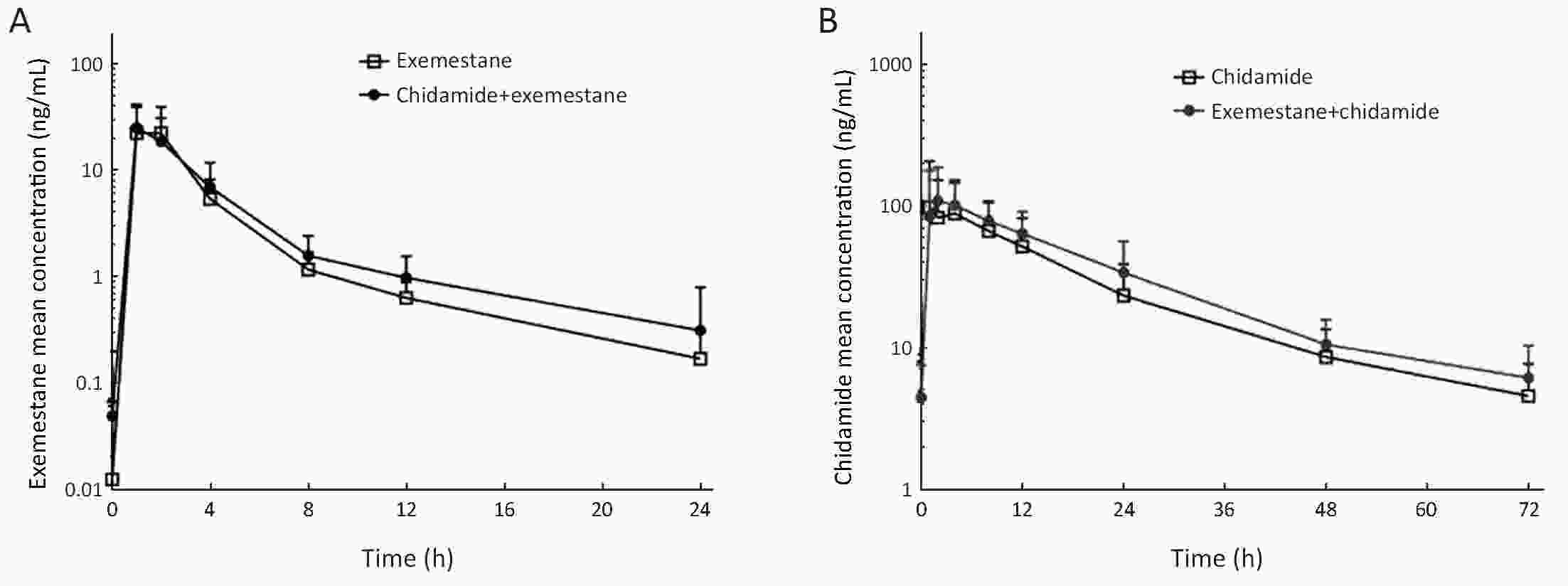
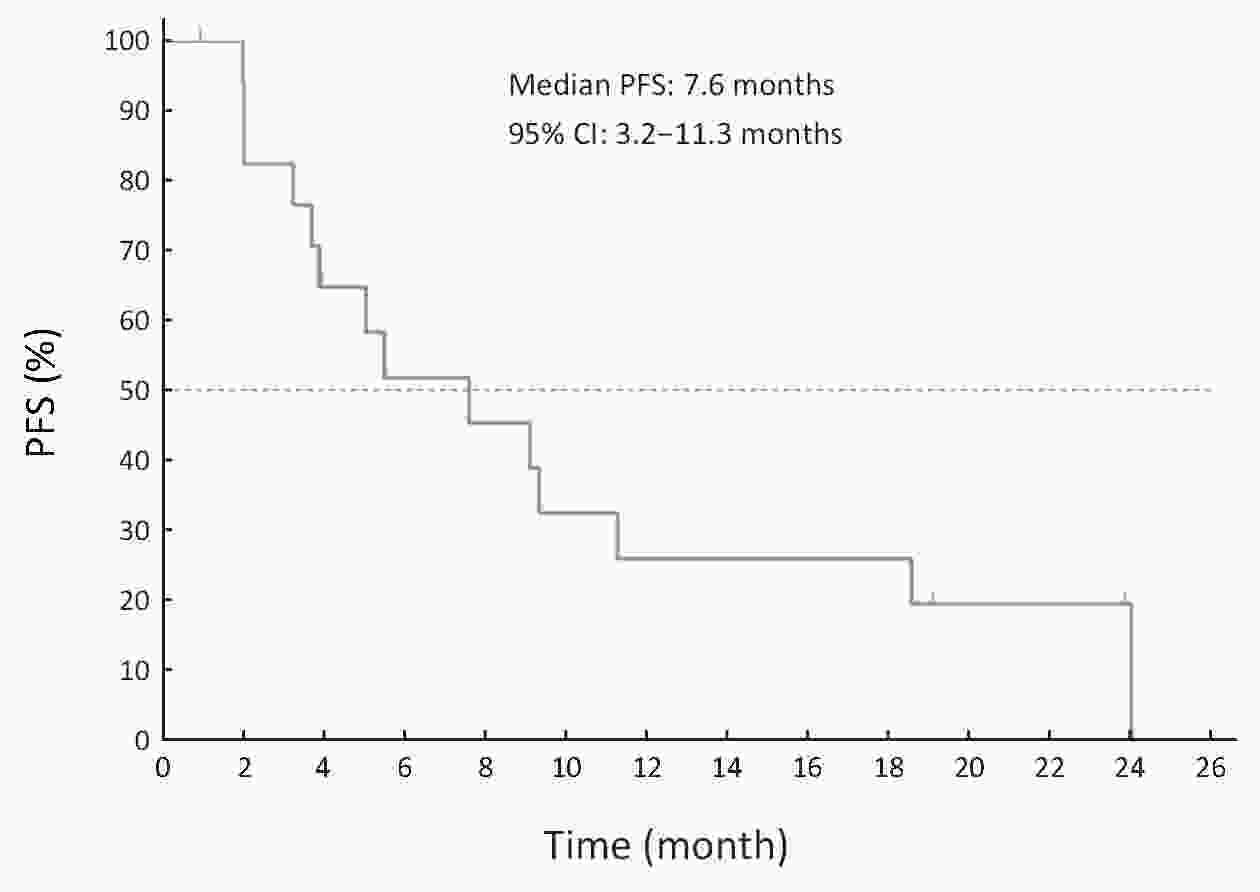
ObjectiveThe recurrence or progression under endocrine therapy in hormone receptor-positive (HR+) advanced breast cancer (ABC) remained a critical clinical challenge. Chidamide is an oral subtype-selective histone deacetylase (HDAC) inhibitor with multiple functions in tumor growth inhibition and microenvironment modulation via epigenetic reprogramming. The purpose of this study was to evaluate the safety, pharmacokinetics (PK), and preliminary efficacy of chidamide in combination with exemestane in HR+ ABC patients. MethodsEligible patients were postmenopausal women with HR+ ABC recurrent or progressed to at least one endocrine therapy. Blood samples were obtained in the run-in period and the first day of combination treatment for PK analysis. In combination treatment, patients were given exemestane 25 mg daily and chidamide 30 mg twice a week (BIW) until progression of disease or intolerable toxicities. A treatment cycle was defined as 4 weeks. Safety, PK parameters, and preliminary efficacy were evaluated. ResultsA total of 20 patients were enrolled between July and December, 2015. The median number of treatments cycle was 5.2 (20.8 weeks) with 2 patients still on treatment at the data cut-off date of October, 2017. The treatment-related adverse events (AE) ≥ grade 3 in more than 2 patients were neutropenia (35%), thrombocytopenia (30%), and leucopenia (20%). The plasma exposure of exemestane was consistent in the presence or absence of chidamide. A slight increase in chidamide exposure was noted in the presence of exemestane, probably due to the inter- and intra-patient variations. The best response in 16 evaluable patients was assessed by Response Evaluation Criteria in Solid Tumors (RECIST), including 4 patients with partial response, 10 patients with stable disease. The median progression-free survival (PFS) was 7.6 months. ConclusionsThe combination of chidamide with exemestane was generally well tolerated with promising preliminary efficacy in HR+ ABC patients. The overall results from this study encourage further pivotal trial in this patient population.
