2019 Vol.31(1)
Display Mode: |
2019, 31(1): 1-28.
doi: 10.21147/j.issn.1000-9604.2019.01.01
Abstract:
2019, 31(1): 29-48.
doi: 10.21147/j.issn.1000-9604.2019.01.02
Abstract:
2019, 31(1): 49-66.
doi: 10.21147/j.issn.1000-9604.2019.01.03
Abstract:
2019, 31(1): 67-83.
doi: 10.21147/j.issn.1000-9604.2019.01.04
Abstract:
2019, 31(1): 84-98.
doi: 10.21147/j.issn.1000-9604.2019.01.05
Abstract:
2019, 31(1): 117-134.
doi: 10.21147/j.issn.1000-9604.2019.01.07
Abstract:
2019, 31(1): 135-143.
doi: 10.21147/j.issn.1000-9604.2019.01.08
Abstract:
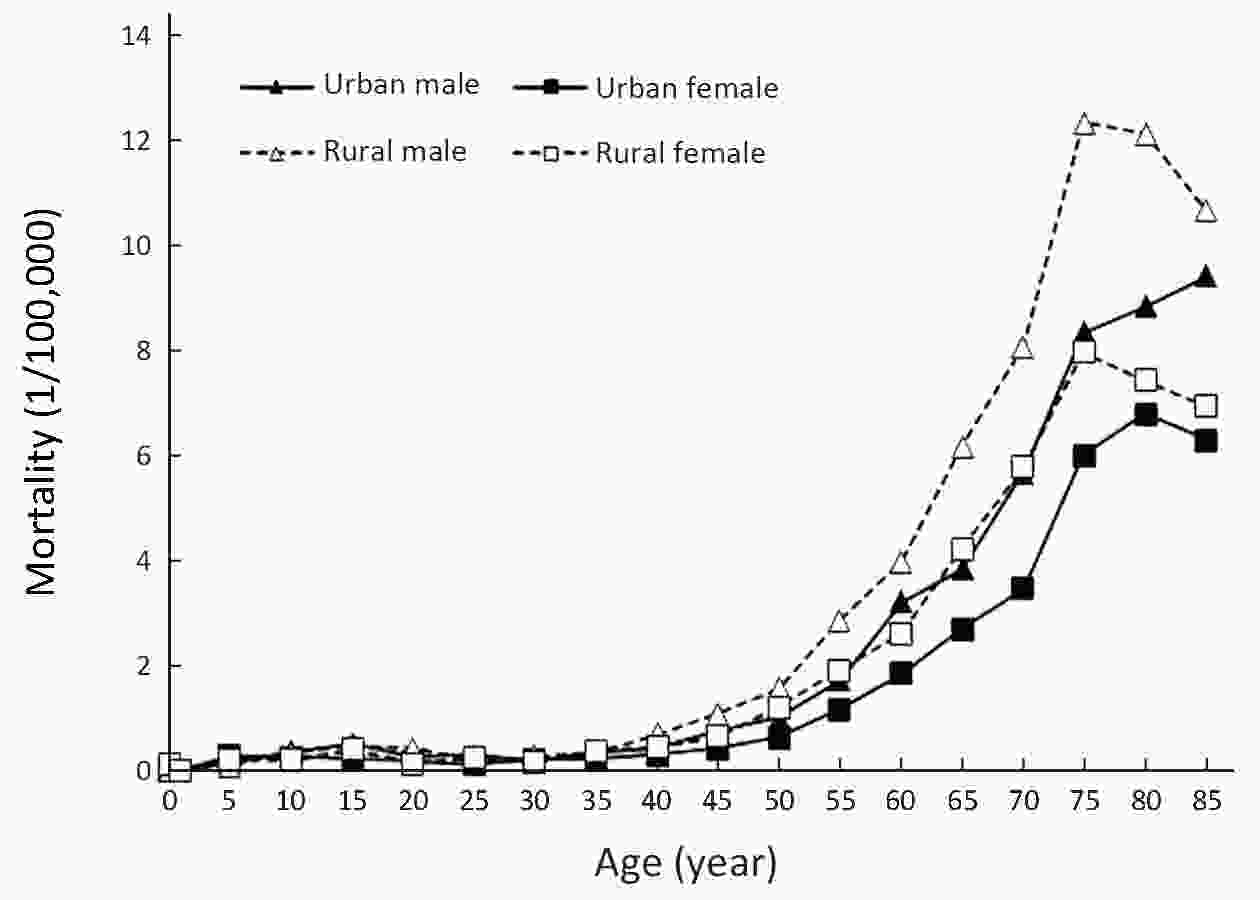
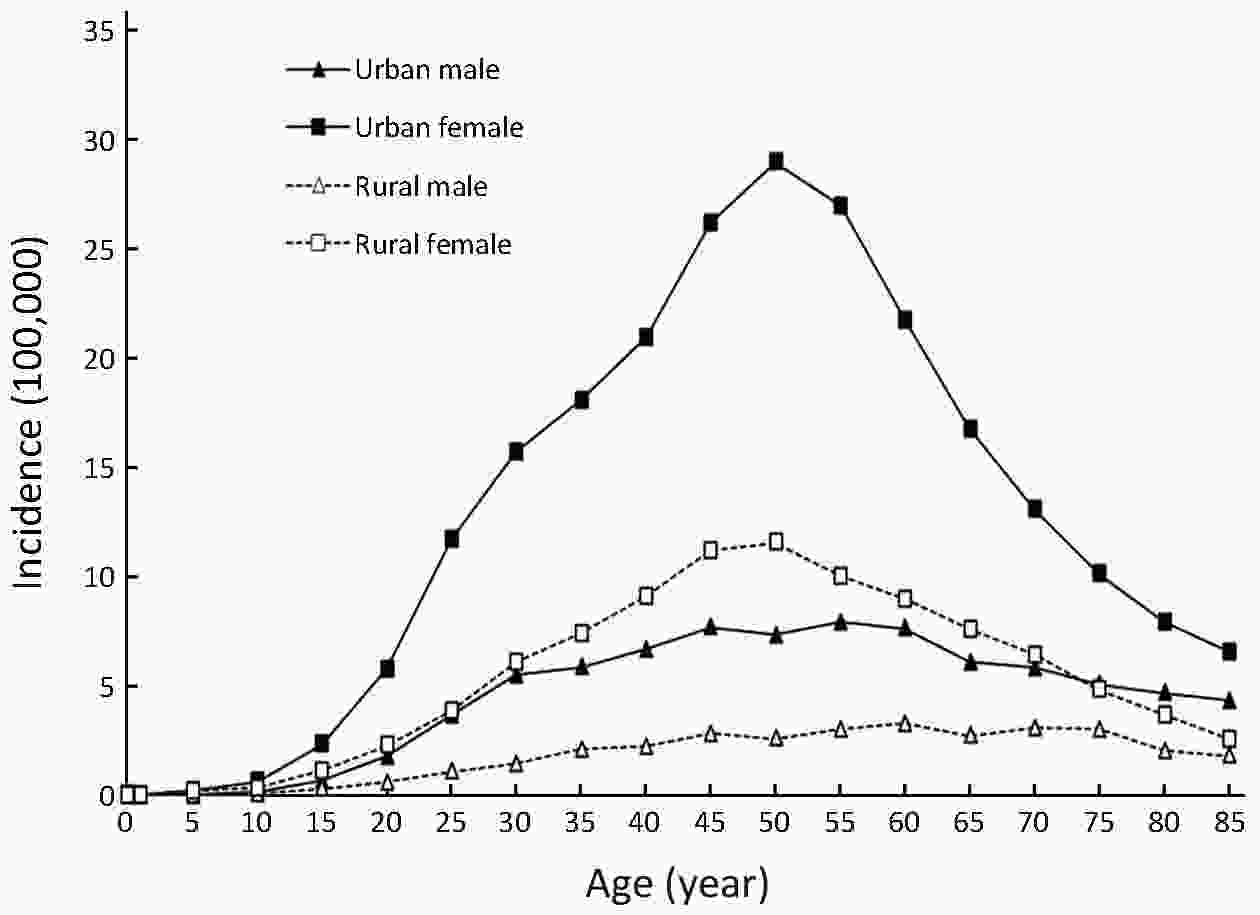
ObjectiveIn this study, we aimed to estimate the updated incidence and mortality of primary bone cancers based on population-based cancer registration data in 2014, collected by the National Central Cancer Registry of China (NCCRC). MethodsIn 2017, 339 registries’ data were qualified based on data quality criteria set down by the NCCRC. Cases of primary bone cancers were retrieved from the national database. We estimated numbers of primary bone cancer cases and deaths in China using age-specific rates and corresponding national population stratified by area, sex, age-group (0, 1−4, 5−9, 10−14, …, 85+). Chinese standard population in 2000 and Segi’s World population were applied for the calculation of age-standardized incidence and mortality rates. ResultsIn 2014, 24,000 primary bone cancer cases and 17,200 deaths attributable to primary bone cancers were estimated to have occurred in China. The crude incidence rate of primary bone cancers was 1.76/100,000, with age-standardized incidence rate by Chinese standard population (ASIRC) and by World standard population (ASIRW) being 1.35/100,000 and 1.32/100,000, respectively. The crude mortality rate of primary bone cancers was 1.26/100,000, with age-standardized mortality rate by Chinese standard population (ASMRC) and by World standard population (ASMRW) being 0.88/100,000 and 0.86/100,000, respectively. Age-specific incidence curve was bimodally distributed with age, with the first peak occurring in the second decade of the life and the second peak in the elderly. Males had higher crude and age-standardized rates for both incidence and mortality compared