2019 Vol.31(3)
Display Mode: |
2019, 31(3): 419-420.
doi: 10.21147/j.issn.1000-9604.2019.03.01
Abstract:
2019, 31(3): 421-422.
doi: 10.21147/j.issn.1000-9604.2019.03.02
Abstract:
2019, 31(3): 423-425.
doi: 10.21147/j.issn.1000-9604.2019.03.03
Abstract:
2019, 31(3): 426-434.
doi: 10.21147/j.issn.1000-9604.2019.03.04
Abstract:
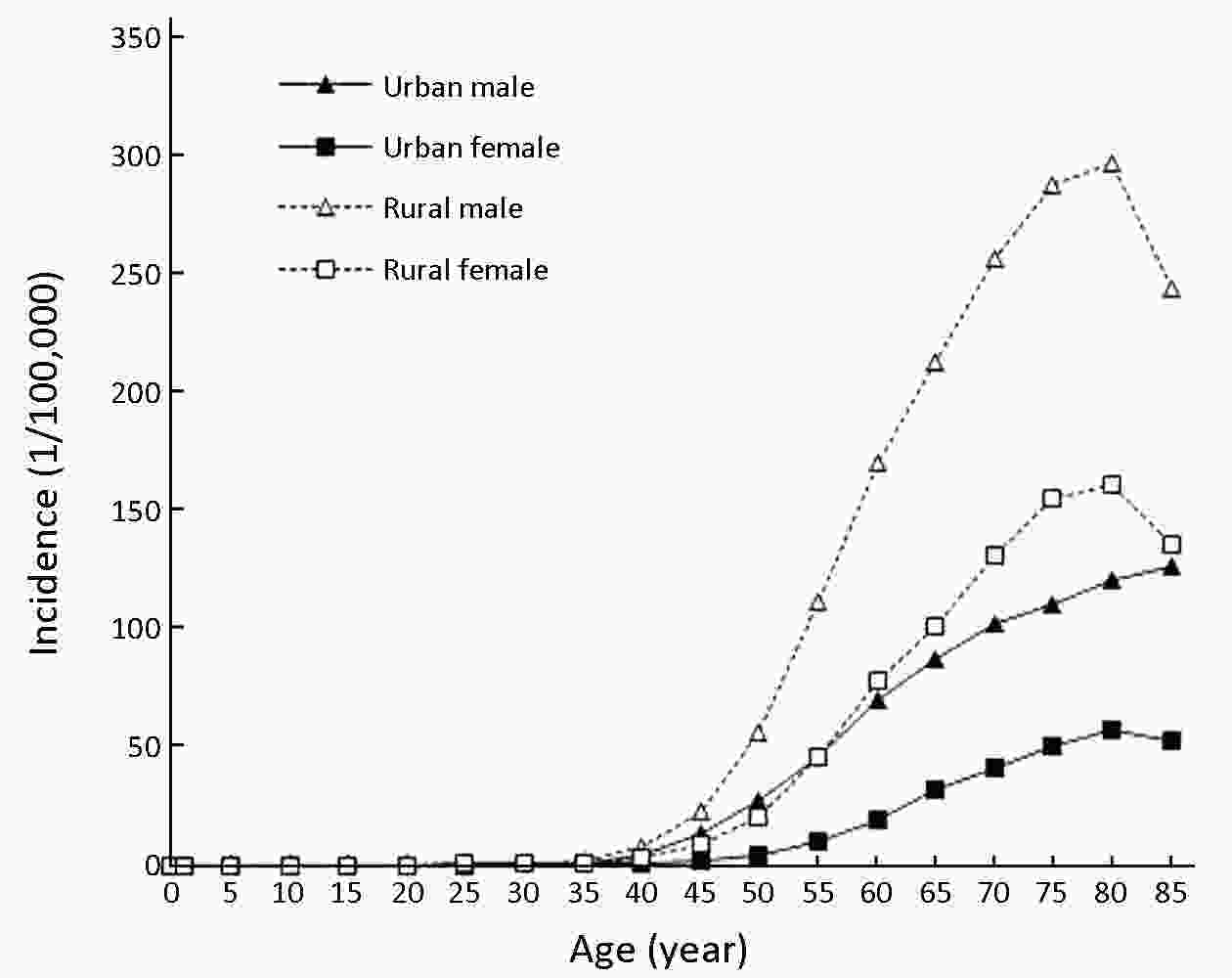
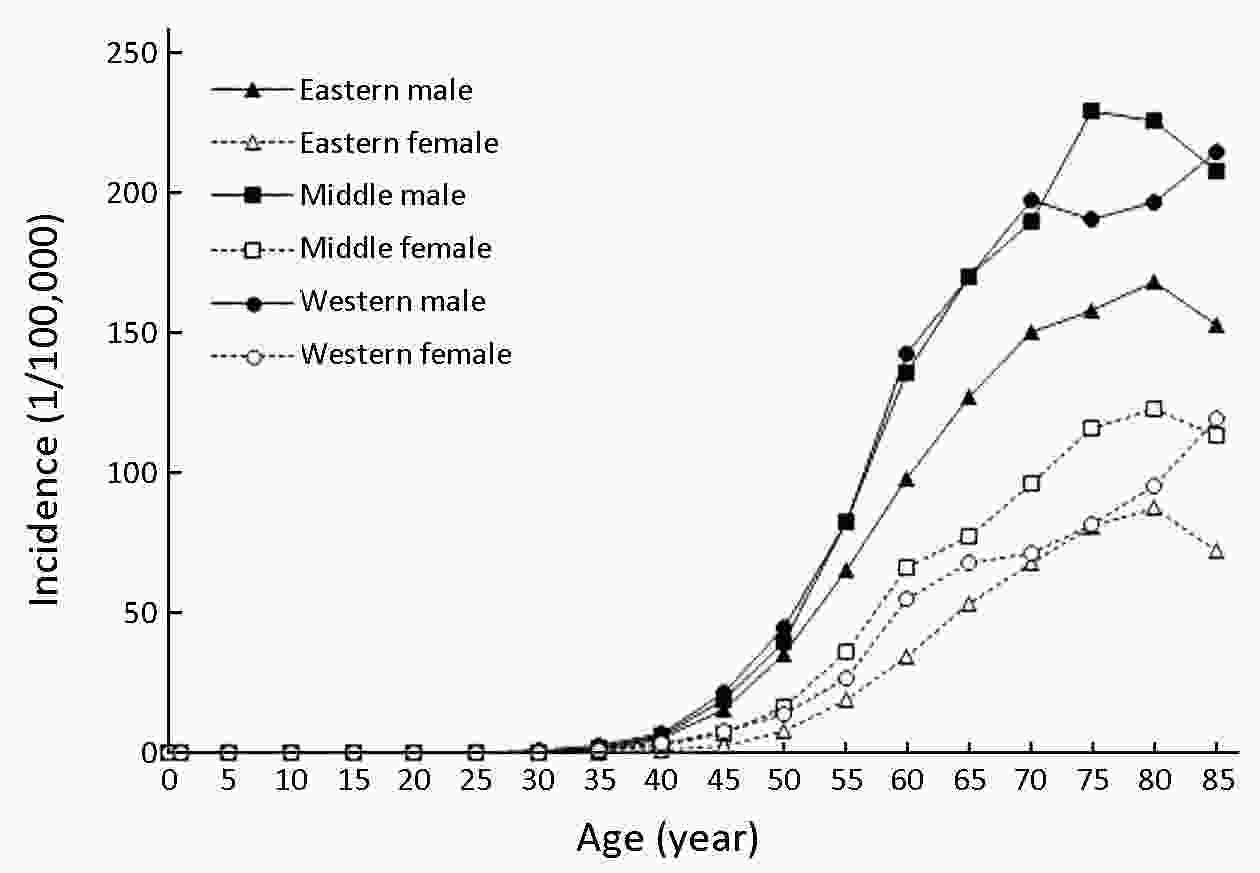
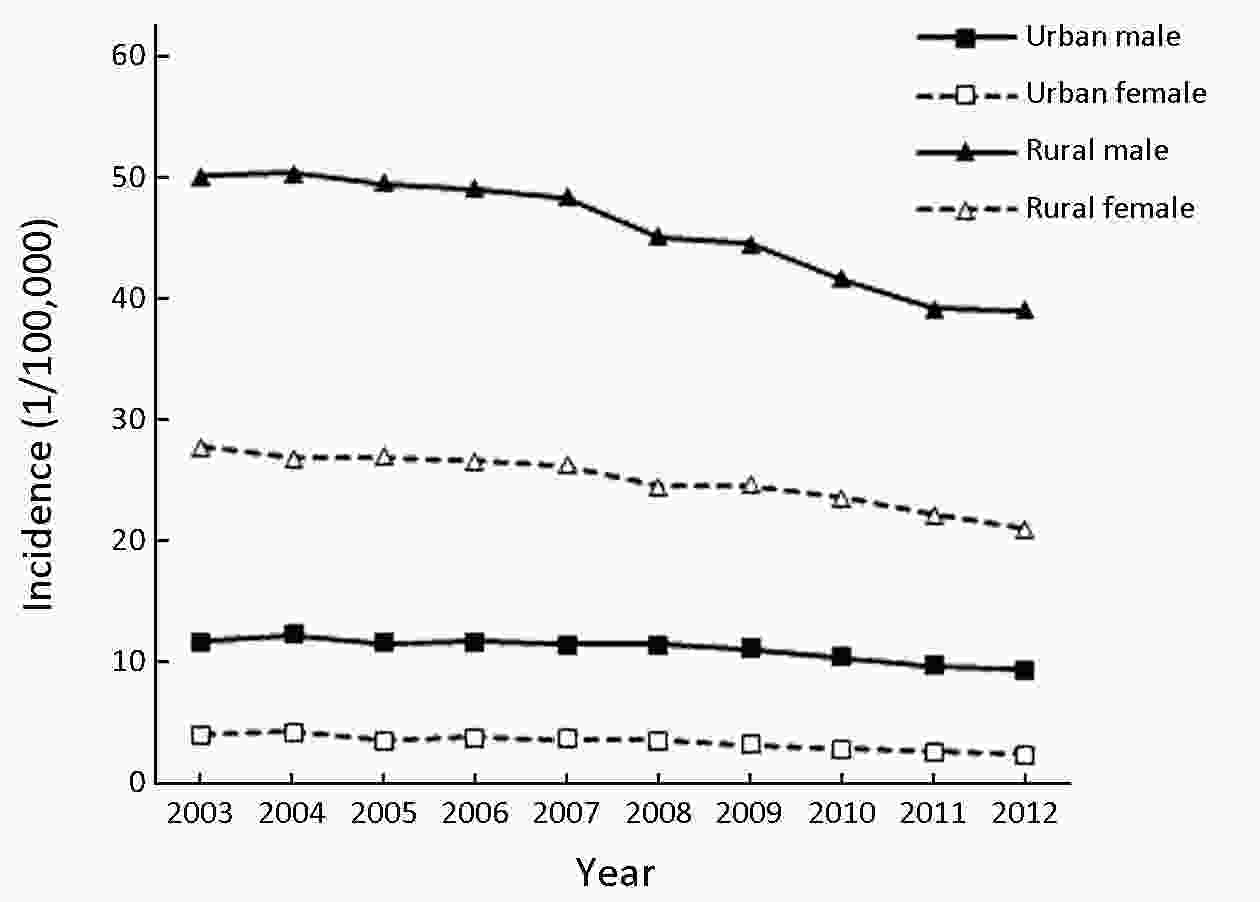
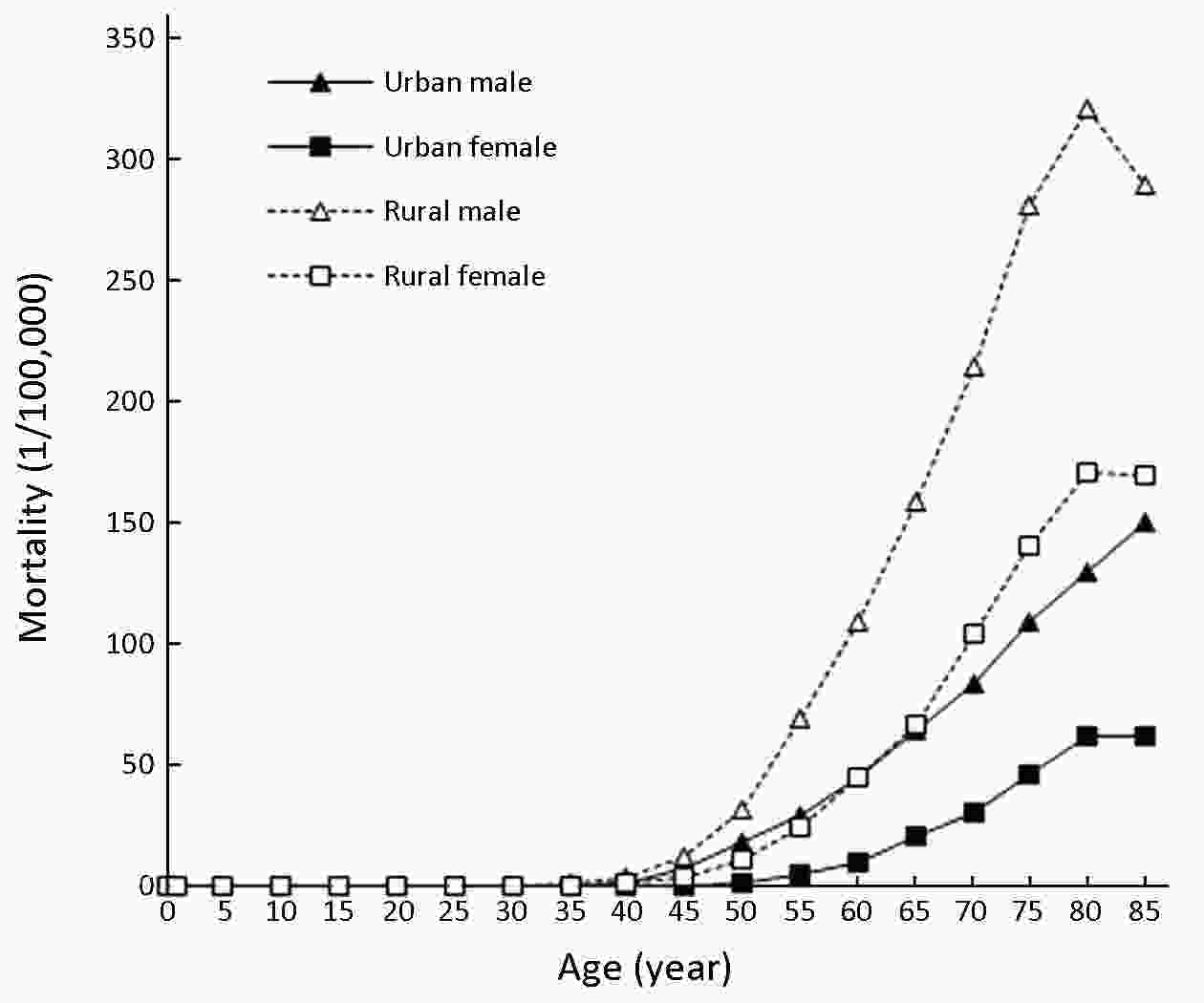
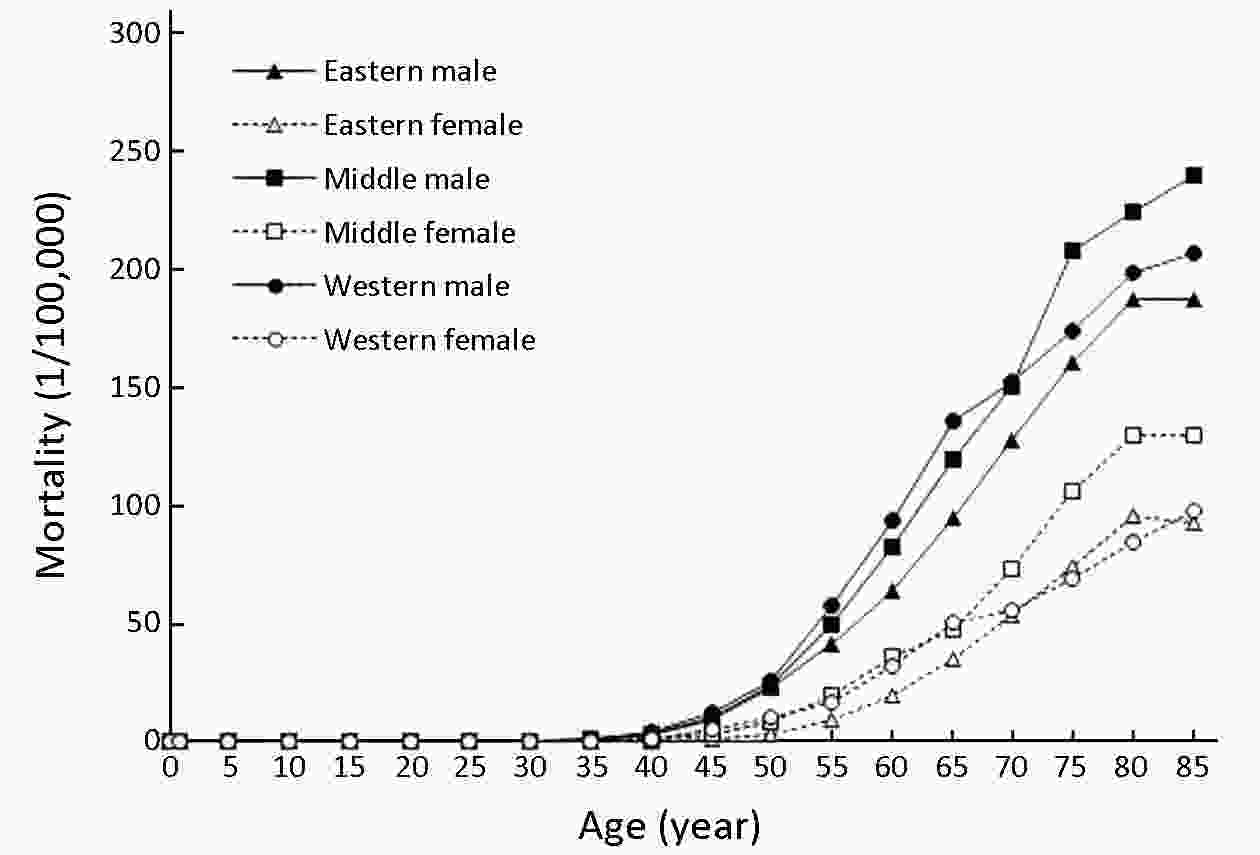
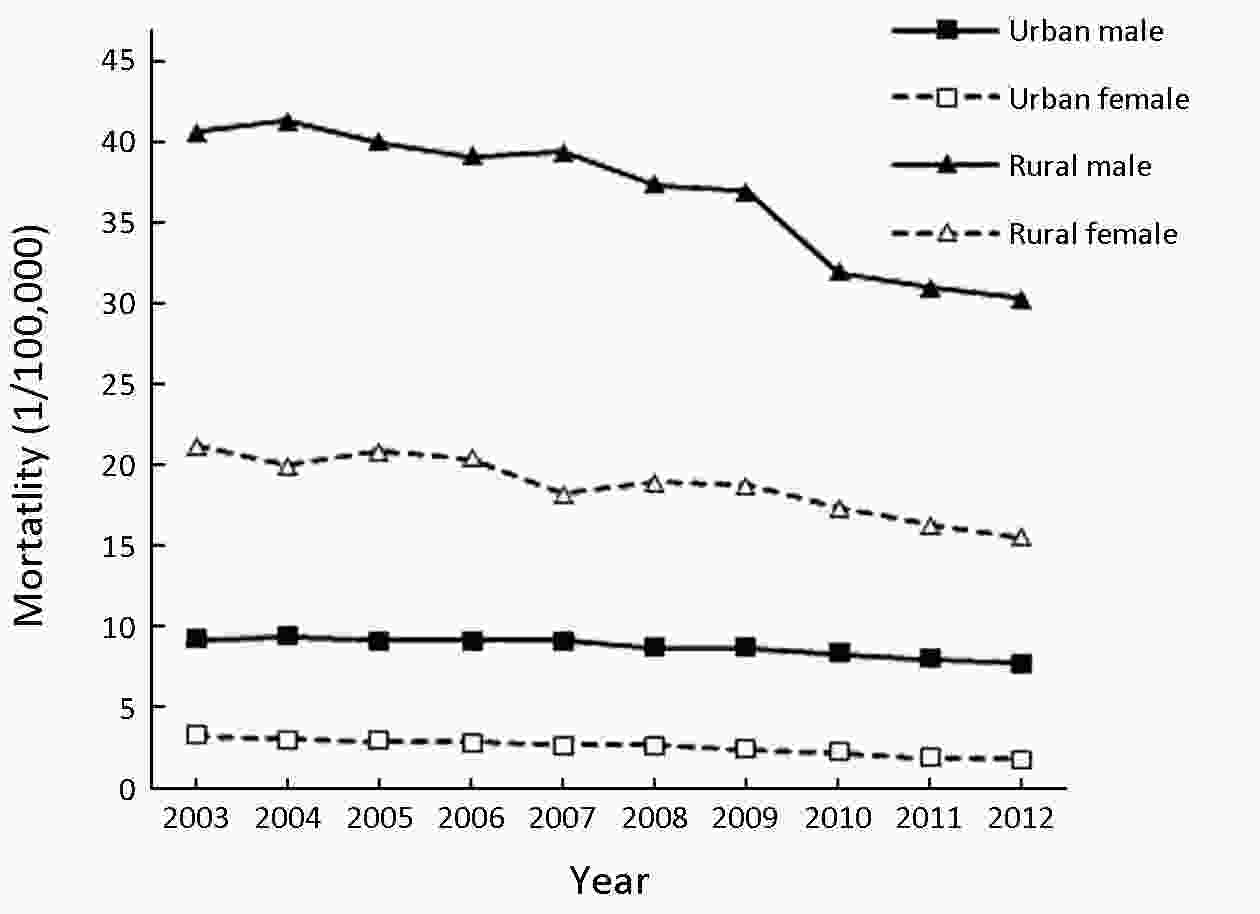
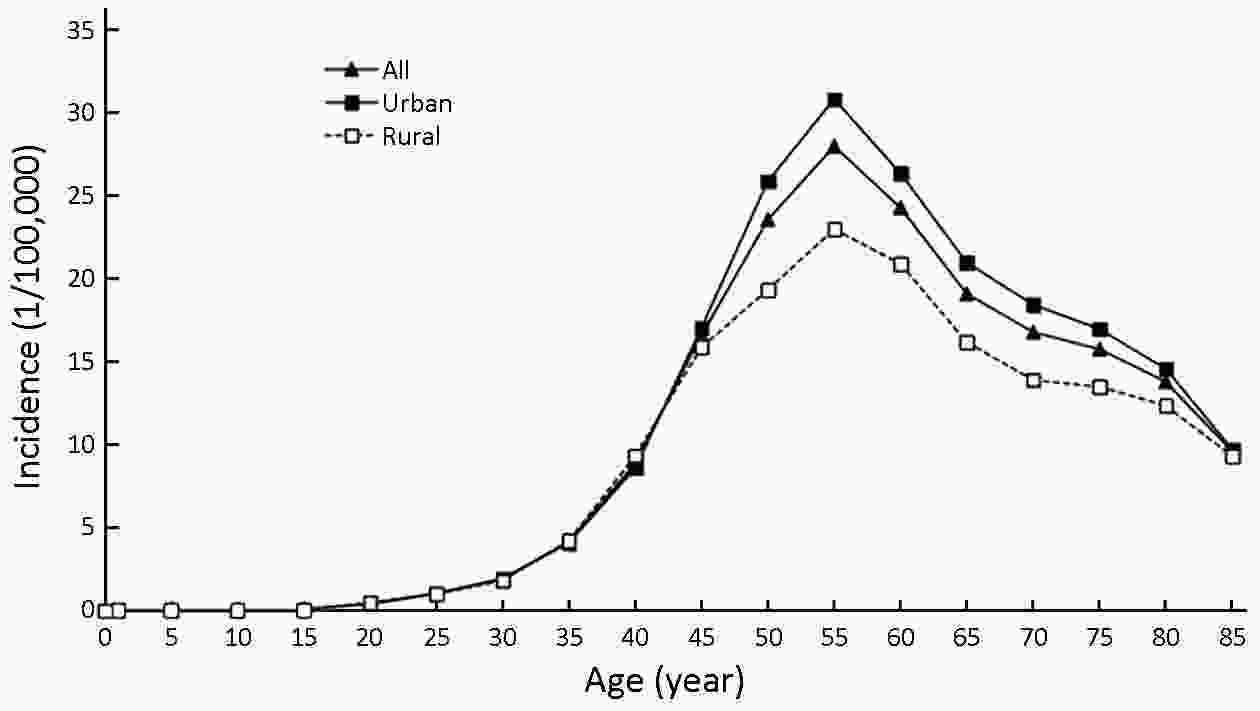
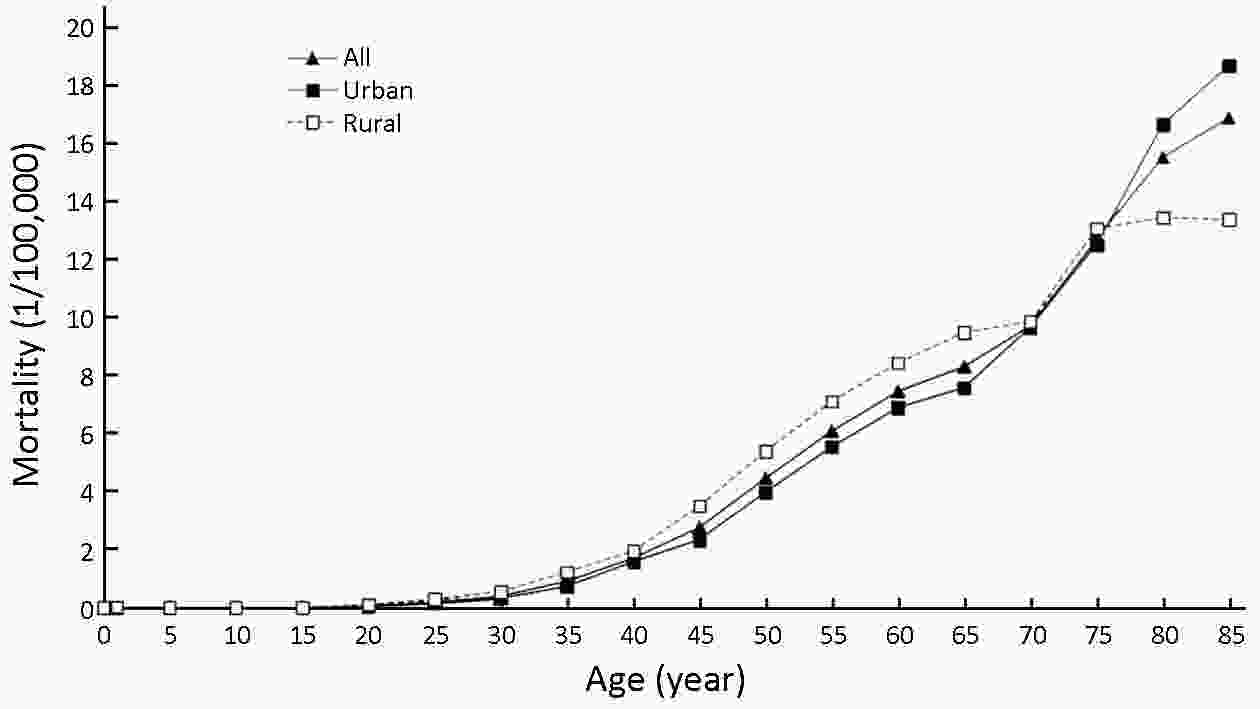
Objective To analyze the incidence and mortality rates of esophagus cancer in China from 2008 to 2012. Methods Incident and mortality cases of esophagus cancer were retrieved from the National Central Cancer Registry (NCCR) database collecting from 135 cancer registries in China during 2008−2012. The incidence and mortality rates of esophagus cancer were calculated by area (urban/rural), region (eastern, middle, western), gender and age group (0, 1−4, 5−84 by 5 years and 85+ years). China census in 2000 and Segi’s world population were applied for age-standardized rates. Joinpoint model was used for time-trend analysis. Results The crude incidence rate of esophagus cancer was 22.57/100,000. The age-standardized incidence rates by China standard population (ASIRC) and by world standard population (ASIRW) were 14.58/100,000 and 14.80/100,000, respectively. The crude mortality rate of esophagus cancer was 17.19/100,000. The age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 10.80/100,000 and 10.86/100,000 respectively. Incidence and mortality rates of esophagus cancer were higher in males than in females and higher in rural areas than in urban areas. The crude incidence rate in middle areas was the highest among all areas, followed by western areas and eastern areas. The age-specific incidence rate of esophagus cancer was relatively low in age groups before 40 years old and then increased after 45 years old. It peaked in the age group of 80−84 years. The patterns of age-specific mortality rates of esophagus cancer were close to those of age-specific incidence rates. The ASIRC of esophagus cancer decreased dramatically by 29.87% between 2003 and 2012, from 14.33/100,000 to 10.05/100,000. The esophagus cancer incidence rate decreased by 3.76% per year (P>0.05). The mortality rate of esophagus cancer decreased annually over the decades from 2003 to 2012 in China (P>0.05). In females, the annual percentage change (APC) of mortality rate was −5.43% [95% confidence intervals (95% CI): −6.50%, −4.30%] (P<0.05) and the mortality rate of esophagus cancer in rural females was statistically significant (APC: −3.20%, 95% CI: −4.20%, −2.20%) (P<0.05). Conclusions The focus of prevention and treatment for esophagus cancer is strengthening primary prevention of esophageal cancer, and promoting esophagus cancer secondary prevention to reduce incidence and mortality rates of esophagus cancer, prolong survival rate of patients and decline the burden of esophagus cancer in China.
2019, 31(3): 435-442.
doi: 10.21147/j.issn.1000-9604.2019.03.05
Abstract:
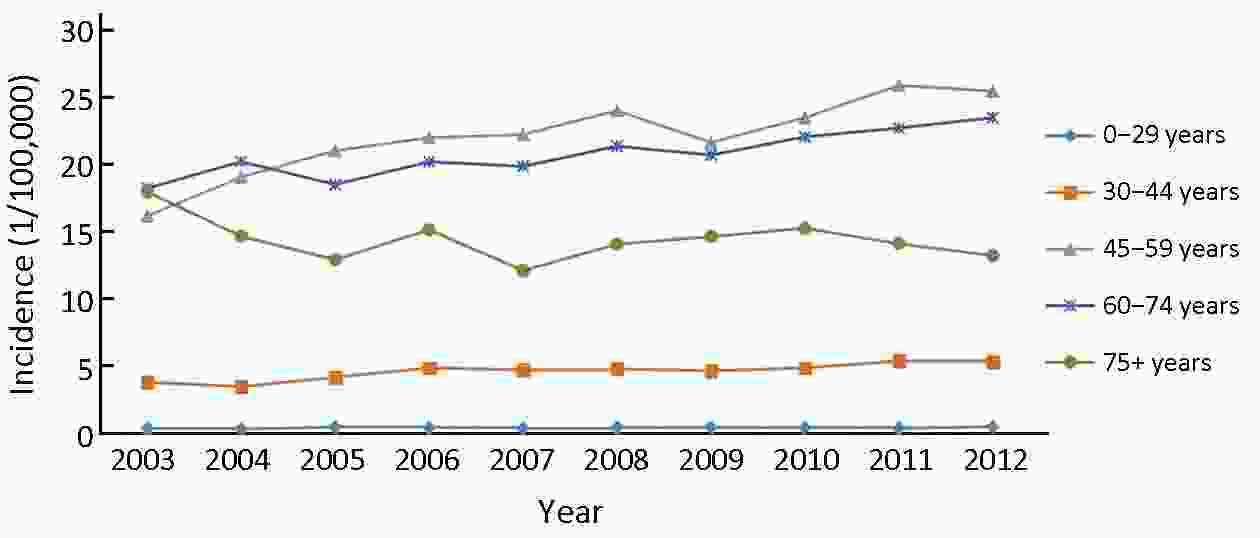
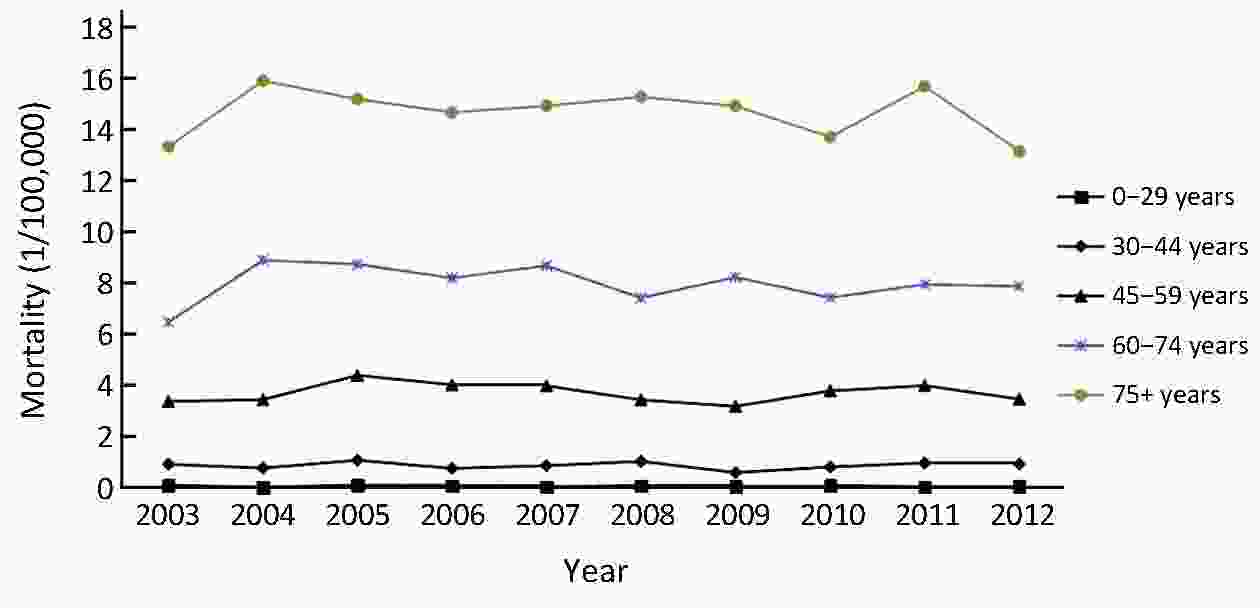