2018, 30(6): 613-622.
doi: 10.21147/j.issn.1000-9604.2018.06.06
Abstract:
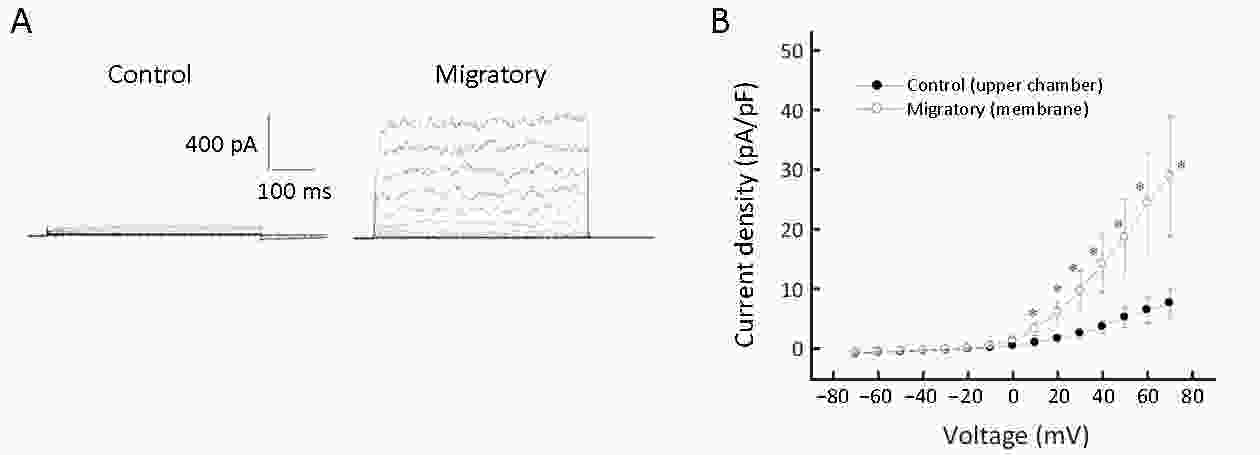
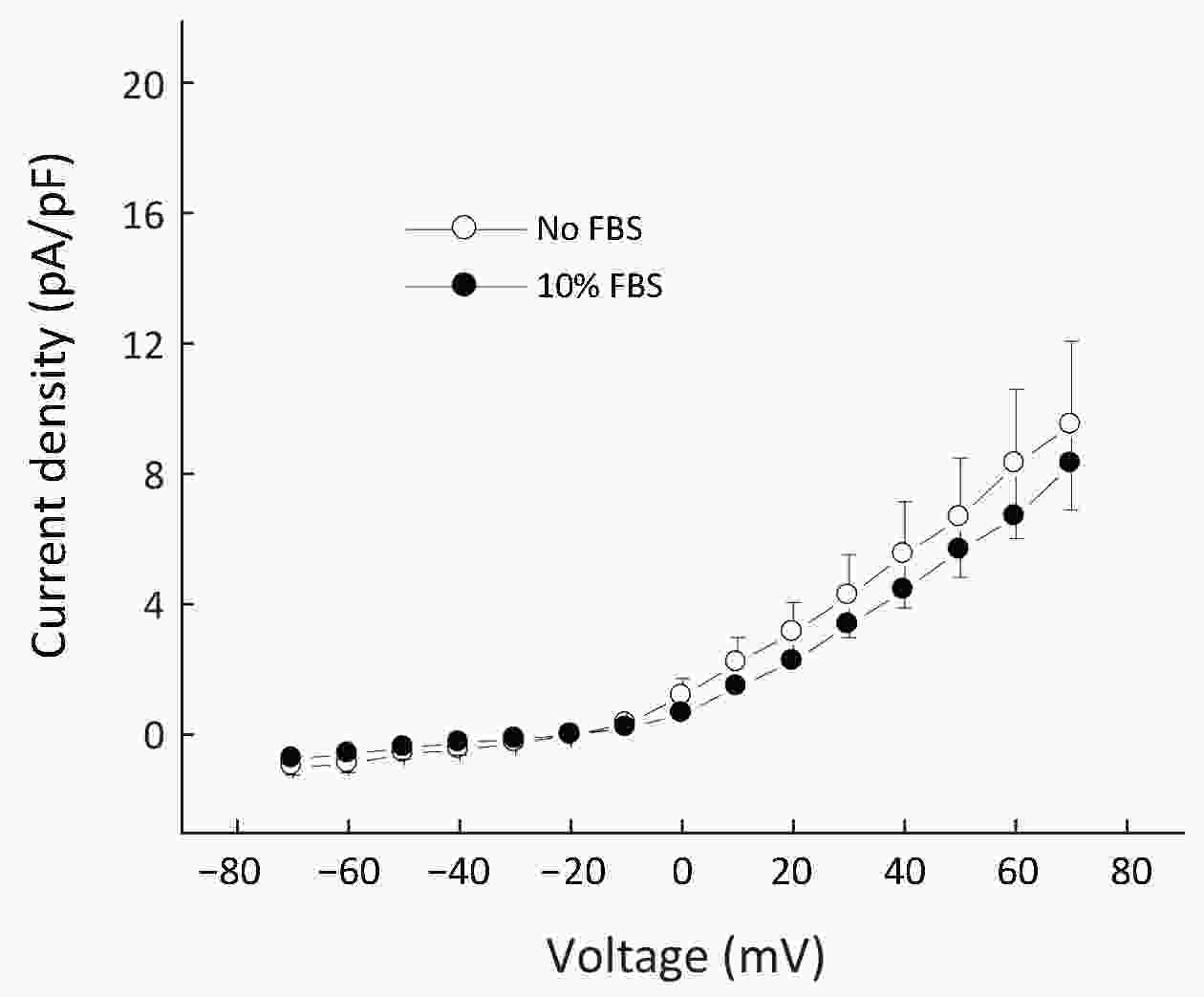
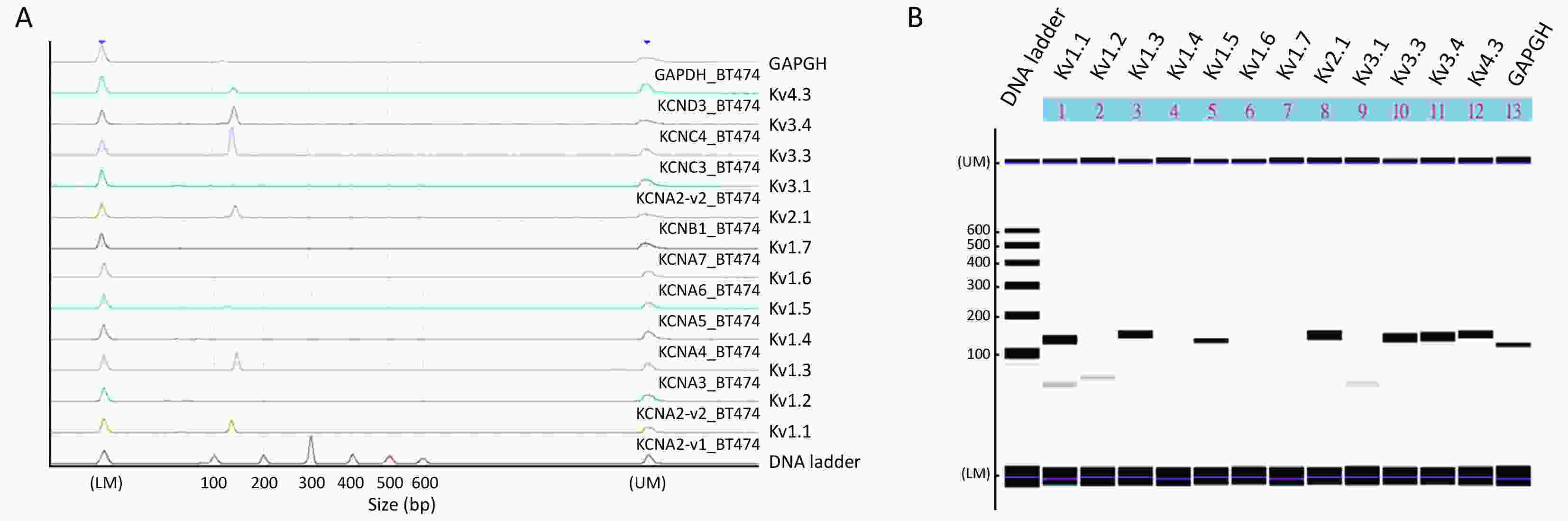
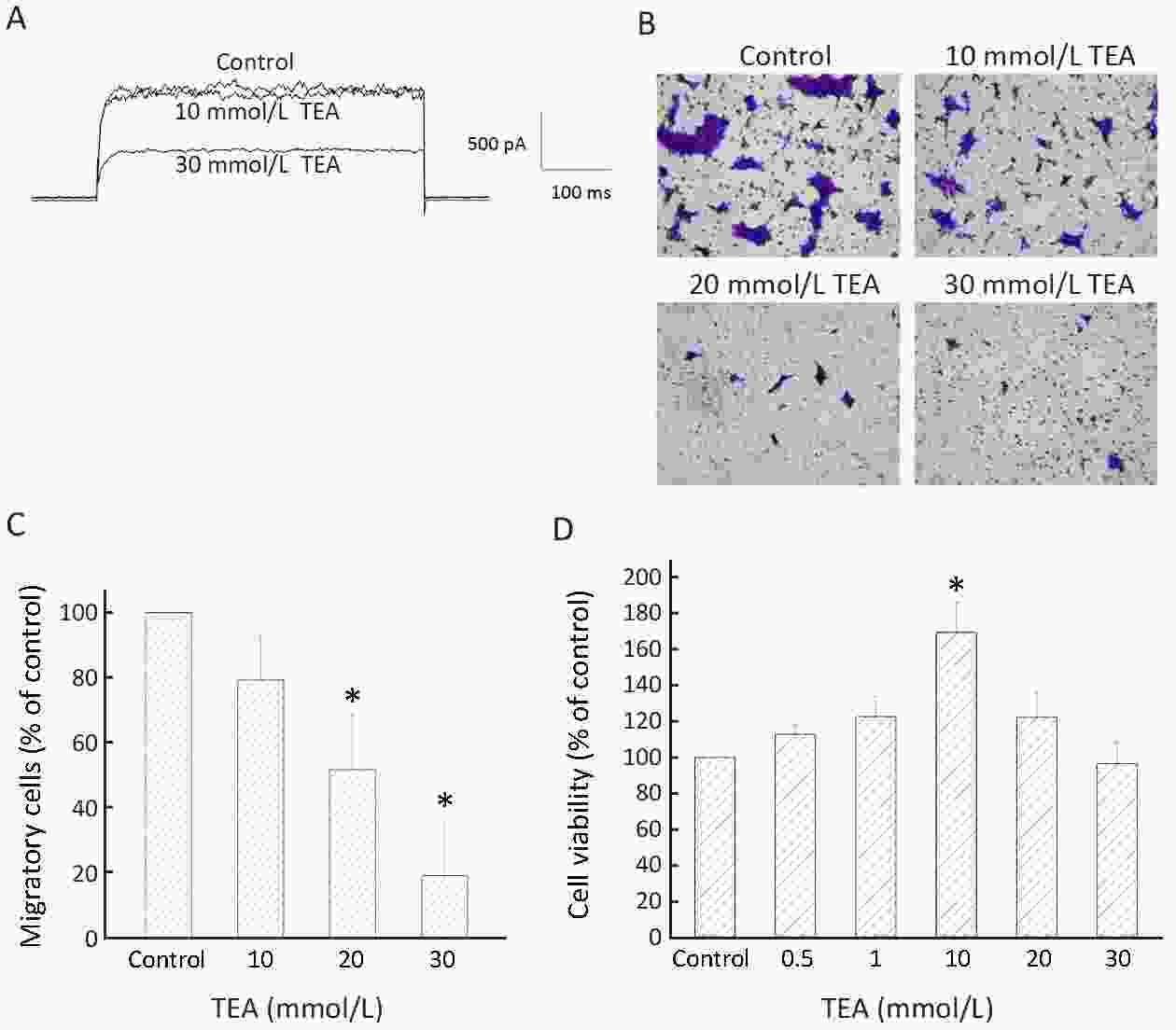
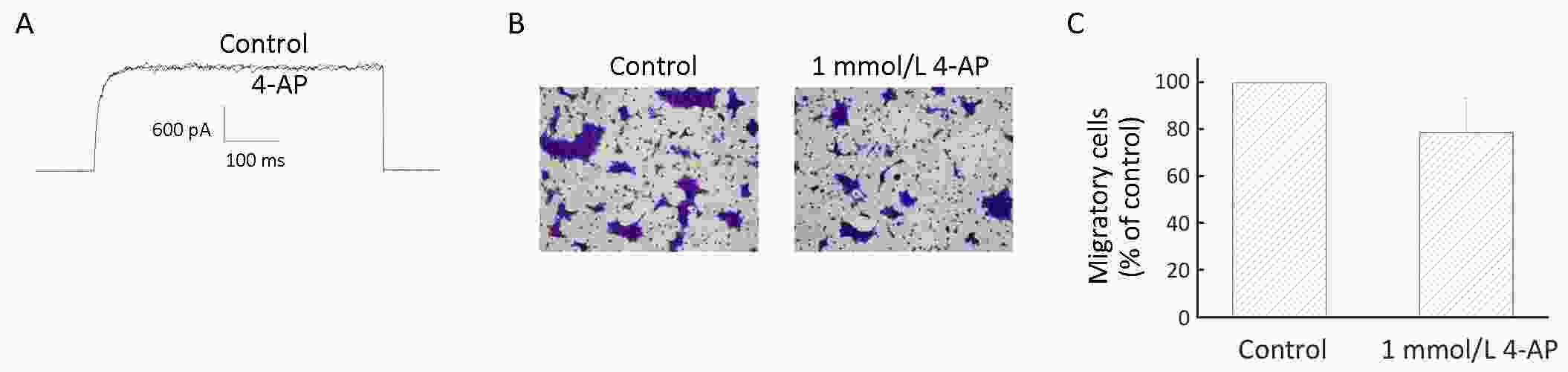
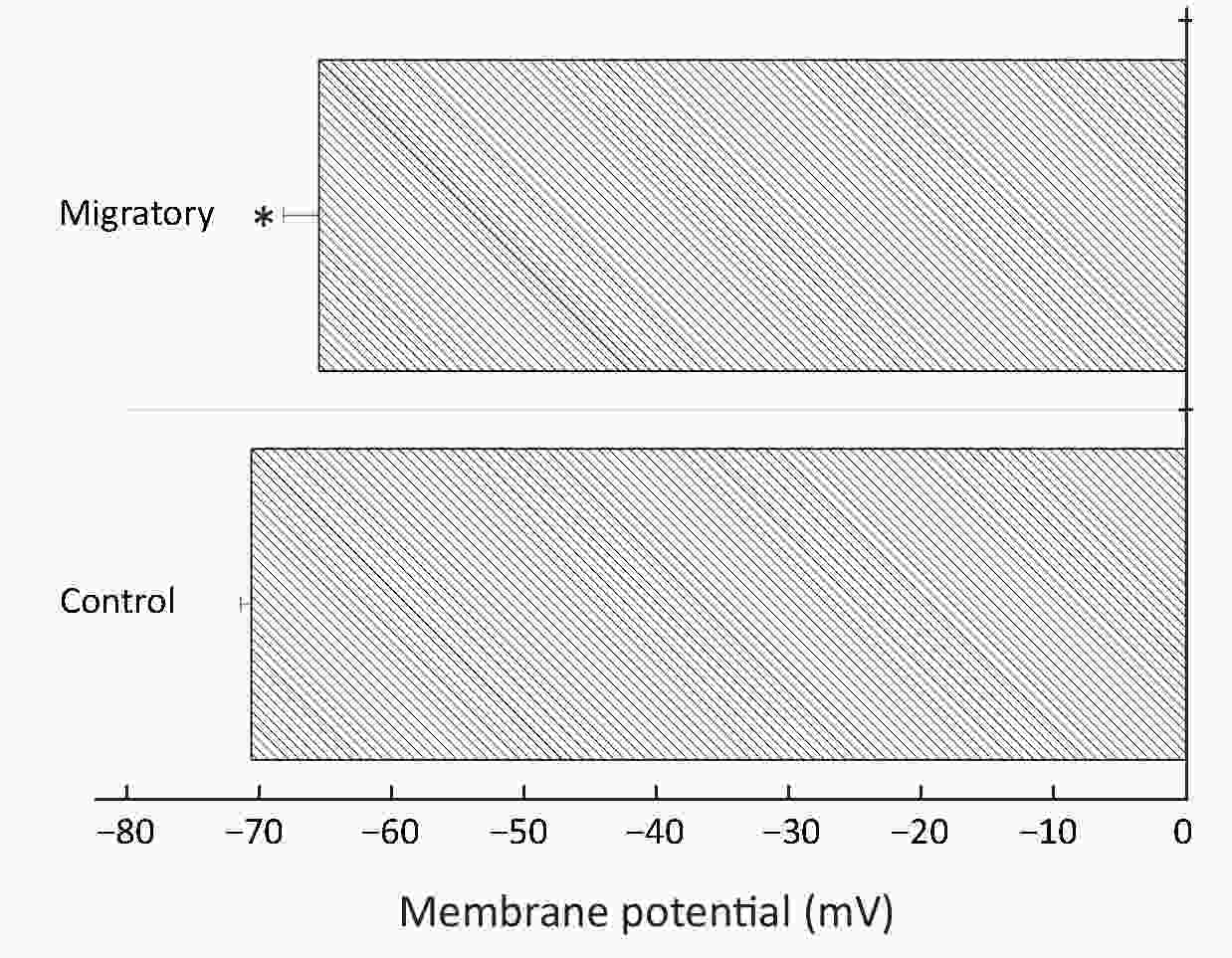
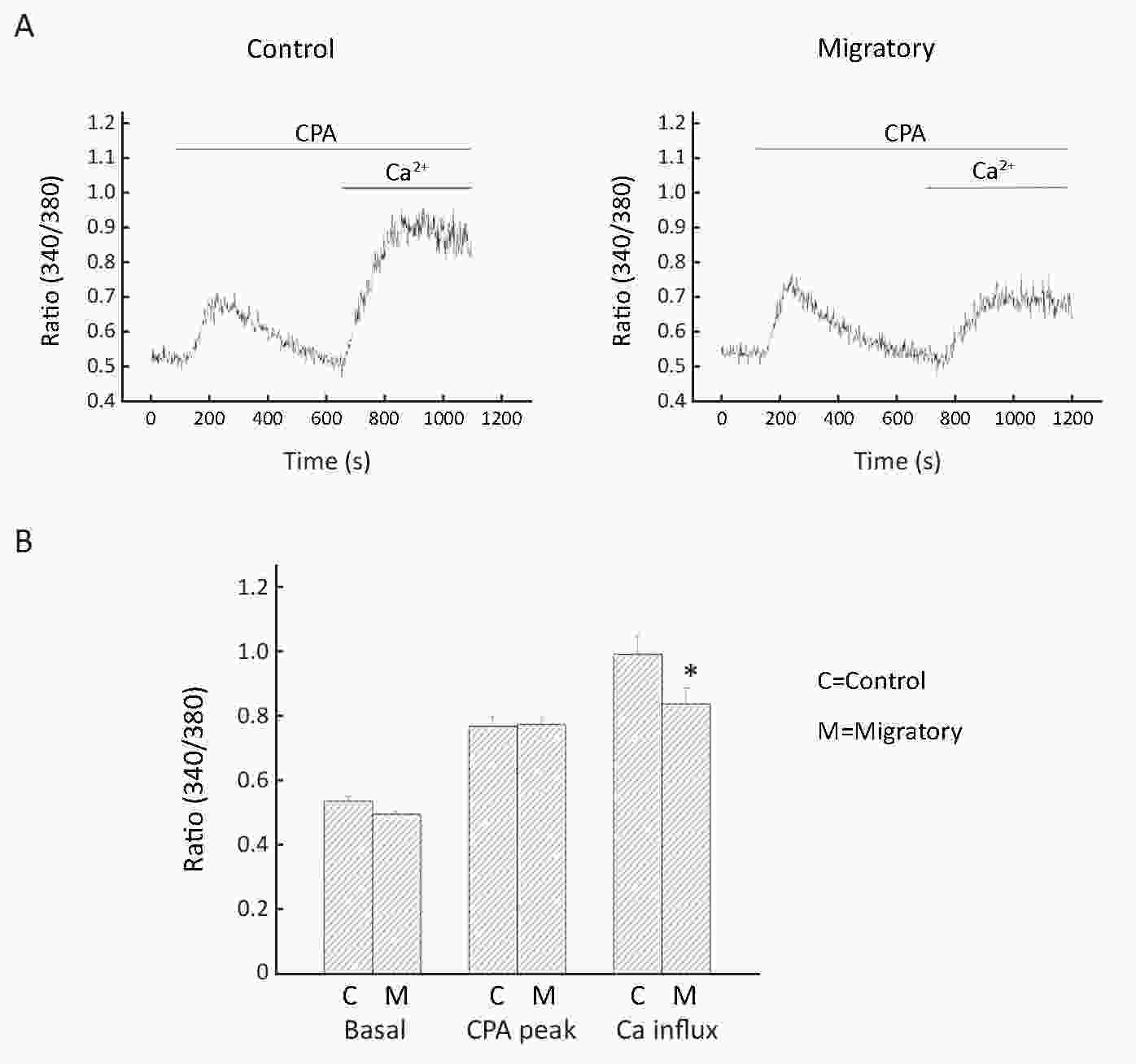
ObjectiveA variety of ion channels have been implicated in breast cancer proliferation and metastasis. Voltage-gated K+ (Kv) channels not only cause repolarization in excitable cells, but are also involved in multiple cellular functions in non-excitable cells. In this study we investigated the role of Kv channels in migration of BT474 breast cancer cells. MethodsTranswell technique was used to separate migratory cells from non-migratory ones and these two groups of cells were subject to electrophysiological examinations and microfluorimetric measurements for cytosolic Ca2+. Cell migration was examined in the absence or presence of Kv channel blockers. ResultsWhen compared with non-migratory cells, migratory cells had much higher Kv current densities, but rather unexpectedly, more depolarized membrane potential and reduced Ca2+ influx. Reverse transcriptase-polymerase chain reaction (RT-PCR) analysis revealed the presence of Kv1.1, Kv1.3, Kv1.5, Kv2.1, Kv3.3, Kv3.4 and Kv4.3 channels. Cell migration was markedly inhibited by tetraethylammonium (TEA), a delayed rectifier Kv channel blocker, but not by 4-aminopyridine, an A-type Kv channel blocker. ConclusionsTaken together, our results show that increased Kv channel expression played a role in BT474 cell migration, and Kv channels could be considered as biomarkers or potential therapeutic targets for breast cancer metastasis. The mechanism(s) by which Kv channels enhanced migration appeared unrelated to membrane hyperpolarization and Ca2+ influx.