with females. Both crude and age-standardized incidence rates were higher in rural areas than in urban areas, so were the crude and age-standardized mortality rates. ConclusionsThis population-based study presents the most recently available estimates on primary bone cancers in China, revealing that the males are 1.34 times as much as females suffering from primary bone cancers and the adolescents in puberty and the elderly are predominantly affected groups by these cancers. High-quality cancer registration data are a prerequisite for undertaking further study for gaining insight into the causes and risk factors for primary bone cancers in China.
2019, 31(1): 144-151.
doi: 10.21147/j.issn.1000-9604.2019.01.09
Abstract:
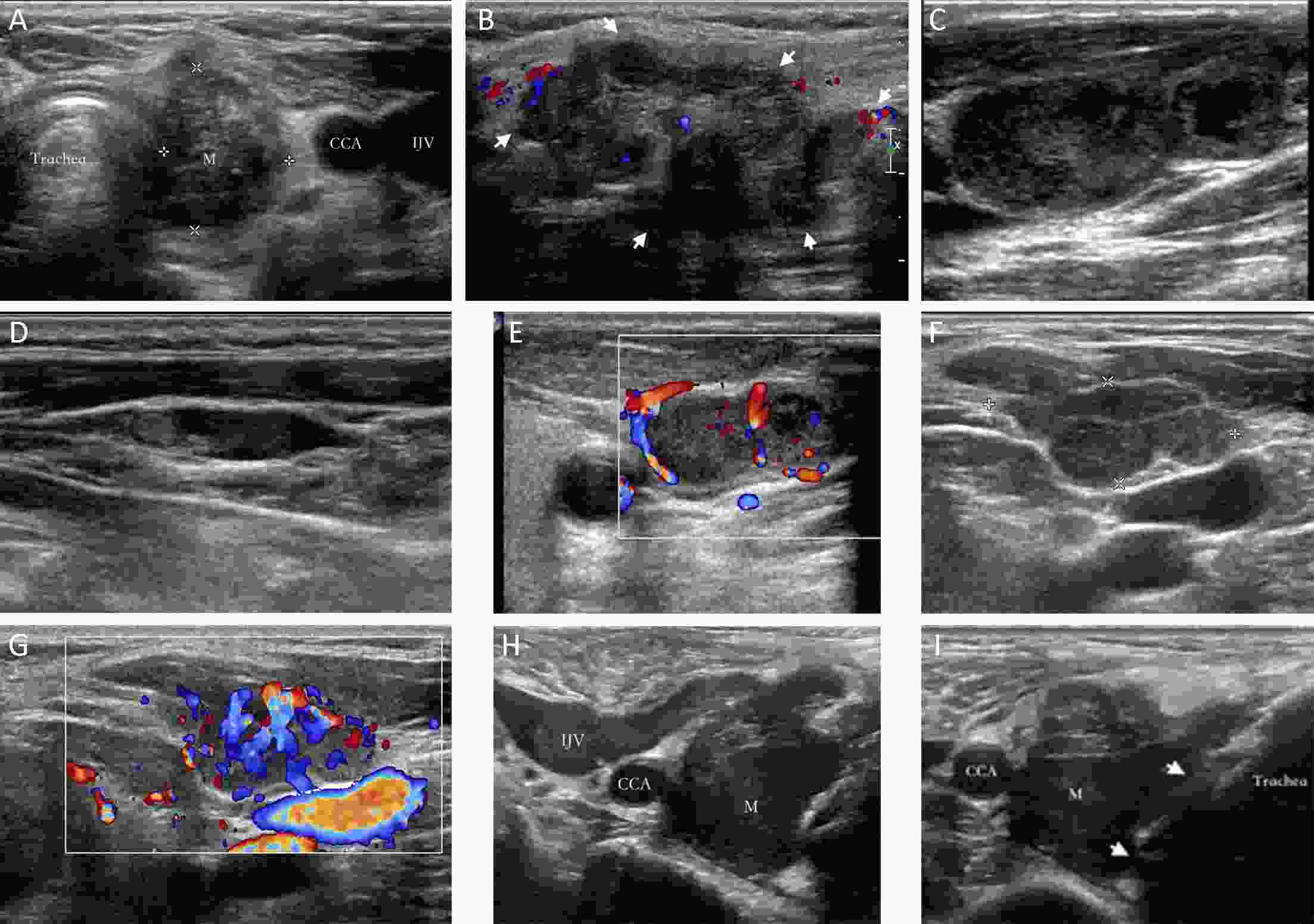
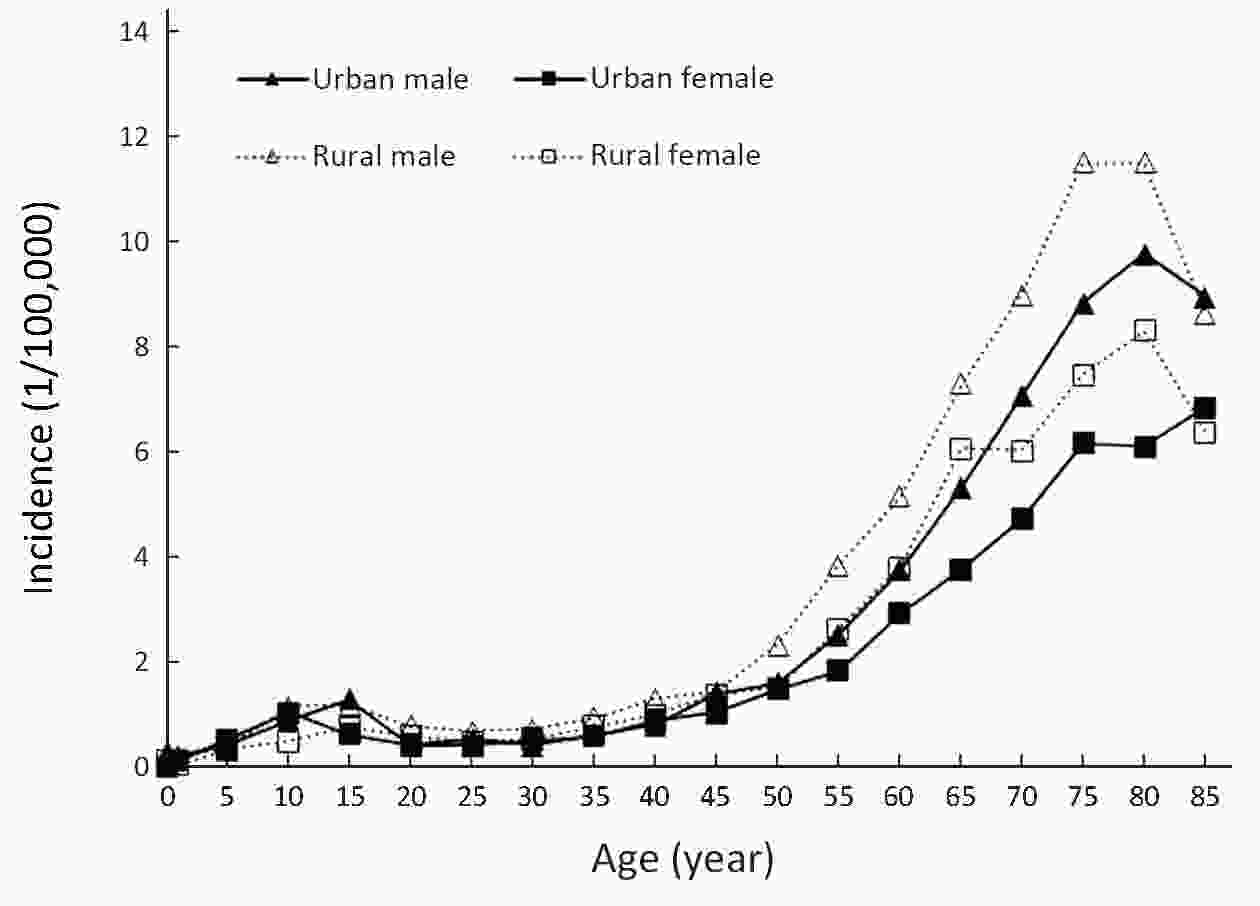
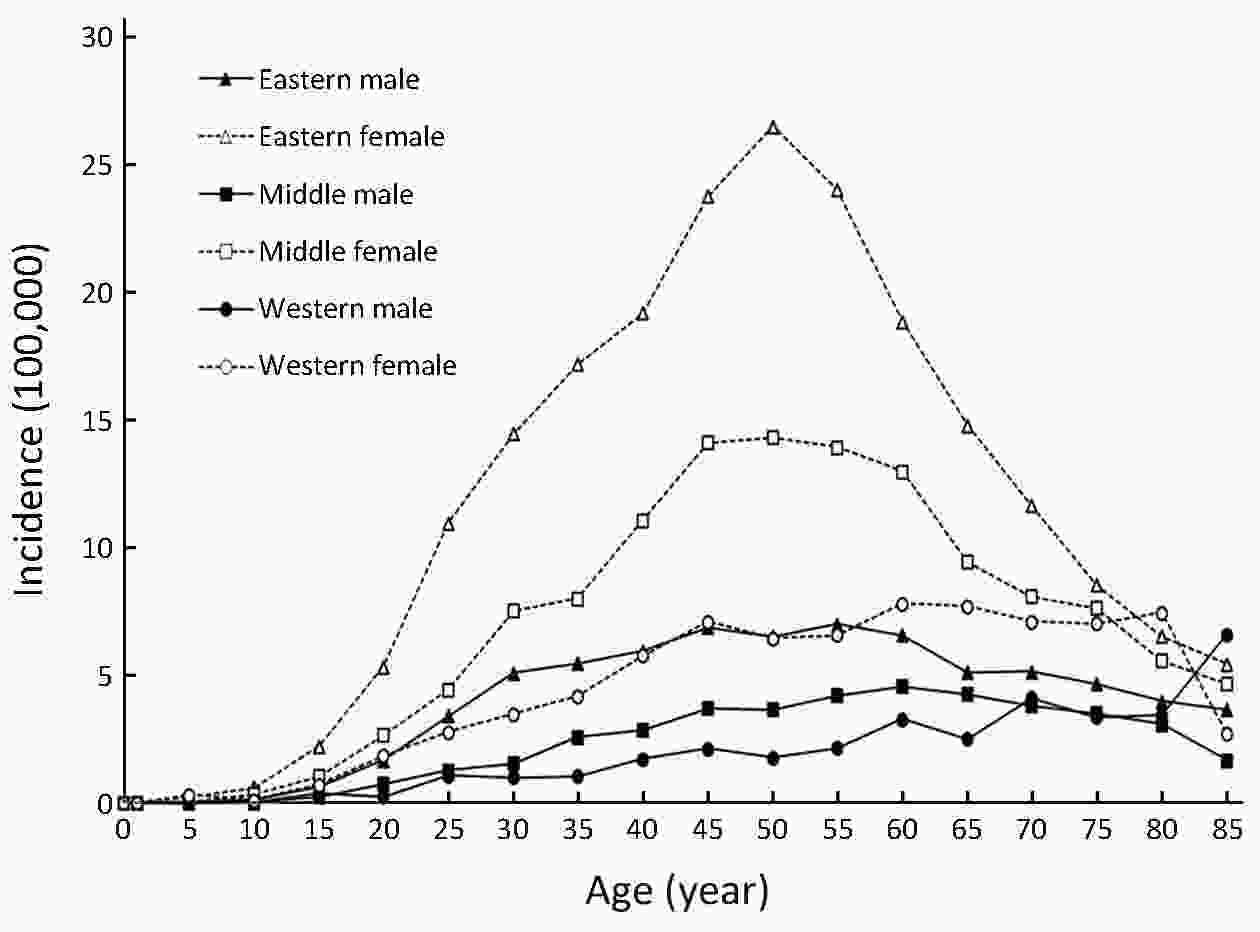
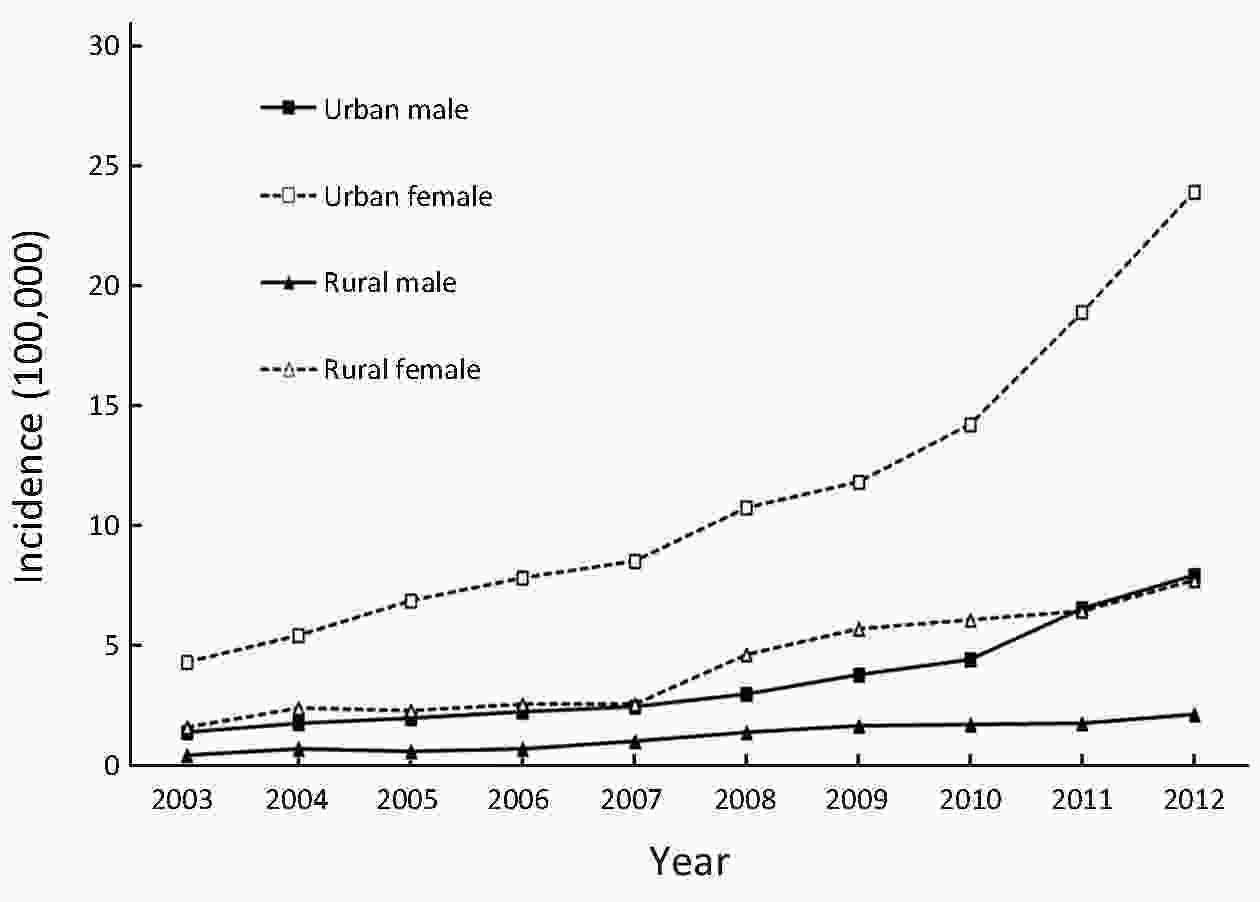
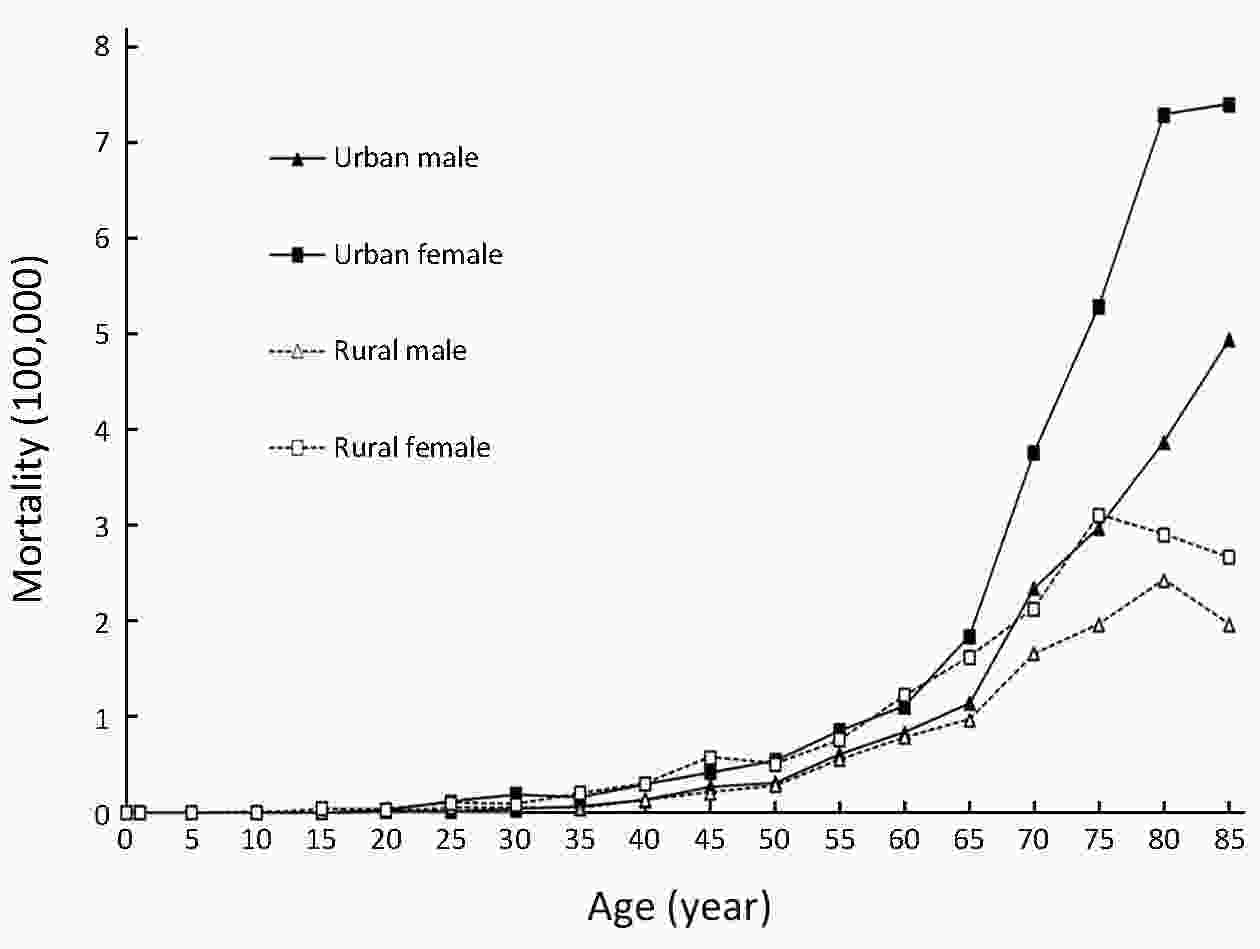
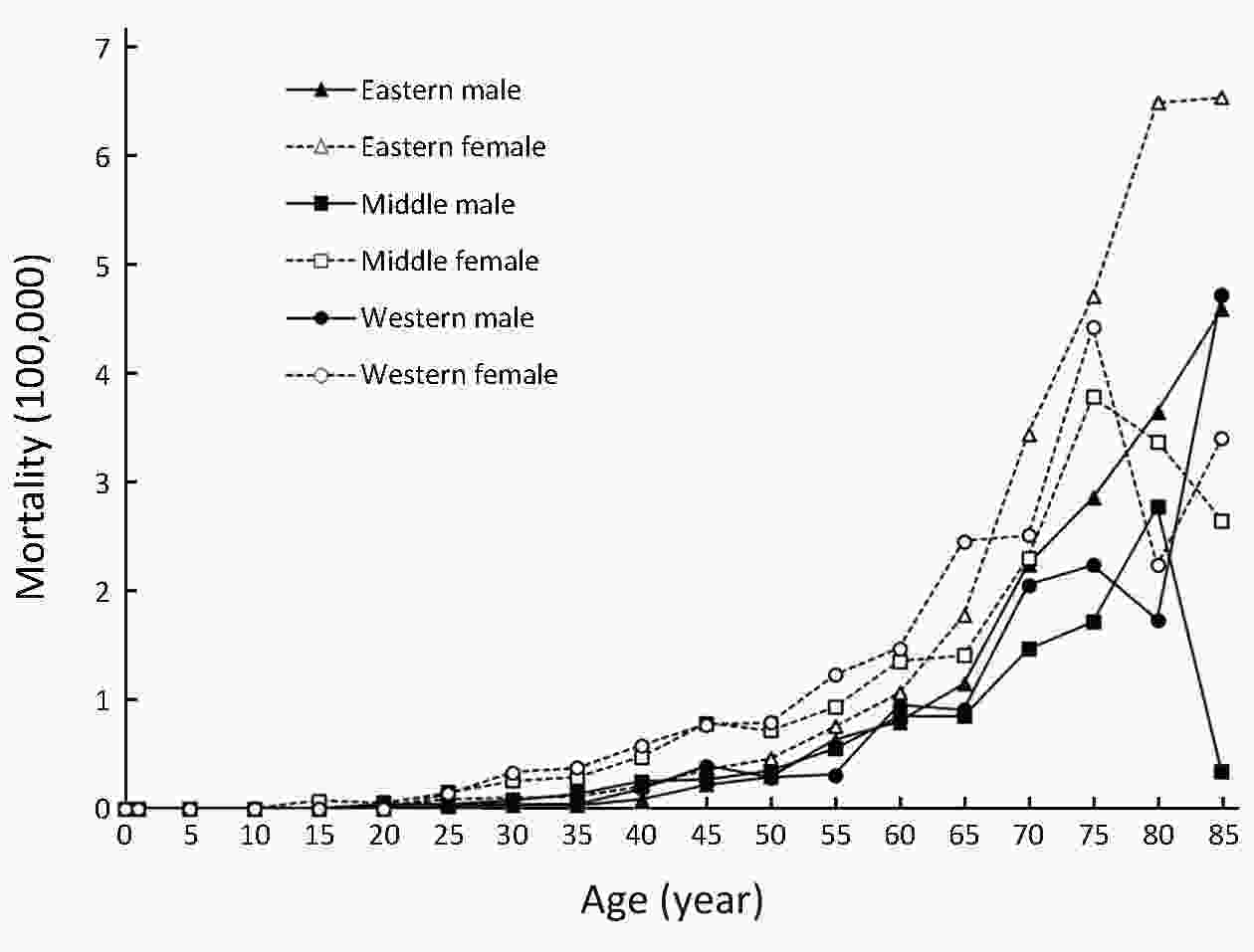
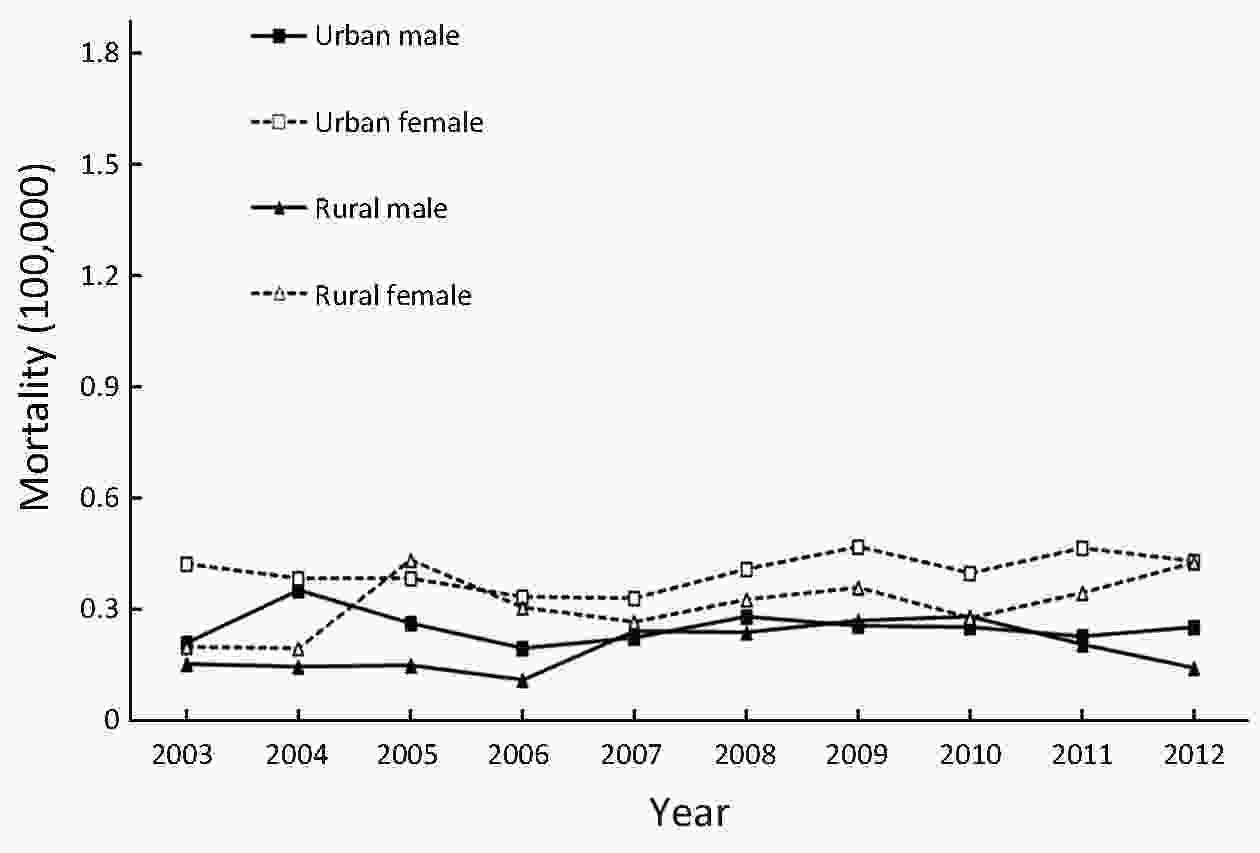
ObjectiveTo analyze the incidence and mortality rates of thyroid cancer (TC) in China from 2008 to 2012. MethodsIncident and death cases of TC were retrieved from the National Central Cancer Registry (NCCR) database collecting from 135 cancer registries in China during 2008−2012. The crude incidence and mortality rates of TC were calculated by area (urban/rural), region (eastern, middle, western), gender and age group (0, 1−4, 5−9, …, 85+). China census in 2000 and world Segi’s population were applied for age-standardized rates. Joinpoint (Version 4.6.0.0) model was used for time-trend analysis. ResultsThe crude incidence rate of TC was 7.56/100,000 which ranked the seventh in overall cancers. The age-standardized incidence rates by China population (ASIRC) and by World population (ASIRW) were 6.25/100,000 and 5.52/100,000, respectively. The crude mortality of TC in China was 0.52/100,000. The age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 0.34/100,000 and 0.32/100,000, respectively. Incidence and mortality rates of TC were higher in females than in males and higher in urban areas than in rural areas. Eastern areas had the highest incidence followed by middle and western areas. TC incidence increased