ObjectiveTo analyze the incidence and mortality rates of corpus uteri cancer in China using 2008−2012 data from the National Central Cancer Registry (NCCR) of China. MethodsWe analyzed 2008−2012 data from 135 cancer registries using NCCR screening methods and criteria. The Chinese standard population in 2000 and Segi’s world population were applied to determine age-standardized incidence and mortality rates. The annual percentage change (APC) in rate was calculated using the Joinpoint Regression Program. ResultsThe crude incidence of corpus uteri cancer was 9.58/100,000, making corpus uteri cancer the ninth most common malignancy in females. The crude mortality was 2.97/100,000, making corpus uteri cancer the 13th leading cause of death from malignant tumors in females. The incidence was higher in urban than in rural areas, but the mortality was higher in rural than in urban areas. The crude incidence was higher in eastern areas than in middle and western areas, while the crude mortality was higher in middle areas than in eastern and western areas. During 2003−2012, the age-standardized incidence rate based on the Chinese standard population in 2000 (ASIRC) with uterine cancer increased significantly by 3.0% annually, while the age-standardized mortality rate based on the Chinese standard population in 2000 (ASMRC) decreased by 0.4% annually, but the decrease was not statistically significant. The APC in incidence rate in the age groups of 30−44 years was 4.2%, which was statistically significant; increases/decreases in other age groups were not statistically significant. From 2003 to 2004, the age groups of 60−74 years showed high incidence, while from 2005 to 2012, the age groups of 45−59 years had high incidence. ConclusionsThe incidence and mortality rates of corpus uteri cancer in China from 2008 to 2012 were relatively low compared with other countries. However, the significant increase in incidence rates and marked decrease in patient age suggest the need to strengthen China’s efforts toward prevention and control of corpus uteri cancer.
2019, 31(3): 443-452.
doi: 10.21147/j.issn.1000-9604.2019.03.06
Abstract:
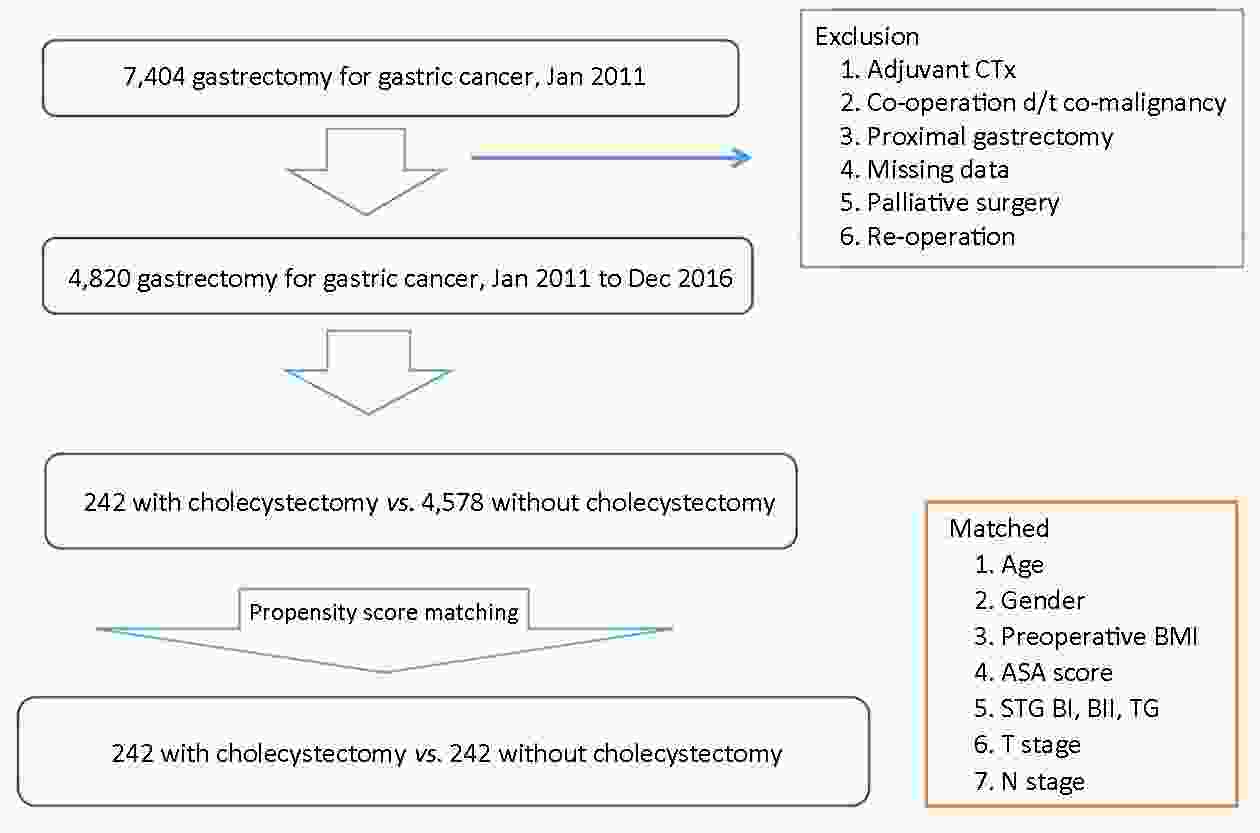
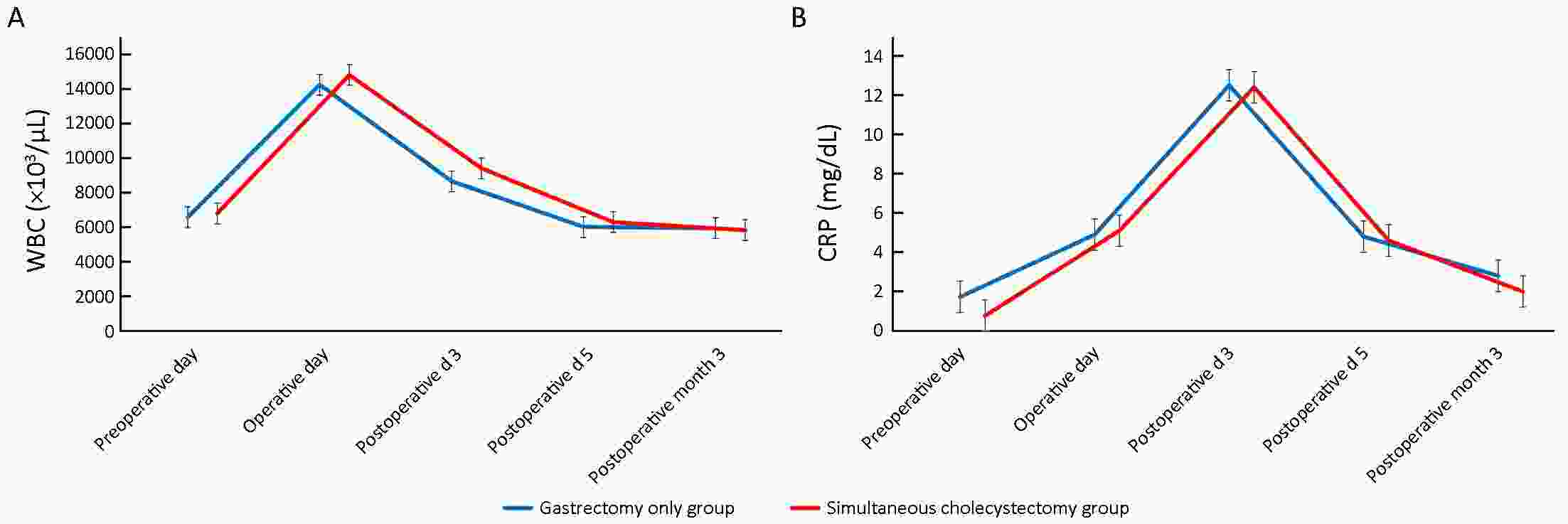
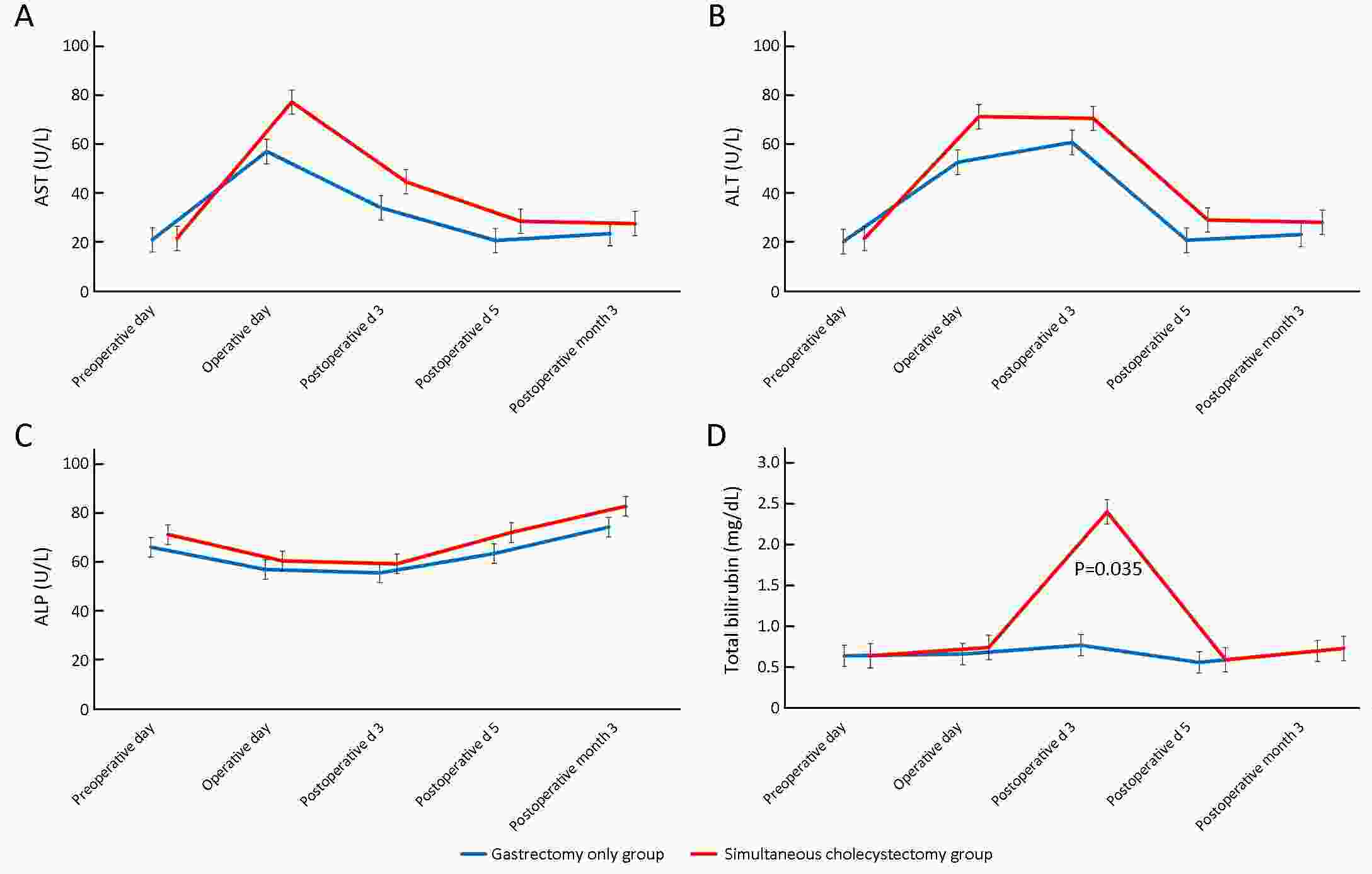
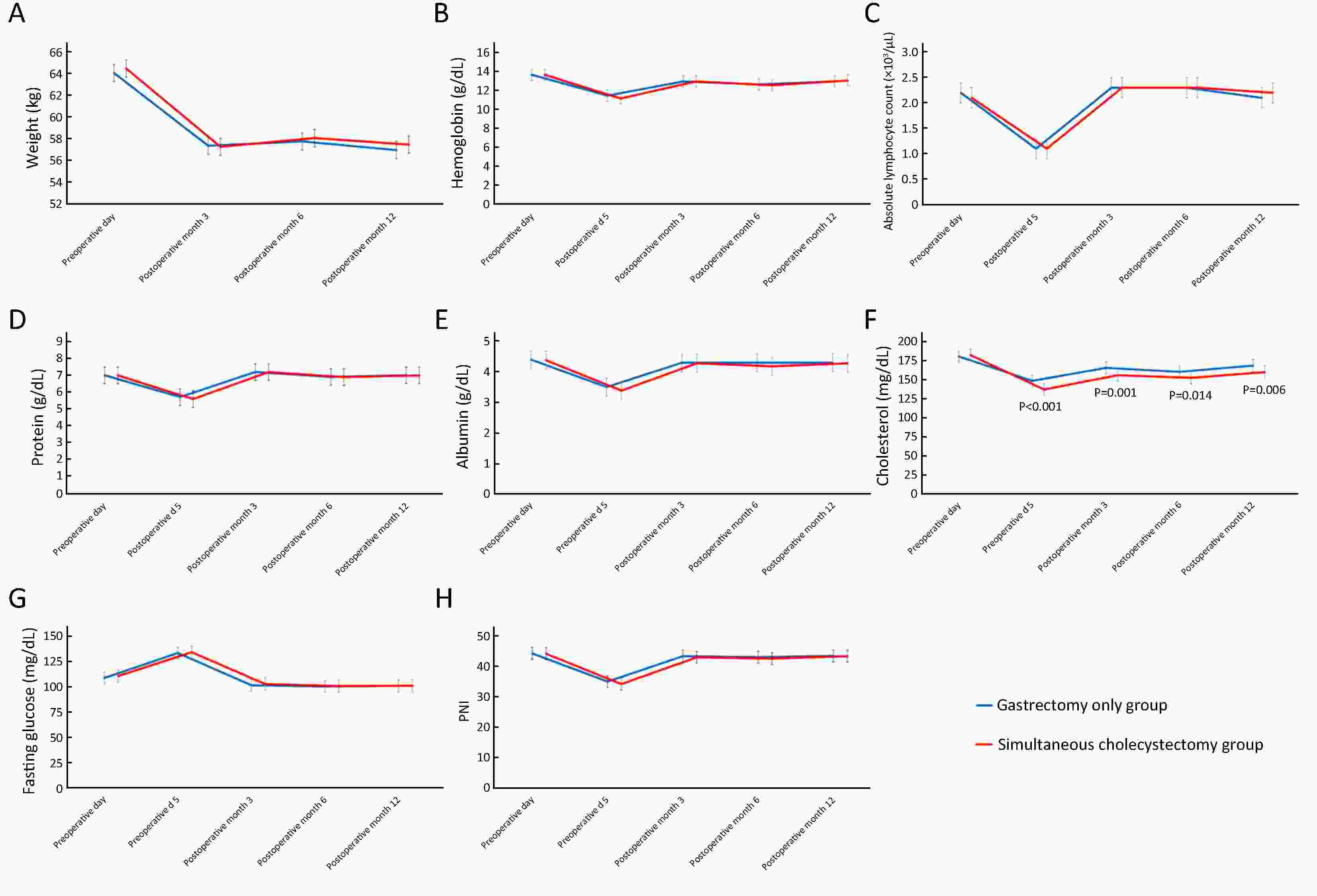
ObjectiveWe aimed to evaluate the effect of simultaneous cholecystectomy on the short-term postoperative outcomes and nutritional status in patients with gastric cancer. MethodsWe retrospectively reviewed data from 4,820 patients with gastric cancer who underwent gastrectomy from January 2011 to December 2016. Patients who underwent only gastrectomy (N=4,578) were matched to those who underwent simultaneous cholecystectomy during gastrectomy (N=242) at a 1:1 ratio using propensity score matching analysis. The nutritional status and inflammatory responses preoperatively and postoperatively and postoperative outcomes were compared between the groups. ResultsThe simultaneous cholecystectomy group showed more intraoperative blood loss and a longer operative time than the gastrectomy only group [150.0 (100.0, 200.0) mL vs. 100.0 (100.0, 200.0) mL, P=0.006; 176.0 (150.0, 210.0) min vs. 155.0 (128.0, 188.0) min, P<0.001, respectively]. Intraoperative event rate, postoperative complication rate, and postoperative recovery did not differ between the groups. All parameters including body weight, the hemoglobin level, absolute lymphocyte count, total protein level, albumin level, fasting glucose level, and prognostic nutritional index excluding the cholesterol level were not significantly different between the groups, and their changing patterns were similar. Although the cholesterol level was significantly lower in the simultaneous cholecystectomy group than in the gastrectomy only group at all follow-up points, the mean value of the decreased cholesterol level was within normal range. ConclusionsIn gastric cancer patients with gallbladder disease, simultaneous cholecystectomy is safe and not associated with additional nutritional loss.