2018, 30(6): 623-632.
doi: 10.21147/j.issn.1000-9604.2018.06.07
Abstract:
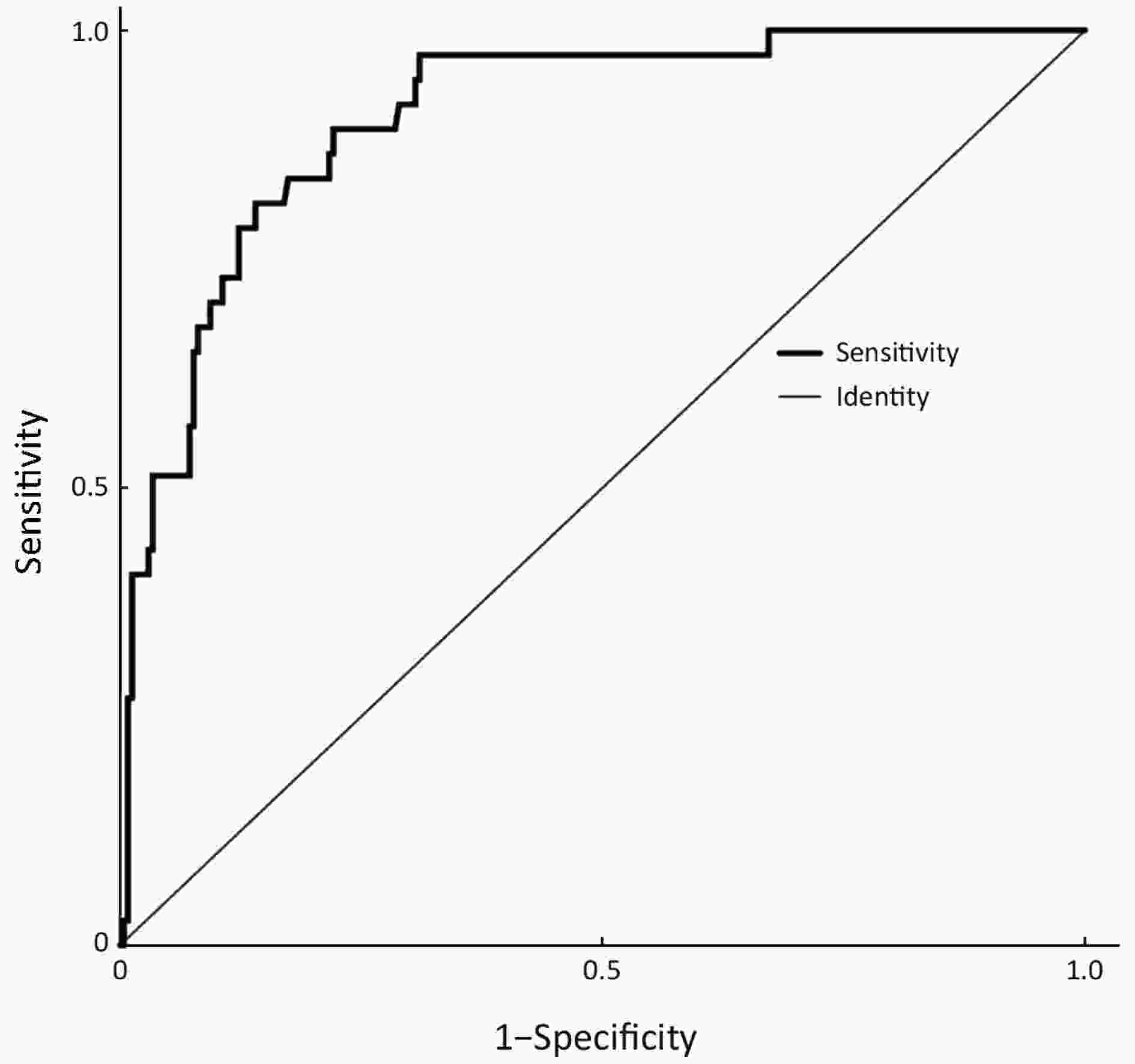
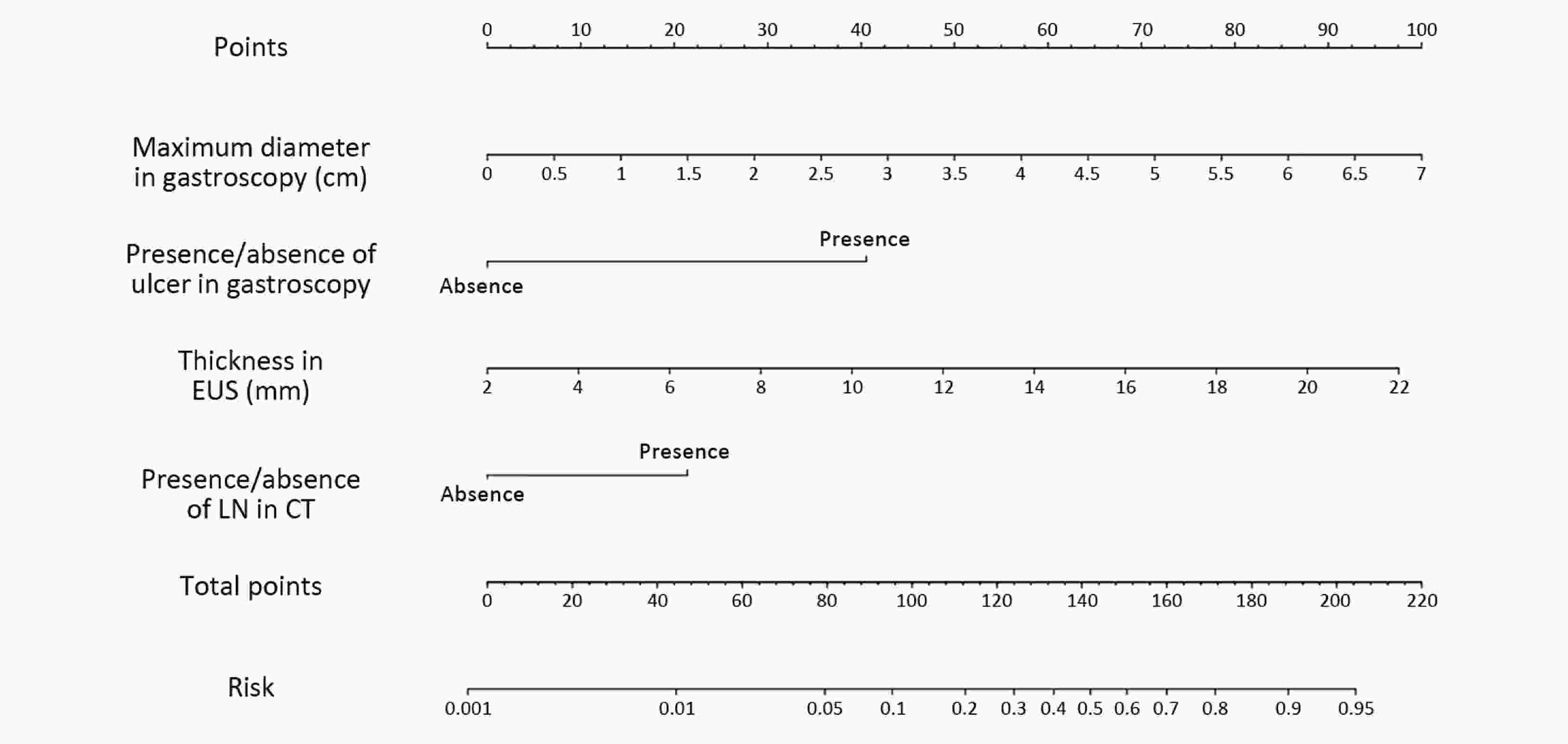
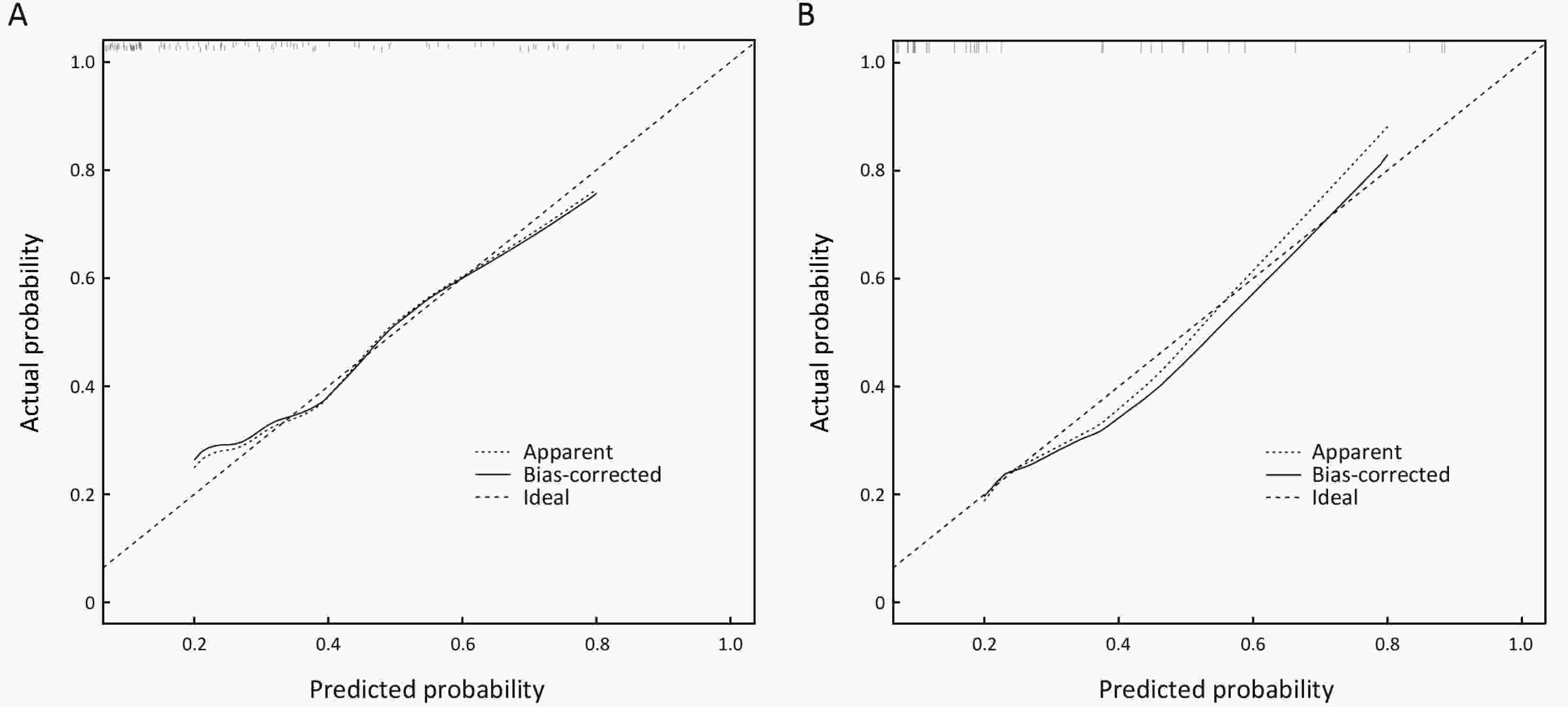
ObjectiveTo create a nomogram to predict the incidence of lymph node metastasis (LNM) in early gastric cancer (EGC) patients and to externally validate the nomogram. MethodsTo construct the nomogram, we retrospectively analyzed a primary cohort of 272 EGC patients. Univariate analysis and a binary logistic regression were performed. A nomogram predicting the incidence of LNM in EGC patients was created. The discrimination ability of the nomogram was measured using the concordance index (c-index), and the nomogram was also calibrated. Then, another prospective cohort of 81 patients was analyzed to validate the nomogram. ResultsIn the primary cohort, LNM was pathologically confirmed in 37 (13.6%) patients. In multivariate analysis, the presence of an ulcer, the maximum lesion diameter observed via gastroscopy, the thickness of the lesion observed via endoscopic ultrasonography, and the presence of enlarged lymph nodes on computed tomography (CT) were independent risk factors for LNM. A nomogram was then created based on the regression model with the c-index of 0.905, and the calibration curve of the nomogram fell approximately on the ideal 45-degree line. The cut-off score of the nomogram was 110, and the sensitivity, specificity, positive predictive and negative predictive values of the nomogram in the primary cohort were 81.1%, 86.0%, 47.6% and 96.7%, respectively, and in the prospective validation cohort were 75.0%, 91.0%, 60.0% and 95.5%, respectively. The calibration curve of the external validation cohort was almost on the 45-degree line. ConclusionsWe developed an effective nomogram predicting the incidence of LNM for EGC patients.