dramatically after age of 15 years, then peaked at 14.08/100,000 in the group of 50−54 years and finally decreased sharply after 55 years old. TC mortality increased with age in population, reaching the peak of 5.09/100,000 in sub-population aged 85 years or older. TC incidence increased by 4.73 times from 2.40/100,000 in 2003 to 13.75/100,000 in 2012 with an average annual increase of 20%, while TC mortality only increased slightly around 0.32/100,000 from 0.26/100,000 to 0.36/100,000. ConclusionsAppropriate targeted prevention, early detection and treatment programs can be carried out to curb the rapid growth trend of TC and control the disease burden.
2019, 31(1): 152-161.
doi: 10.21147/j.issn.1000-9604.2019.01.10
Abstract:
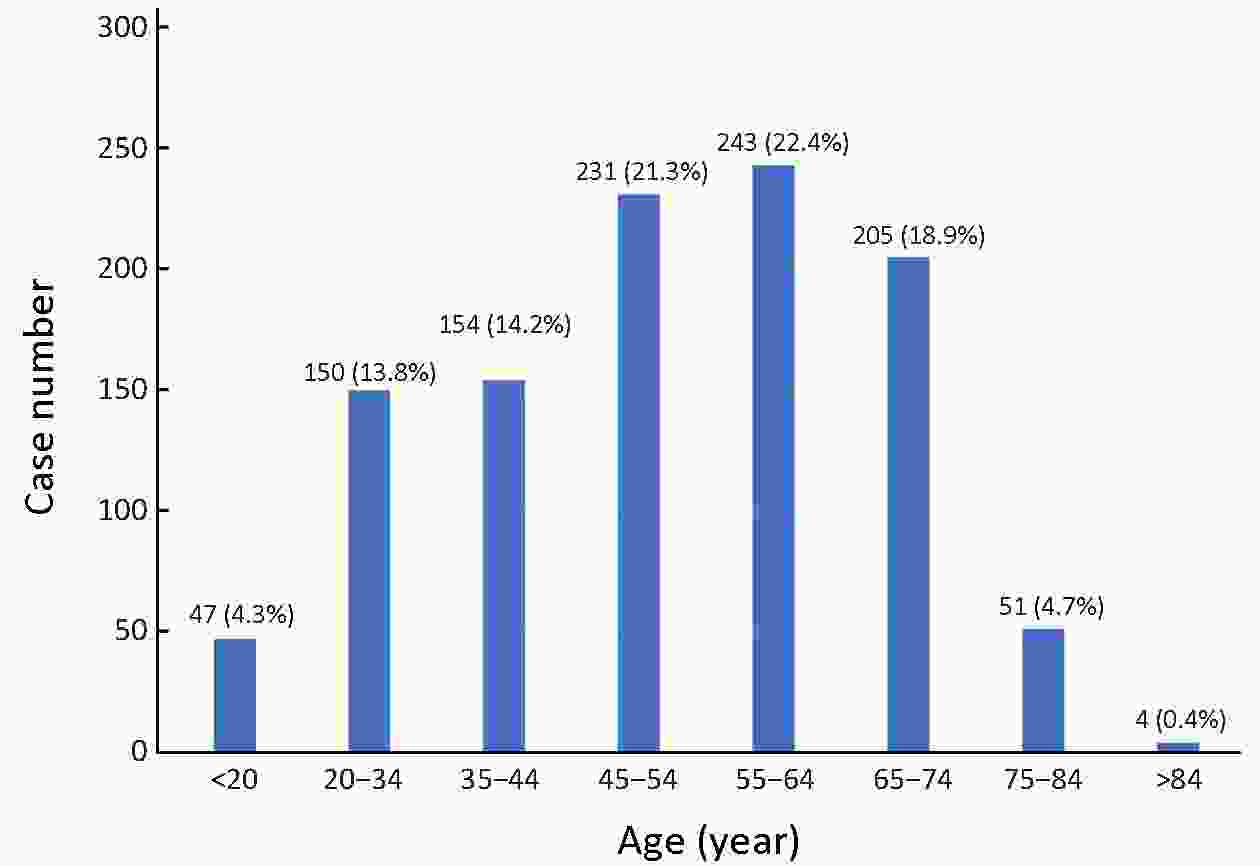
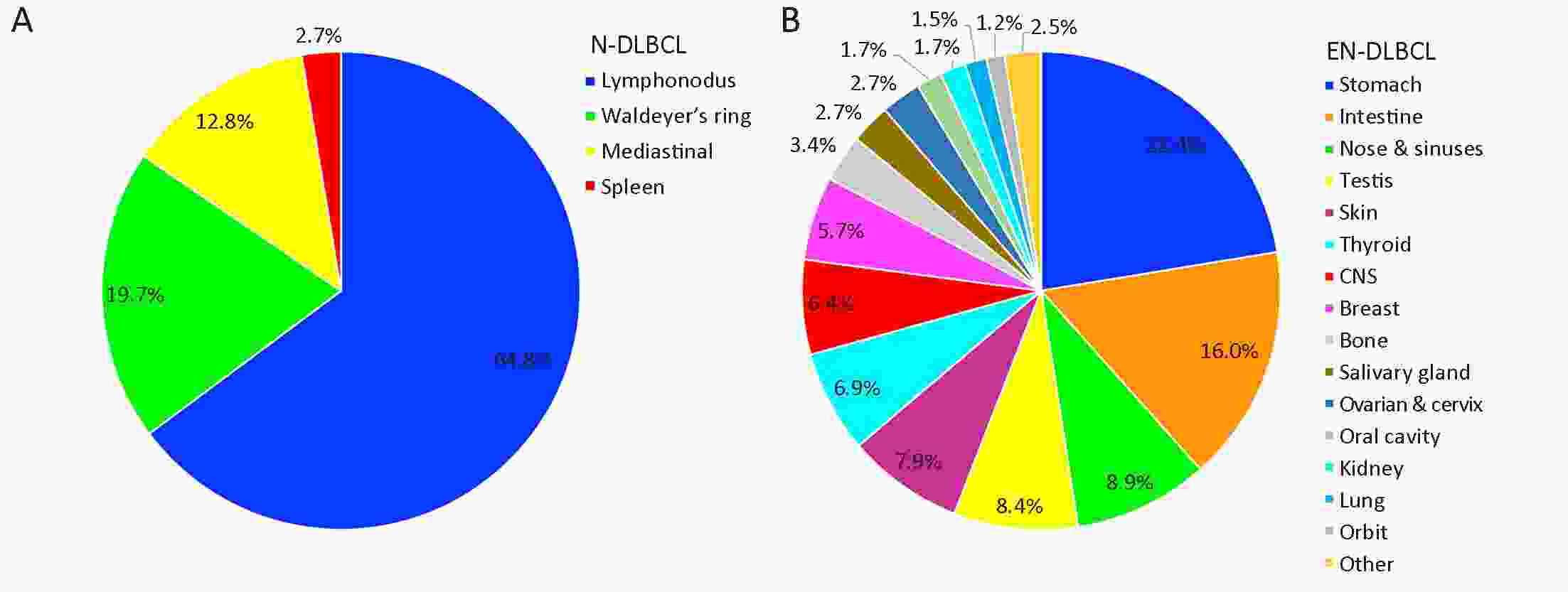
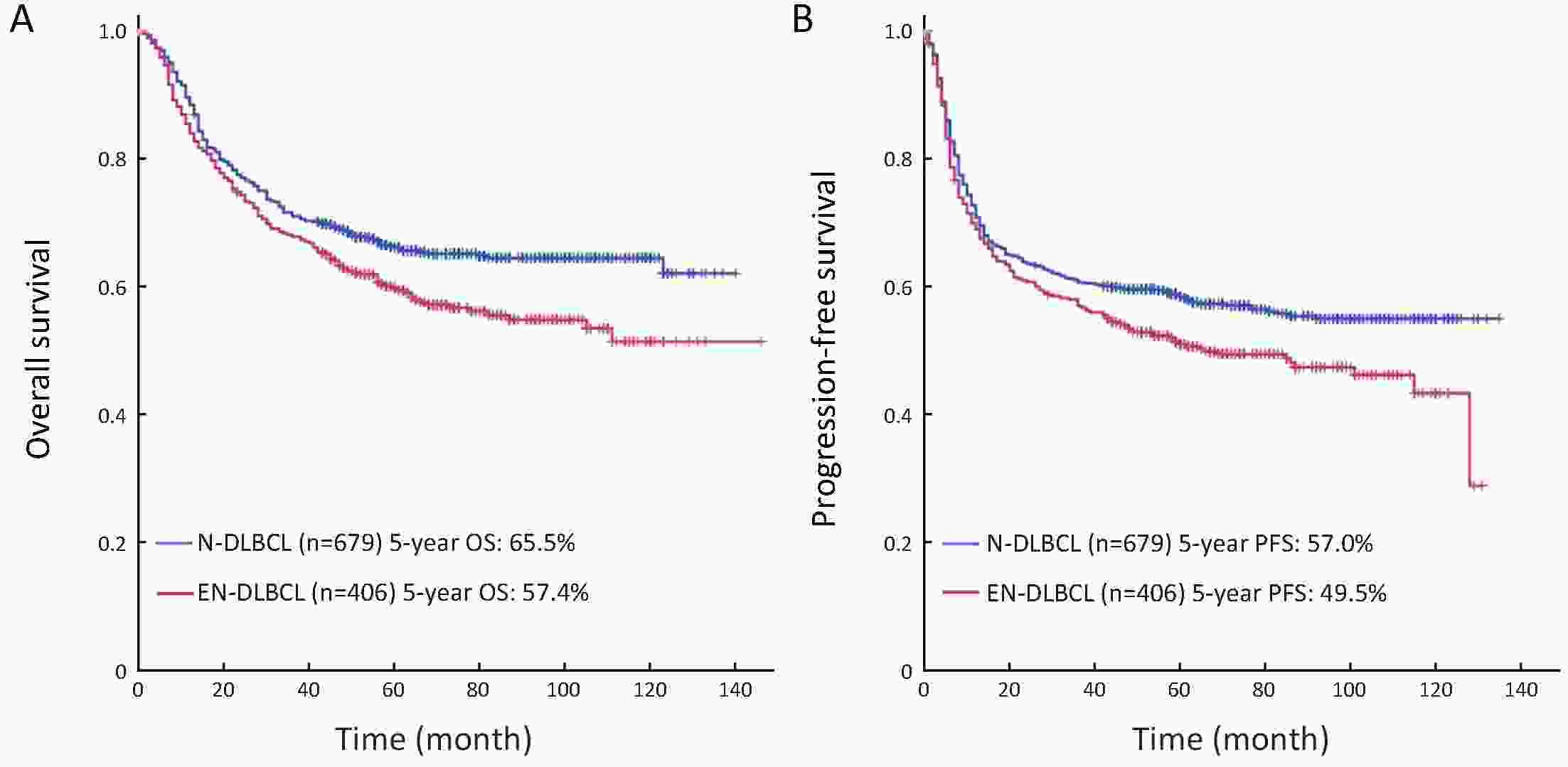
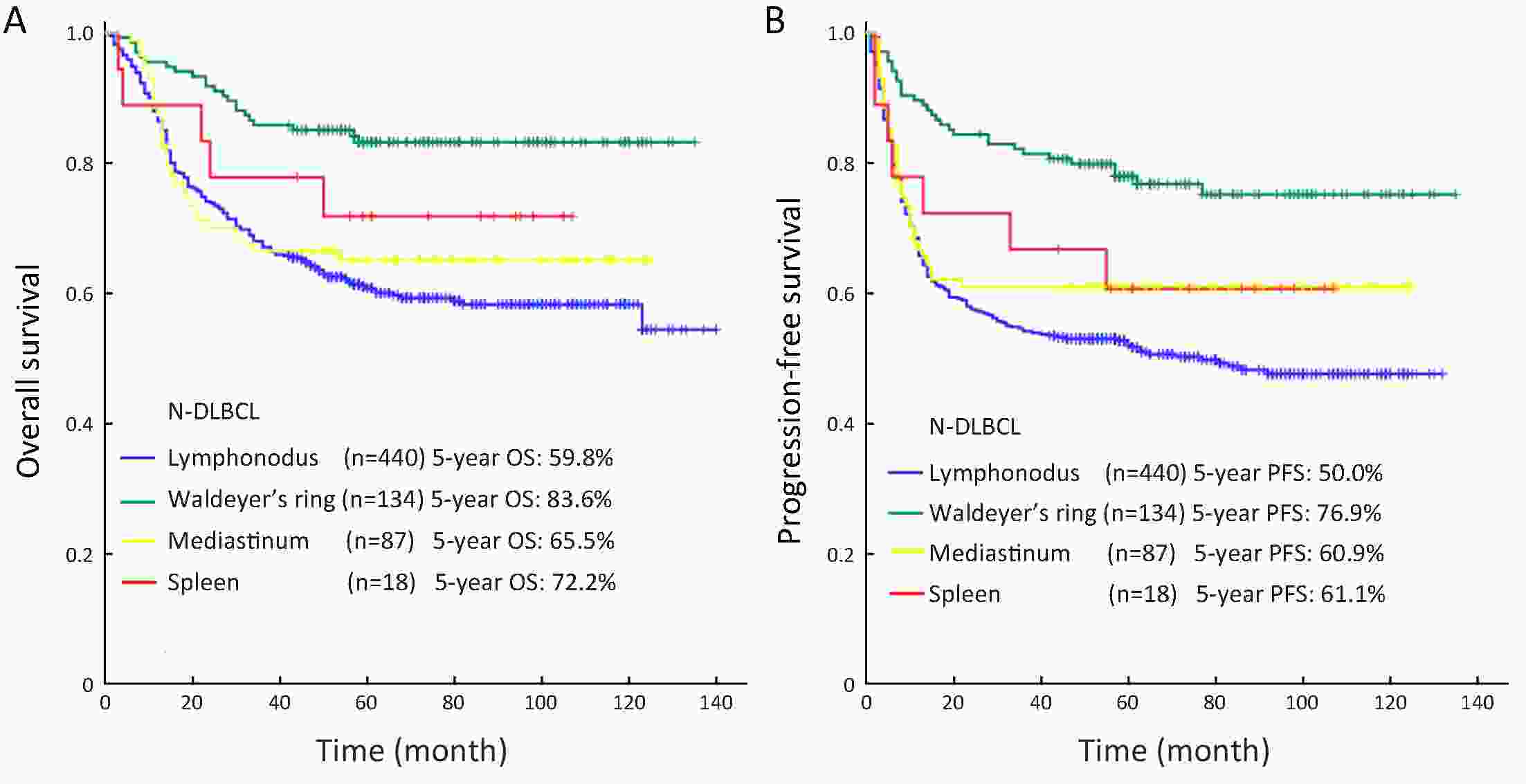
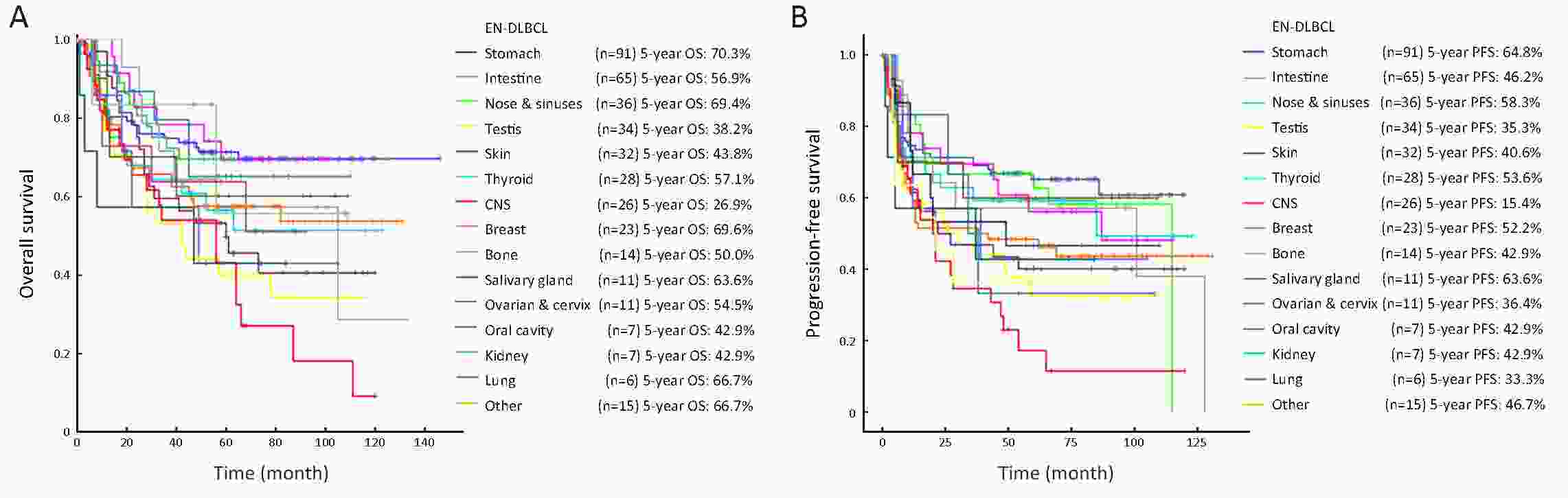
ObjectiveTo explore the clinicobiologic features and outcomes of diffuse large B-cell lymphoma (DLBCL) patients in China according to the primary site. MethodsA total of 1,085 patients diagnosed with DLBCL in National Cancer Center/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College during a 6-year period were enrolled. Their clinical characteristics and outcomes were analyzed according to the primary site. ResultsIn the 1,085 patients, 679 (62.6%) cases were nodal DLBCL (N-DLBCL) and 406 cases (37.4%) were extranodal DLBCL (EN-DLBCL). The most common sites of N-DLBCL were lymphonodus (64.8%), Waldeyer’s ring (19.7%), mediastinum (12.8%) and spleen (2.7%), while in EN-DLBCL, stomach (22.4%), intestine (16.0%), nose and sinuses (8.9%), testis (8.4%), skin (7.9%), thyroid (6.9%), central nervous system (CNS) (6.4%), breast (5.7%), bone (3.4%), and salivary gland (2.7%) were most common. N-DLBCL patients tend to present B symptoms, bulky disease, and elevated LDH more often, while age >60 years, extranodal sites >1, Ann Arbor stage I or II, bone marrow involvement, and Ki-67 index >90% were usually seen in EN-DLBCL. The 5-year overall survival (OS) rate and progression-free survival (PFS) rate for all patients were 62.5% and 54.2%. The 5-year OS rate for patients with N-DLBCL and EN-DLBCL