2019, 31(3): 453-461.
doi: 10.21147/j.issn.1000-9604.2019.03.07
Abstract:
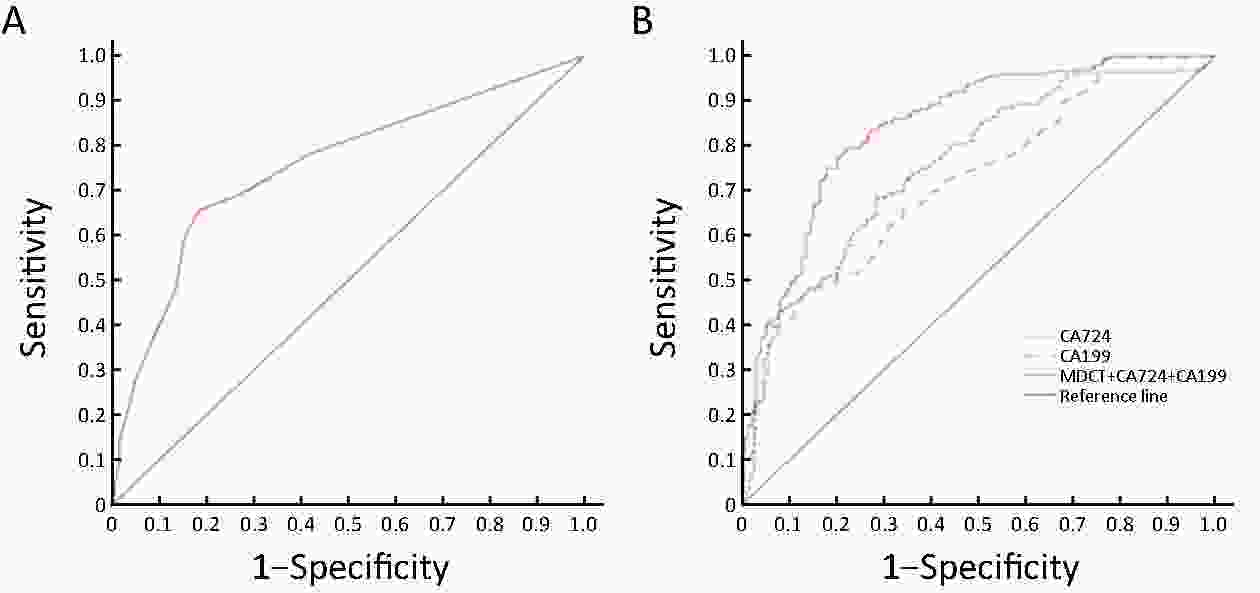
Objective Multidetector-row computed tomography (MDCT) and serum tumor biomarkers are commonly used to evaluate the preoperative lymph node metastasis and the clinical staging of gastric cancer (GC). This study intends to evaluate the clinical predictive value of MDCT and serum tumor biomarkers in lymph node metastasis of GC. Methods The clinicopathologic data of 445 GC patients who underwent radical gastrectomy were retrospectively analyzed to evaluate the diagnostic value of MDCT and serum tumor biomarkers in lymph node metastatic staging of GC before surgery. Results With the multinomial logistic regression analysis, the independent relative factors of lymph node metastasis of GC were identified as tumor size, depth of tumor invasion, vessel invasion, vascular embolus, and soft tissue invasion. The optimal critical value of the short diameter of lymph nodes detected by MDCT scanning for evaluation of preoperative lymph node metastasis was 6.0 mm, with 75.7% as predictive accuracy of lymph node metastasis compared to the postoperative pathological results of GC patients. In addition, the critical value of the short diameter of lymph nodes combined with serum tumor biomarkers [including carbohydrate antigen (CA)-724 and CA-199] could show an enhancement of predictive sensitivity of lymph node metastasis (up to 89.3%) before surgery. Conclusions MDCT combined with serum tumor biomarkers should be adopted to improve preoperative sensitivity and accuracy of lymph node metastasis for GC patients.
2019, 31(3): 463-470.
doi: 10.21147/j.issn.1000-9604.2019.03.08
Abstract:
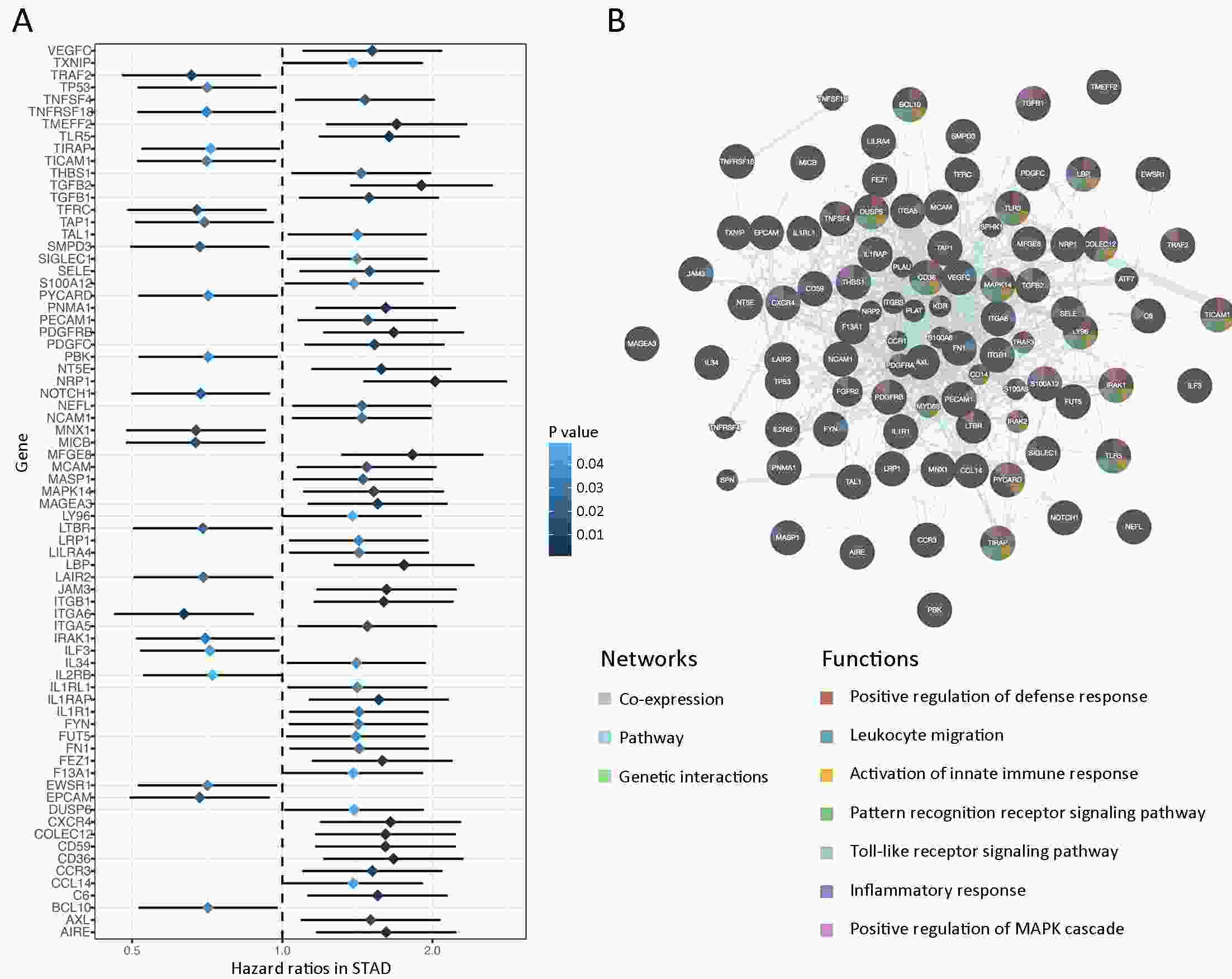
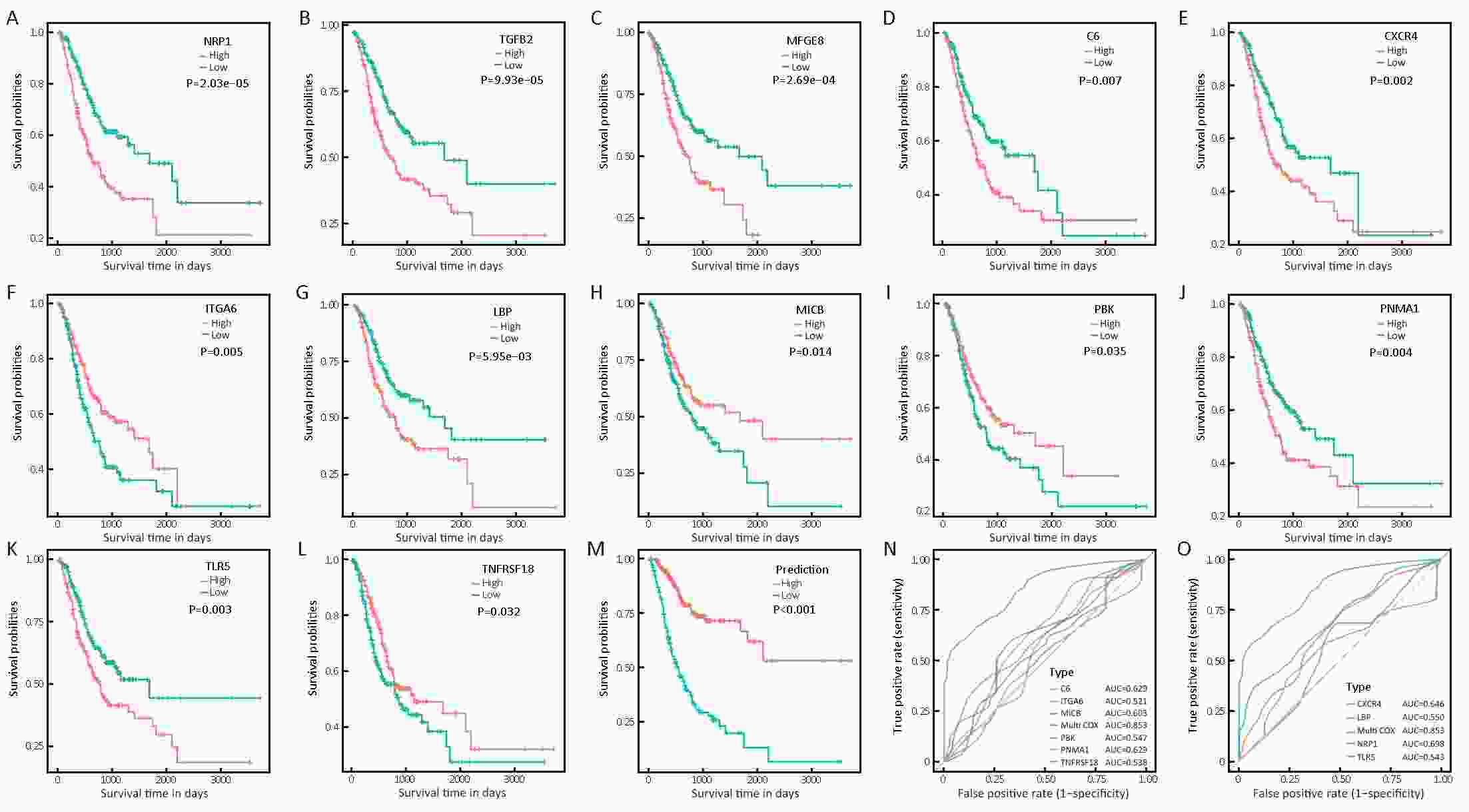
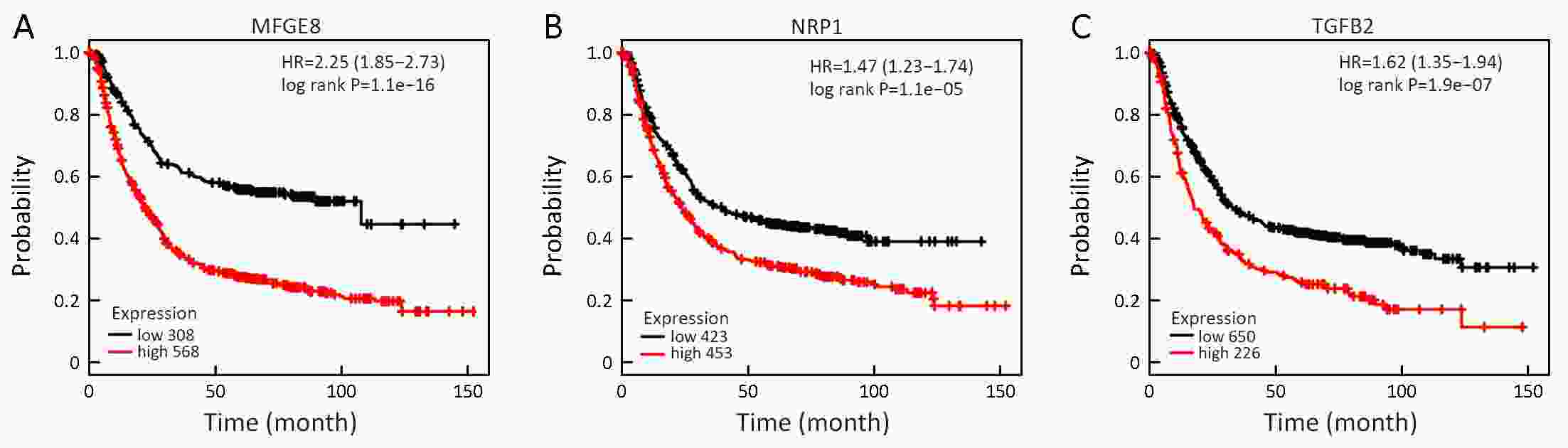
ObjectiveTumor microenvironment, especially the host immune system, plays a pivotal role in tumor initiation and progression. Profiling of immune signature within tumor might uncover biomarkers for targeted therapies and clinical outcomes. However, systematic analysis of immune-related genes in gastric cancer (GC) has not been reported. MethodsExpressions of a total of 718 immune-related genes were generated in 372 stomach adenocarcinoma (STAD) patients from The Cancer Genome Atlas (TCGA) database using RNA-sequencing data. Integrated bioinformatics analyses were performed to identify prognostic factors as well. ResultsSurvival analyses revealed 73 genes, which were significantly associated with patient’s overall survival (OS). Taken together with clinicopathological parameters, we established a predictive model, containing 10 immune-related genes, which were NRP1, C6, CXCR4, LBP, PNMA1, TLR5, ITGA6, MICB, PBK and TNFRSF18, with powerful efficiency in distinguishing satisfactory or poor survival of STAD patients. Moreover, the top 3 ranked prognostic genes, NRP1, TGFβ2 and MFGE8, were also significantly associated with patient’s OS by an independent validation achieved from Kaplan-Meier plotter database. ConclusionsWe profiled prognostic immune signature and established prognostic predictive model for GC, which could reflect immune disorders within tumor microenvironment, and also may provide novel predictive and therapeutic targets for GC patients in the near future.