2018, 30(6): 633-646.
doi: 10.21147/j.issn.1000-9604.2018.06.08
Abstract:
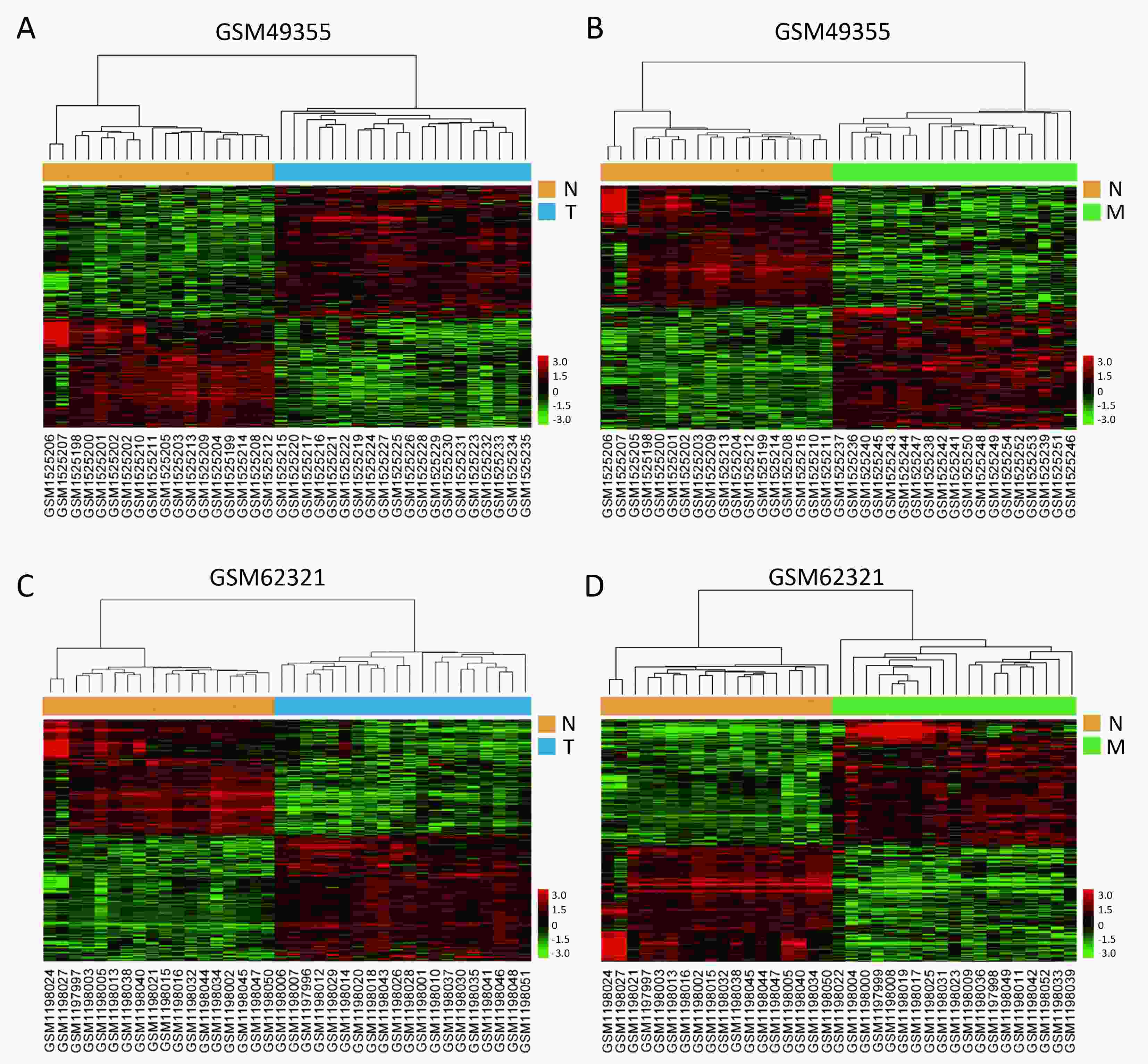
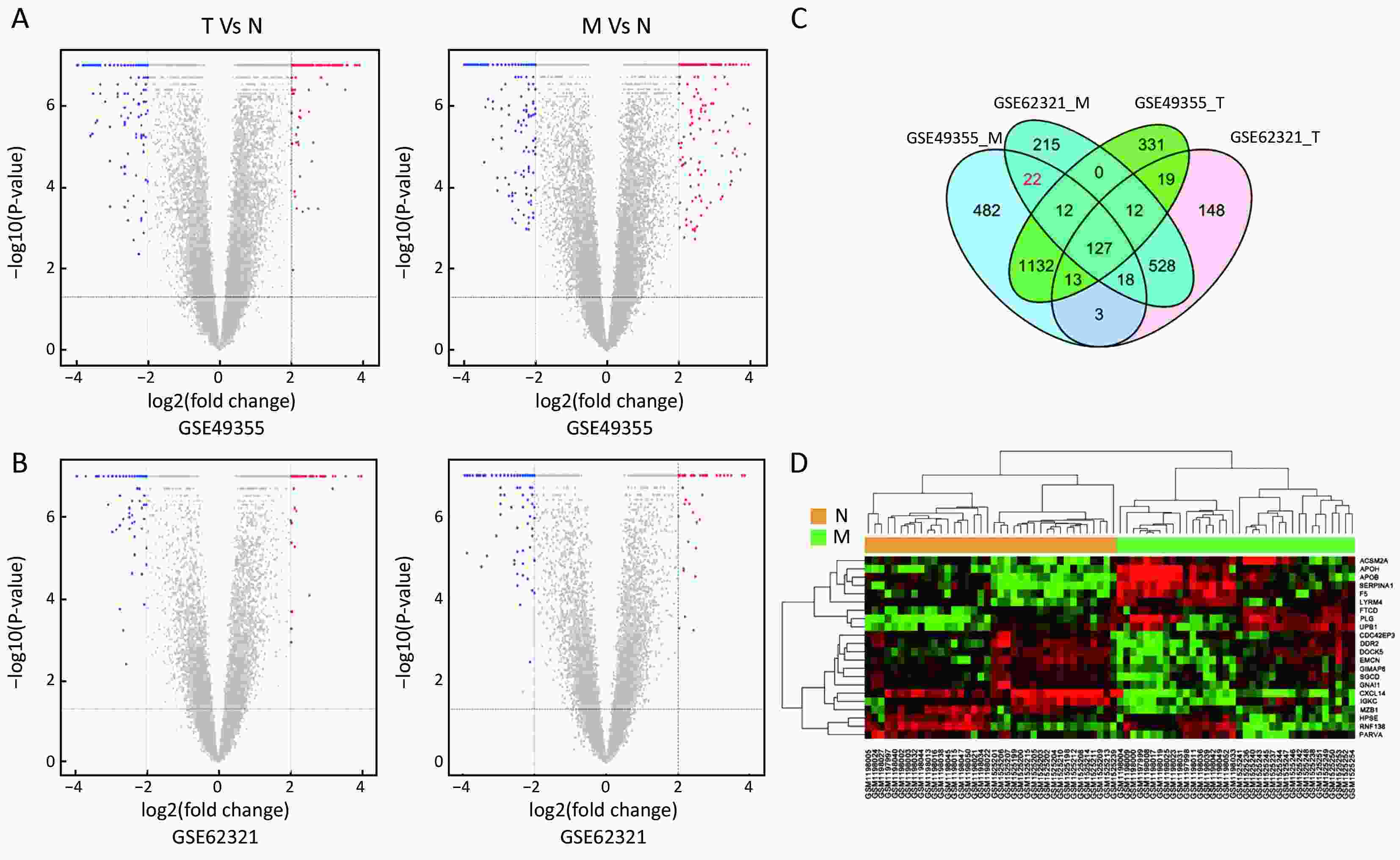
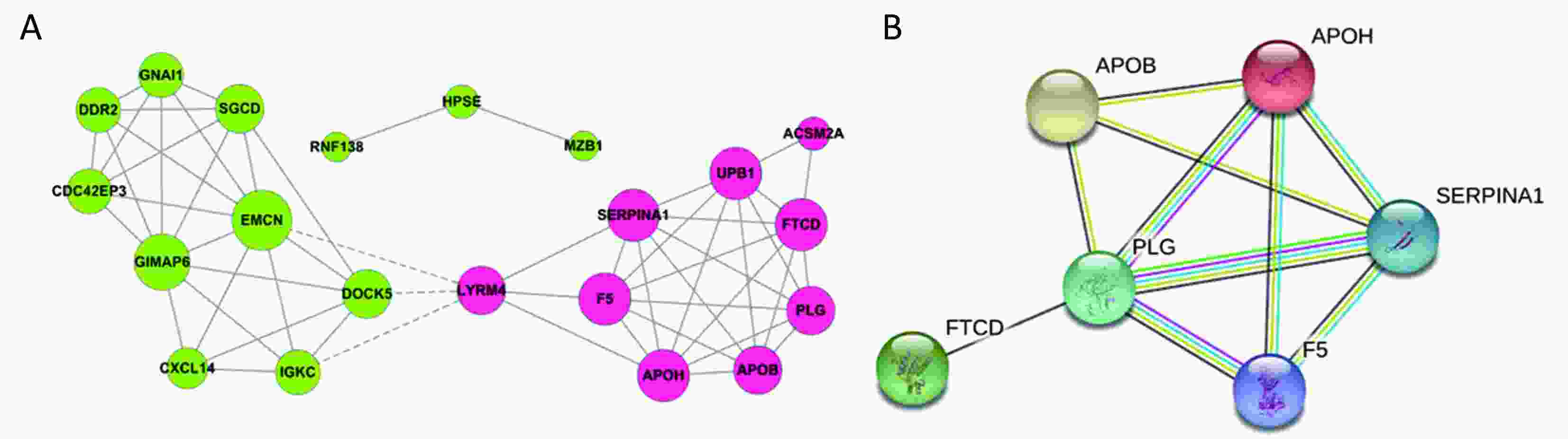
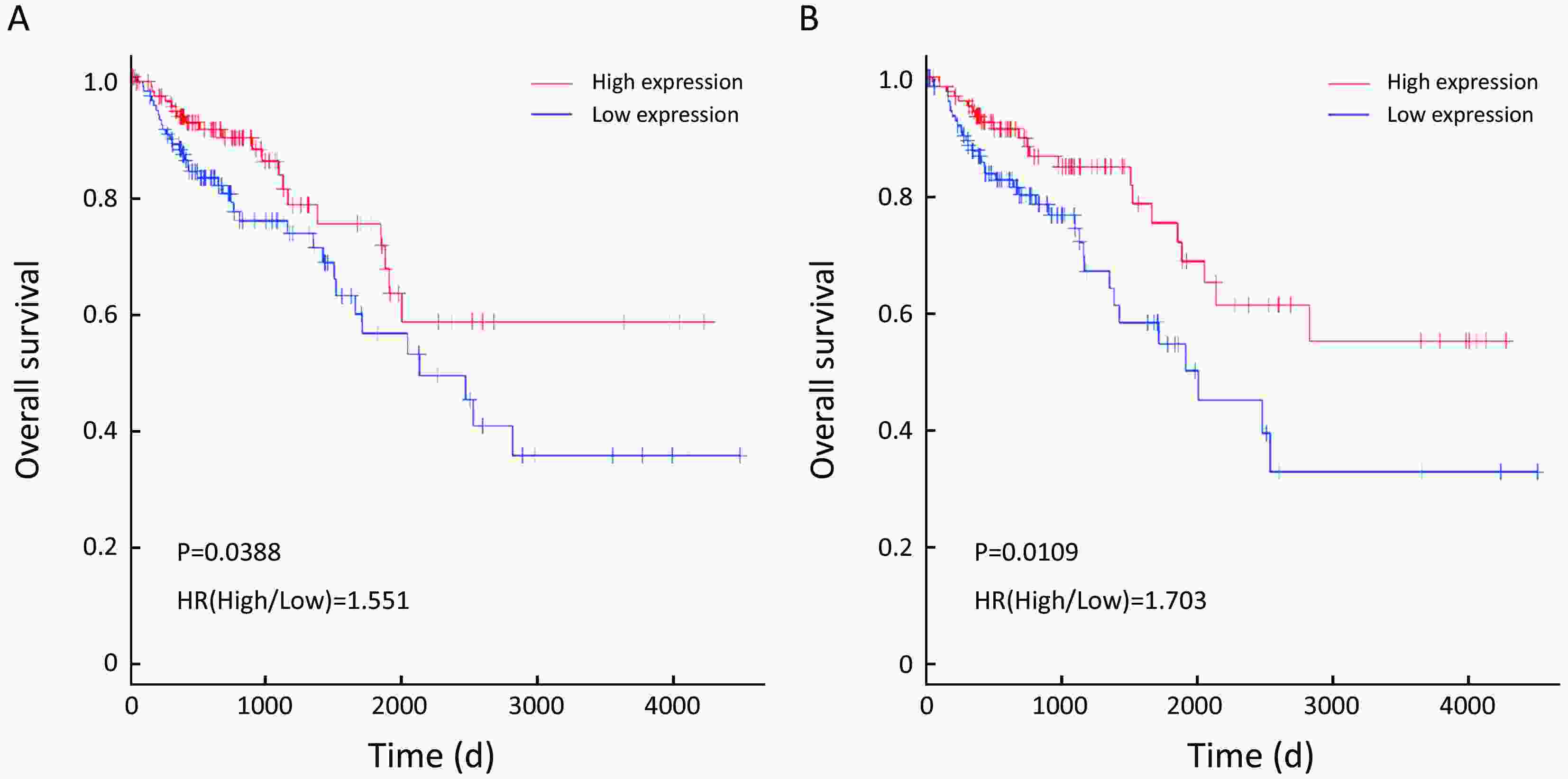
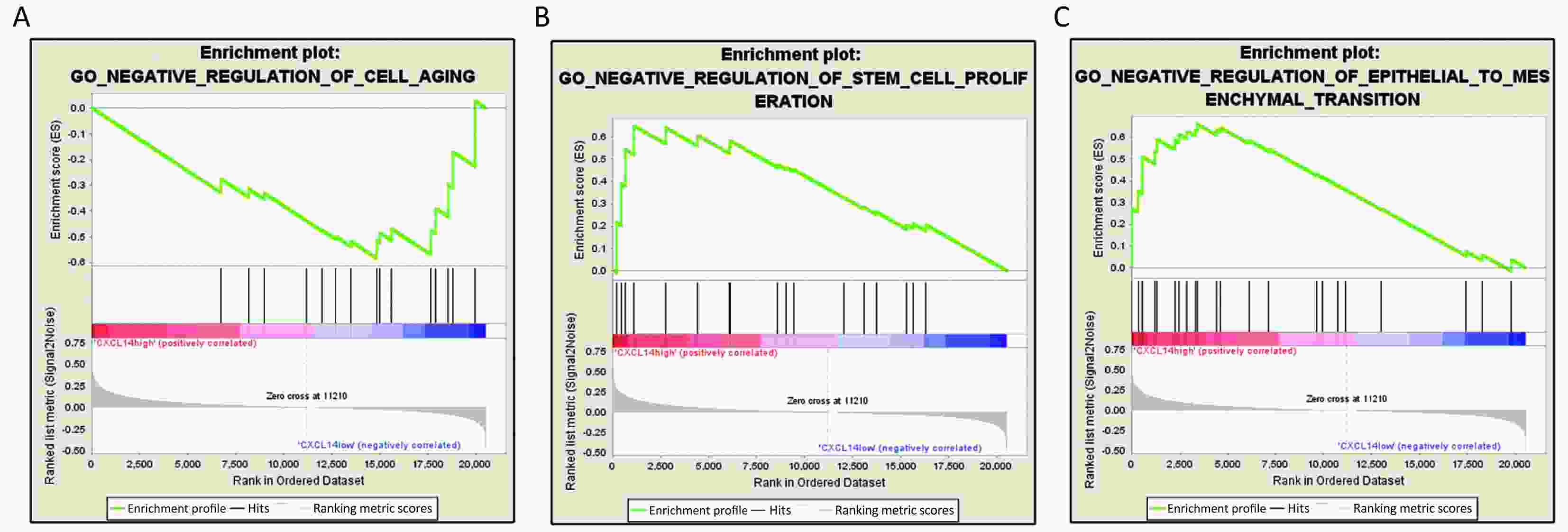
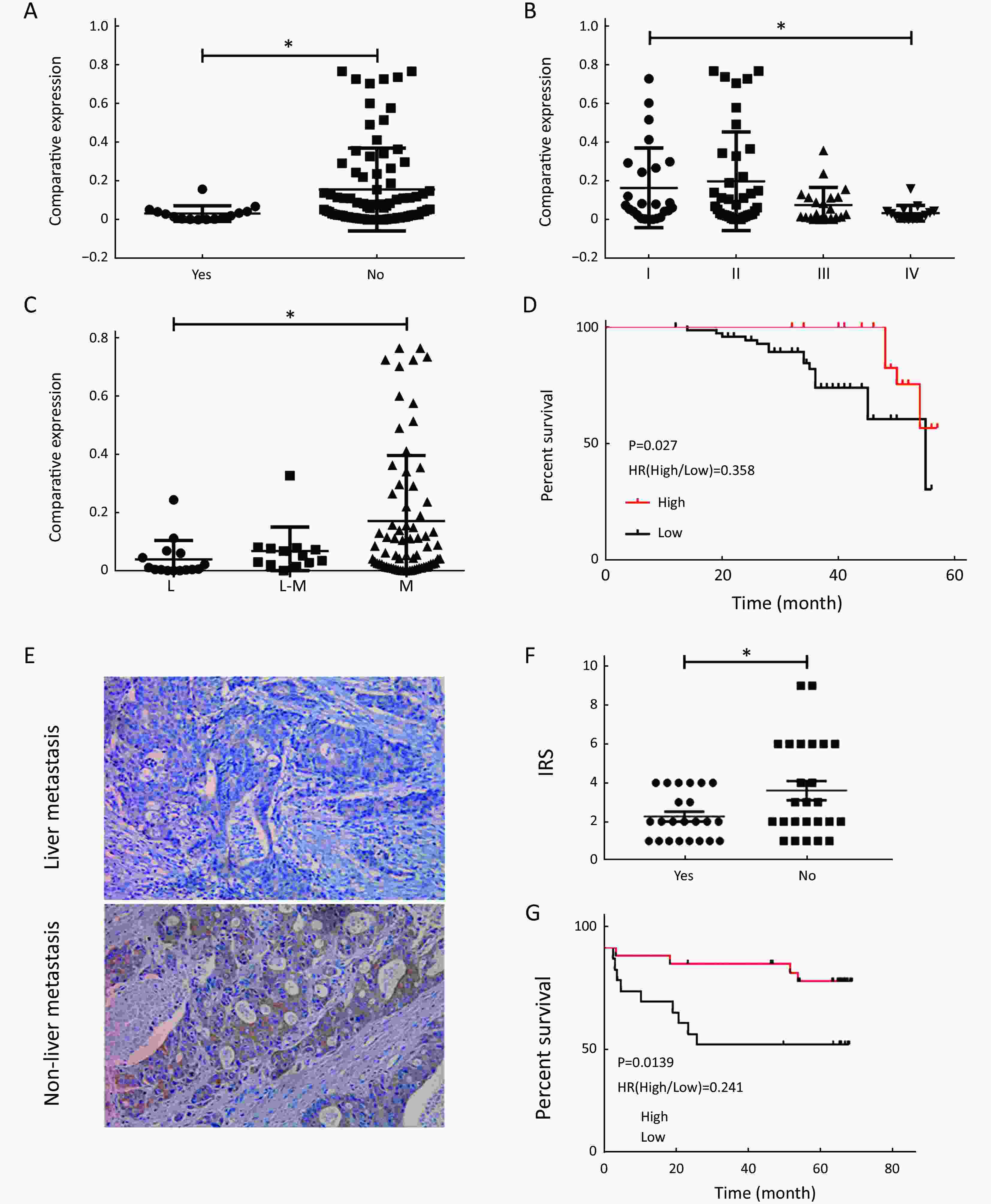
ObjectiveLiver metastasis, which contributes substantially to high mortality, is the most common recurrent mode of colon carcinoma. Thus, it is necessary to identify genes implicated in metastatic colonization of the liver in colon carcinoma. MethodsWe compared mRNA profiling in 18 normal colon mucosa (N), 20 primary tumors (T) and 19 liver metastases (M) samples from the dataset GSE49355 and GSE62321 of Gene Expression Omnibus (GEO) database. Gene ontology (GO) and pathways of the identified genes were analyzed. Co-expression network and protein-protein interaction (PPI) network were employed to identify the interaction relationship. Survival analyses based on The Cancer Genome Atlas (TCGA) database were used to further screening. Then, the candidate genes were validated by our data. ResultsWe identified 22 specific genes related to liver metastasis and they were strongly associated with cell migration, adhesion, proliferation and immune response. Simultaneously, the results showed that C-X-C motif chemokine ligand 14 (CXCL14) might be a favorable prediction factor for survival of patients with colon carcinoma. Importantly, our validated data further suggested that lower CXCL14 represented poorer outcome and contributed to metastasis. Gene set enrichment analysis (GSEA) showed that CXCL14 was negatively related to the regulation of stem cell proliferation and epithelial to mesenchymal transition (EMT). ConclusionsCXCL14 was identified as a crucial anti-metastasis regulator of colon carcinoma for the first time, and might provide novel therapeutic strategies for colon carcinoma patients to improve prognosis and prevent metastasis.