were 65.5% and 56.9% (P=0.008), and the 5-year PFS were 57.0% and 49.0% (P=0.020). Waldeyer’s ring originated DLBCL possessed the highest 5-year OS rate (83.6%) and PFS rate (76.9%) in N-DLBCL. The top five EN-DLBCL subtypes with favorable prognosis were stomach, breast, nose and sinuses, lung, salivary gland, with 5-year OS rate: 70.3%, 69.6%, 69.4%, 66.7% and 63.6%, respectively. While CNS, testis, oral cavity and kidney originated EN-DLBCL faced miserable prognosis, with 5-year OS rate of 26.9%, 38.2%, and 42.9%. ConclusionsIn our study, primary sites were associated with clinical characteristics and outcomes. Compared with EN-DLBCL, N-DLBCL had better prognosis.
2019, 31(1): 162-170.
doi: 10.21147/j.issn.1000-9604.2019.01.11
Abstract:
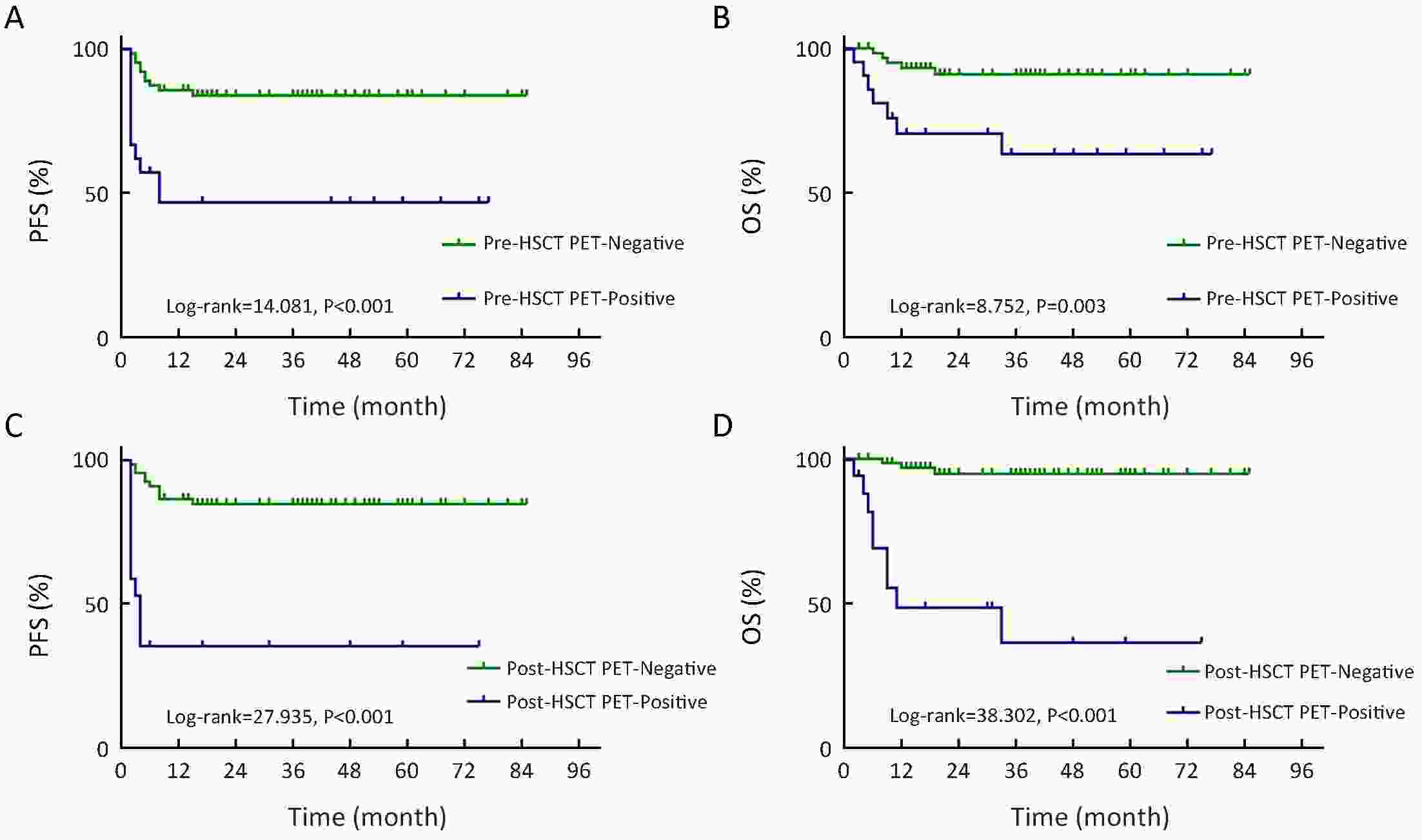
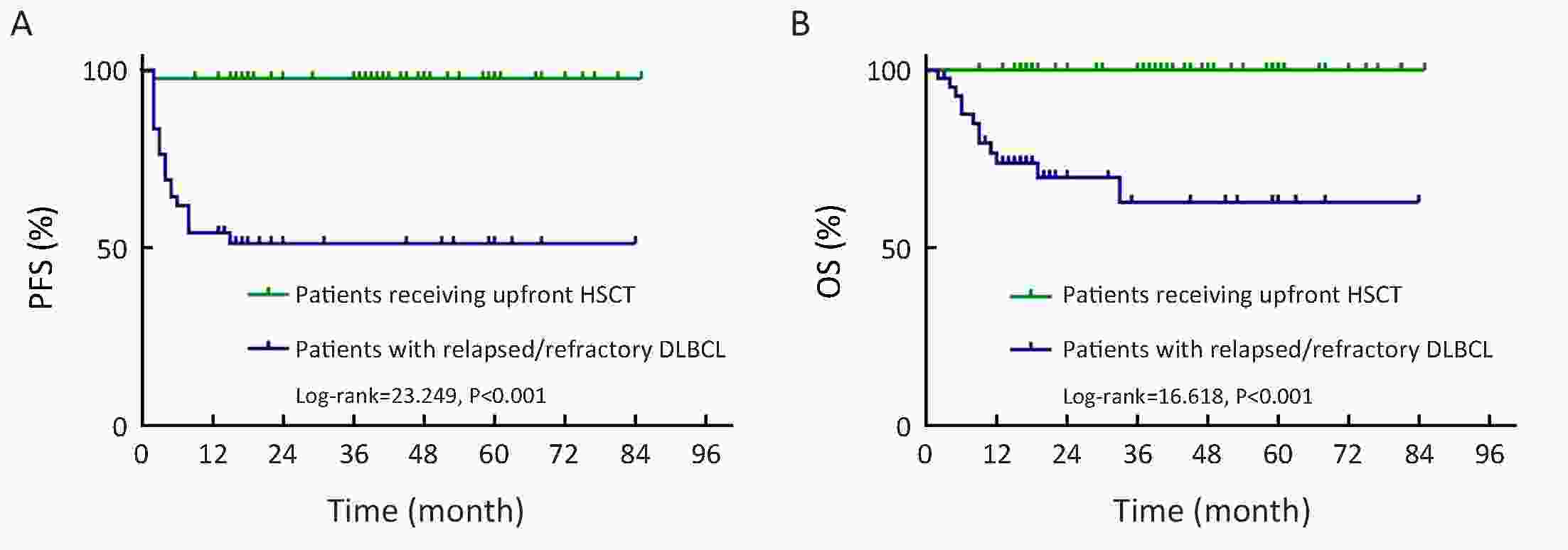
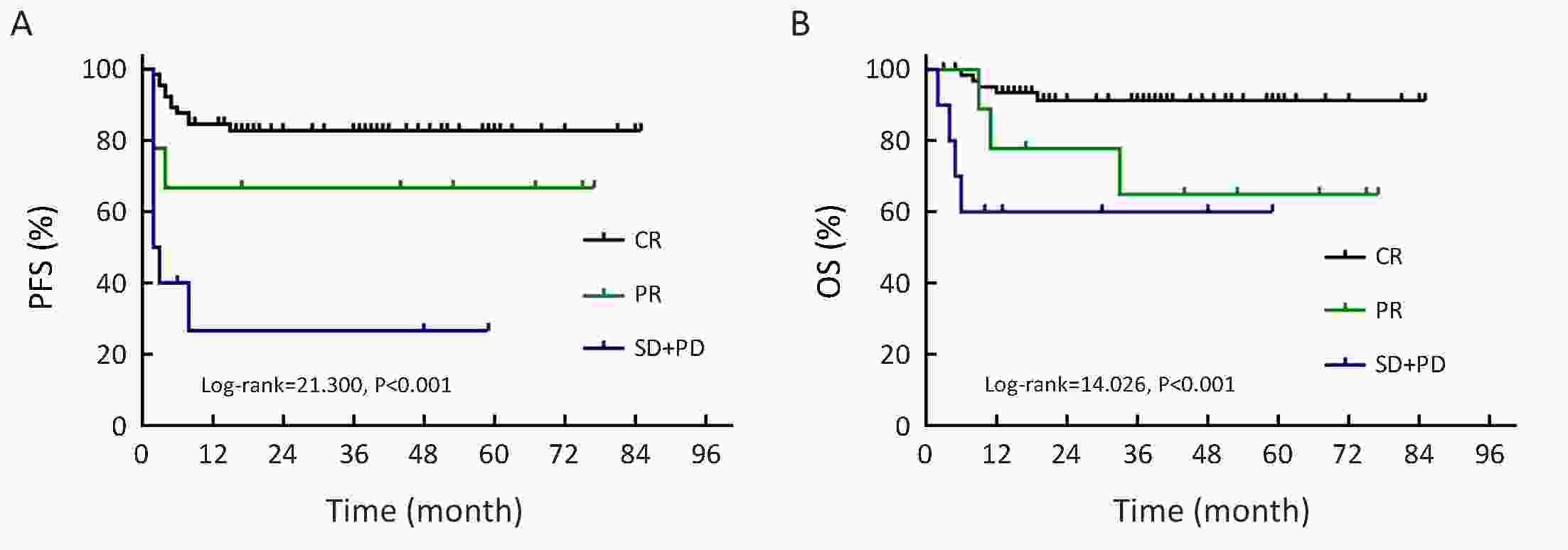
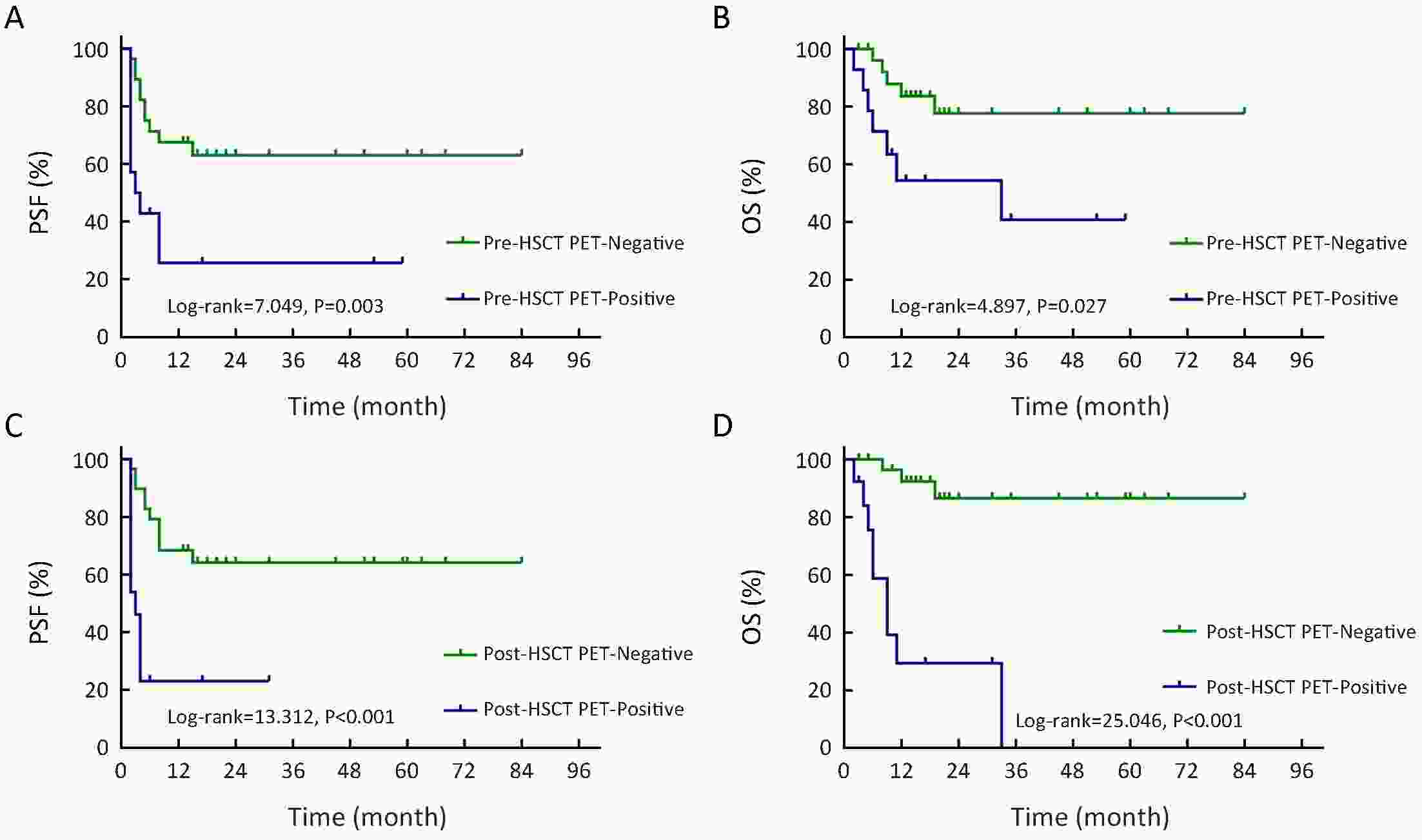
ObjectiveHigh-dose chemotherapy (HDC) followed by autologous hematopoietic stem cell transplantation (auto-HSCT) plays an important role in improving outcomes of diffuse large B cell lymphoma (DLBCL) patients. 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)/computed tomography (CT) has been widely accepted in response assessment and prediction of prognosis in DLBCL. Here, we report the value of 18F-FDG PET/CT pre- and post-HSCT in predicting outcomes of patients with DLBCL. MethodsDLBCL patients who had PET/CT scan before and after HSCT were included. PET results were interpreted based upon Deauville criteria. The prognostic value of 18F-FDG PET/CT in auto-HSCT was evaluated. ResultsEighty-four patients were enrolled. In univariate analysis, pre- and post-HSCT PET findings were correlated with 3-year progression-free survival (PFS) [hazard ratio (HR)=4.391, P=0.001; HR=7.607, P<0.001] and overall survival (OS) (HR=4.792, P=0.008; HR=26.138, P<0.001). Patients receiving upfront auto-HSCT after first-line treatment had better outcomes than relapsed/refractory DLBCL patients (3-year PFS, P<0.001; 3-year OS, P<0.001). In the relapsed/refractory patients, pre- and post-HSCT PET findings were also associated with 3-year PFS (P=0.003 vs. P<0.001) and OS (P=0.027 vs. P<0.001). A significant correlation was observed