2019, 31(3): 471-480.
doi: 10.21147/j.issn.1000-9604.2019.03.09
Abstract:
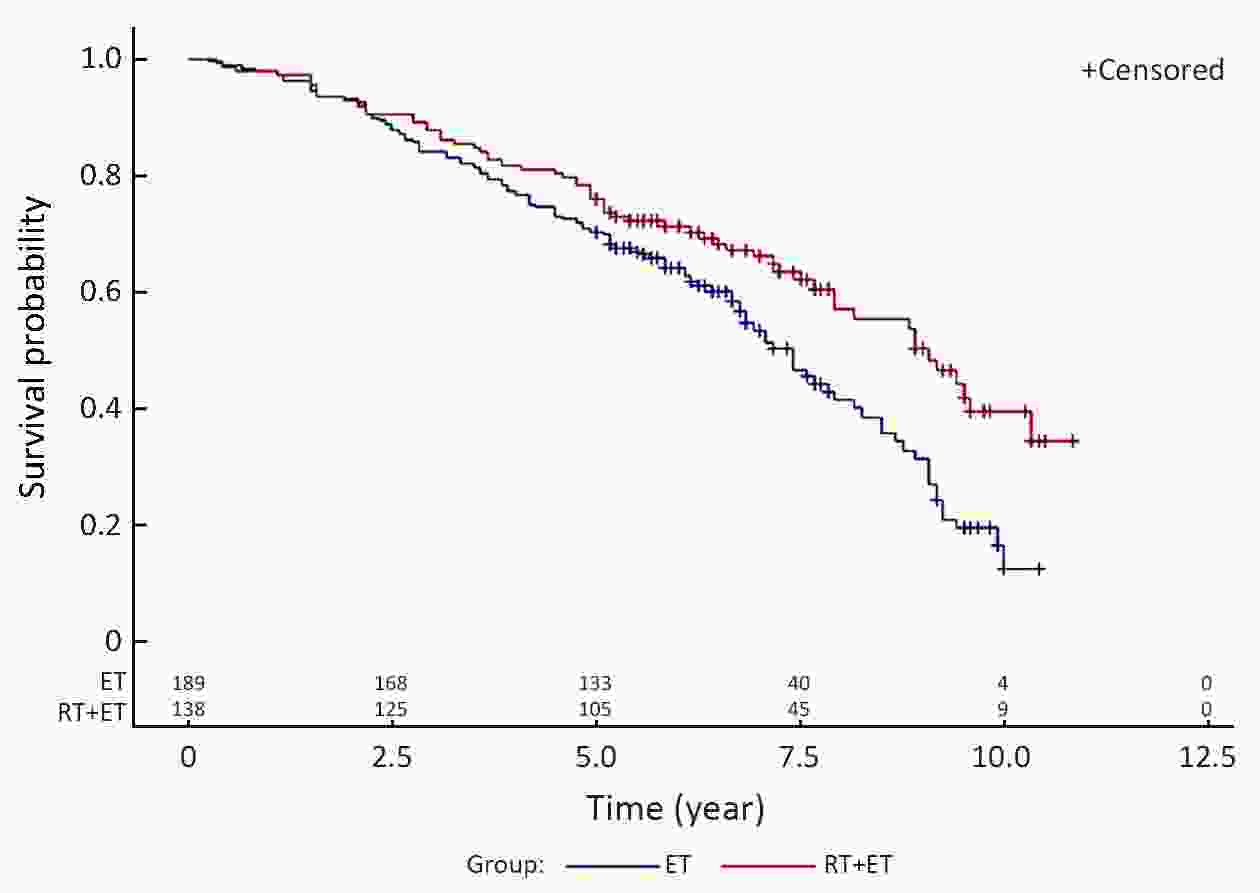
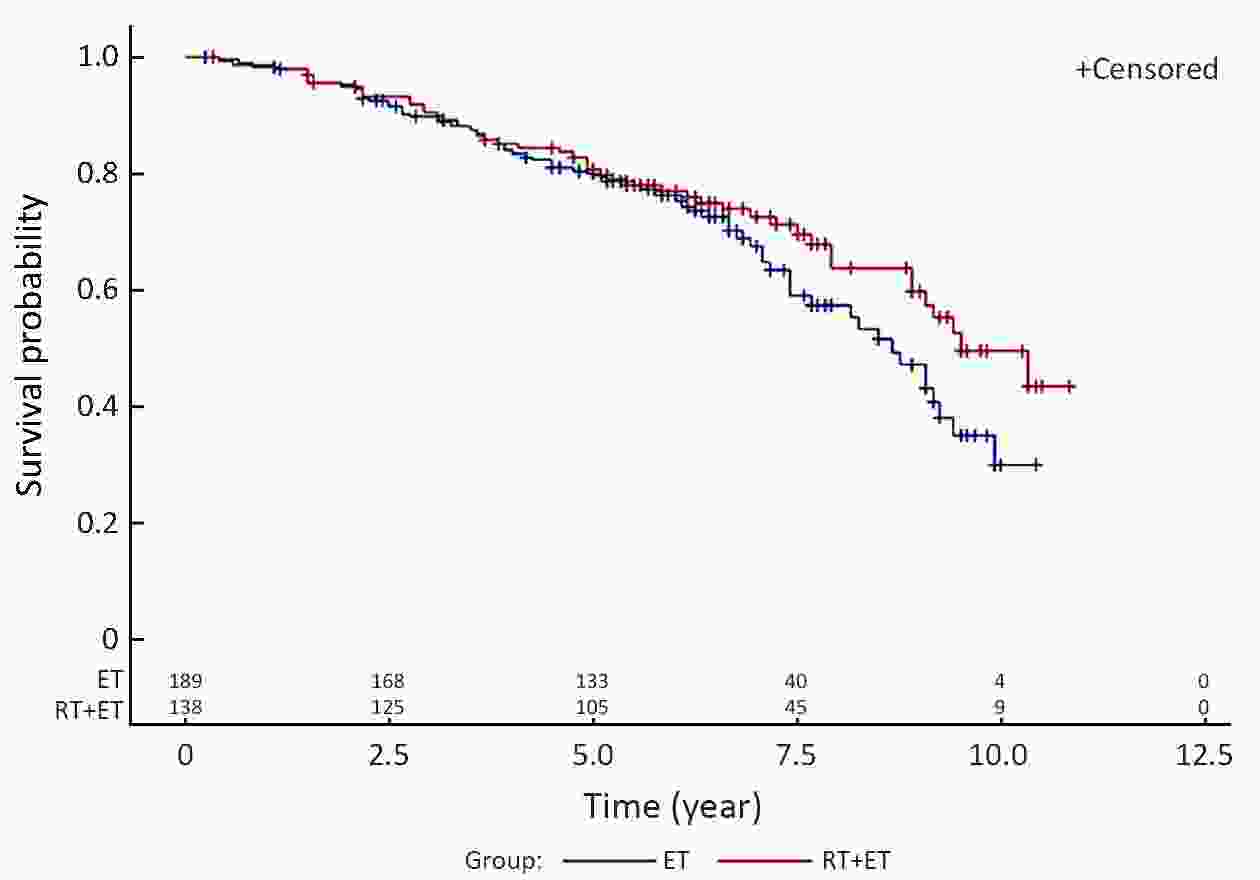
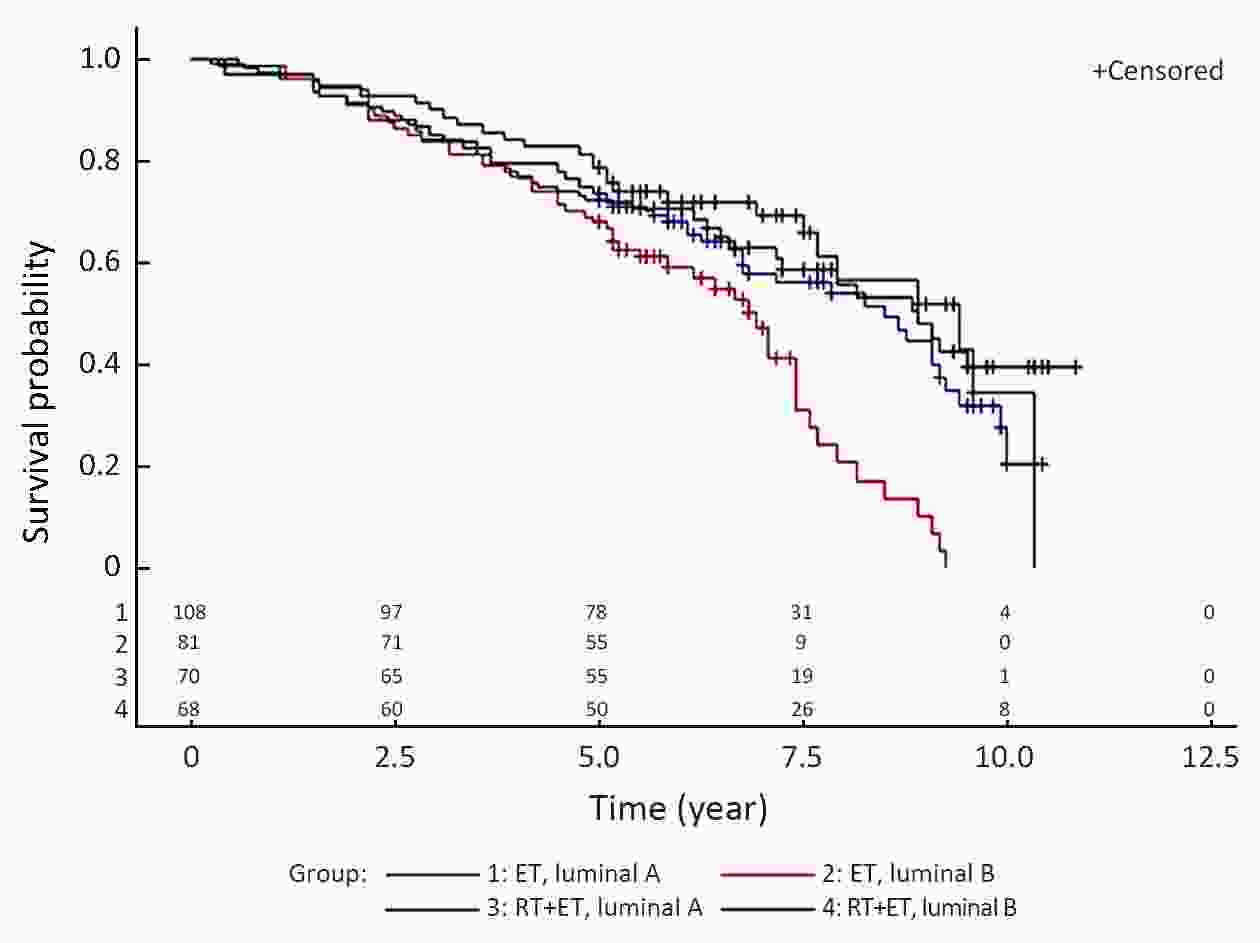
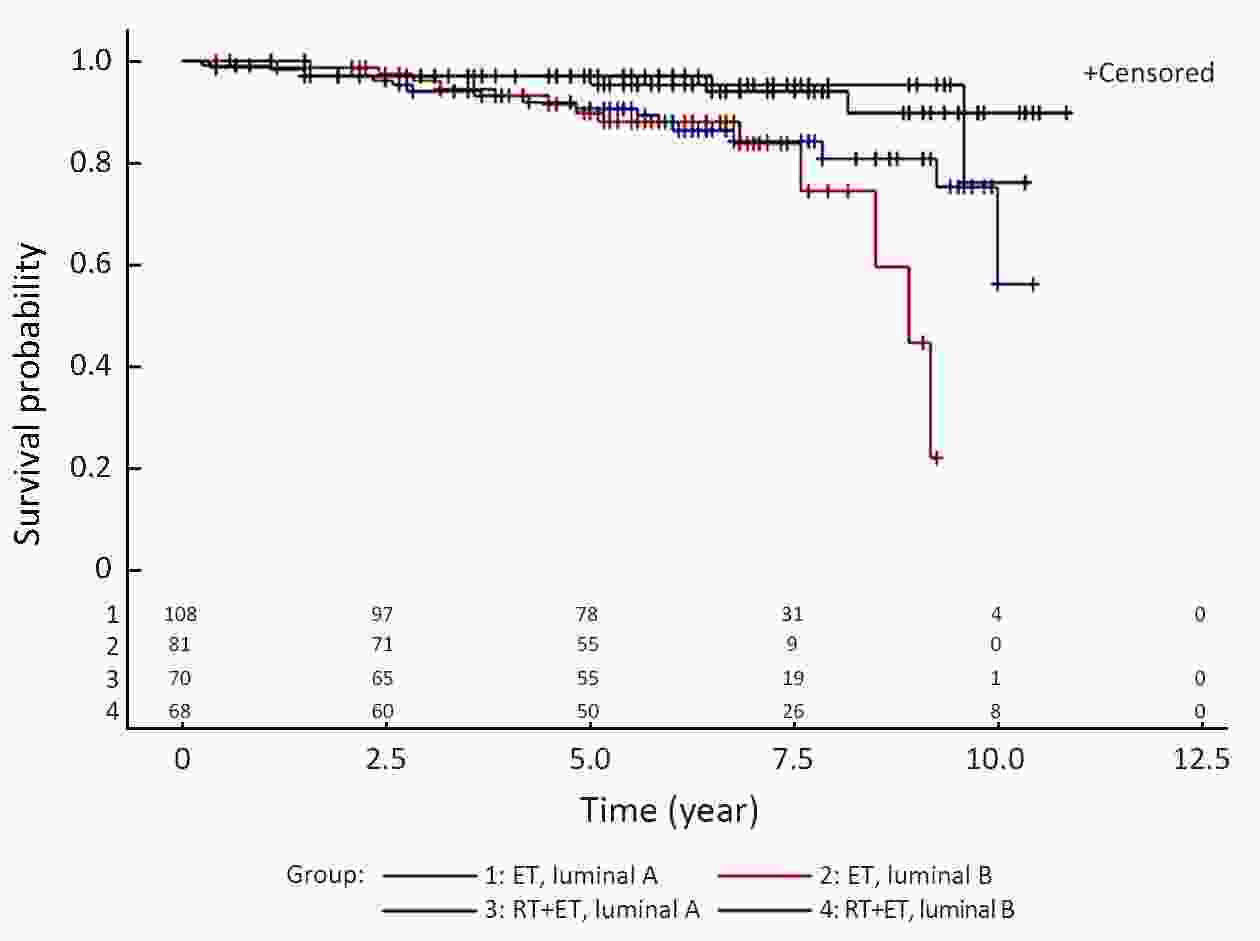
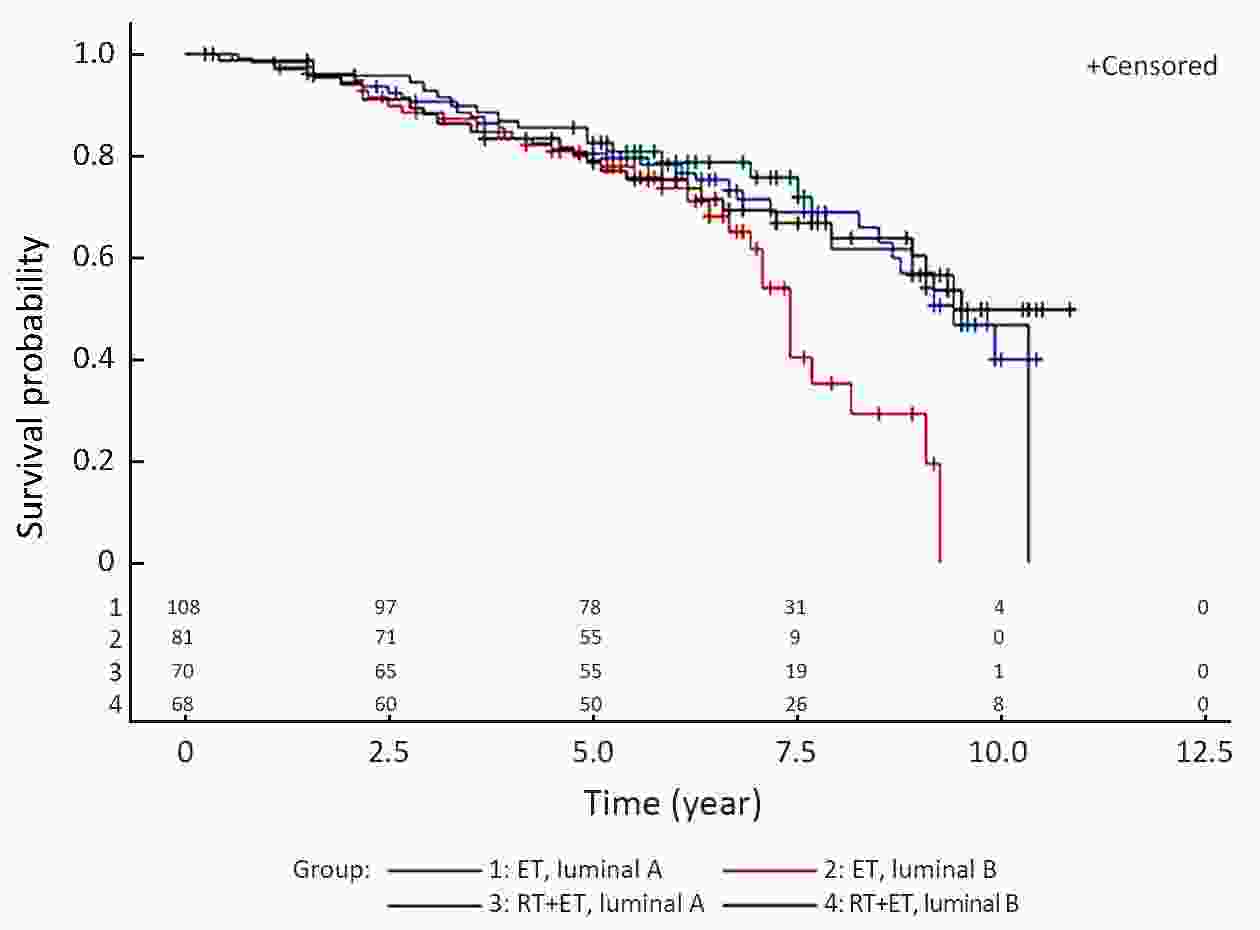
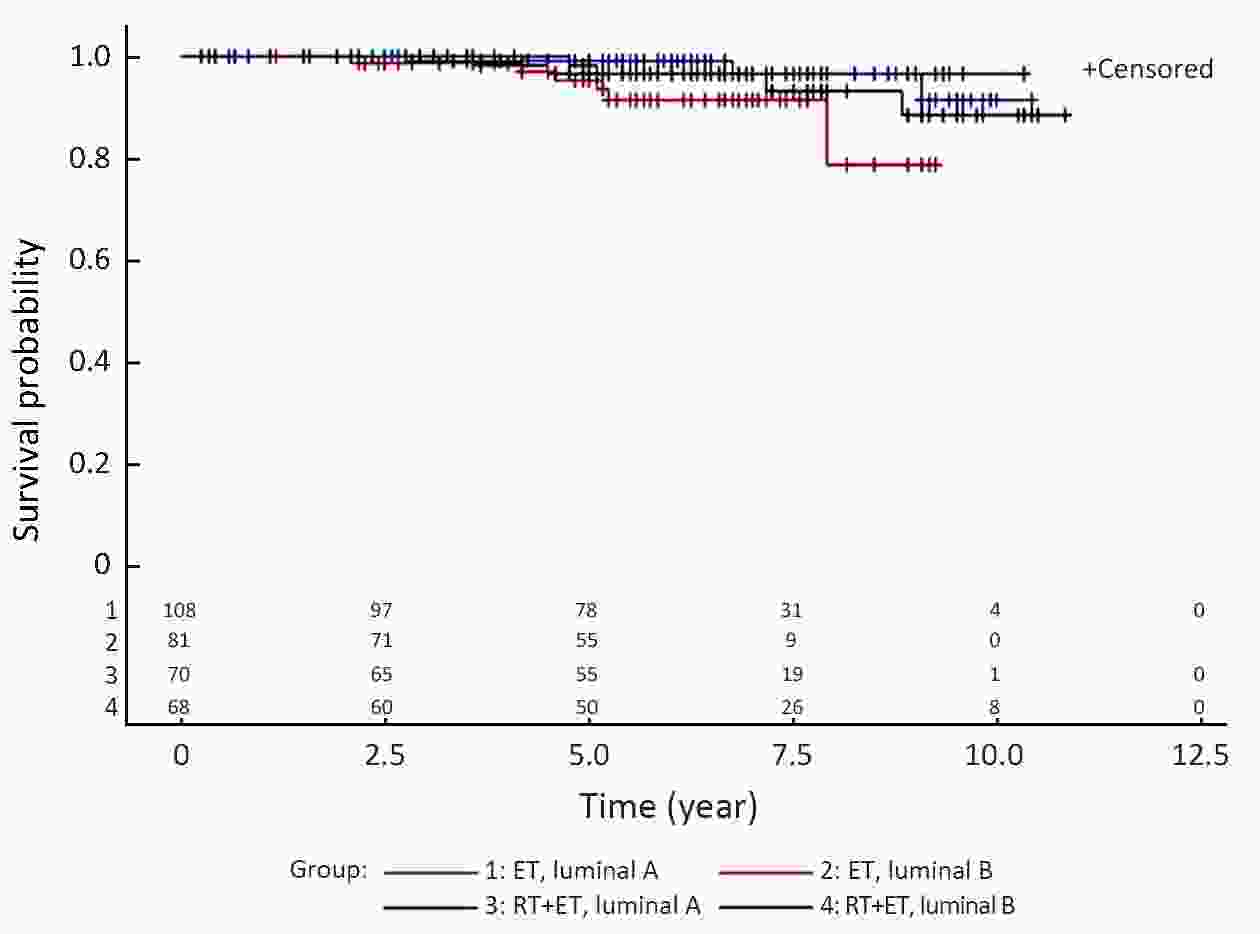
Objective The present study examined the effect of radiotherapy on recurrence and survival in elderly patients with hormone receptor-positive early breast cancer. Methods A retrospective analysis of 327 patients aged ≥65 years, with stage I−II, hormone receptor-positive breast cancer who underwent breast-conserving surgery and received endocrine therapy (ET) or radiotherapy plus endocrine therapy (ET+RT) was performed. Both groups were divided into luminal A type and luminal B type subgroups. Evaluation criteria were 5-year disease-free survival (DFS), local relapse rate (LRR), overall survival (OS), and distant metastasis rate (DMR). Results There were significant differences in 5-year DFS [hazard ratio (HR)=1.59, 95% confidence interval (95% CI), 1.15−2.19; P=0.005] and LRR (HR=3.33, 95% CI, 1.51−7.34; P=0.003), whereas there were no significant differences in OS and DMR between ET group and ET+RT group. In luminal A type, there was no significant difference in 5-year DFS, LRR, OS and DMR between ET group and ET+RT group. In luminal B type, there were statistically significant differences in 5-year DFS (HR=2.19, 95% CI, 1.37−3.49; P=0.001), LRR (HR=5.45, 95% CI, 1.65−17.98; P=0.005), and OS (HR=1.75, 95% CI, 1.01−3.05; P=0.048) between ET group and ET+RT group. In the ET group, there were significant differences between luminal A type and luminal B type in 5-year DFS (HR=1.84, 95% CI, 1.23−2.75; P=0.003) and OS (HR=1.76, 95% CI, 1.07−2.91; P=0.026). Conclusions After breast-conserving surgery, radiotherapy can reduce the LRR and improve the DFS and OS of luminal B type elderly patients, whereas luminal A type elderly patients do not benefit from radiotherapy. Without radiotherapy, luminal A type patients have better DFS and OS than luminal B type patients.