2018, 30(6): 647-655.
doi: 10.21147/j.issn.1000-9604.2018.06.09
Abstract:
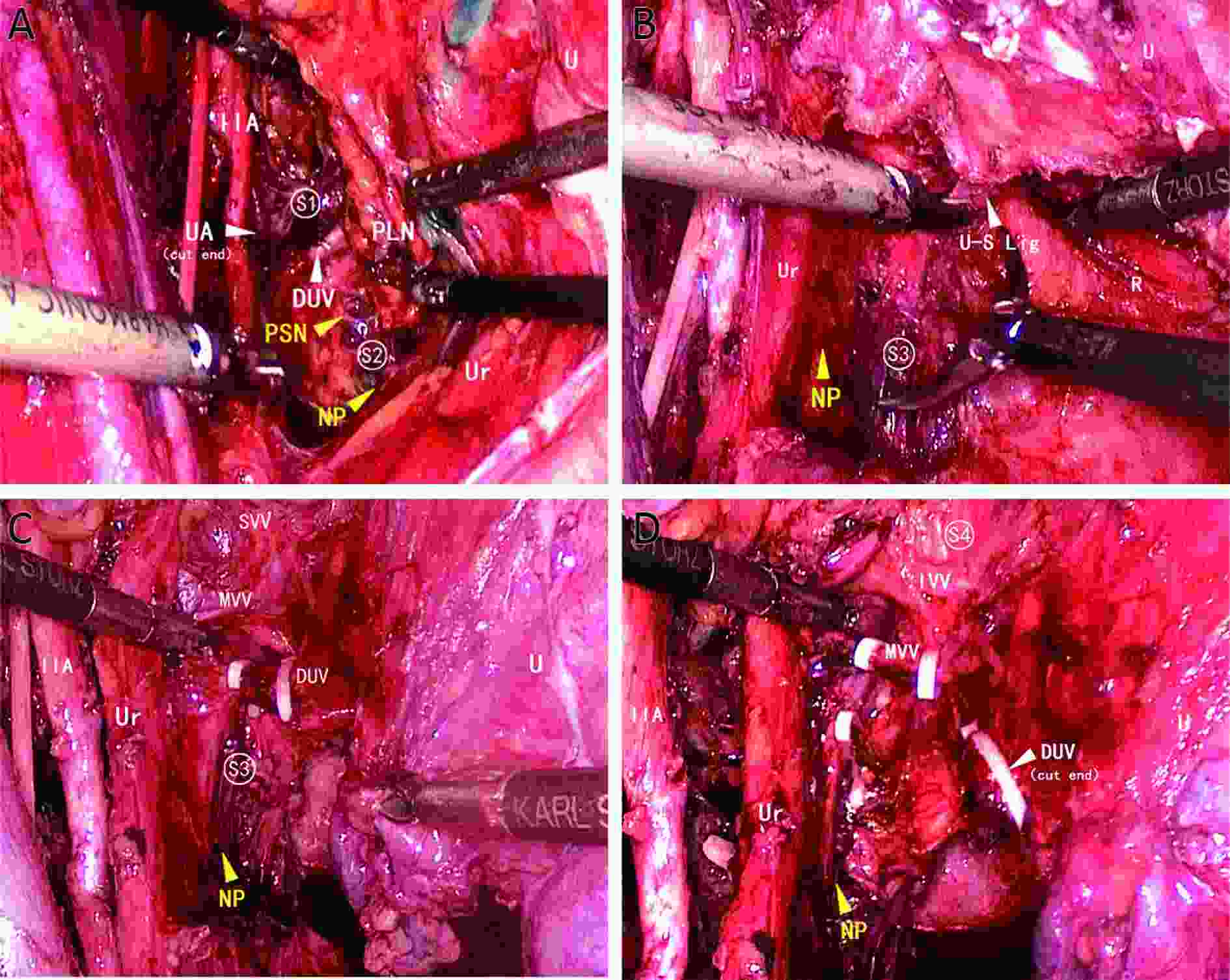
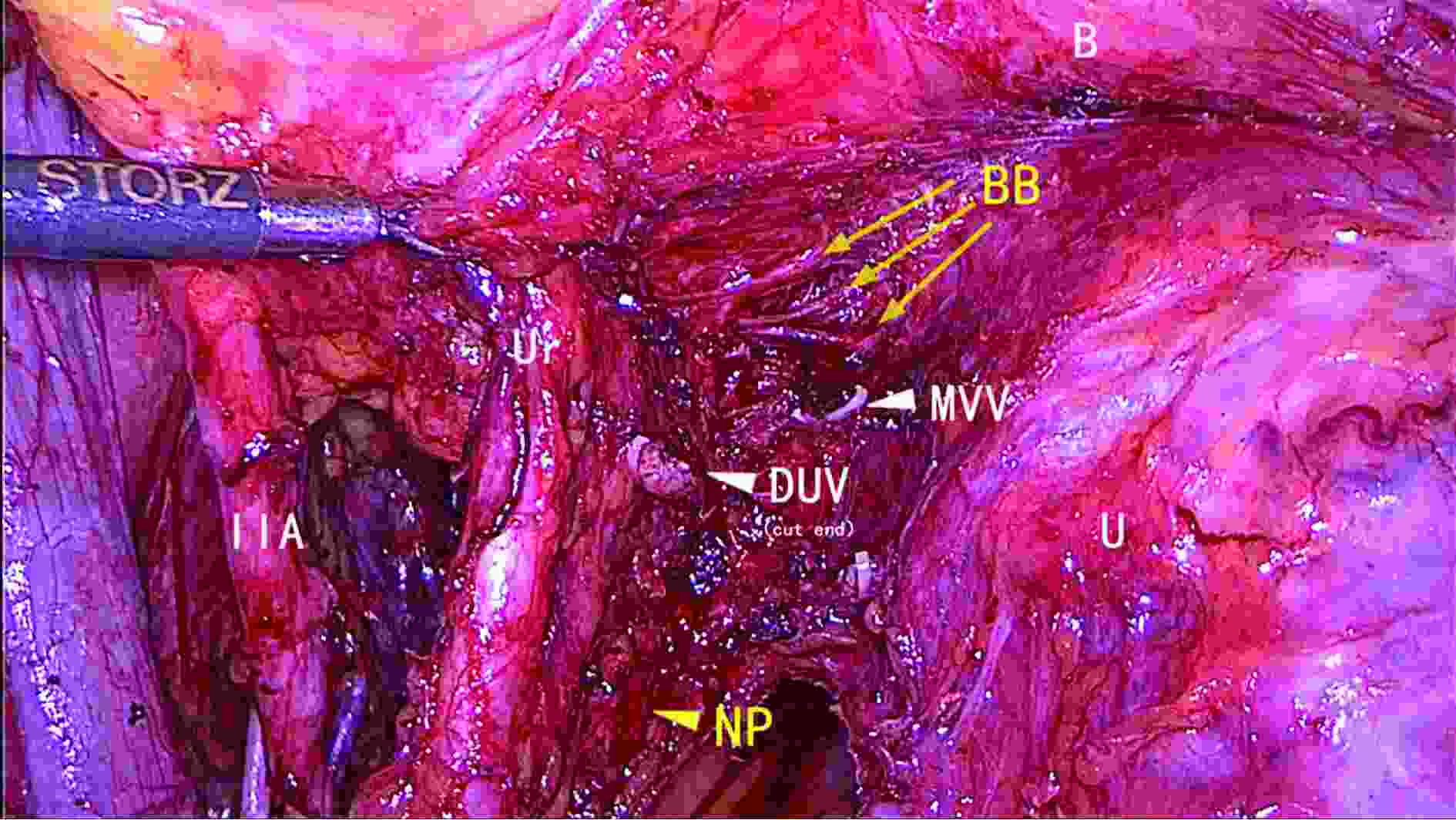
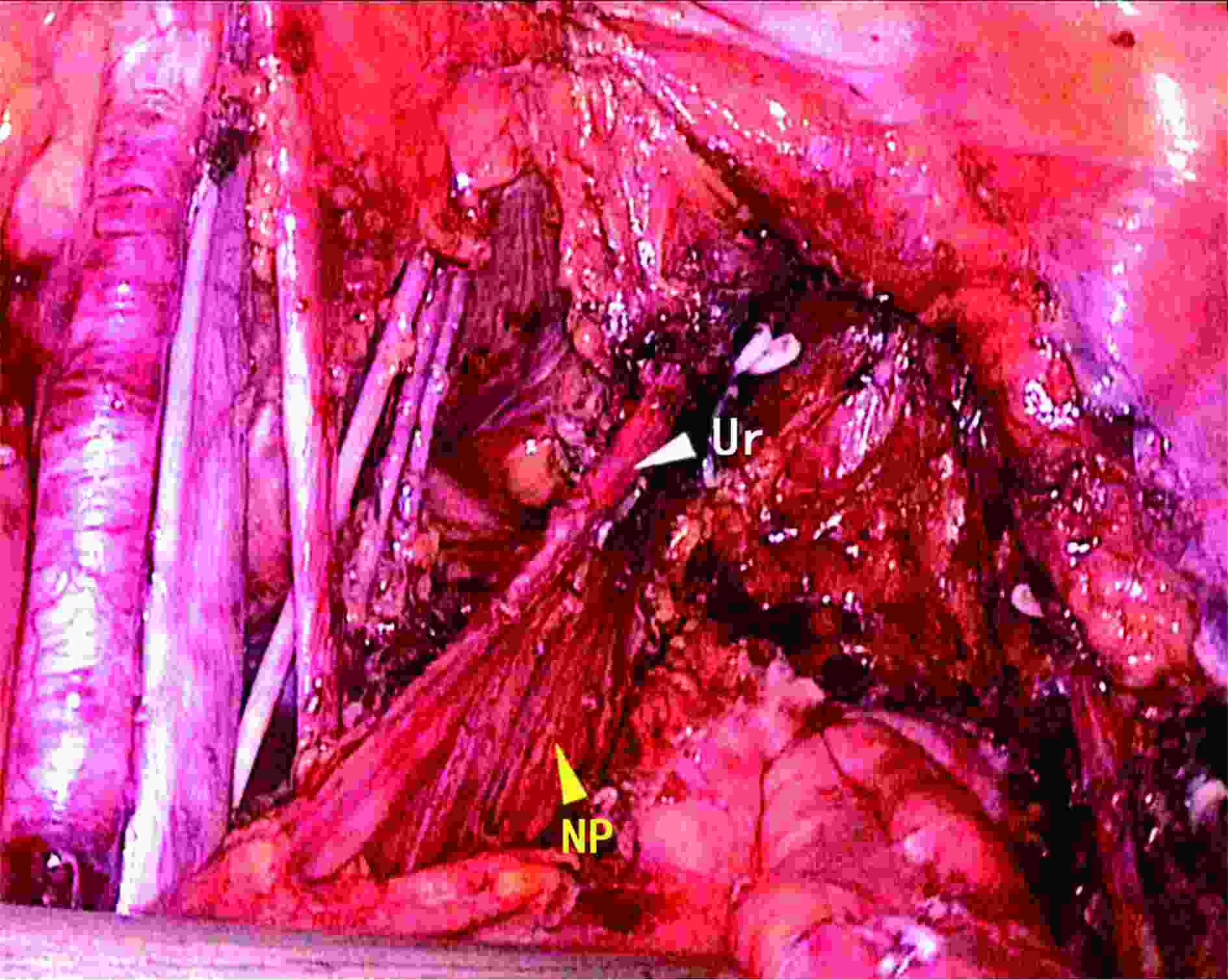
ObjectiveThe aim of this study was to investigate the feasibility of using ultrasonic scalpel combined with vascular clip in parametrial management, called limited energy parametrial resection/dissection (LEPRD), in laparoscopic nerve plane-sparing radical hysterectomy (NPSRH), a modified nerve-sparing radical hysterectomy (NSRH); and to evaluate its effectiveness in pelvic autonomic nerve preservation. MethodsFrom July 2012 to January 2016, 257 consecutive patients with stage IB1 to IIA2 cervical cancer who underwent NPSRH were included in this study. Patients were divided into three cohorts according to the different parametrial resection modality. The clinical, pathological and surgery-related parameters were compared between the three groups. Short- and long-term postoperative bladder functions were evaluated. ResultsLEPRD was attempted in 94 patients, and was successful in 65 (69.1%) patients (LEPRD group). The remaining 29 (30.9%) patients required bipolar coagulation after failure of vascular clipping (combined modality group). Routine bipolar cautery was used in the other 163 patients during the parametrial resection (bipolar group). The blood loss in the LEPRD group was significantly lower than those in the other two groups (P<0.001). The rate of successful Foley removal on postoperative day 7 was significantly higher in the LEPRD group than in the bipolar group (P=0.022). The incidence of chronic voiding dysfunction was significantly lower in the LEPRD group than in the bipolar group (P=0.019). ConclusionsIt is feasible to perform LEPRD in NPSRH for cervical cancers. This kind of limited energy surgical technique is associated with less blood loss, and leads to improved postoperative bladder function.