between clinical response to chemotherapy before auto-HSCT and outcomes of patients in the entire cohort (3-year PFS, P<0.001; 3-year OS, P<0.001) and in the subgroup of 21 patients with positive pre-HSCT PET (3-year PFS, P=0.084; 3-year OS, P=0.240). A significant association between survival and post-HSCT PET findings was observed in multivariate analysis (HR=5.168, P<0.001). ConclusionsPET results before and after HSCT are useful prognostic factors for DLBCL patients receiving HSCT. Patients who responded to chemotherapy, even those with positive pre-HSCT PET, are appropriate candidates for auto-HSCT.
2019, 31(1): 171-177.
doi: 10.21147/j.issn.1000-9604.2019.01.12
Abstract:
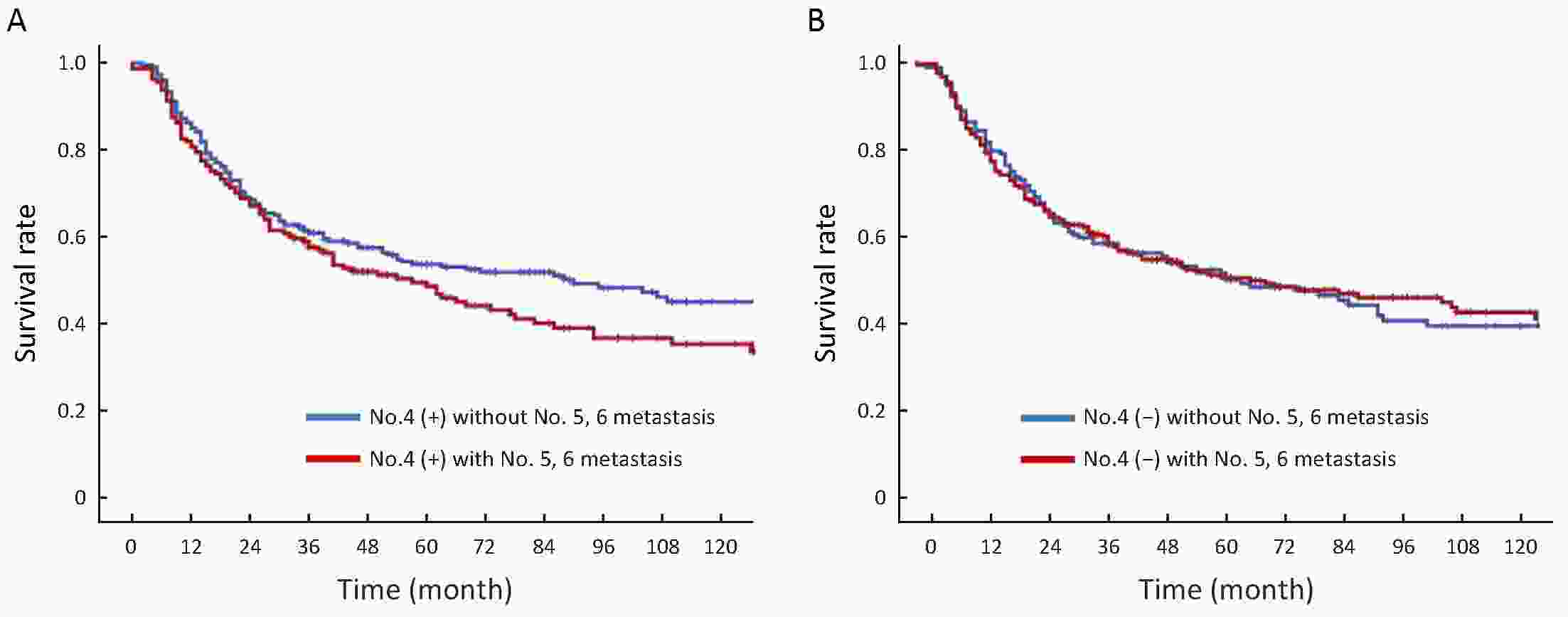
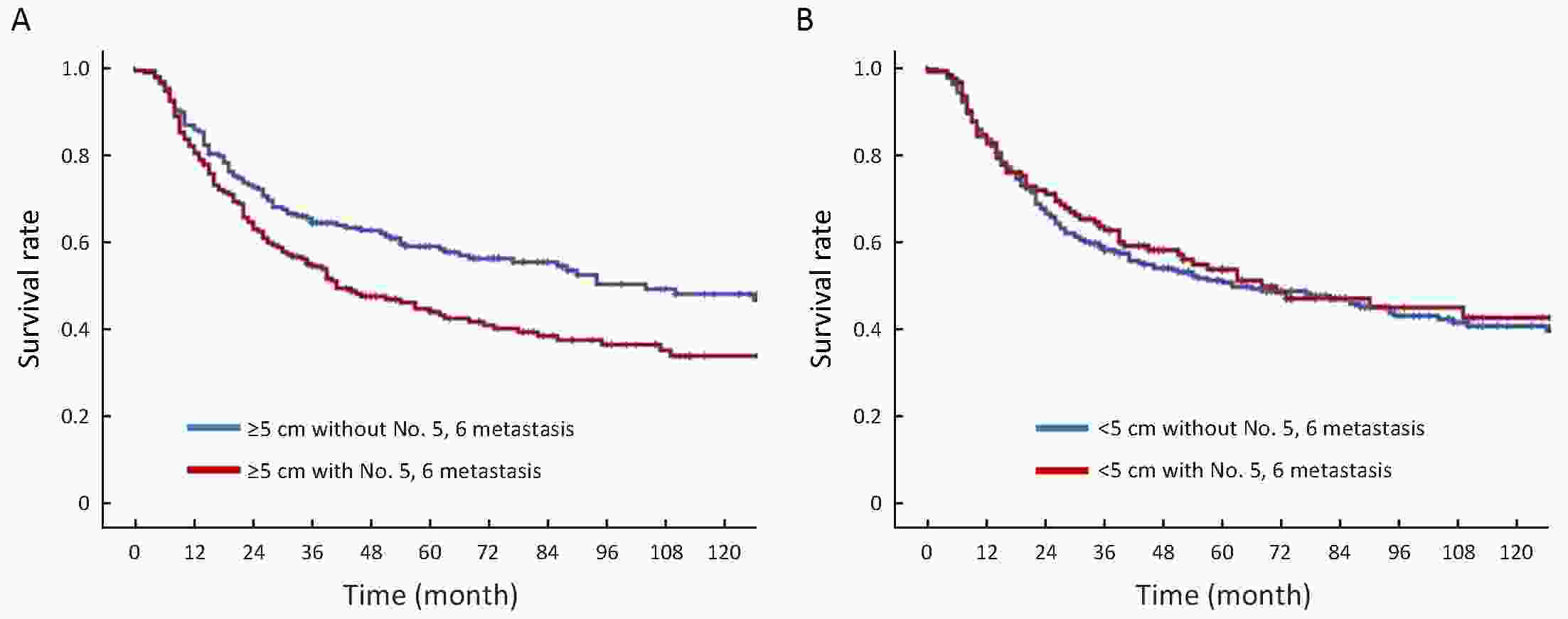
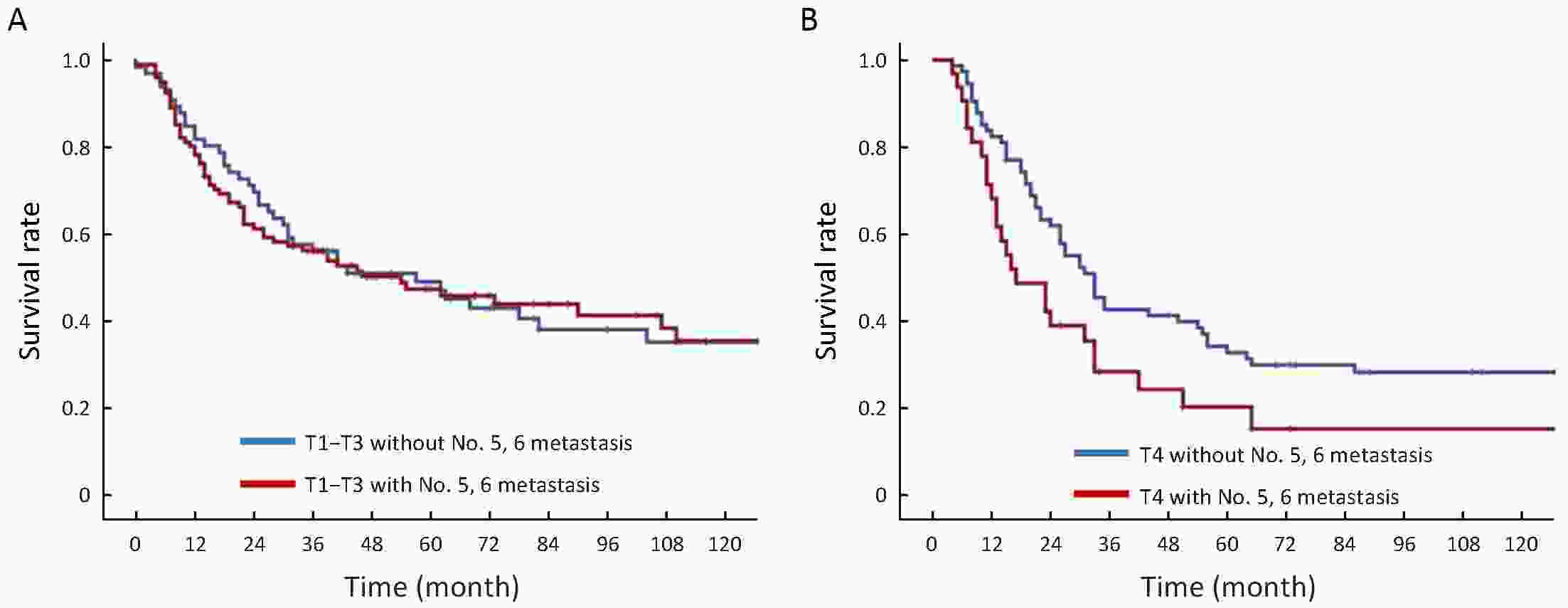
ObjectiveThe current surgical treatment guidelines for early proximal gastric cancer (PGC) still lack agreement. Lymphadenectomy of lymph nodes No. 5 and No. 6 is the major difference between total and proximal gastrectomy. We elucidated the appropriate surgical procedure for PGC by investigating the pathological characteristics and prognostic significance of lymph nodes No. 5 and No. 6. MethodsIn total, 333 PGC patients who underwent total gastrectomy were enrolled in this study. We investigated their clinicopathological characteristics and the metastatic patterns of the lymph nodes. Patients with metastasis in lymph nodes No. 5 and No. 6 were combined into one group and we compared the difference in survival between those with and without metastasis in lymph nodes No. 5, 6 (lymph nodes No. 5 and No. 6 in any group of metastasis) for different subgroups. ResultsThe metastatic rates for lymph nodes No. 5 and No. 6 in PGC were 9.91% and 16.11%, respectively. The metastatic rate for both lymph nodes No. 5, 6 was 20.42%. Multivariate analysis showed that positive metastasis in lymph node No. 4, depth of invasion, and tumor size were independently correlated with the presence of metastasis in lymph nodes No. 5, 6. ConclusionsWhen lymph node No. 4 is positive (intraoperative pathology) or tumor size ≥5 cm or T4 stage, lymphadenectomy should be performed for lymph nodes No. 5 and No. 6, and total gastrectomy is recommended.