2019, 31(3): 481-488.
doi: 10.21147/j.issn.1000-9604.2019.03.10
Abstract:
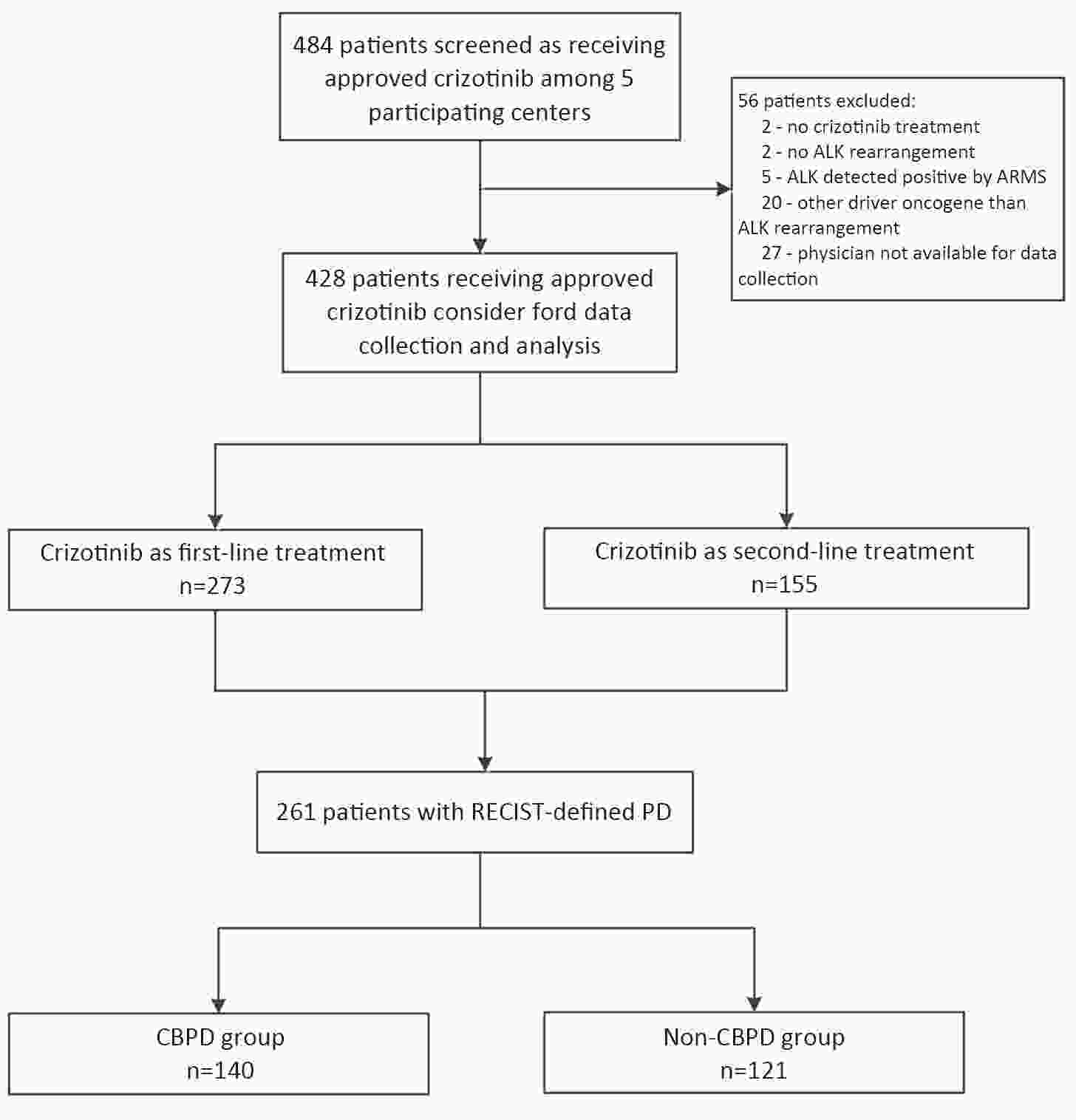
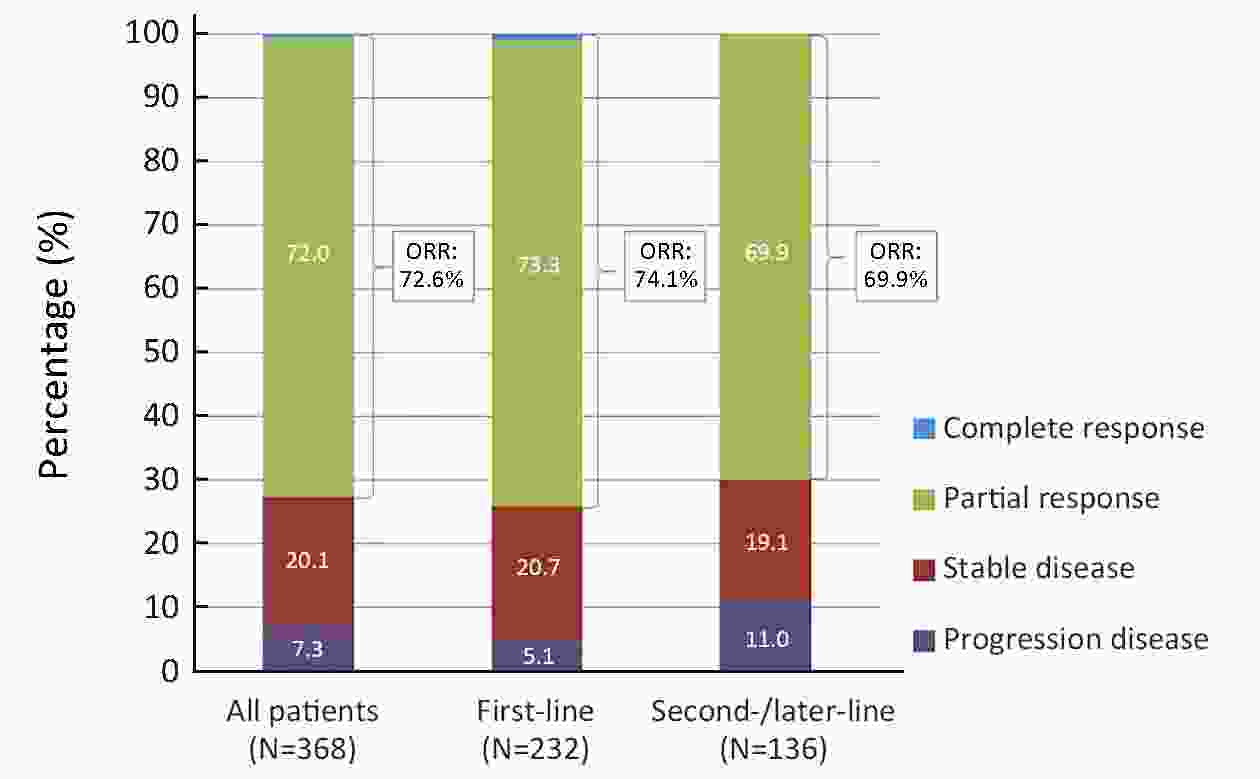
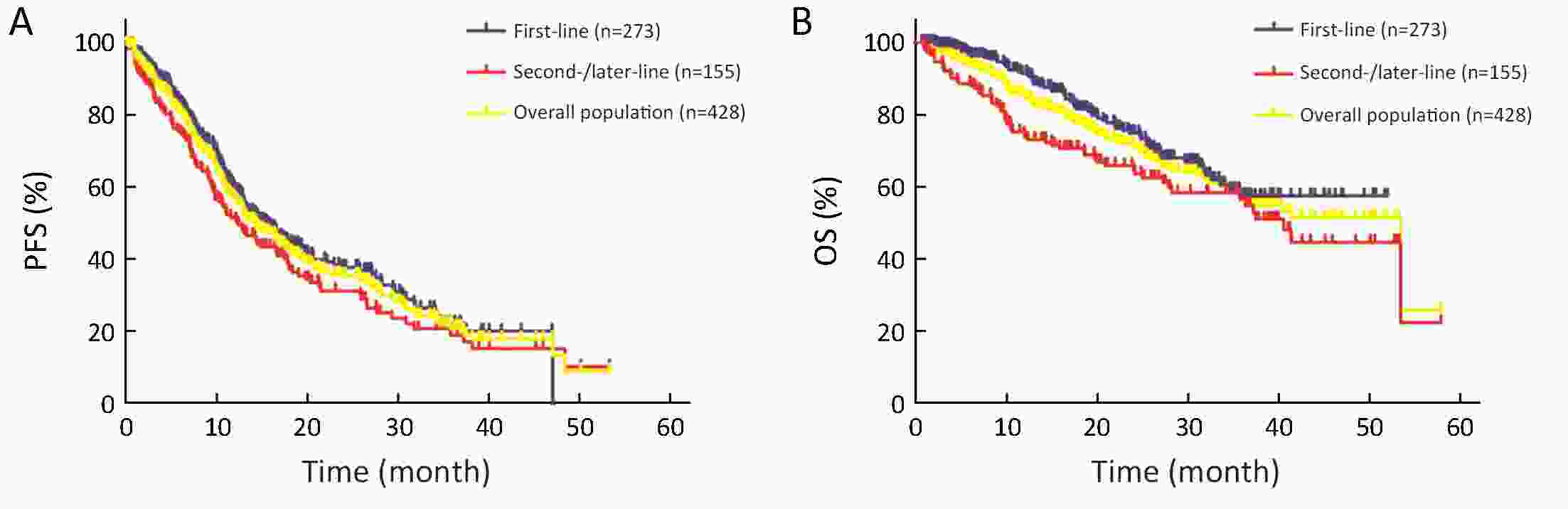
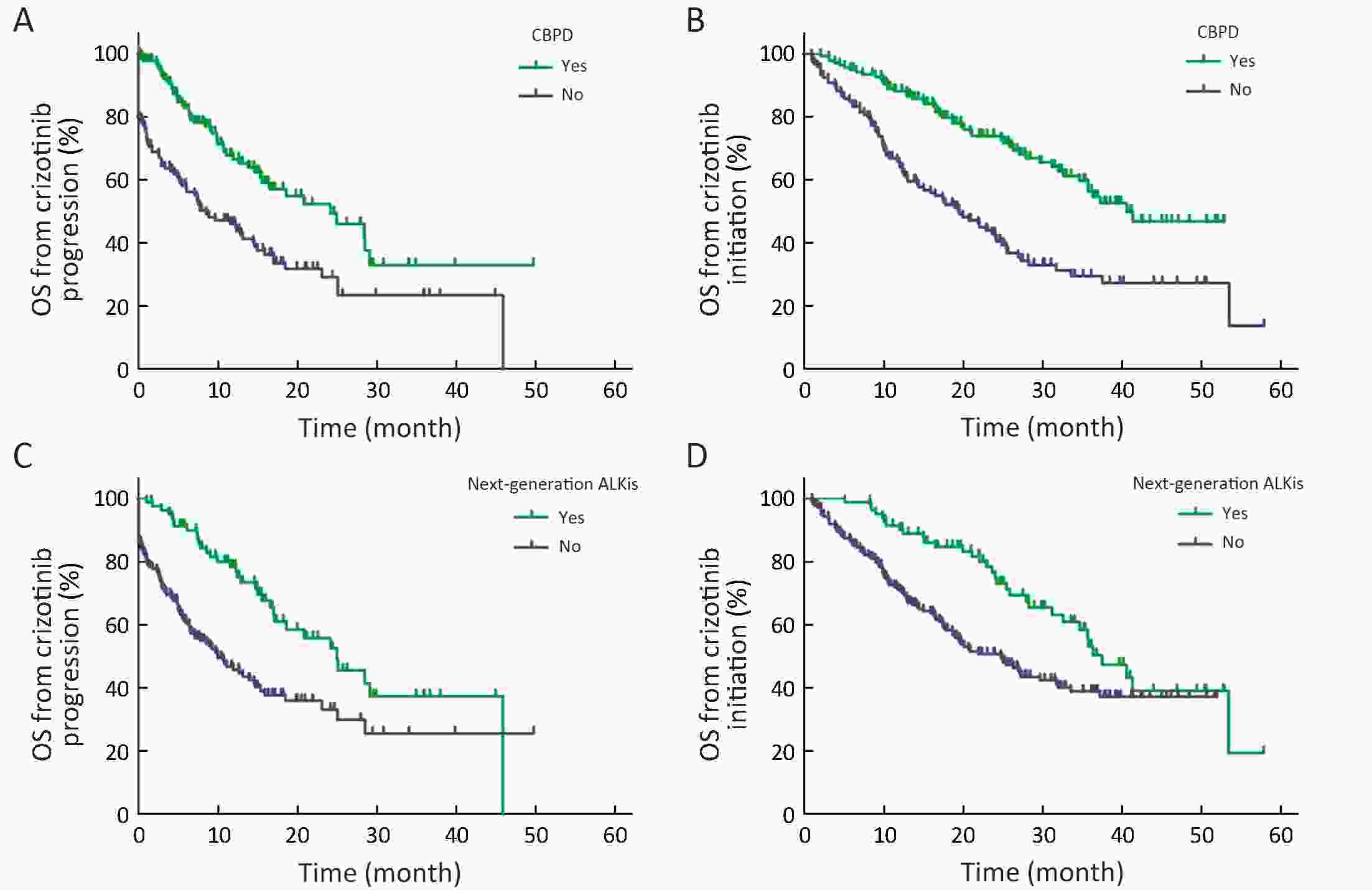
Objective Crizotinib has demonstrated promising efficacy in patients with anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer (NSCLC) in clinical trials. We conducted this retrospective multicenter study to assess the outcomes of crizotinib therapy in, to our knowledge, a large sample cohort of patients with ALK-positive advanced NSCLC. Methods We reviewed the medical records of 484 unselected ALK-positive NSCLC patients treated with crizotinib at 5 cancer centers in China from January 2013 to November 2017. Clinical data were collected from the initiation of crizotinib therapy to Response Evaluation Criteria in Solid Tumors (RECIST)-defined progressive disease (PD). Results A total of 428 eligible ALK-positive NSCLC patients were enrolled, 273 (63.8%) of whom received crizotinib as first-line treatment. The median progression-free survival (PFS) and overall survival (OS) from the initiation of crizotinib treatment were 14.4 [95% confidence interval (95% CI), 12.4−16.4] months and 53.4 (95% CI, 33.7−73.1) months, respectively. In subgroup analyses, patients who received crizotinib as first-line treatment showed a higher disease control rate (DCR) and a longer median OS compared with second-/later-line crizotinib treatment (94.8% and OS not reached vs. 89.0% and 40.5 months, respectively). For 261 patients with RECIST-defined PD, multivariate Cox analysis revealed that in patients who received first-line crizotinib therapy, continued crizotinib beyond progressive disease (CBPD) and next-generation ALK inhibitors after crizotinib failure were associated with improved survival. Conclusions This study has demonstrated the clinically meaningful benefit of crizotinib treatment in a large cohort of Chinese ALK-positive NSCLC patients. CBPD and next-generation ALK inhibitor treatment may provide improved survival after RECIST-defined progression on crizotinib.
2019, 31(3): 489-498.