2018, 30(6): 656-668.
doi: 10.21147/j.issn.1000-9604.2018.06.10
Abstract:
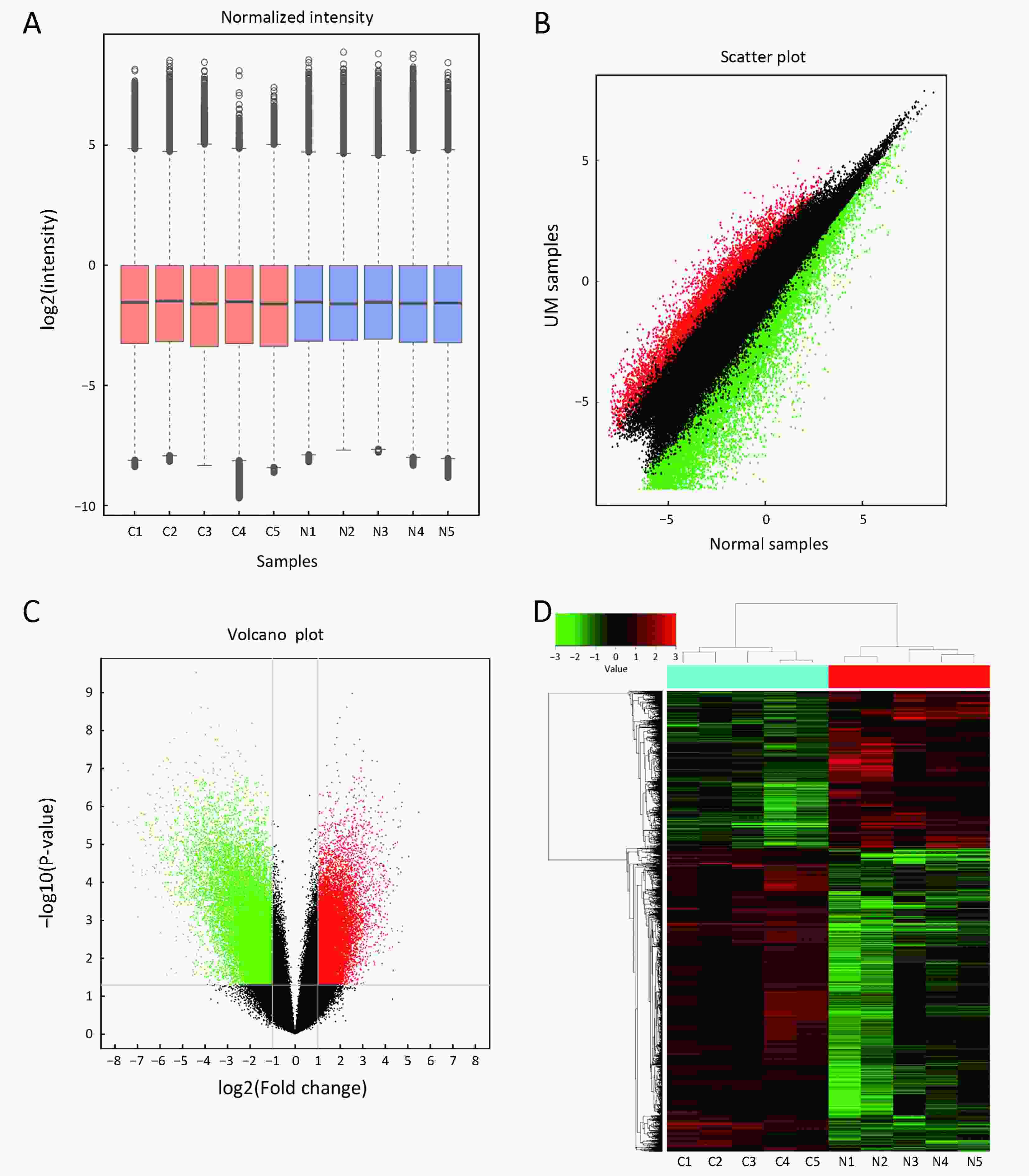
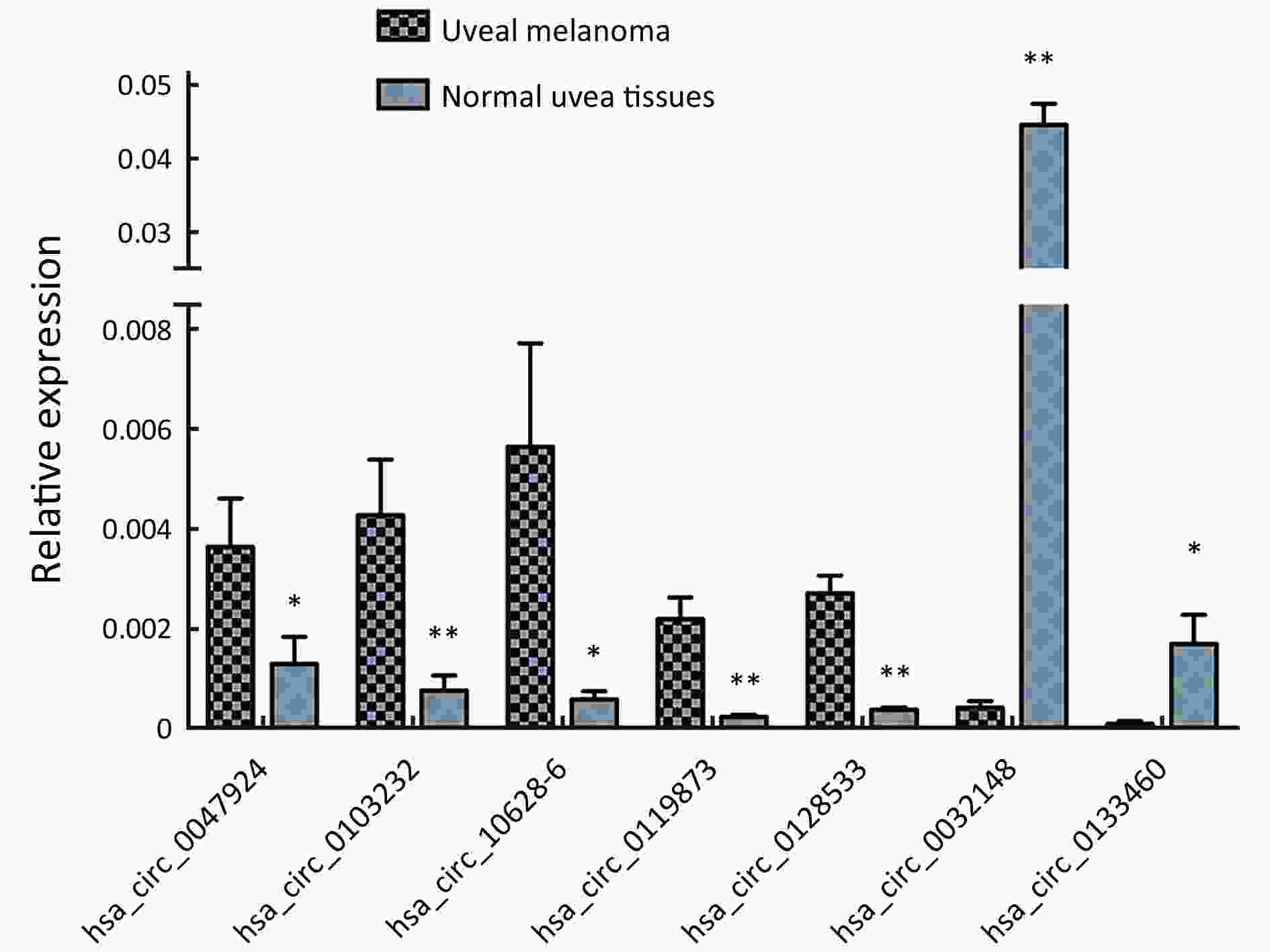
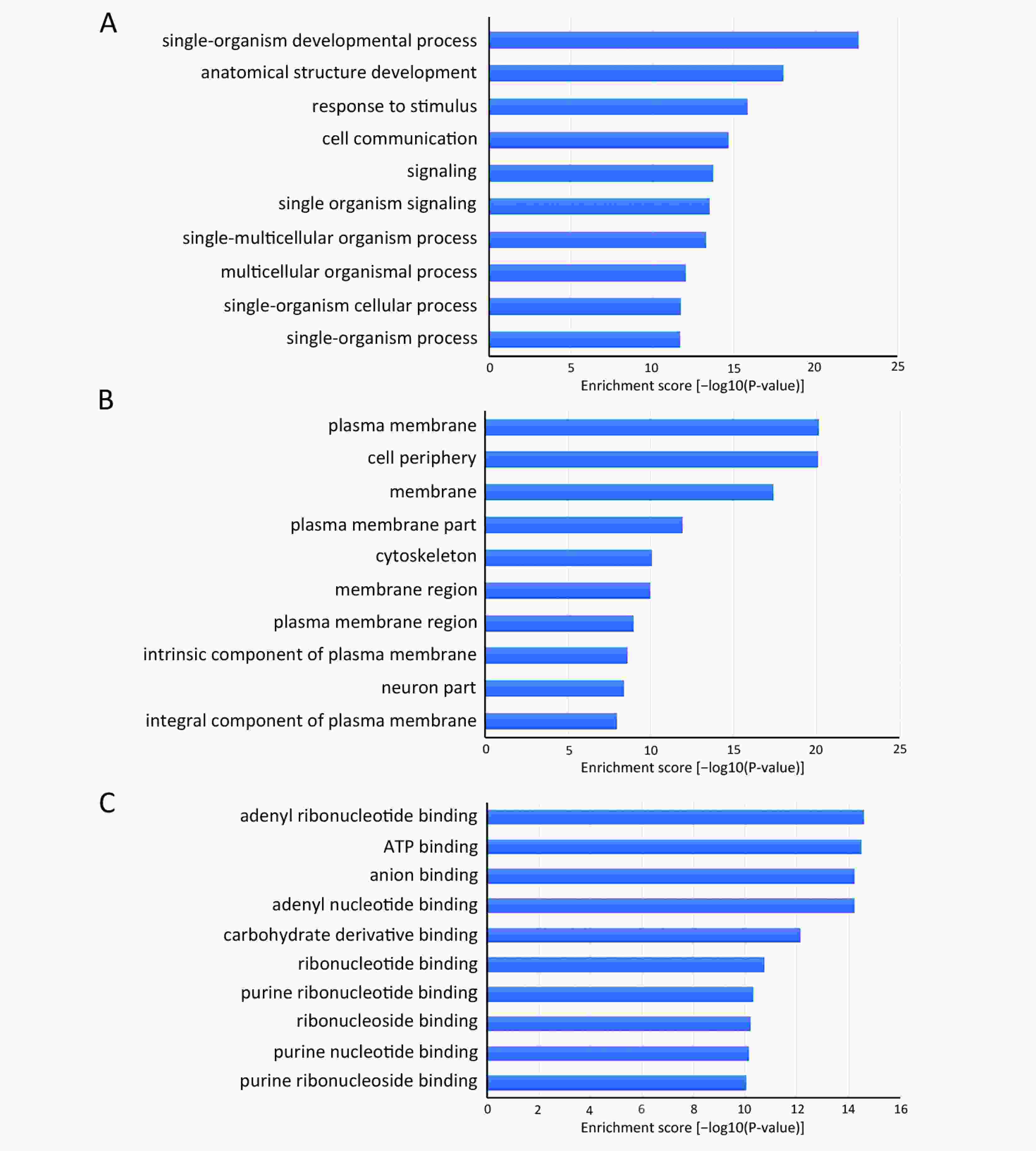
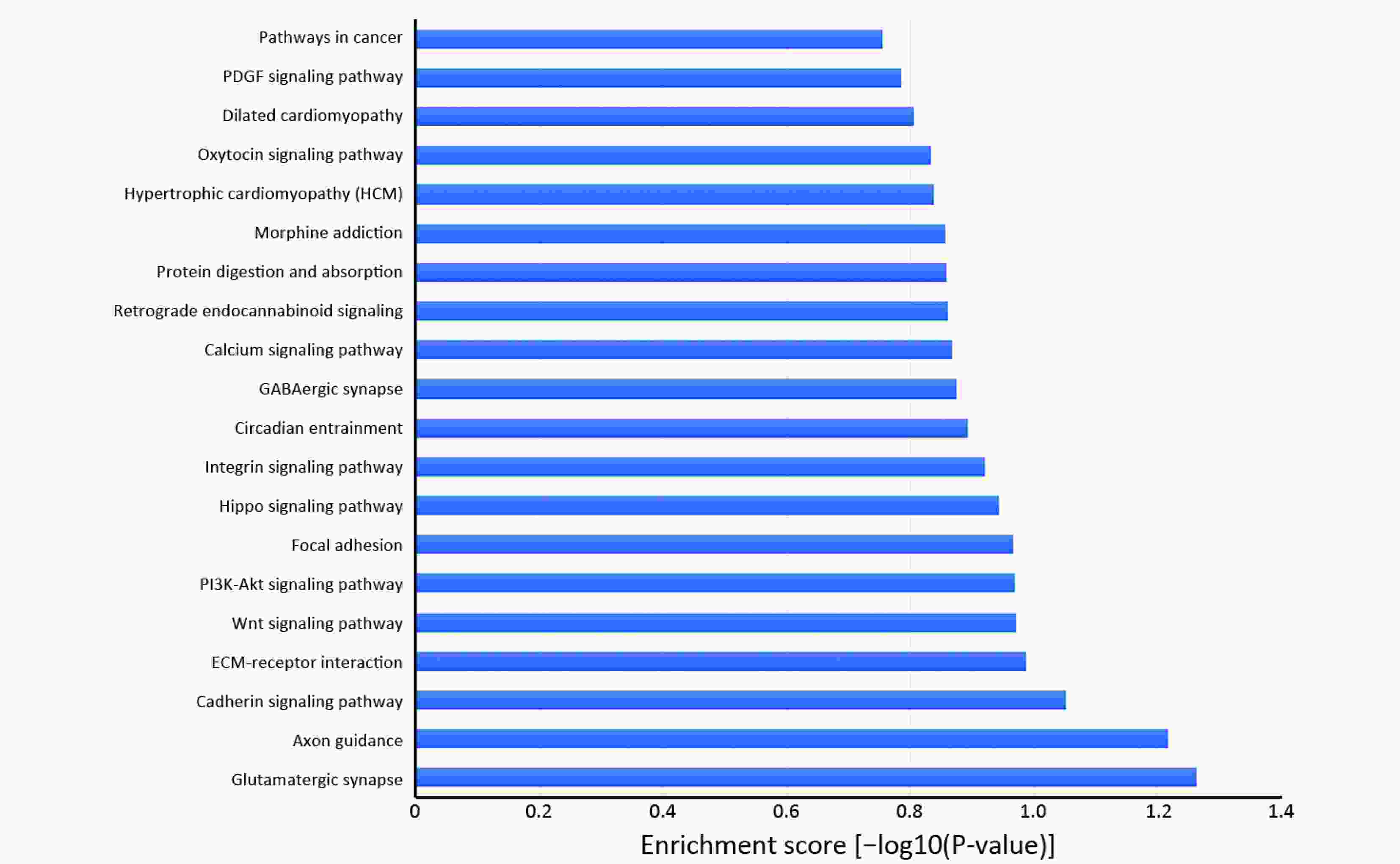
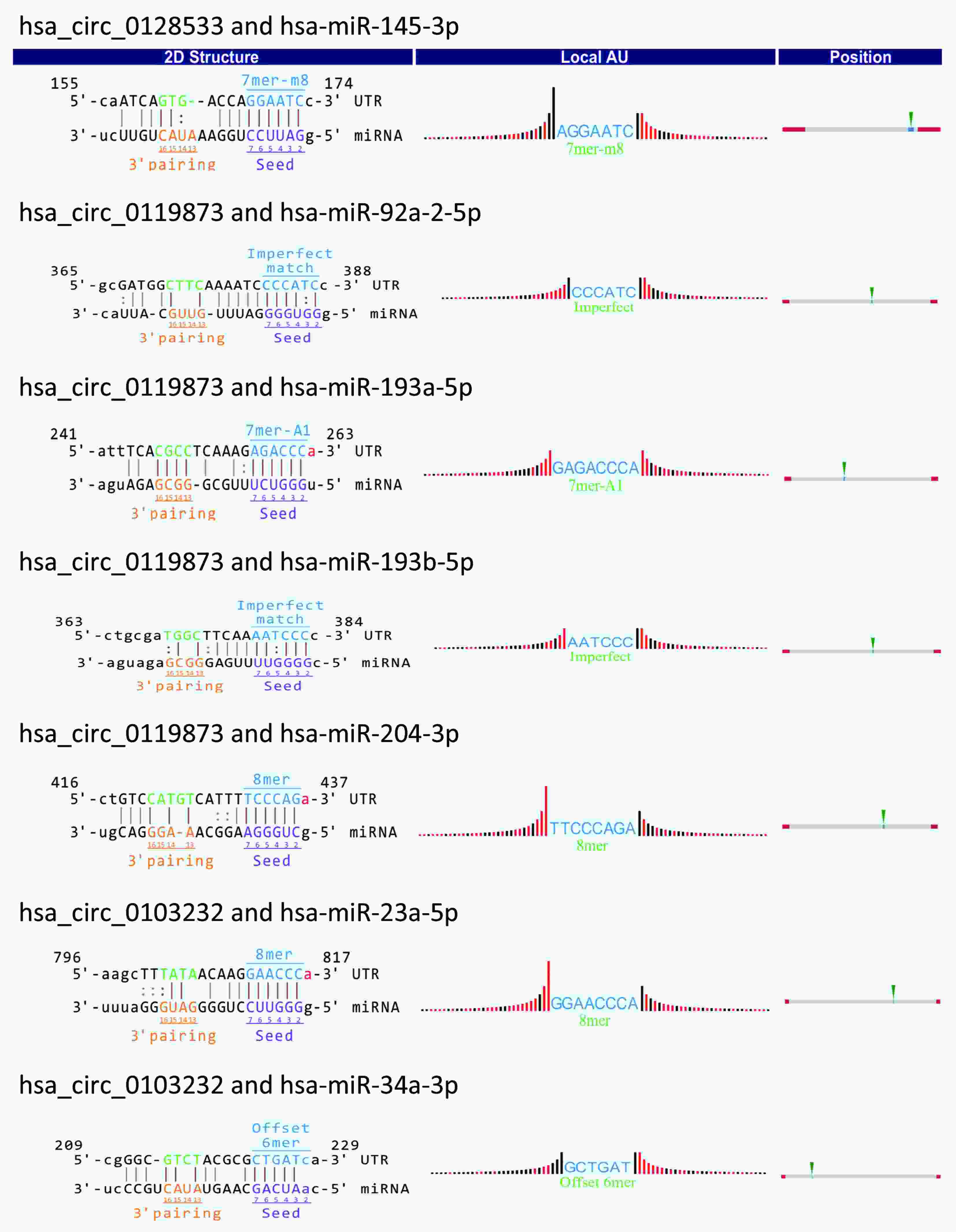
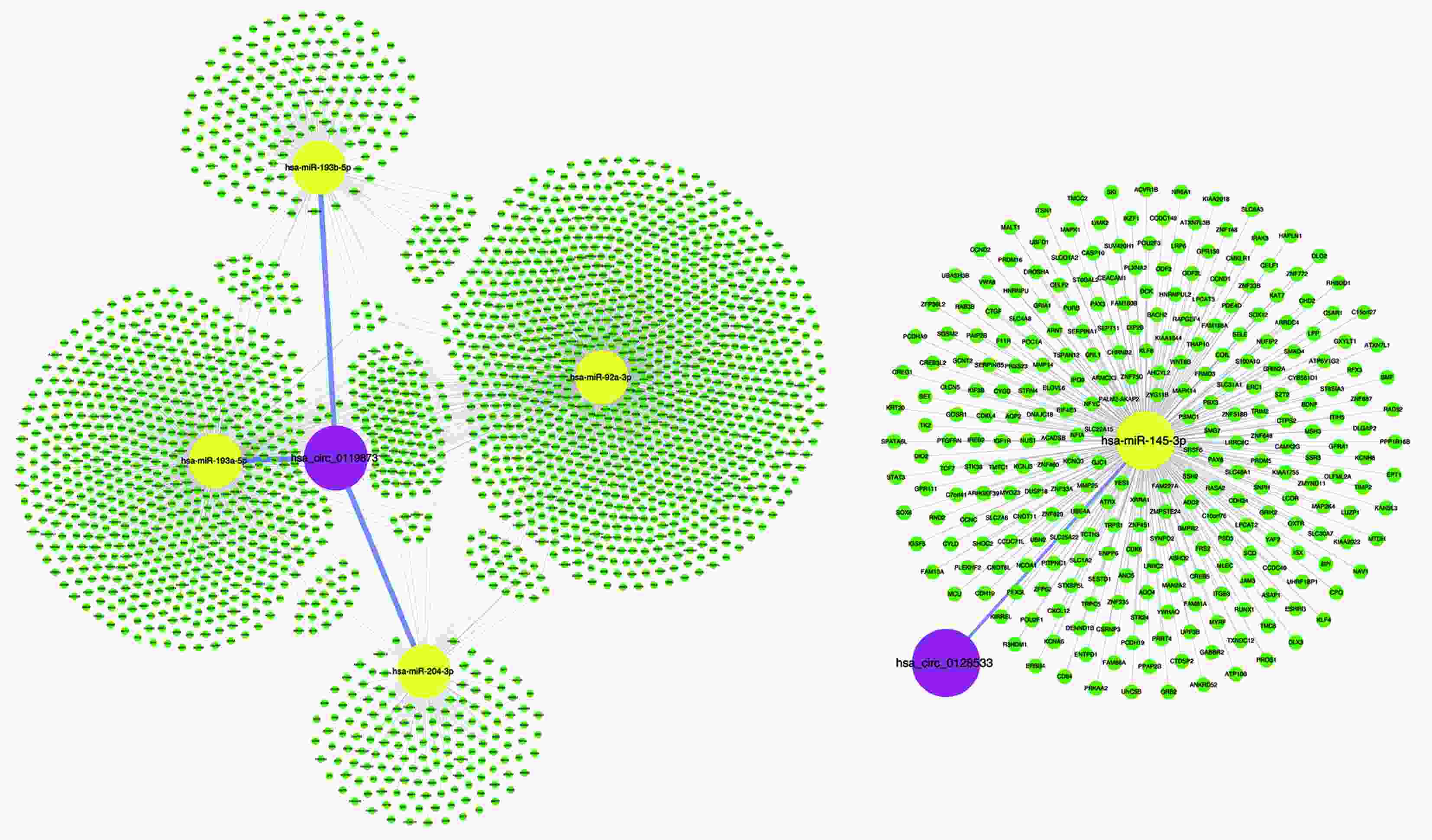
ObjectiveThe present study aimed to investigate circular RNA (circRNA) expression in uveal melanoma (UM). MethodsFirst, we used microarray to compare the expression profiles of circRNA in five UM samples and five normal uvea tissues. Next, bioinformatics analyses, including gene ontology (GO) analysis and pathway analysis, were applied to study these differentially expressed circRNAs to predict pathogenic pathways that may be involved. Quantitative real-time polymerase chain reaction (qRT-PCR) in 20 UM samples and 20 normal uvea samples was used to confirm the circRNA expression profiles obtained from the microarray data. Finally, we analyzed the interaction between validated circRNAs and their potential cancer-associated miRNA targets. ResultsIn total, 50,579 circRNAs [fold change (FC) ≥2.0; P<0.05], including 20,654 up-regulated and 29,925 down-regulated circRNAs, were identified as differentially expressed between UM tissues and normal uvea tissues. We used qRT-PCR to verify seven dysregulated circRNAs indicated by the microarray data, including hsa_circ_0119873, hsa_circ_0128533, hsa_circ_0047924, hsa_circ_0103232, hsa-circRNA10628-6, hsa_circ_0032148 and hsa_circ_0133460, which may be promising candidates to study future molecular mechanisms. ConclusionsThis study explored, for the first time, the abnormal expression of circRNAs in UM and described the expression profile of circRNAs, providing a new potential target for the mechanism of UM and future treatment of UM.