2019, 31(1): 178-187.
doi: 10.21147/j.issn.1000-9604.2019.01.13
Abstract:
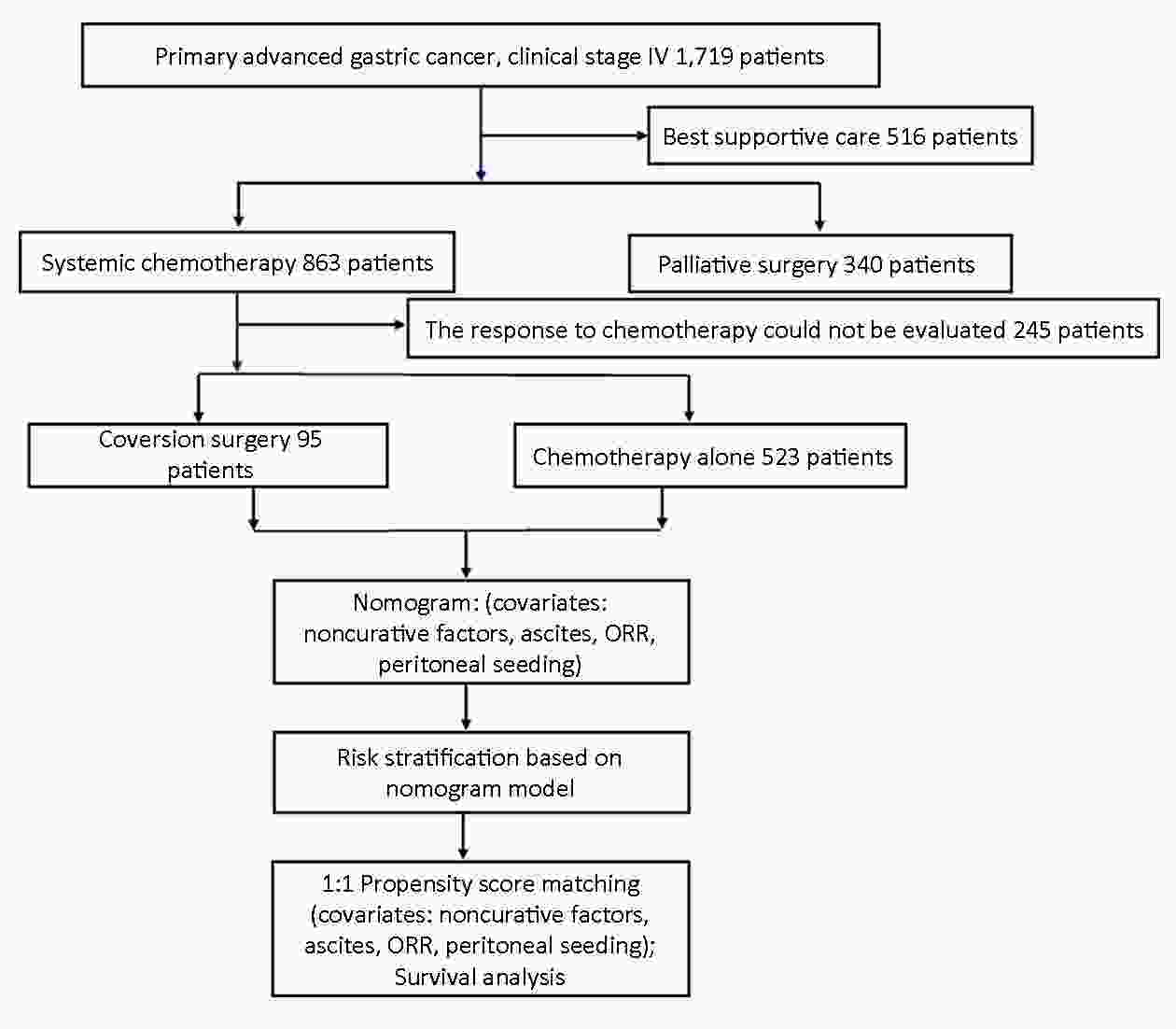
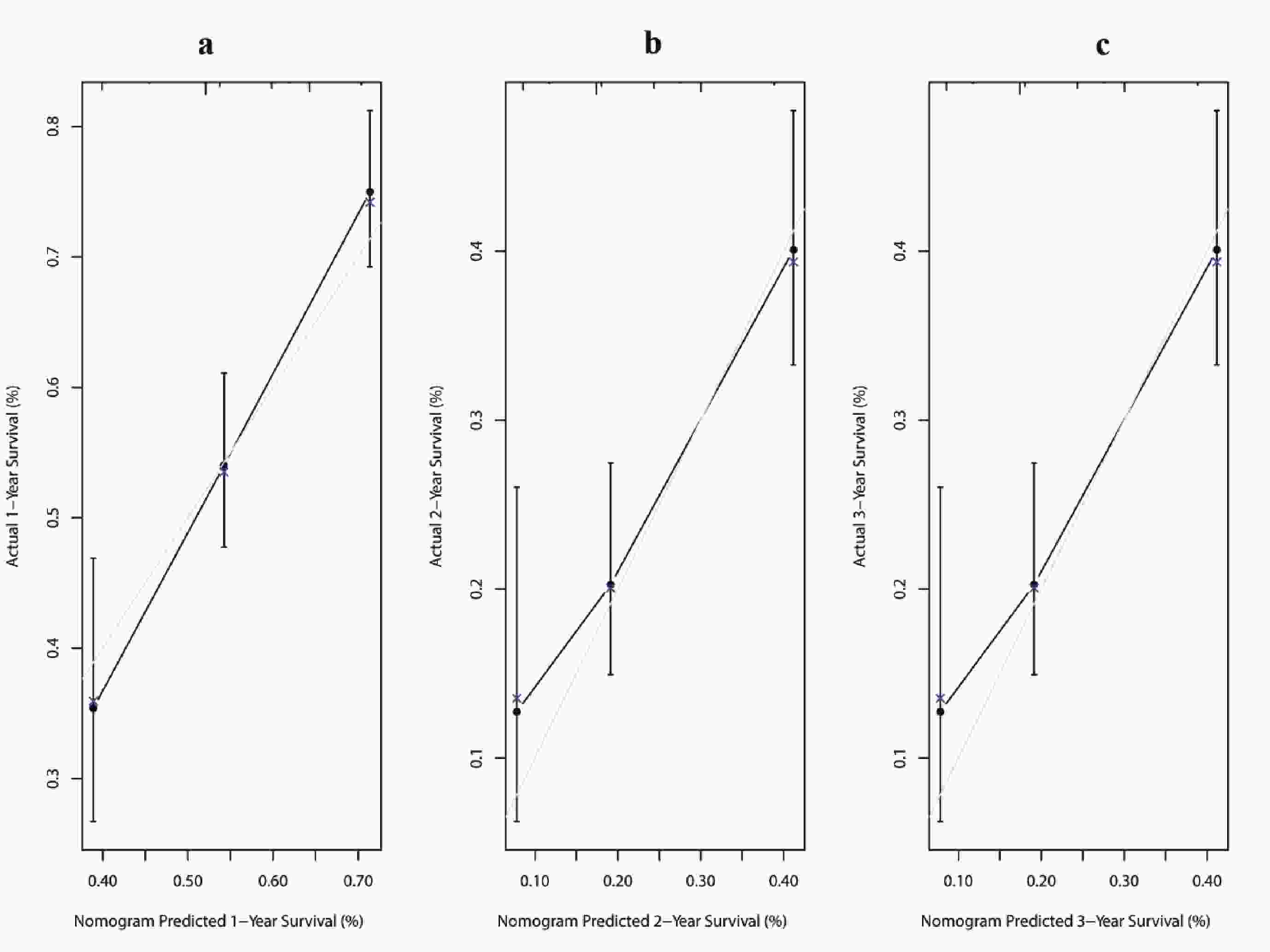
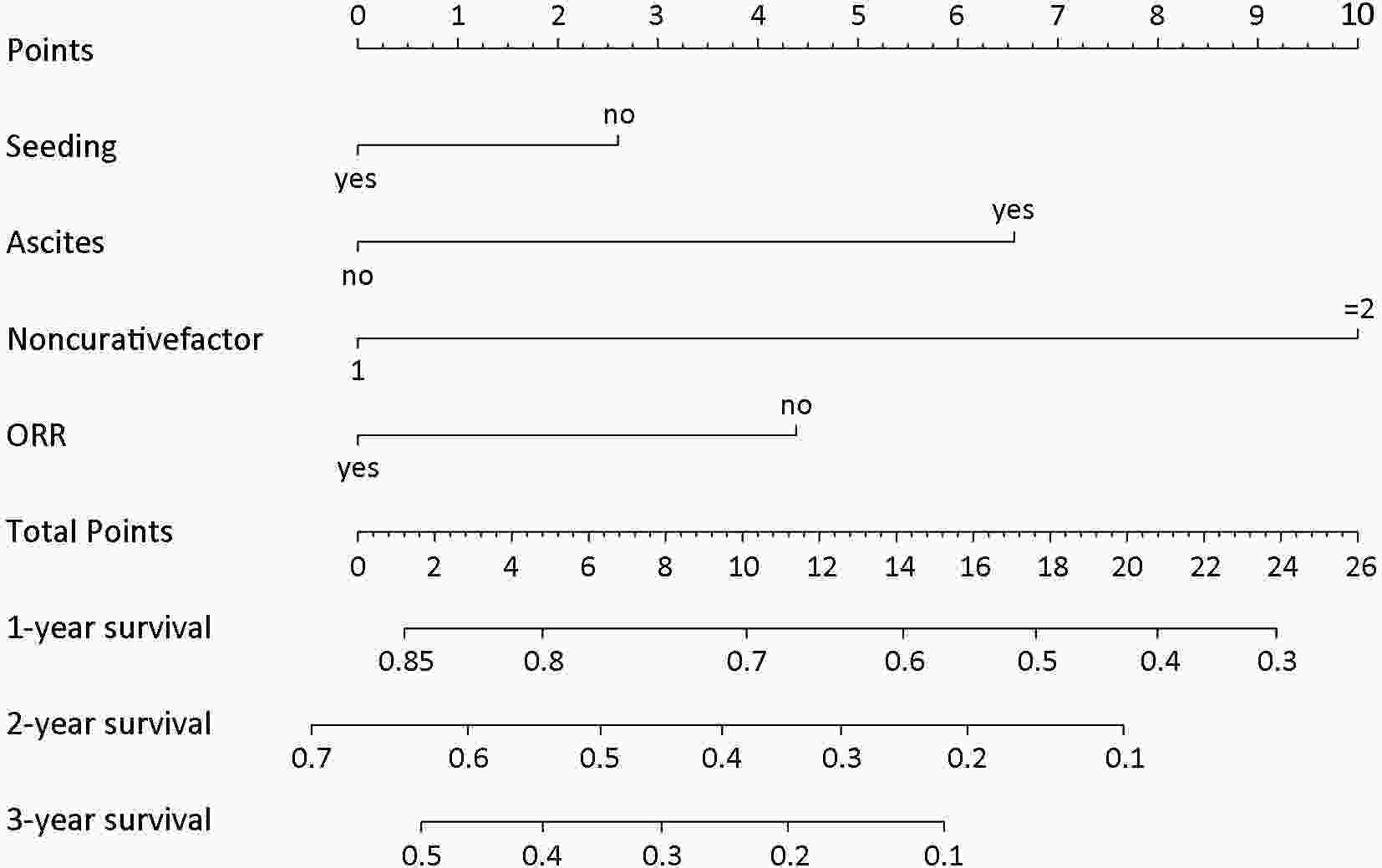
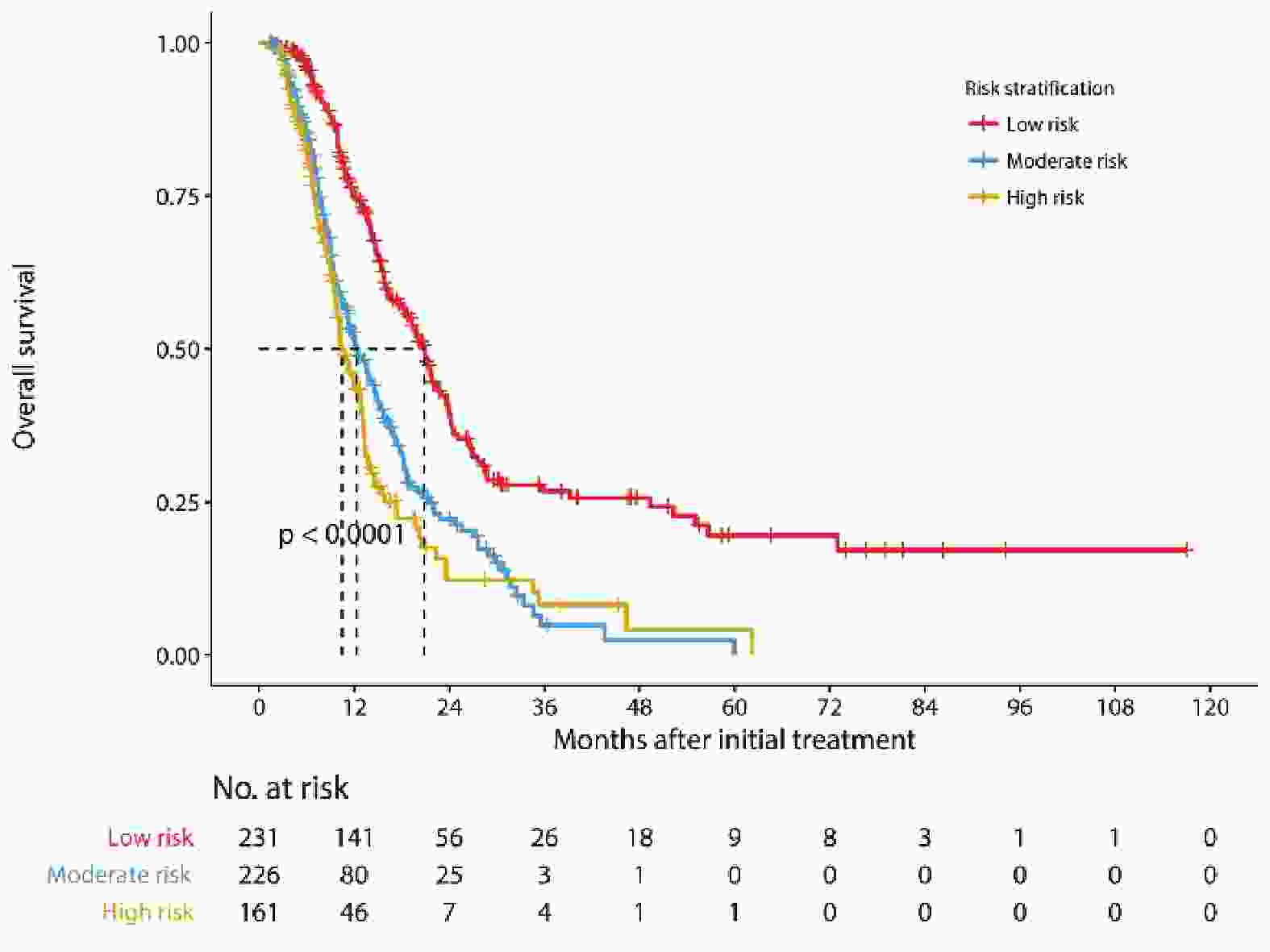
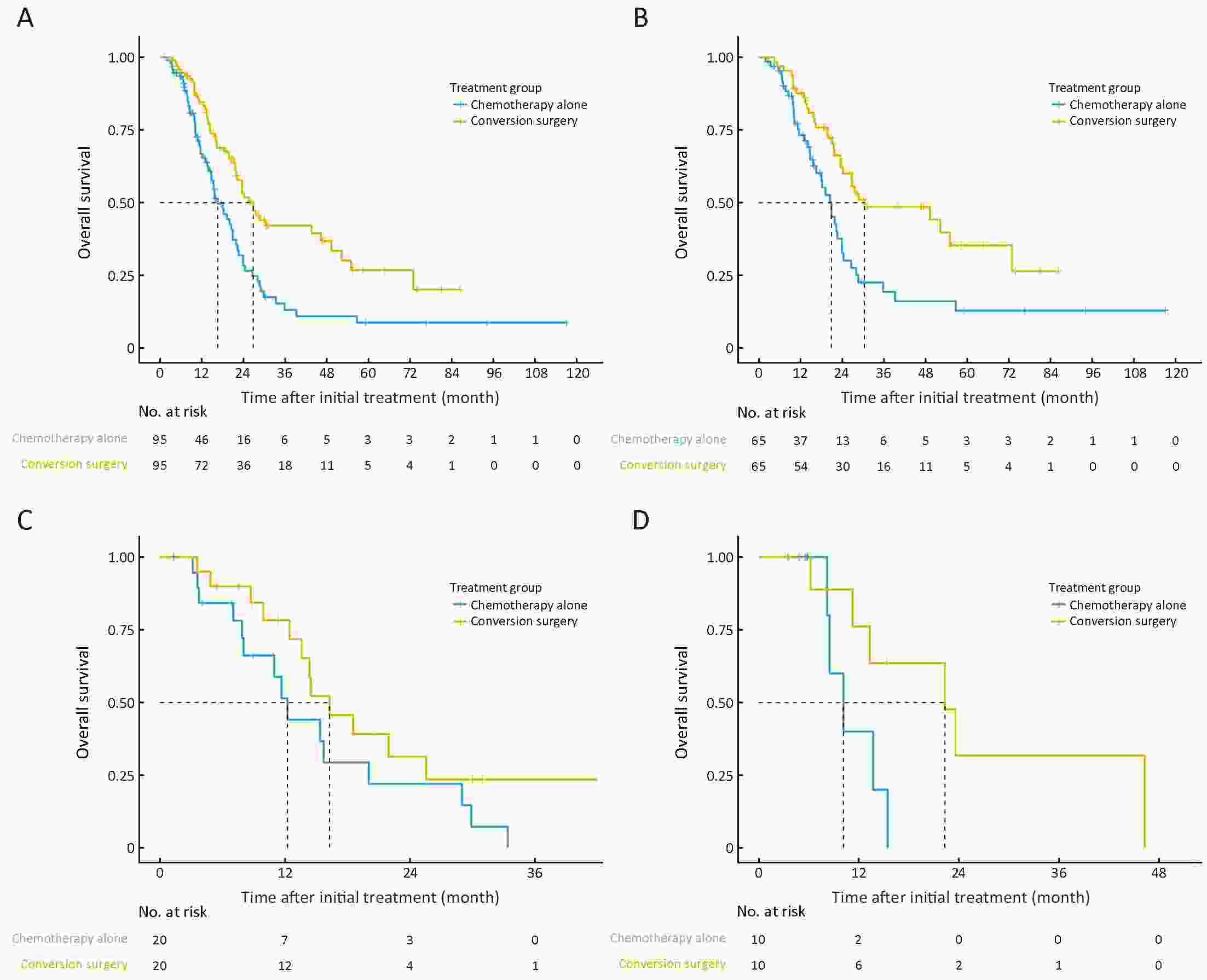
ObjectiveConversion surgery is a surgery with a purpose of R0 resection in primary advanced gastric cancer (GC) that responded well to systemic chemotherapy. This study aimed to explore the efficacy of conversion surgery for advanced GC. MethodsA total of 618 advanced GC patients receiving systemic chemotherapy were stratified into low-, moderate- and high-risk groups based on a nomogram-predicted probability of overall survival. The survival of conversion surgery and chemotherapy alone groups was compared using the log-rank test and Cox regression analysis after propensity score matching (PSM). ResultsA nomogram with good discrimination (concordance index: 0.65) and accurate calibration was constructed. After PSM, the median survival time (MST) of conversion surgery was 26.80 months, compared with 16.60 months of chemotherapy alone (P<0.001). Conversion surgery was associated with a longer MST for patients in the low-risk group (30.40 months vs. 20.90 months, P=0.013), whereas it was not associated with prolonged survival in the moderate- and high-risk groups (P=0.221 and P=0.131, respectively). ConclusionsConversion surgery was associated with longer survival, especially for low-risk population.