doi: 10.21147/j.issn.1000-9604.2019.03.11
Abstract:
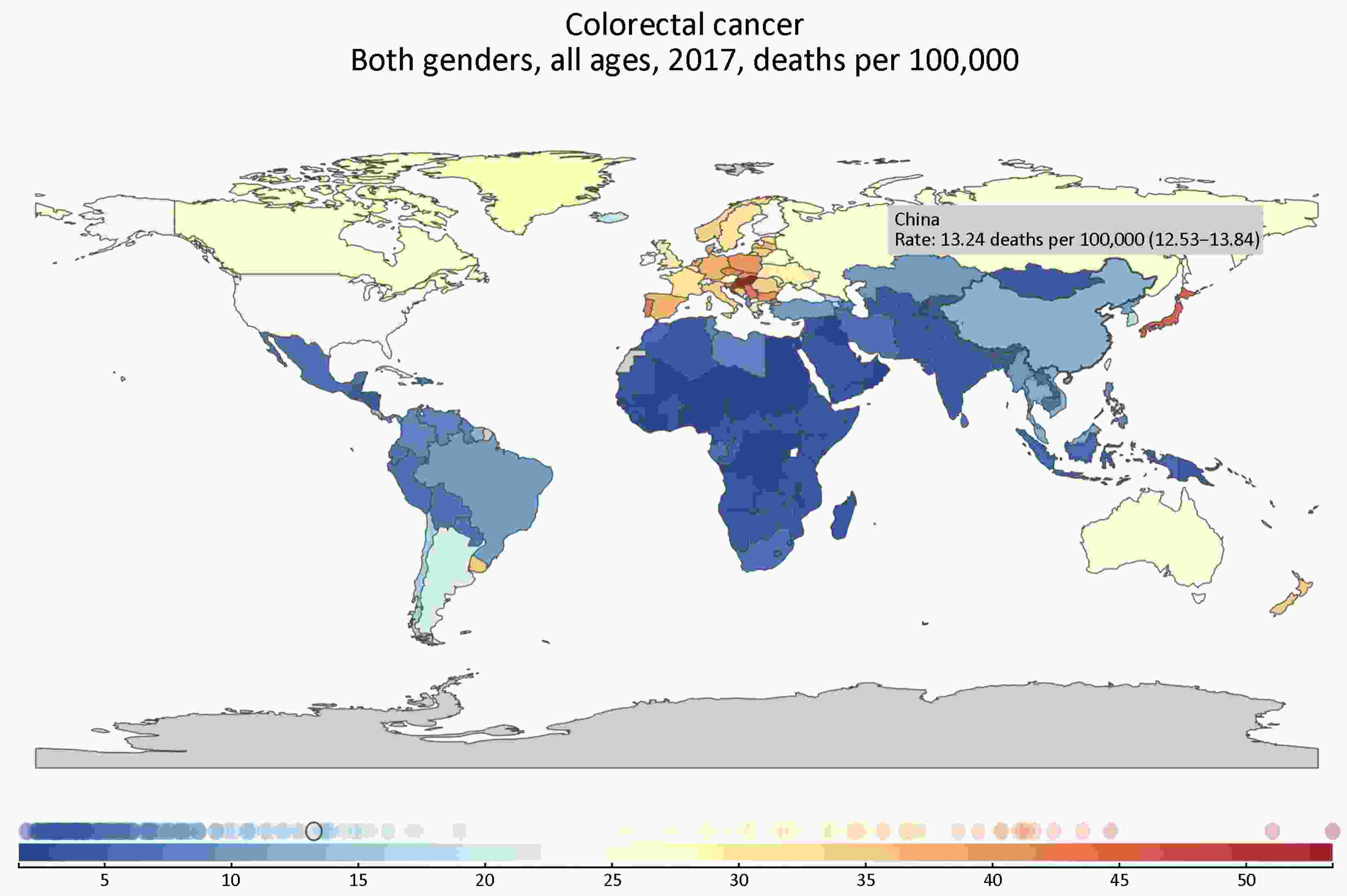
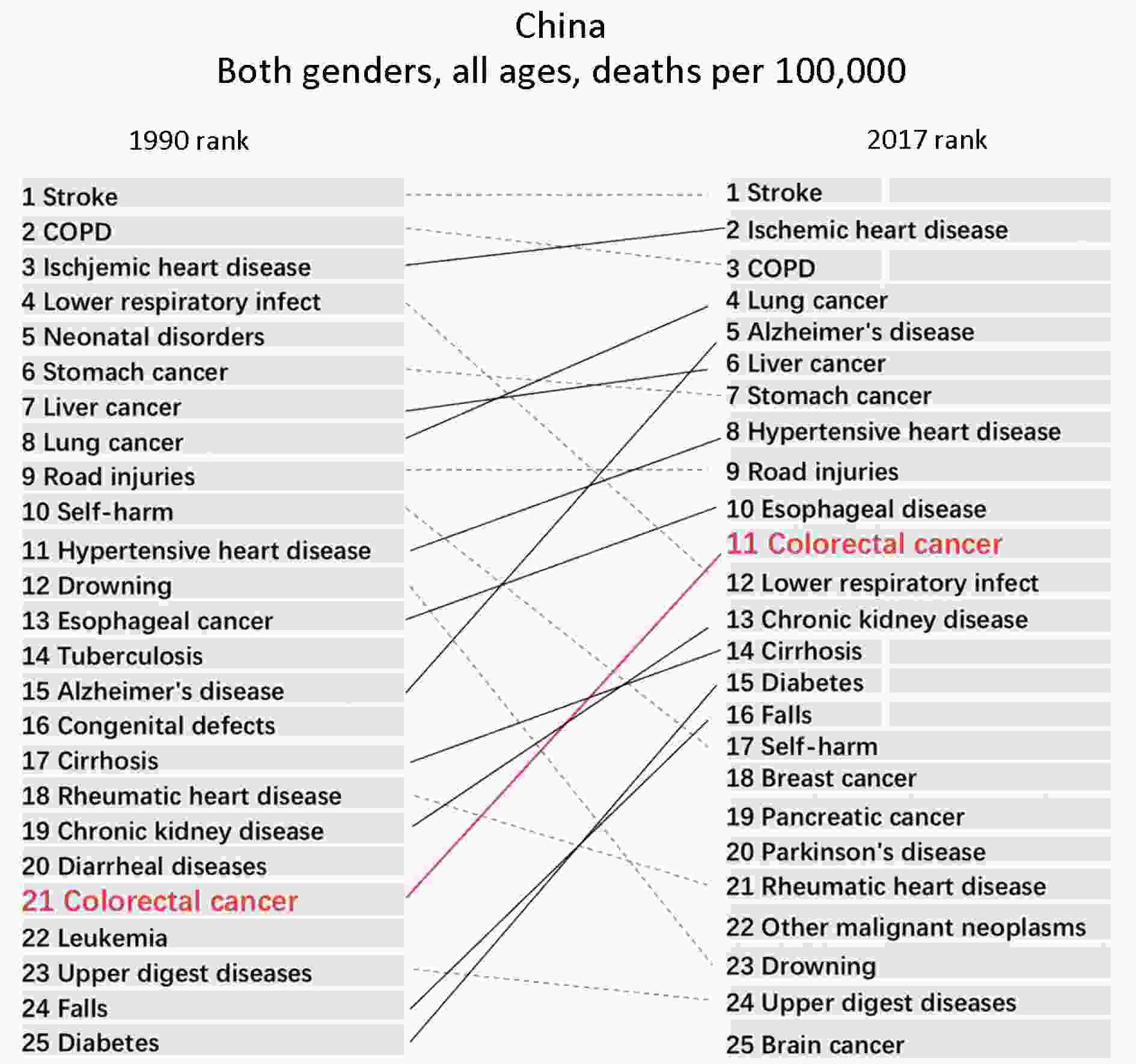
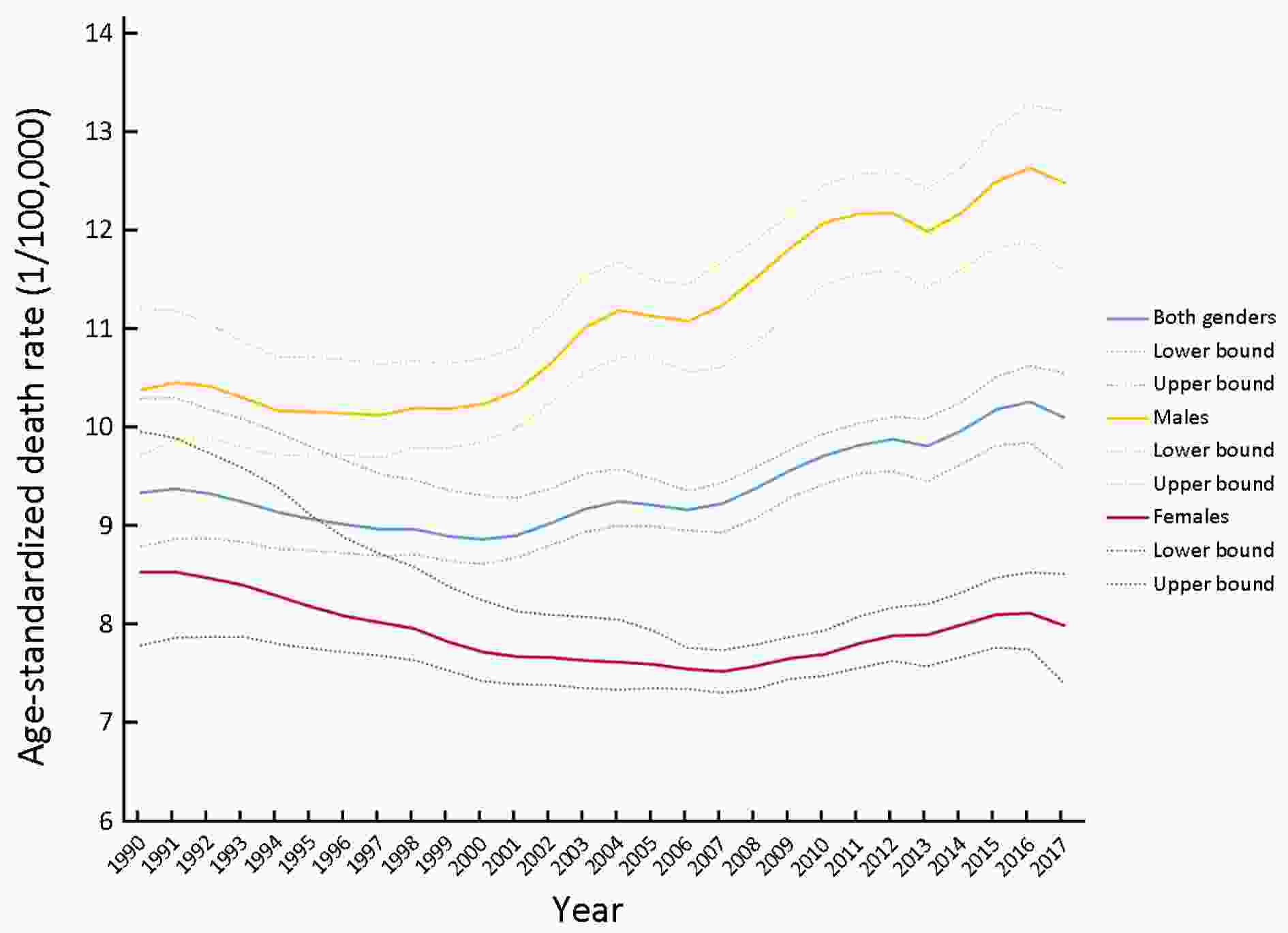
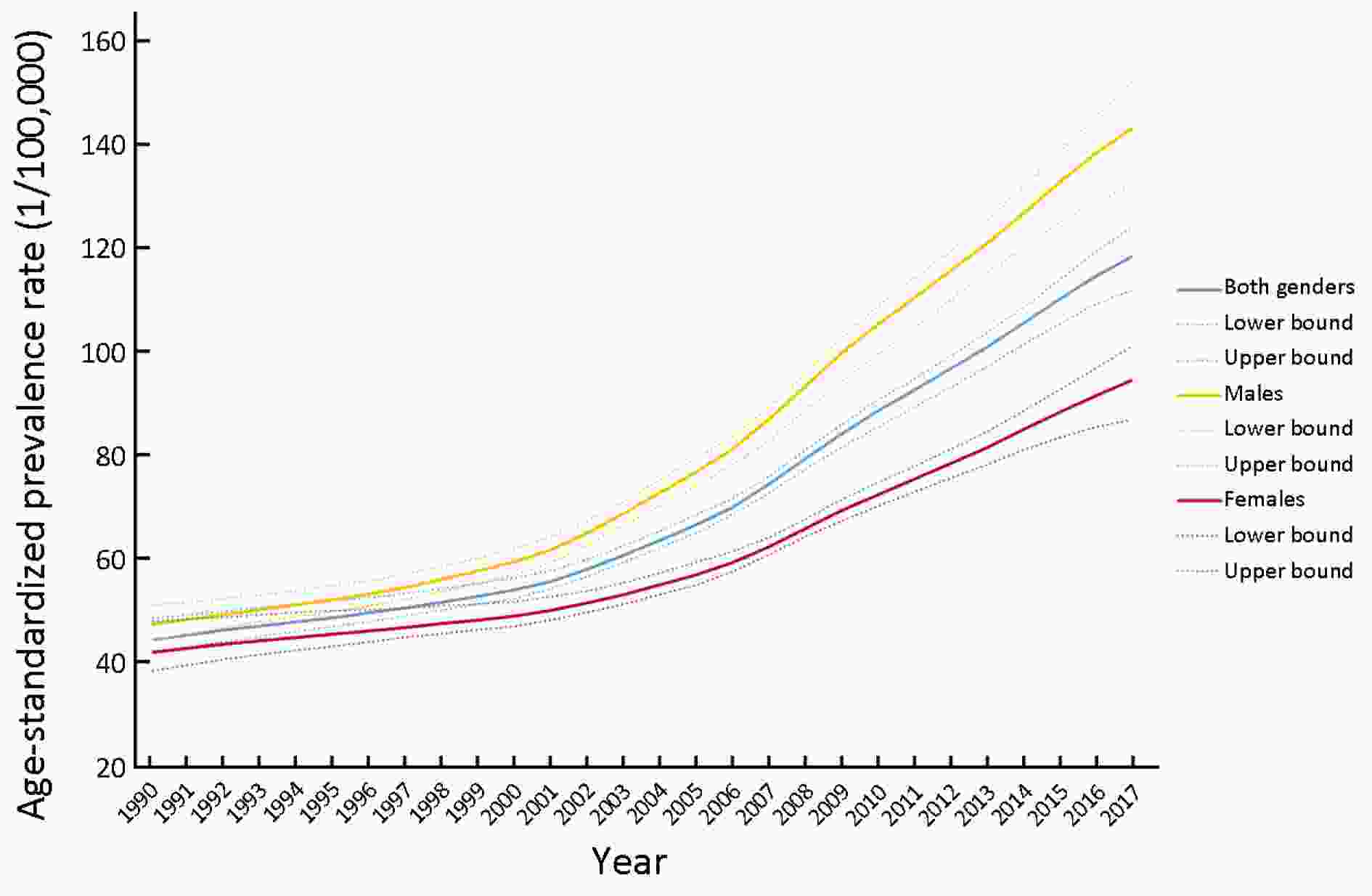
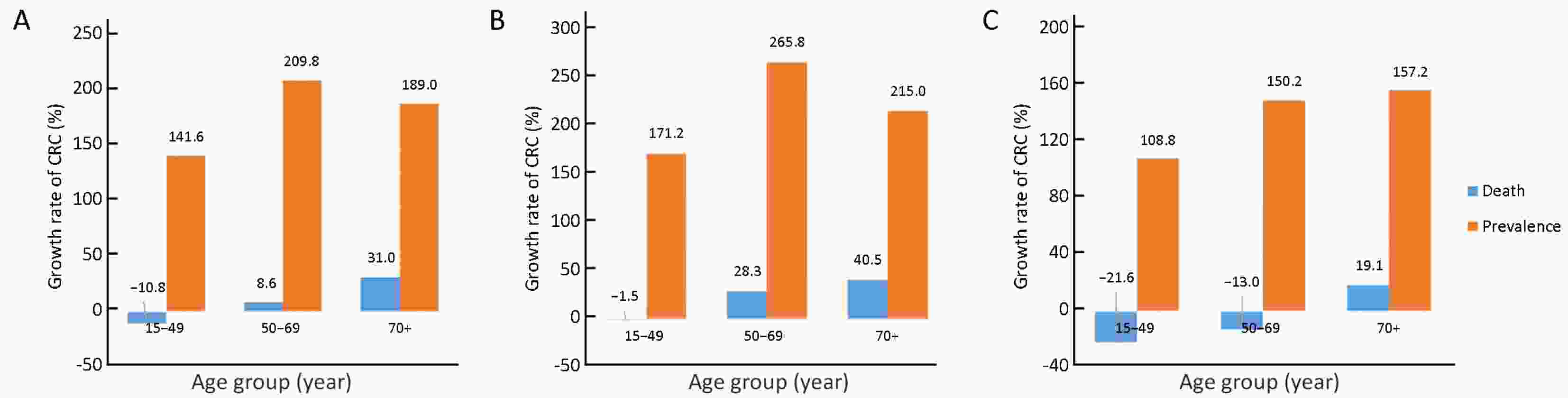
ObjectiveOur goal is to analyze the trend of colorectal cancer (CRC) regarding the death, incidence and prevalence rates over time, and to provide epidemiological knowledge basis for health policy revision by comparing data about fatal outcomes of CRC in 2017 to those data in 1990, which was extracted from the Global Burden of Disease (GBD). MethodsThe time trend and changes of CRC burden from 1990 to 2017 were measured by using the methods and results from the Institute for Health Metrics and Evaluation (IHME) GBD 2017, based on the rates of death, incidence and prevalence. ResultsThe death rate of CRC is 13.24/100,000, accounting for 1.79% of total deaths in China in 2017. In 1990, CRC ranked 21st in all causes of death in China compared to its 11th ranking in 2017. The death, incidence and prevalence rate of CRC were standardized by the age scale of the global population in 2010, the change of standardized death rate of CRC was not significant, from 9.33/100,000 in 1990 to 10.10/100,000 in 2017. The standardized incidence rate of CRC significantly increased from 12.18/100,000 in 1990 to 22.42/100,000 in 2017. The standardized prevalence rate of CRC significantly increased from 44.55/100,000 in 1990 to 118.40/100,000 in 2017. The trend of the prevalence rate in both genders grow higher in 2017 compared to the 1990, resulting in 141.6%, 209.8% and 189.0% for the studied three age groups (15−49, 50−69 and 70+ years old), respectively. The death rate increased in the age groups of 50−69 and 70+ years in both genders (8.6% and 31.0% respectively), in contrast to a decrease of death rate in the age group of 15−49 years old (−10.8%). ConclusionsChina experienced a stunning increase in terms of incidence and prevalence rate of CRC from 1990 to 2017. To decrease the burden of CRC, prevention and management of known risk factors should be promoted through national polices.
2019, 31(3): 499-510.
doi: 10.21147/j.issn.1000-9604.2019.03.12
Abstract:
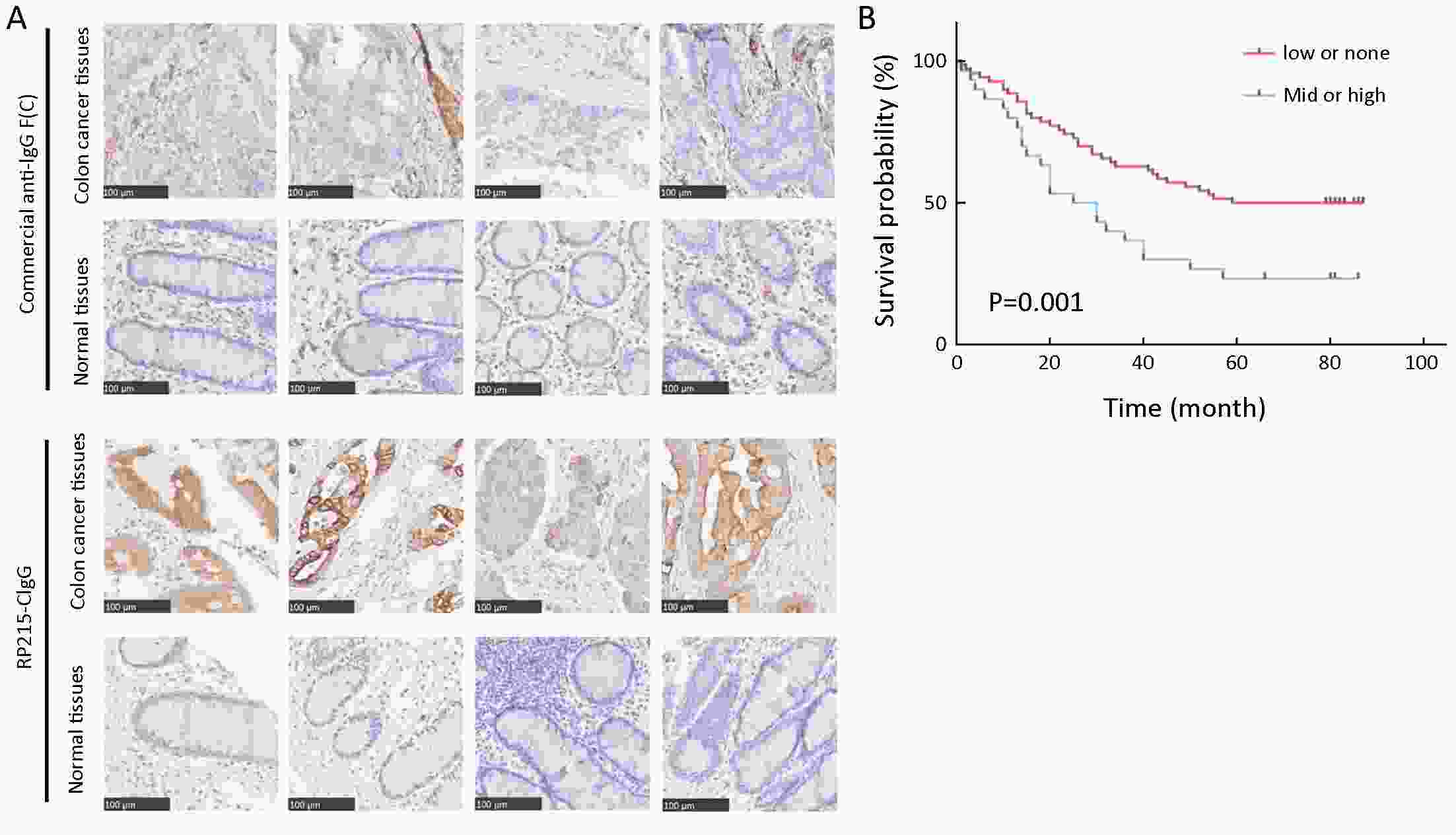
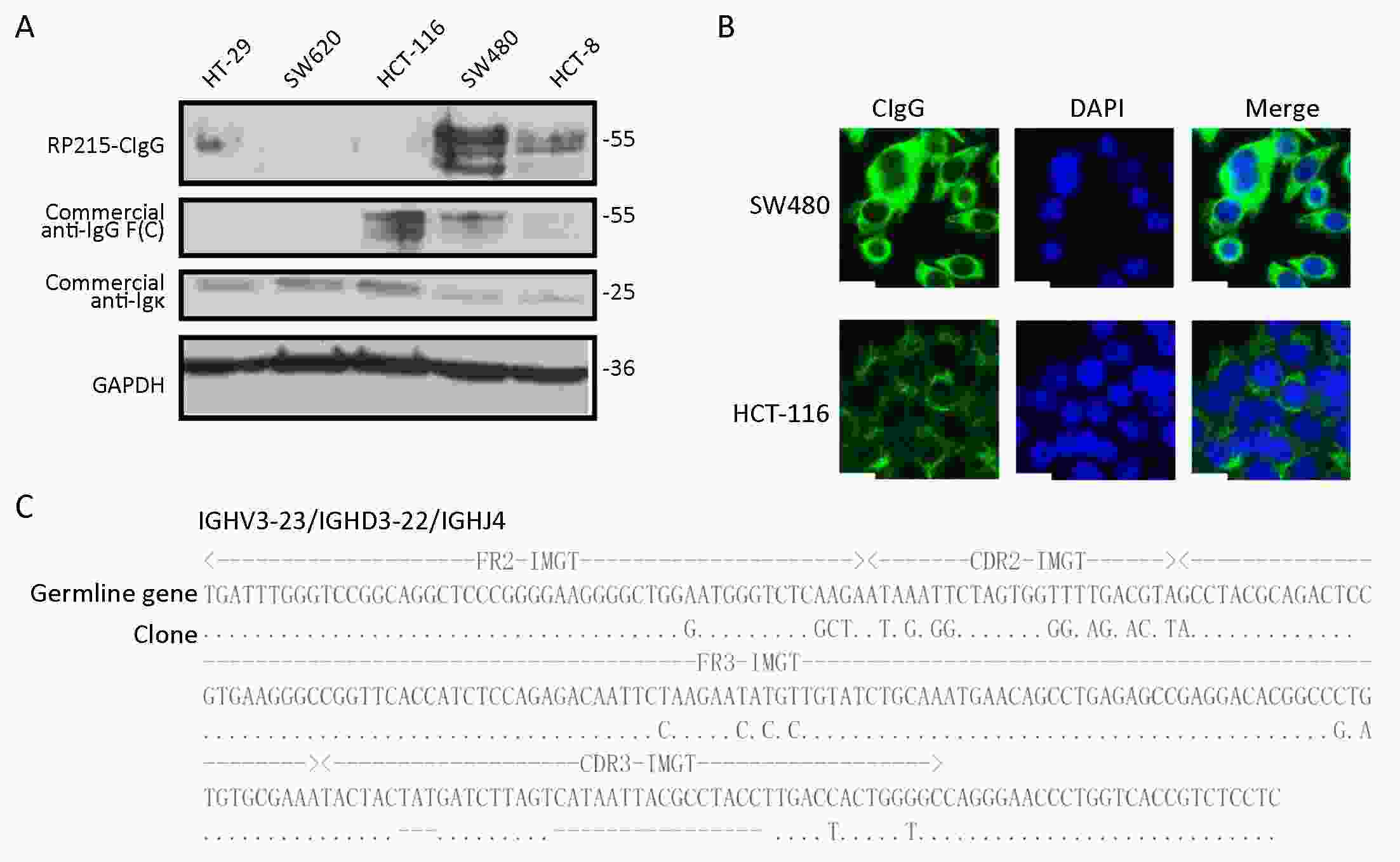
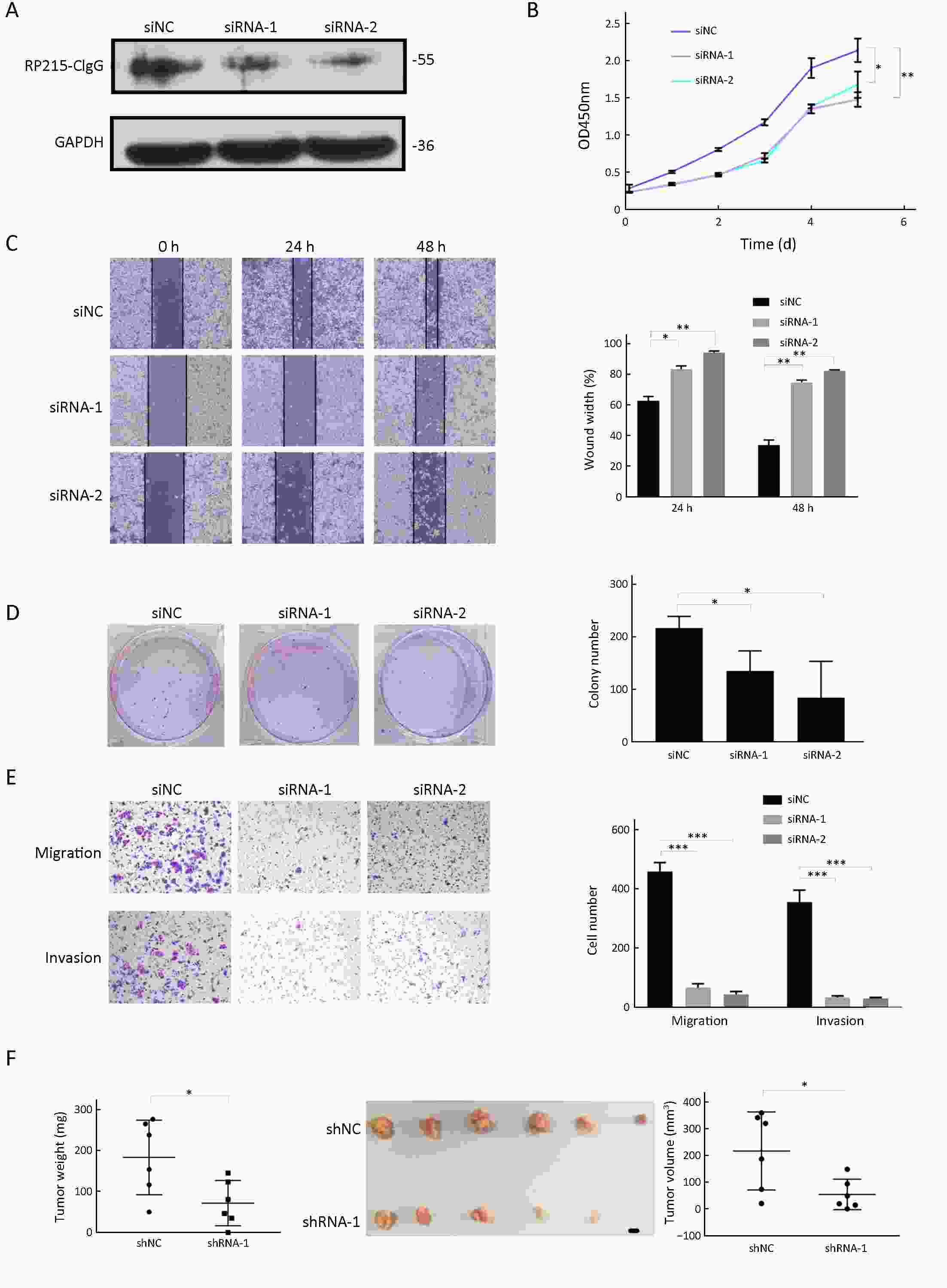
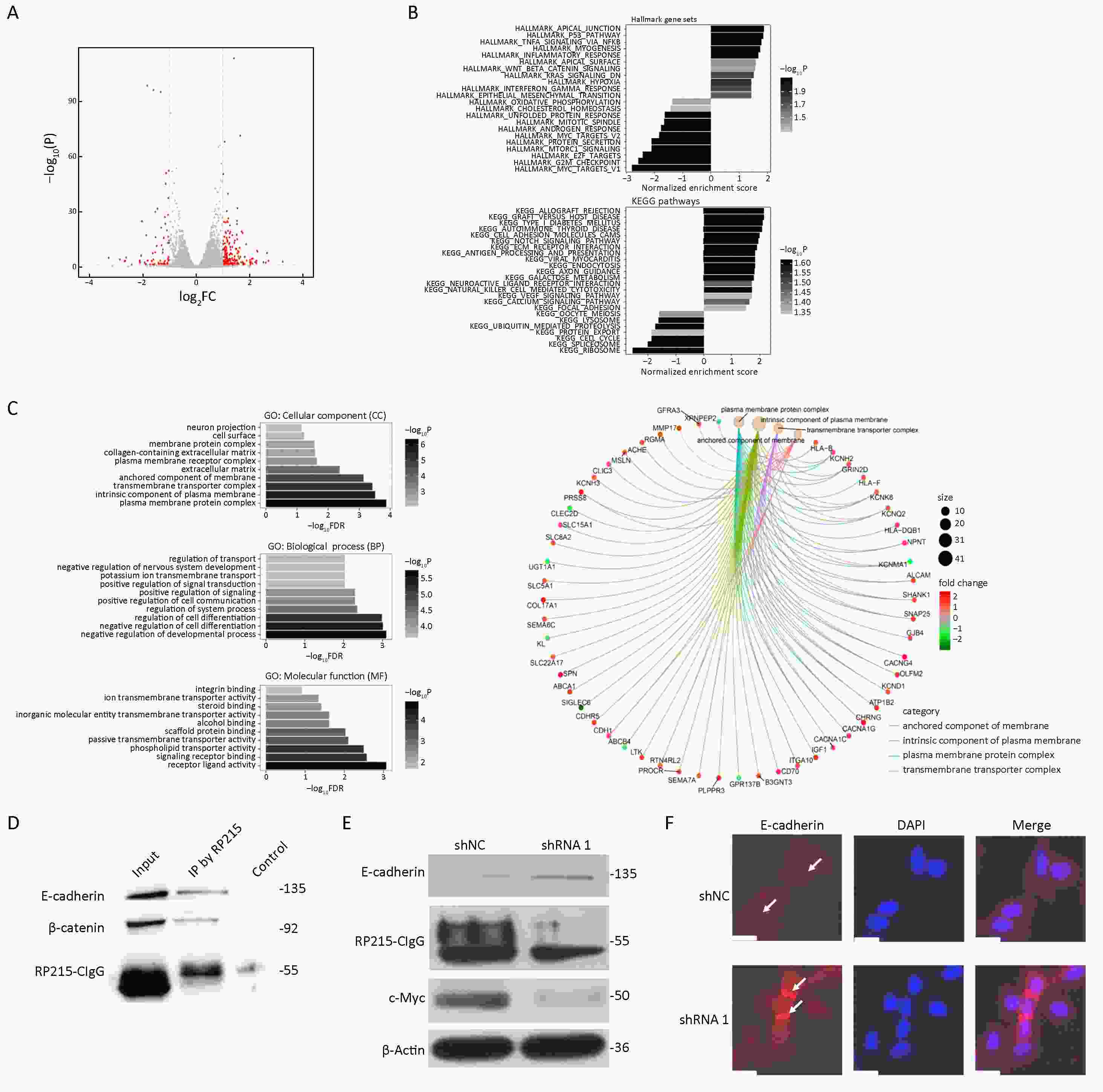
ObjectiveCurrently, no satisfactory targets for colorectal cancer or markers for immunotherapy and diagnosis and prognosis are available. Immunoglobulin G (IgG) is widely expressed in many cancers, and it promotes cancer progression. This study explored the role of cancer-derived IgG (CIgG) in colorectal cancer. MethodsFirst, using a monoclonal antibody to CIgG, we examined the expression levels of CIgG in colorectal cancer cell lines by western