2018, 30(6): 669-676.
doi: 10.21147/j.issn.1000-9604.2018.06.11
Abstract:
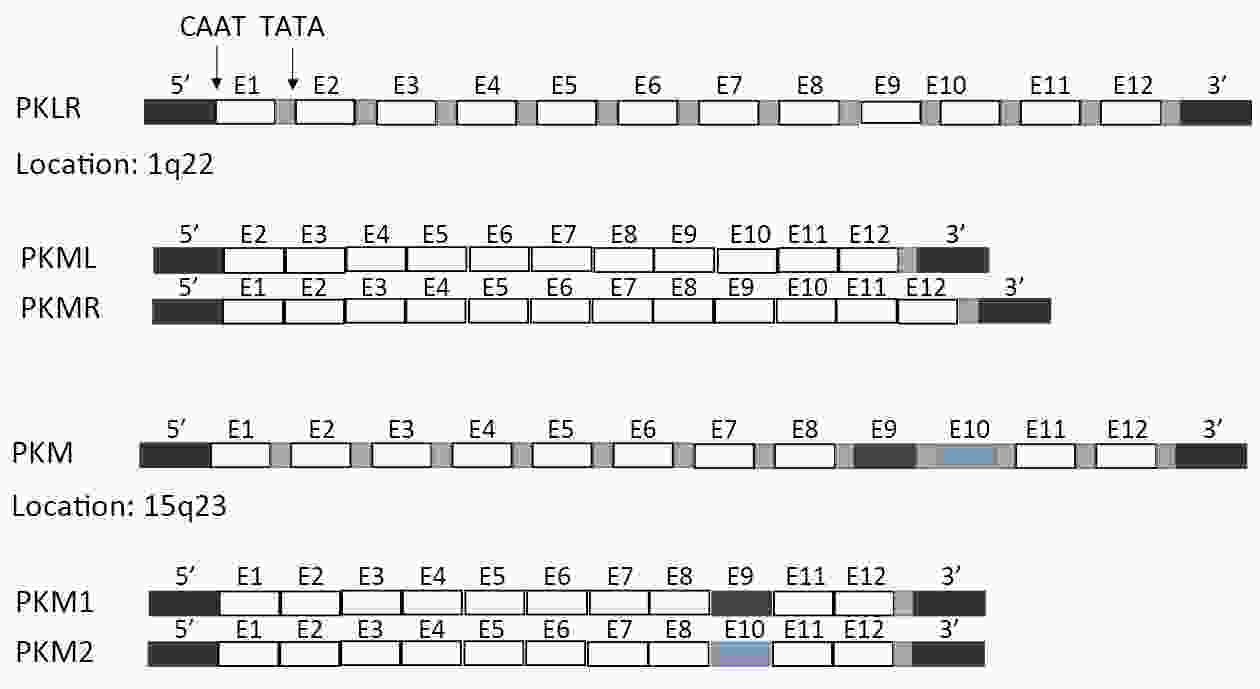
Gastrointestinal (GI) cancer is one of the most common causes of cancer-related deaths worldwide. Tumor markers are valuable in detecting post-surgical recurrence or in monitoring response to chemotherapy. Pyruvate kinase isoform M2 (PKM2), a glycolytic enzyme catalyzing conversion of phosphoenolpyruvate (PEP) to pyruvate, confers a growth advantage to the tumor cells and enables them to adapt to the tumor microenvironment. In this review, we have summarized current research on the expression and regulation of PKM2 in tumor cells, and its potential role in GI carcinogenesis and progression. Furthermore, we have also discussed the potential of PKM2 as a diagnostic and screening marker, and a therapeutic target in GI cancer.
Gastrointestinal (GI) cancer is one of the most common causes of cancer-related deaths worldwide. Tumor markers are valuable in detecting post-surgical recurrence or in monitoring response to chemotherapy. Pyruvate kinase isoform M2 (PKM2), a glycolytic enzyme catalyzing conversion of phosphoenolpyruvate (PEP) to pyruvate, confers a growth advantage to the tumor cells and enables them to adapt to the tumor microenvironment. In this review, we have summarized current research on the expression and regulation of PKM2 in tumor cells, and its potential role in GI carcinogenesis and progression. Furthermore, we have also discussed the potential of PKM2 as a diagnostic and screening marker, and a therapeutic target in GI cancer.

 Abstract
Abstract FullText HTML
FullText HTML PDF 1546KB
PDF 1546KB