2019, 31(1): 188-202.
doi: 10.21147/j.issn.1000-9604.2019.01.14
Abstract:
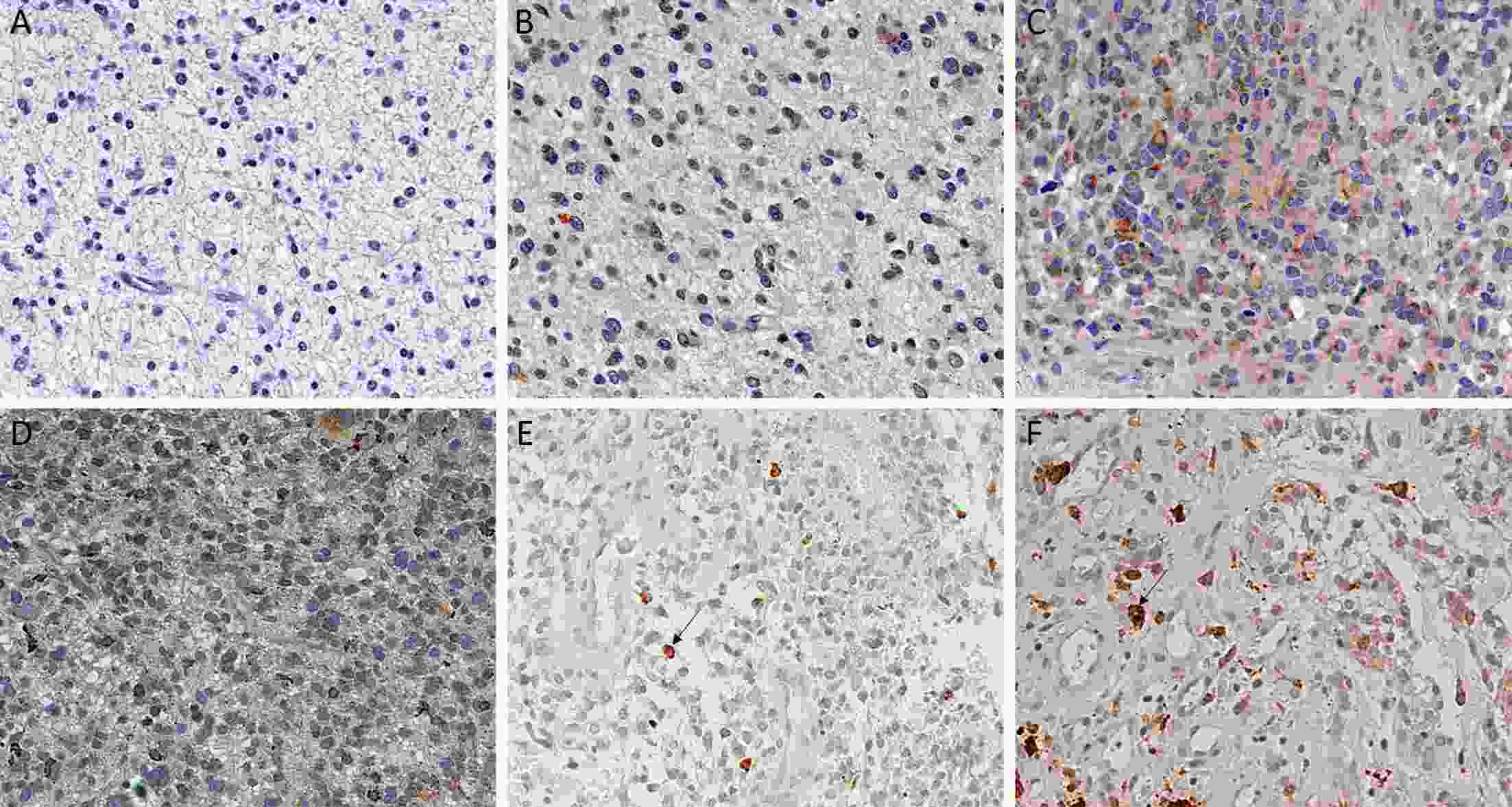
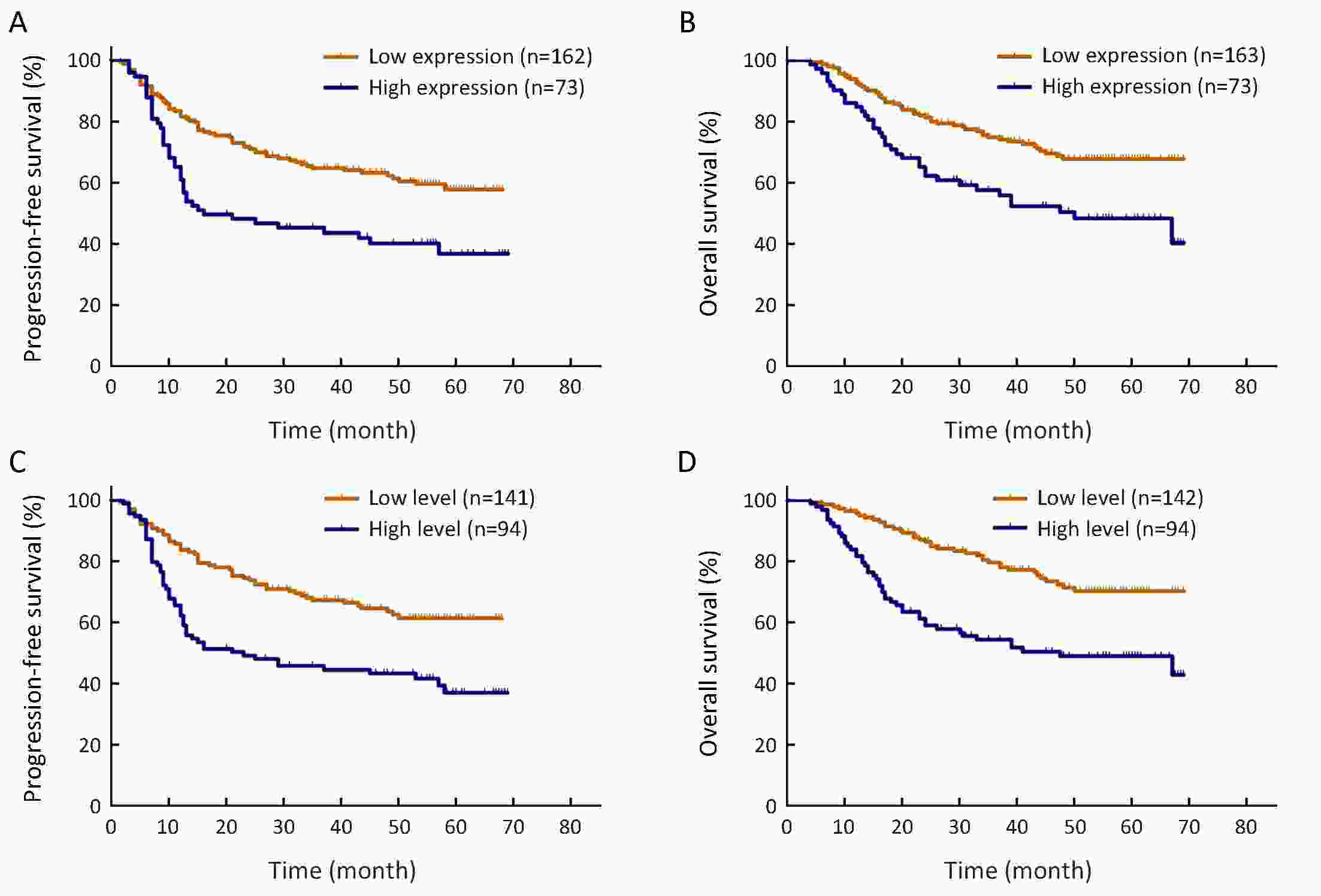
ObjectiveTo determine the prognostic implications and clinical significance of epidermal growth factor receptor variant III (EGFRvIII) expression and EGFRvIII nuclear translocation in Chinese human gliomas. MethodsWe retrospectively examined EGFRvIII expression and EGFRvIII nuclear translocation using immunohistochemistry in specimens of 240 Chinese patients with glioma, including 84 World Health Organization (WHO) II gliomas, 84 WHO III gliomas and 72 glioblastomas (WHO IV). Factors that correlated with EGFRvIII and EGFRvIII nuclear translocation expression were analyzed by the Chi-square test. Kaplan-Meier methodology and Cox regression were used for the survival analysis. ResultsLog-rank tests showed that patient age, Karnofsky performance scale (KPS) score, tumor grade, EGFRvIII expression, EGFRvIII nuclear translocation, 1p/19q codeletion, isocitrate dehydrogenase (IDH) mutation, Ki-67 labeling index and O6-methylguanine-DNA methyltransferase (MGMT) status (P<0.05) were significantly correlated with overall survival (OS) time. Multivariate Cox regression analysis revealed that patient age, tumor grade, EGFRvIII nuclear translocation, 1p/19q codeletion, and IDH mutation (P<0.05) were significantly correlated with OS. Patients with a high level of EGFRvIII nuclear translocation (≥7%) had both significantly shorter OS [hazard ratio (HR): 1.920, 95% confidence interval (95% CI): 1.228−3.003, P=0.004] and progression-free survival (PFS) times (HR: 1.661, 95% CI: 1.116−2.471, P=0.012) than those with a low level of EGFRvIII nuclear translocation (<7%). ConclusionsA high level of EGFRvIII nuclear translocation in glioma is an independent factor indicating a poor prognosis, but EGFRvIII expression is not an independent clinical prognostic factor. The level of EGFRvIII nuclear translocation maybe a novel and crucial prognostic biomarker in glioma.