blot and immunofluorescence analyses and in tissue specimens by immunohistochemistry. Second, the variable region gene was amplified by nested polymerase chain reaction (PCR), and PCR products were sequenced and analyzed. Third, we investigated the effect of CIgG on colorectal cancer cells by cell proliferation, wound healing, migration and invasion assays, and colony formation assay. Fourth, we performed in vivo tumorigenicity experiments to explore the effect of CIgG on tumorigenicity. Finally, we used RNA-seq analysis and co-immunoprecipitation experiments to further clarify possible mechanisms of CIgG. ResultsWe found that CIgG is widely expressed in colorectal cancer cells, and the overexpression of CIgG indicates significantly poor colorectal cancer prognosis. Furthermore, CIgG knockdown significantly inhibits the proliferation, migration and invasion ability of cells, and tumor growth in vivo. RNA-seq analysis indicated that CIgG knockdown results primarily in changes in expression of apical junction and epithelial-mesenchymal transition-related genes. CIgG may be involved in colorectal cancer invasion and metastasis through interacting with E-cadherin. ConclusionsCIgG is a potential human oncogene in colorectal cancer and that it has potential for application as a novel target in targeted therapy and a marker for prognostic evaluation.
2019, 31(3): 511-520.
doi: 10.21147/j.issn.1000-9604.2019.03.13
Abstract:
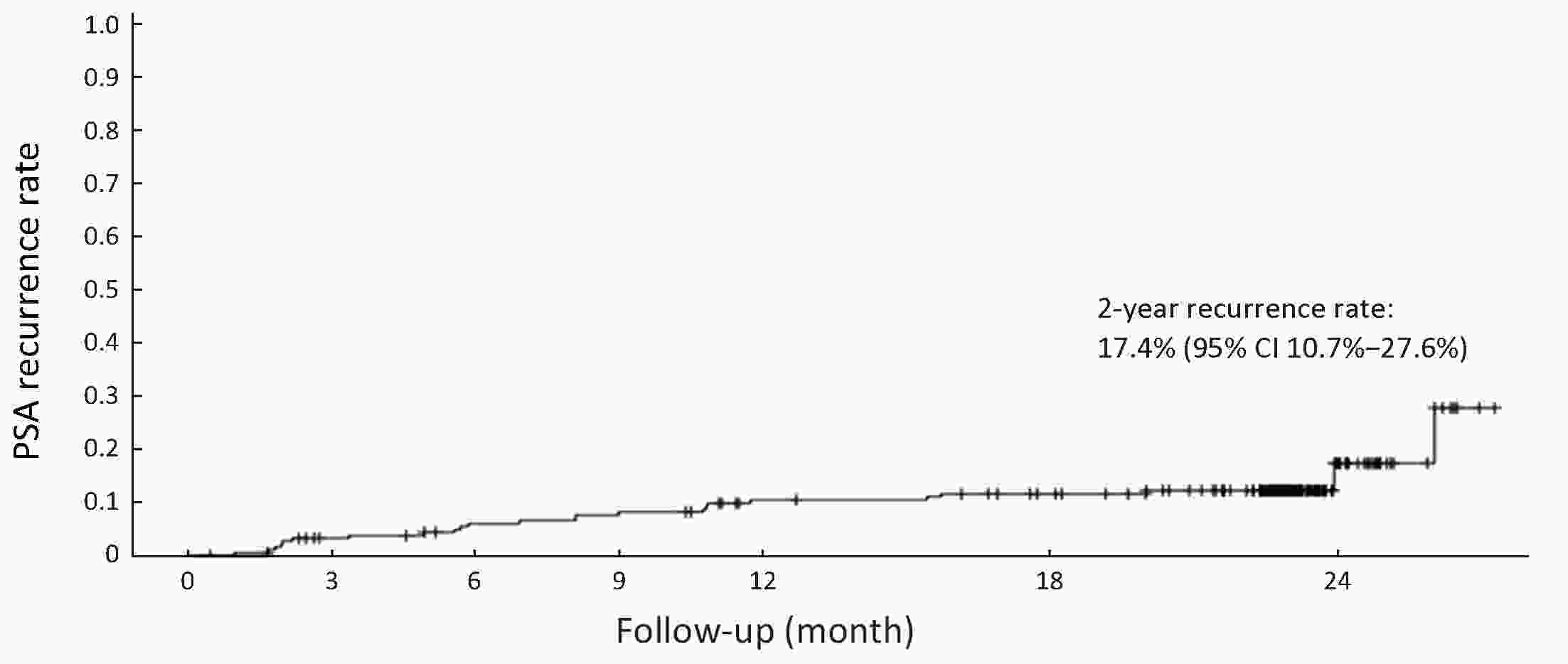
ObjectivePotential of combined androgen blockade (CAB) has not been explored extensively in Chinese males with prostate cancer (PCa). Therefore, this study evaluated the 2-year prostate-specific antigen (PSA) recurrence rate and quality of life (QoL) in patients with high-risk localized and locally advanced PCa receiving adjuvant hormone therapy (HT) after radical prostatectomy (RP). MethodsThis prospective, multicenter, observational study conducted in 18 centers across China enrolled patients with high-risk factor (preoperative PSA>20 ng/mL or Gleason score >7) or locally advanced PCa. Different adjuvant HT were administered after RP according to investigator’s decision in routine clinical practice. Relationship of baseline and postoperative characteristics was assessed with recurrence rate. PSA recurrence rate and Functional Assessment of Cancer Therapy-Prostate (FACT-P) QoL scores were recorded at 12 months and 24 months. Kaplan-Meier analysis was used to construct the PSA recurrence rate during follow-up. ResultsA total of 189 patients (mean age: 66.9±6.5 years) were recruited, among which 112 (59.3%) patients showed serum PSA>20 ng/mL preoperatively. The highest postoperative pathological advancement noticed was from clinical T2 (cT2) to pathological T3 (pT3) (43.9%) stage. The majority of the patients (66.1%) received CAB as adjuvant