2019, 31(1): 203-211.
doi: 10.21147/j.issn.1000-9604.2019.01.15
Abstract:
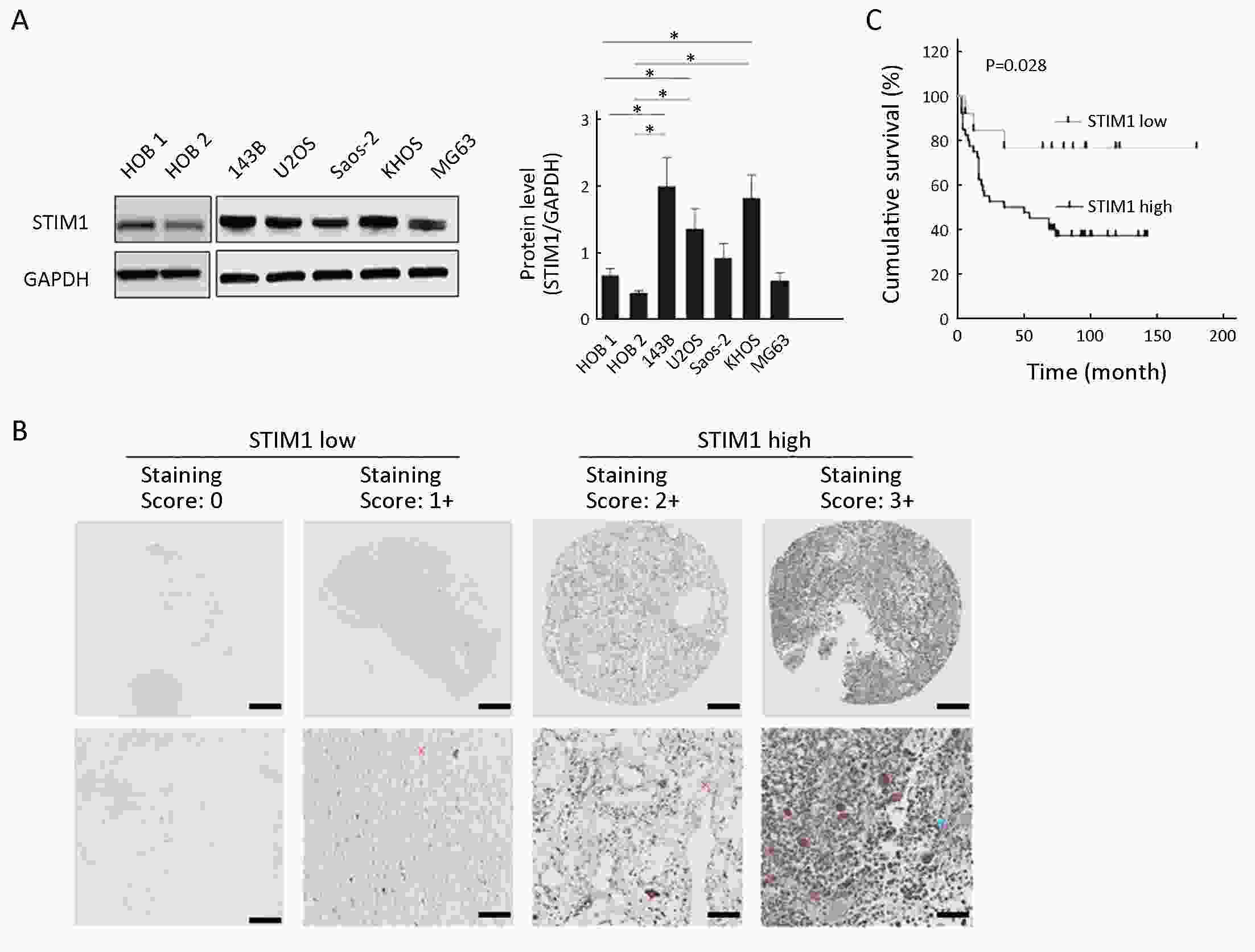
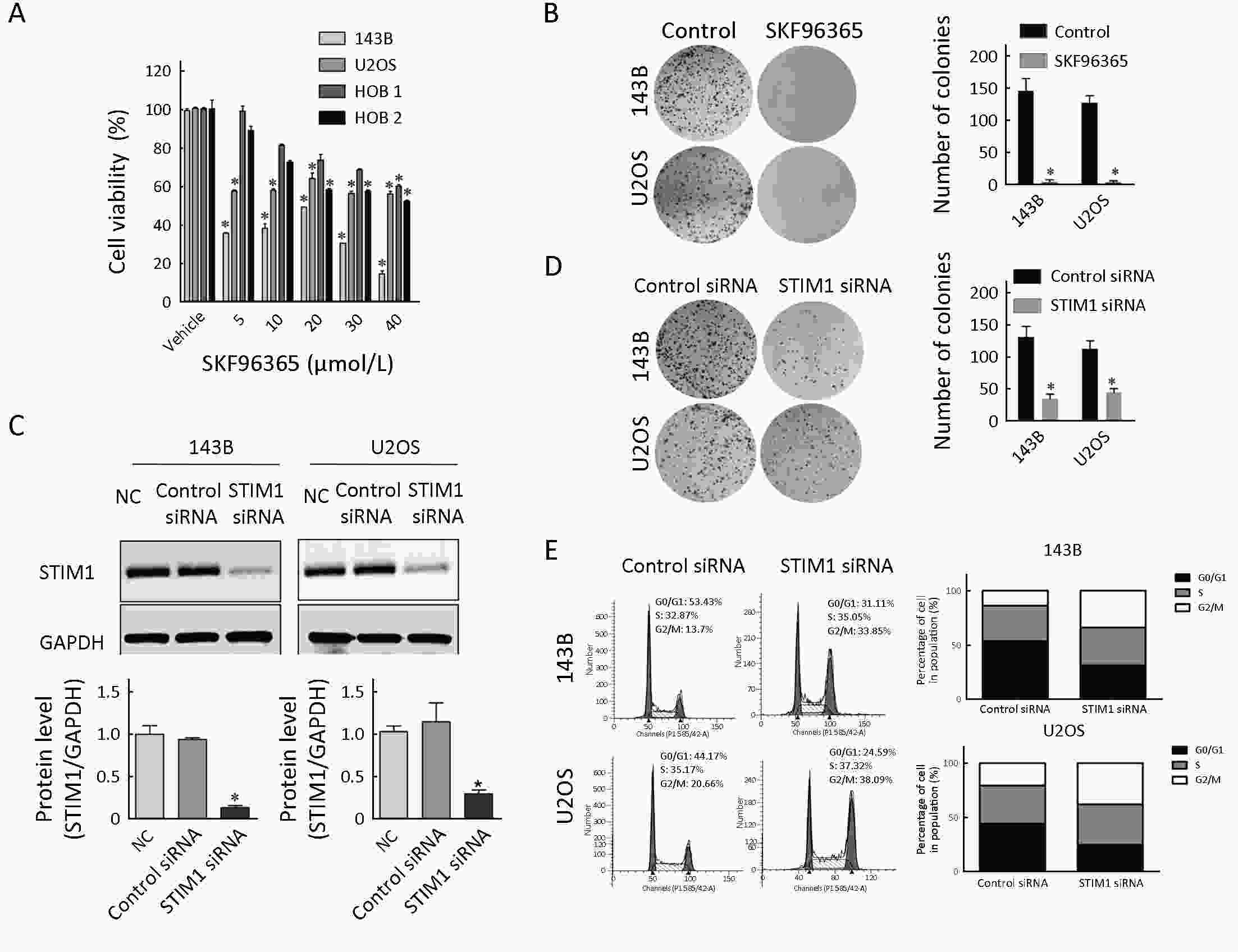
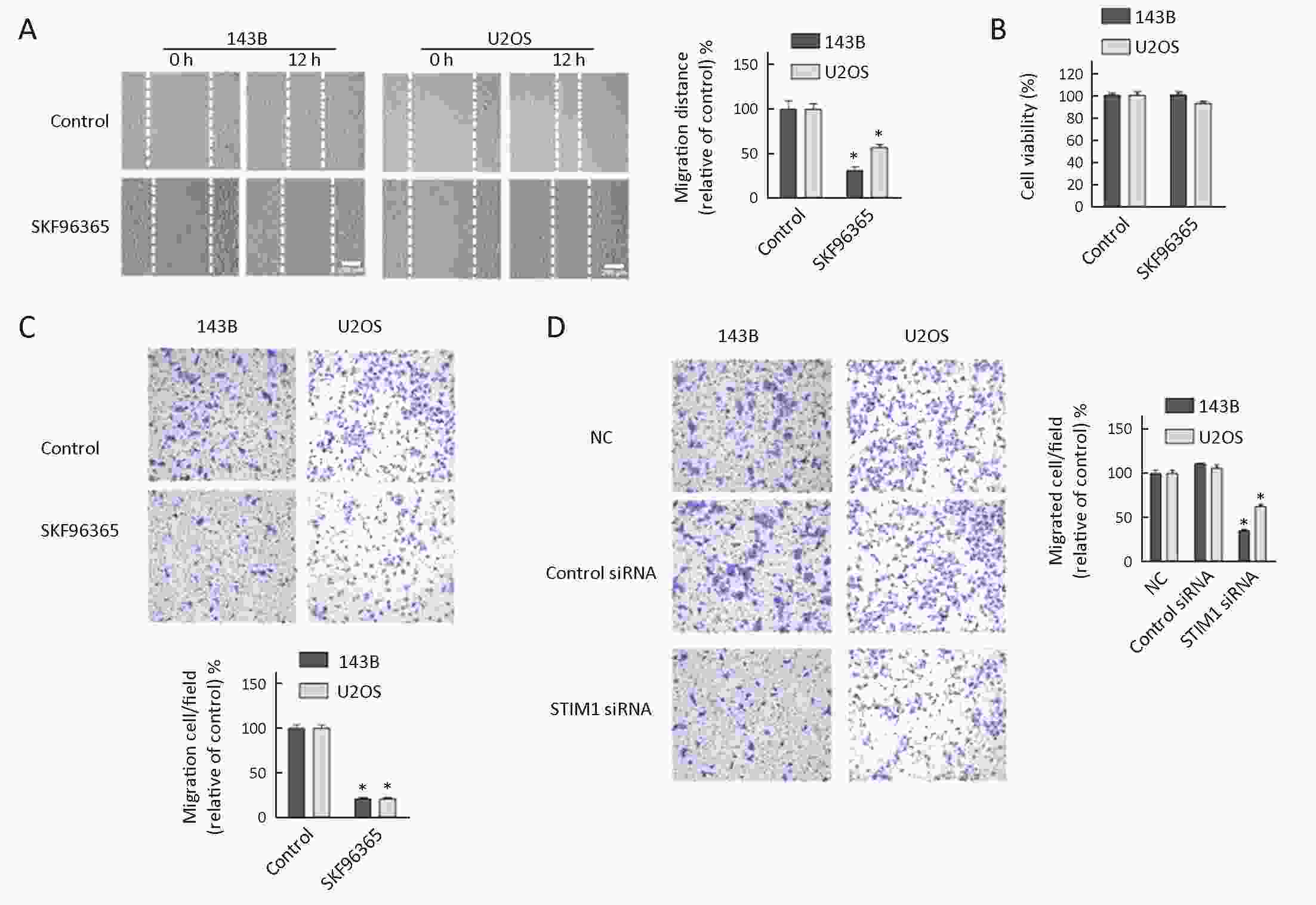
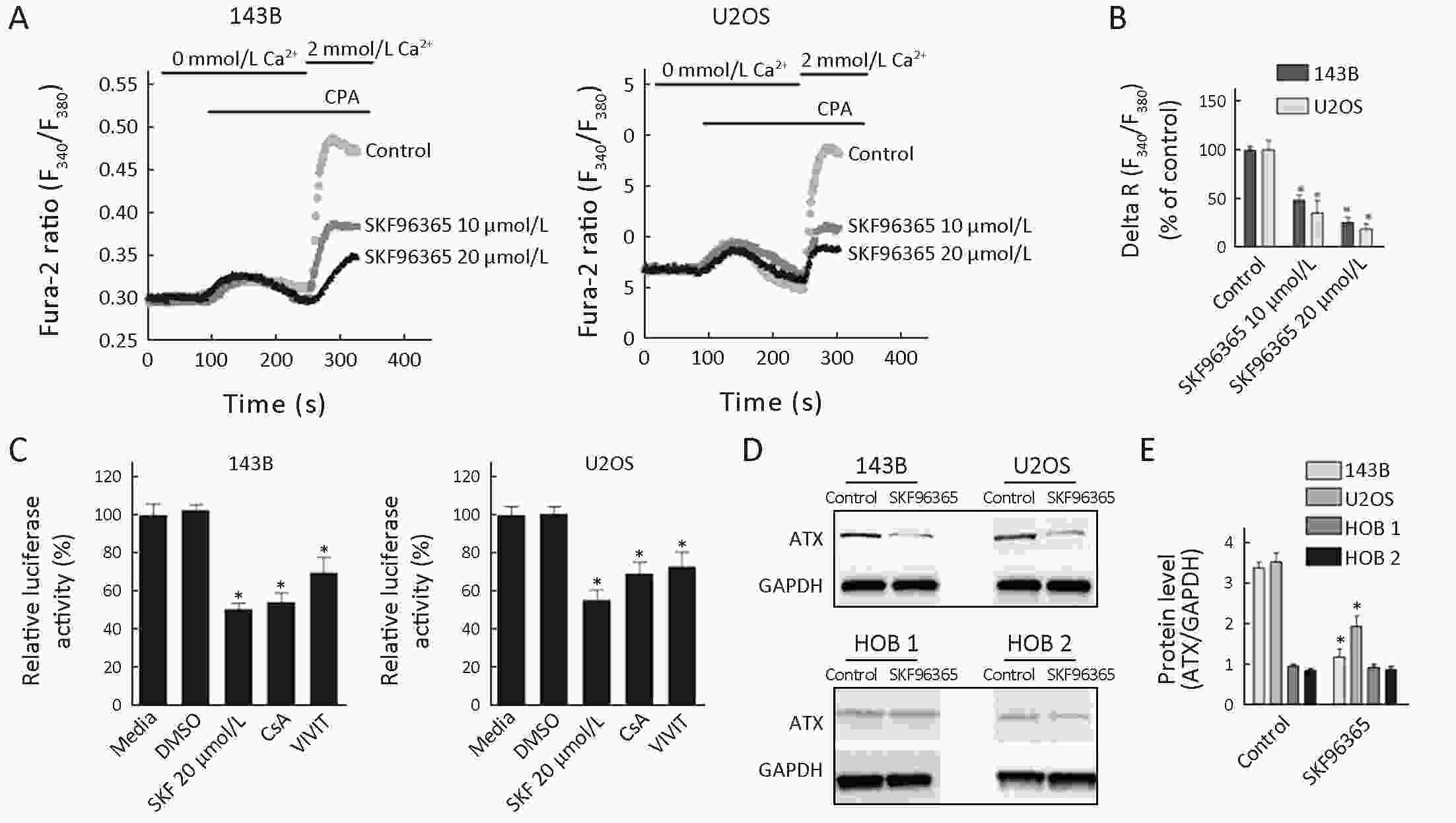
ObjectiveTo examine the role of store-operated calcium entry (SOCE) and stromal interaction molecule 1 (STIM1) in survival and migration of osteosarcoma cells and investigate what blockade of store-operated Ca2+ contributes to the regulation of osteosarcoma cells. MethodsFirst, we examined the expression levels of STIM1 in osteosarcoma cell lines by Western analysis and in tissue specimens by immunohistochemistry. Second, we investigated the effect of SOCE and STIM1 on osteosarcoma cell viability using MTS assays and on cell proliferation using colony formation. Third, we investigated the role of SOCE and STIM1 in cell migration using wound healing assays and Boyden chamber assays. Finally, we studied the effect of SOCE on the nuclear factor of activated T-cells cytoplasmic 1 (NFATc1) activity by luciferase assays. ResultsSTIM1 was overexpressed in osteosarcoma cell lines and tissue specimens and was associated with poor survival of osteosarcoma patients. Also, inhibition of SOCE and STIM1 decreased the cell viability and migration of osteosarcoma cells. Furthermore, our results showed that blockade of store-operated Ca2+ channels involved down-regulation of NFATc1 in osteosarcoma cells. ConclusionsSTIM1 is essential for osteosarcoma cell functions, and STIM1 and Ca2+ entry pathway could be further explored as molecular targets in the treatment of osteosarcoma.
2019, 31(1): 212-222.
doi: 10.21147/j.issn.1000-9604.2019.01.16
Abstract:
Colorectal cancer is closely related to inflammation and immune response. Radiotherapy, as a major treatment for colorectal cancer, plays a central role in cancer control. Inflammation caused by ionizing radiation can exert either anti- or pro-tumorigenic effects. Additionally, radiotherapy can elicit an anti-tumor response not only in radiation of target lesions but also in radiation of remote lesions. However, the immune mechanism underlying this effect has not been thoroughly elucidated yet. The combination therapeutic regimen of radiotherapy with other therapeutic methods, including chemotherapy and immunotherapy, has been applied in clinical practice. Meanwhile, radiation toxicity and radiosensitivity have long been problems that affect a patient’s quality of life and morbidity. Researchers have found that the abovementioned problems are closely associated with gut microbiota. Here we discuss the impact of immune response induced by radiotherapy on tumor regression and the impact of intestinal flora on the consequent clinical efficacy.
Colorectal cancer is closely related to inflammation and immune response. Radiotherapy, as a major treatment for colorectal cancer, plays a central role in cancer control. Inflammation caused by ionizing radiation can exert either anti- or pro-tumorigenic effects. Additionally, radiotherapy can elicit an anti-tumor response not only in radiation of target lesions but also in radiation of remote lesions. However, the immune mechanism underlying this effect has not been thoroughly elucidated yet. The combination therapeutic regimen of radiotherapy with other therapeutic methods, including chemotherapy and immunotherapy, has been applied in clinical practice. Meanwhile, radiation toxicity and radiosensitivity have long been problems that affect a patient’s quality of life and morbidity. Researchers have found that the abovementioned problems are closely associated with gut microbiota. Here we discuss the impact of immune response induced by radiotherapy on tumor regression and the impact of intestinal flora on the consequent clinical efficacy.

 Abstract
Abstract FullText HTML
FullText HTML PDF 364KB
PDF 364KB