HT, for a median duration of 20.0 months. The least recurrence (15.2%) was noticed in patients treated with CAB, followed by those treated with luteinizing hormone-releasing hormone agonist (LHRHa) (16.1%), and antiandrogen (19.0%), with non-significant difference noted among the groups. None of the baseline or postoperative characteristics was related with PSA recurrence in our study. The 24-month FACT-P QoL score of 119 patients treated for >12 months showed significant improvement above baseline compared with those treated for ≤12 months. ConclusionsAdjuvant CAB therapy after RP showed reduction trend in 2-year PSA recurrence rate in high-risk Chinese patients with localized and locally advanced PCa, compared with adjuvant anti-androgens (AA) or LHRHa therapy. Further long-term therapy (>12 months) significantly improved QoL compared to short-term HT therapy, suggesting the beneficial effect of long-term CAB therapy in improving QoL.
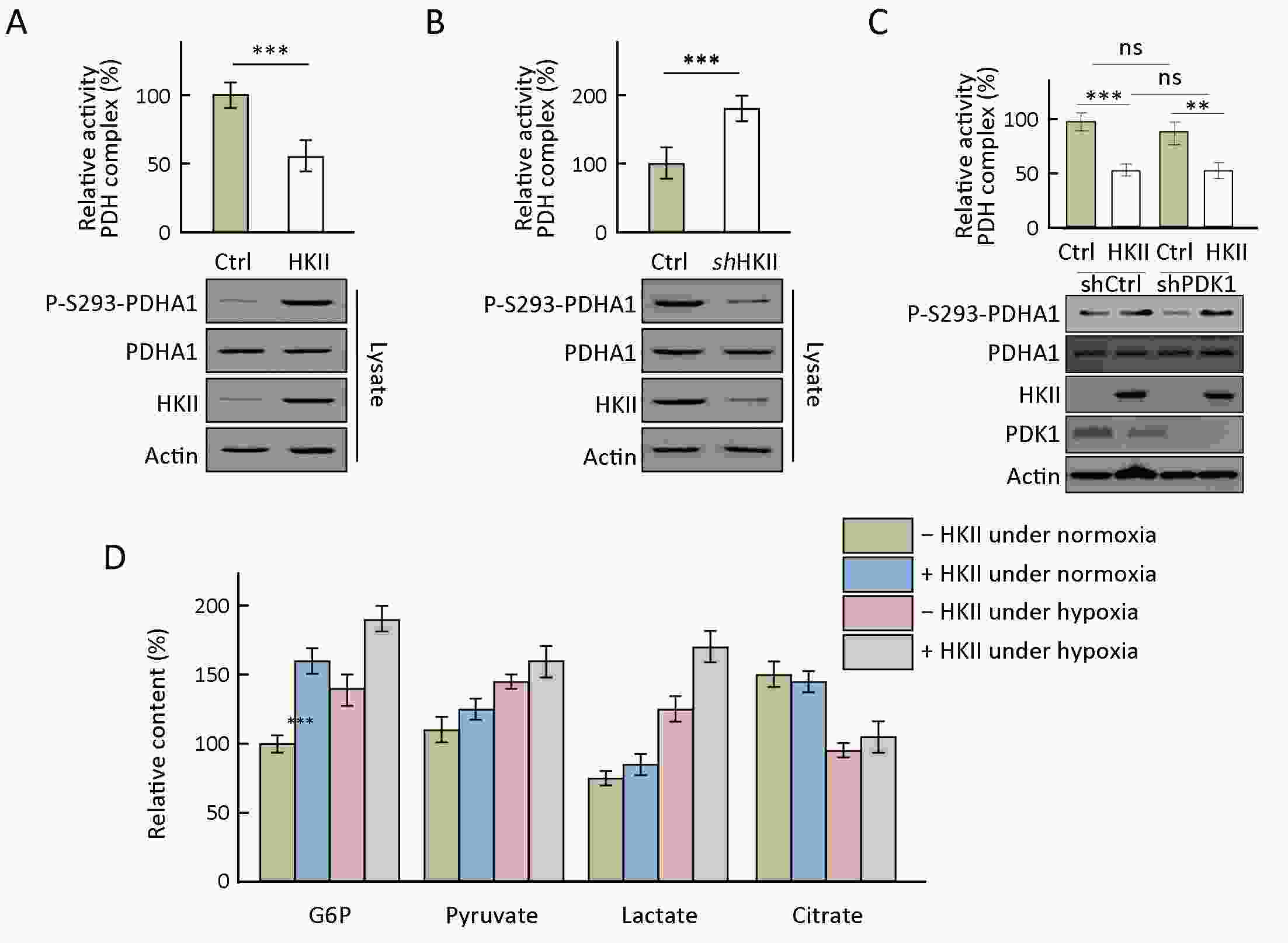
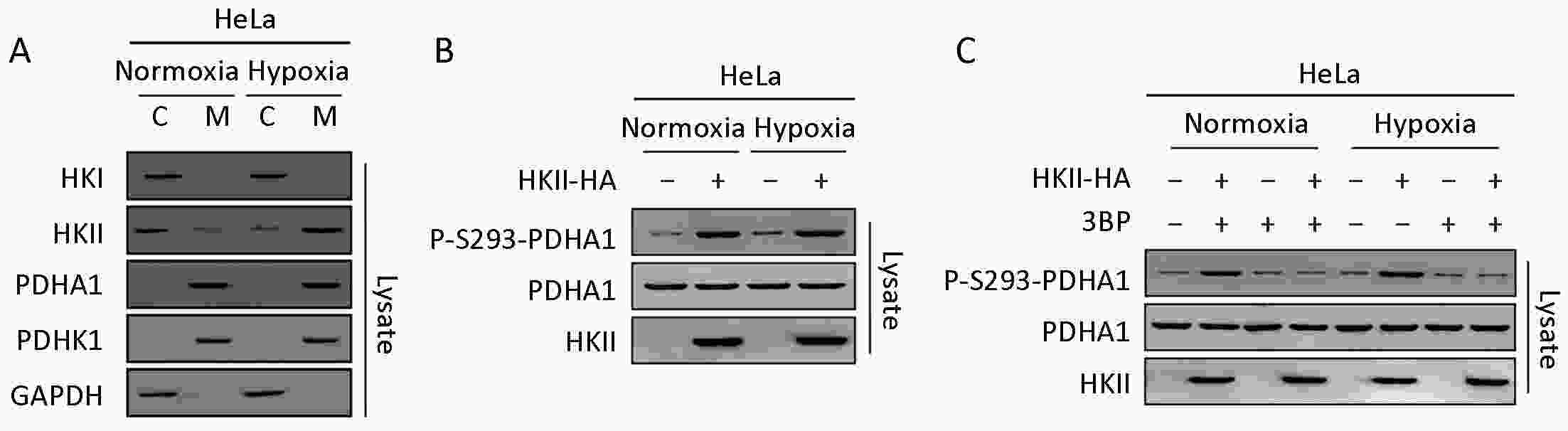
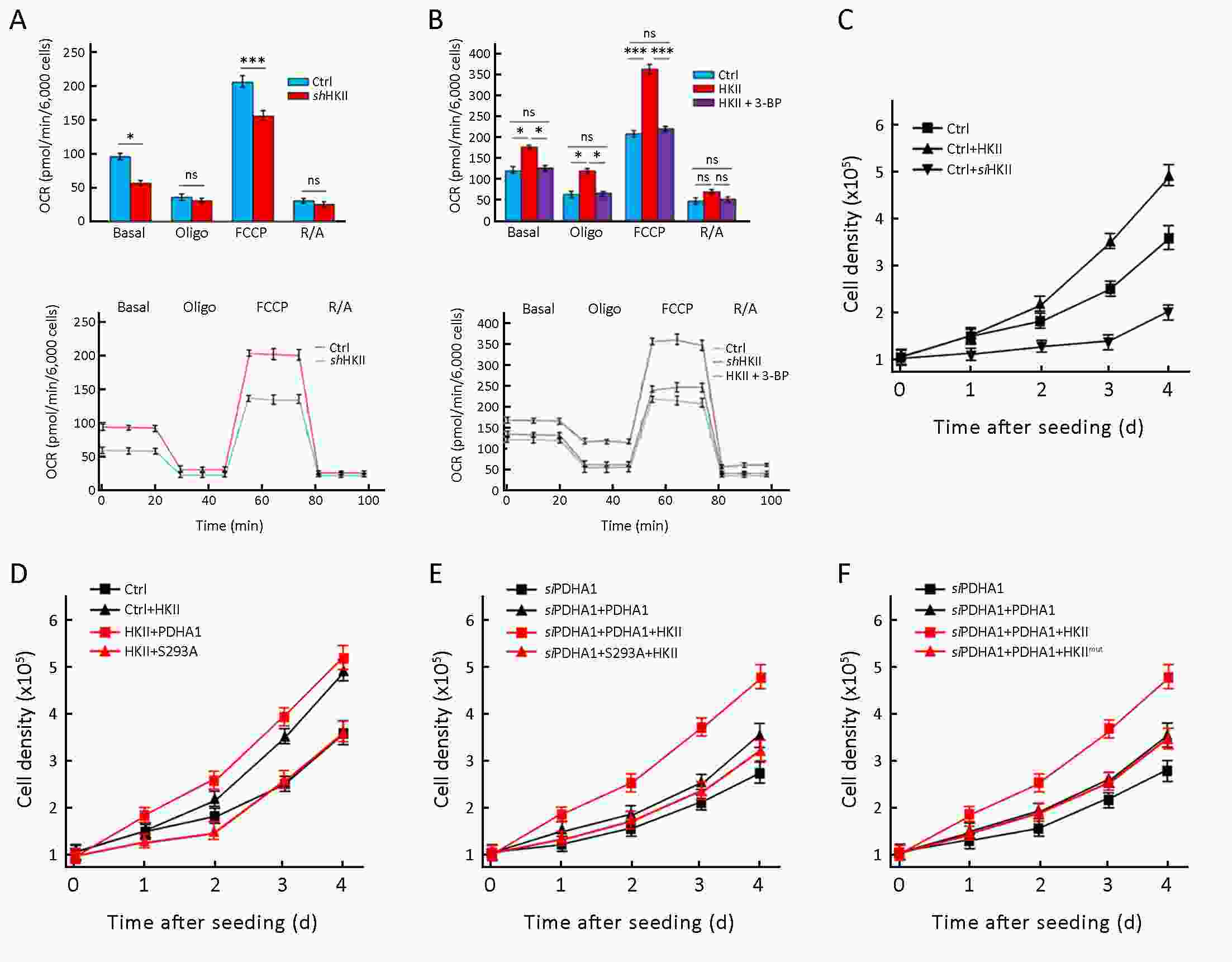
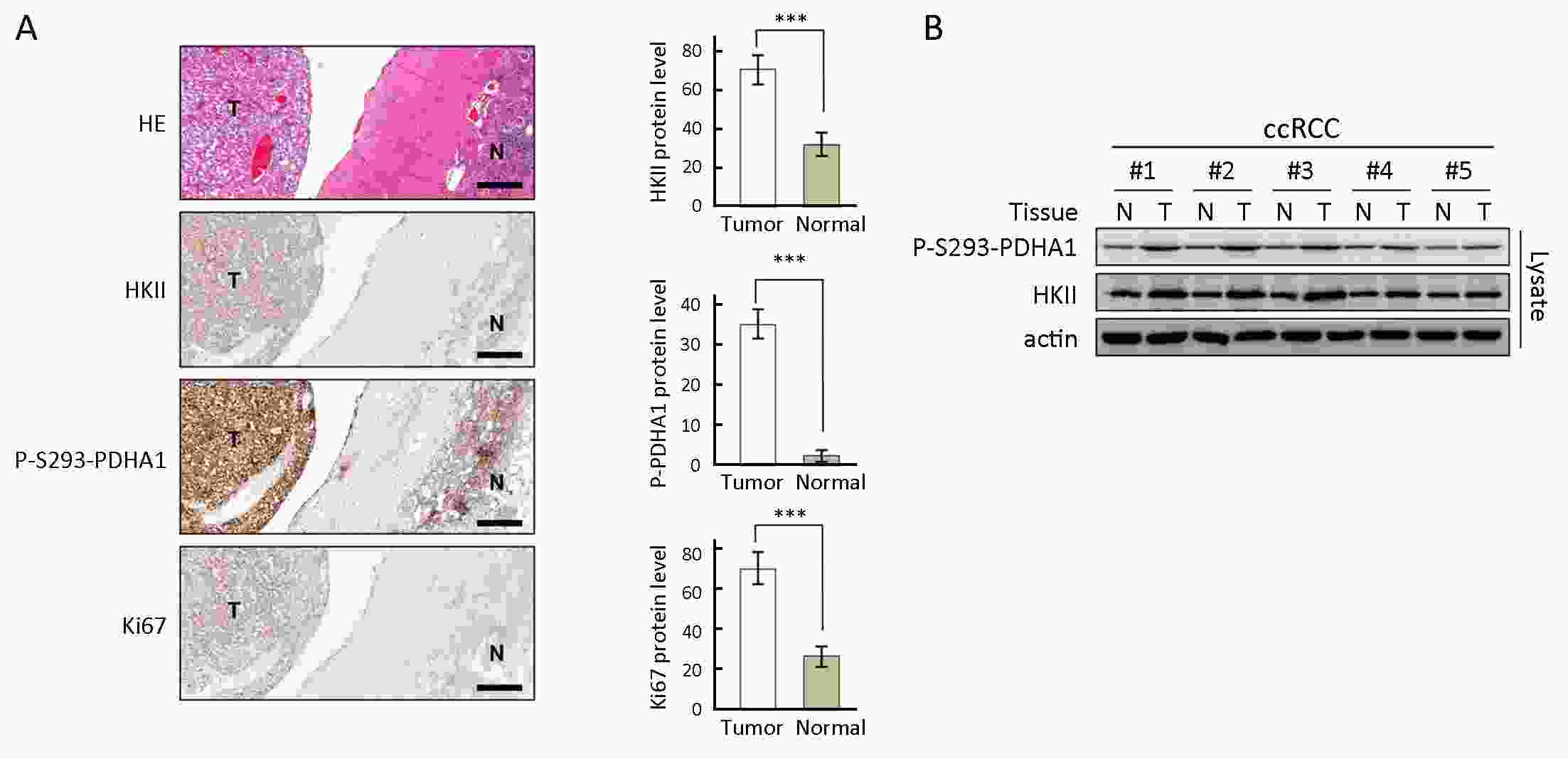
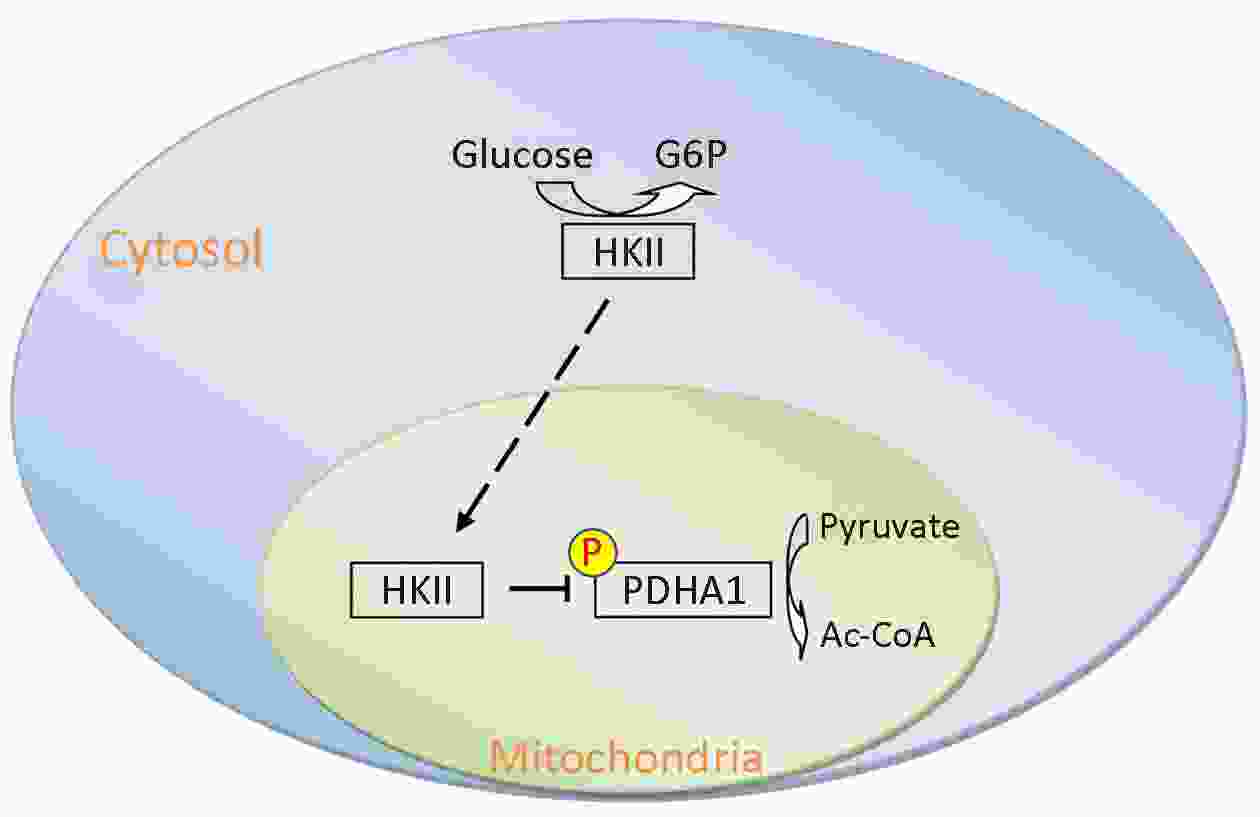
Hexokinase II promotes the Warburg effect by phosphorylating alpha subunit of pyruvate dehydrogenase
2019, 31(3): 521-532.
doi: 10.21147/j.issn.1000-9604.2019.03.14
Abstract:
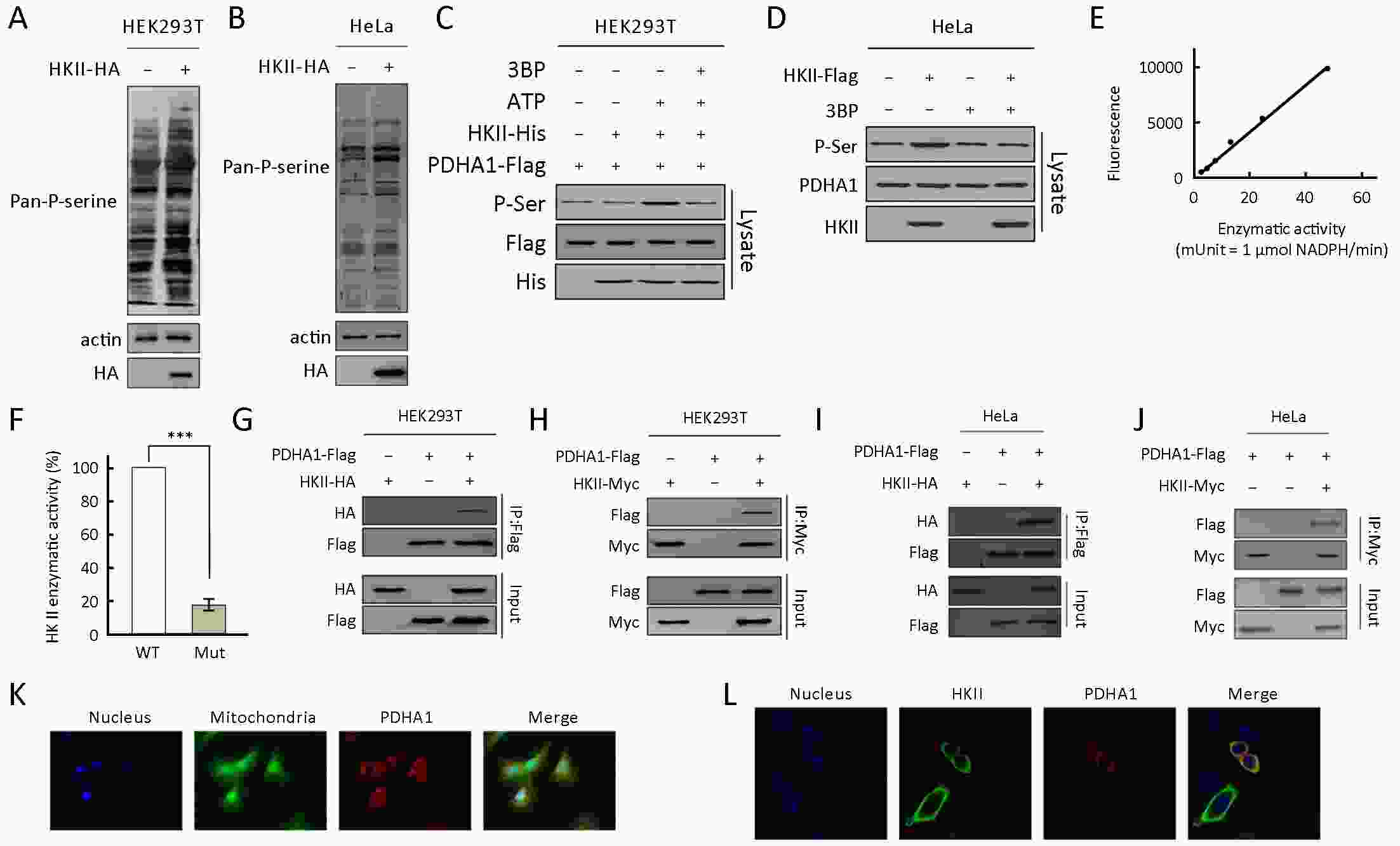
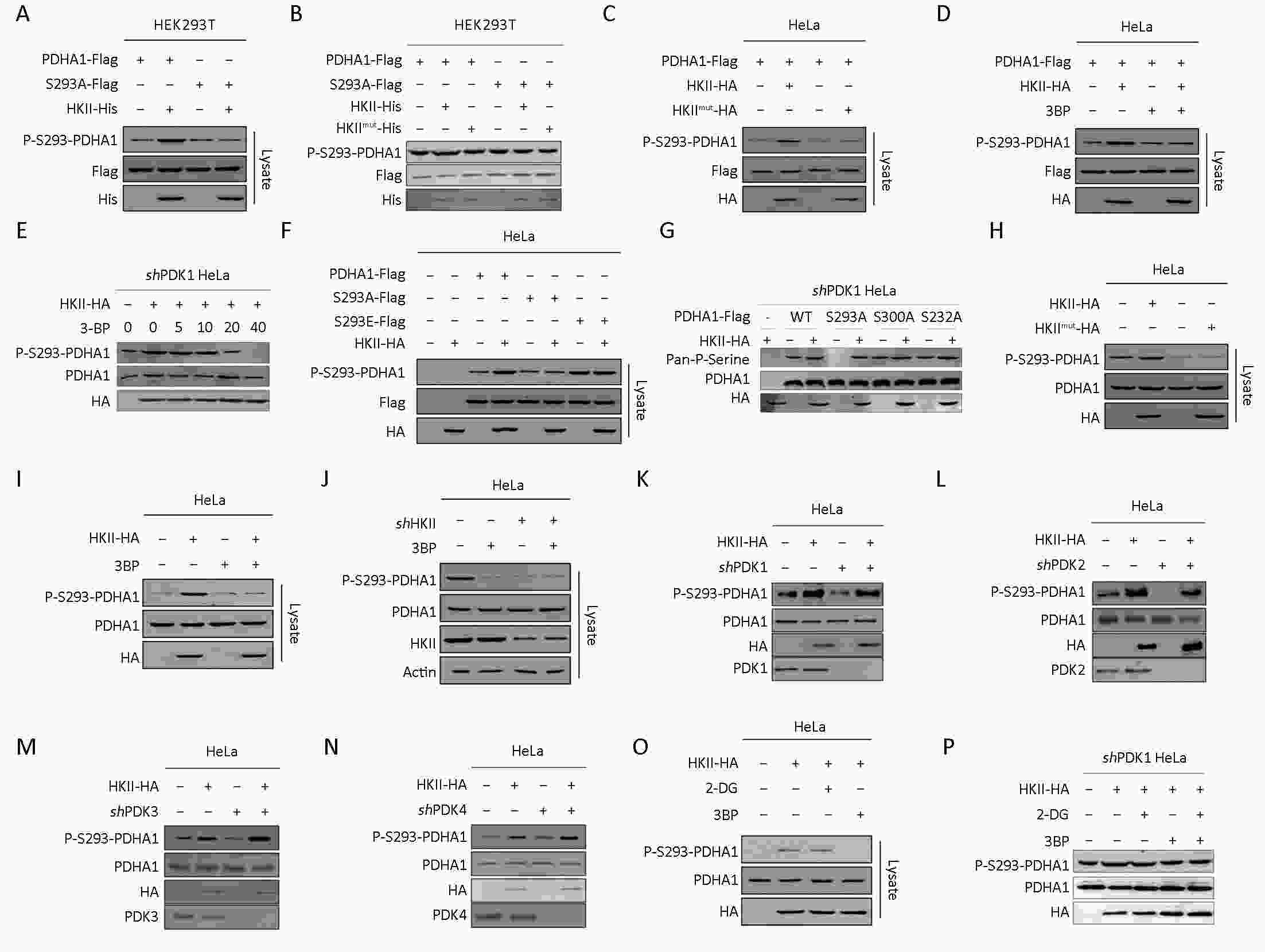
Objective Tumor cells rely heavily on glycolysis regardless of oxygen tension, a phenomenon called the Warburg effect. Hexokinase II (HKII) catalyzes the first irreversible step of glycolysis and is often overexpressed in tumor cells. Mitochondrial HKII couples glycolysis and oxidative phosphorylation while maintaining mitochondrial membrane integrity. In this study, we investigated the role of HKII in promoting the Warburg effect in cancer cells. Methods HKII-mediated phosphorylation of the alpha subunit of pyruvate dehydrogenase (PDHA1) was tested in HEK293T cells and clear cell renal cell carcinoma (ccRCC) specimens using gene knockdown, western blotting, immunohistochemistry, and immunofluorescence. Results It was determined that HKII could not only transform glucose into glucose-6-phosphate, but also transfer the phosphate group of ATP onto PDHA1. In addition, it was found that HKII increased the phosphorylation of Ser293 on PDHA1, decreasing pyruvate dehydrogenase (PDH) complex activity and thus rerouting the metabolic pathway and promoting the Warburg effect. The overexpression of HKII correlated with the phosphorylation of PDHA1 and disease progression in ccRCC. Conclusions The data presented here suggest that HKII is an important biomarker in the evaluation and treatment of cancer.
2019, 31(3): 533-546.
doi: 10.21147/j.issn.1000-9604.2019.03.15
Abstract:
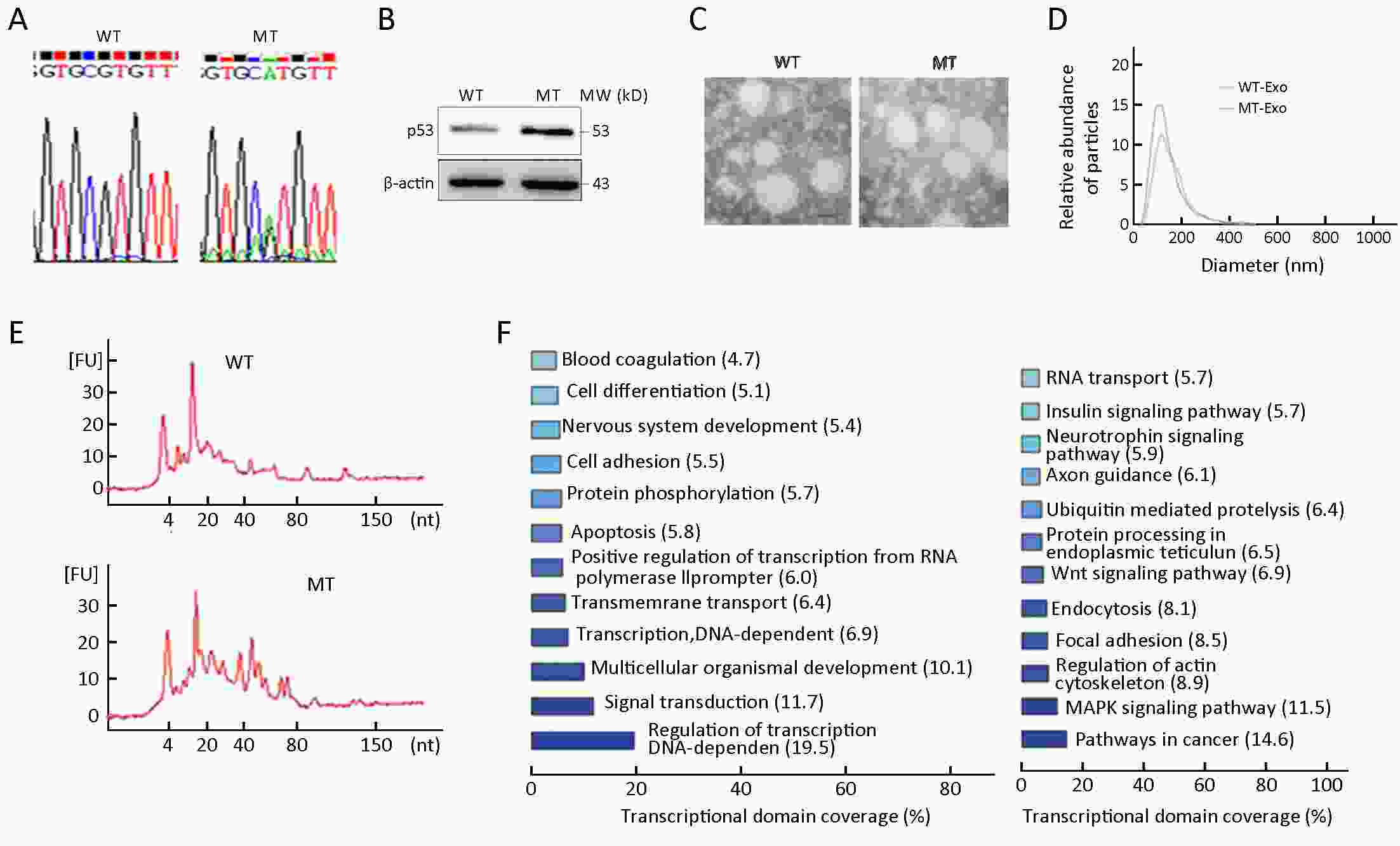
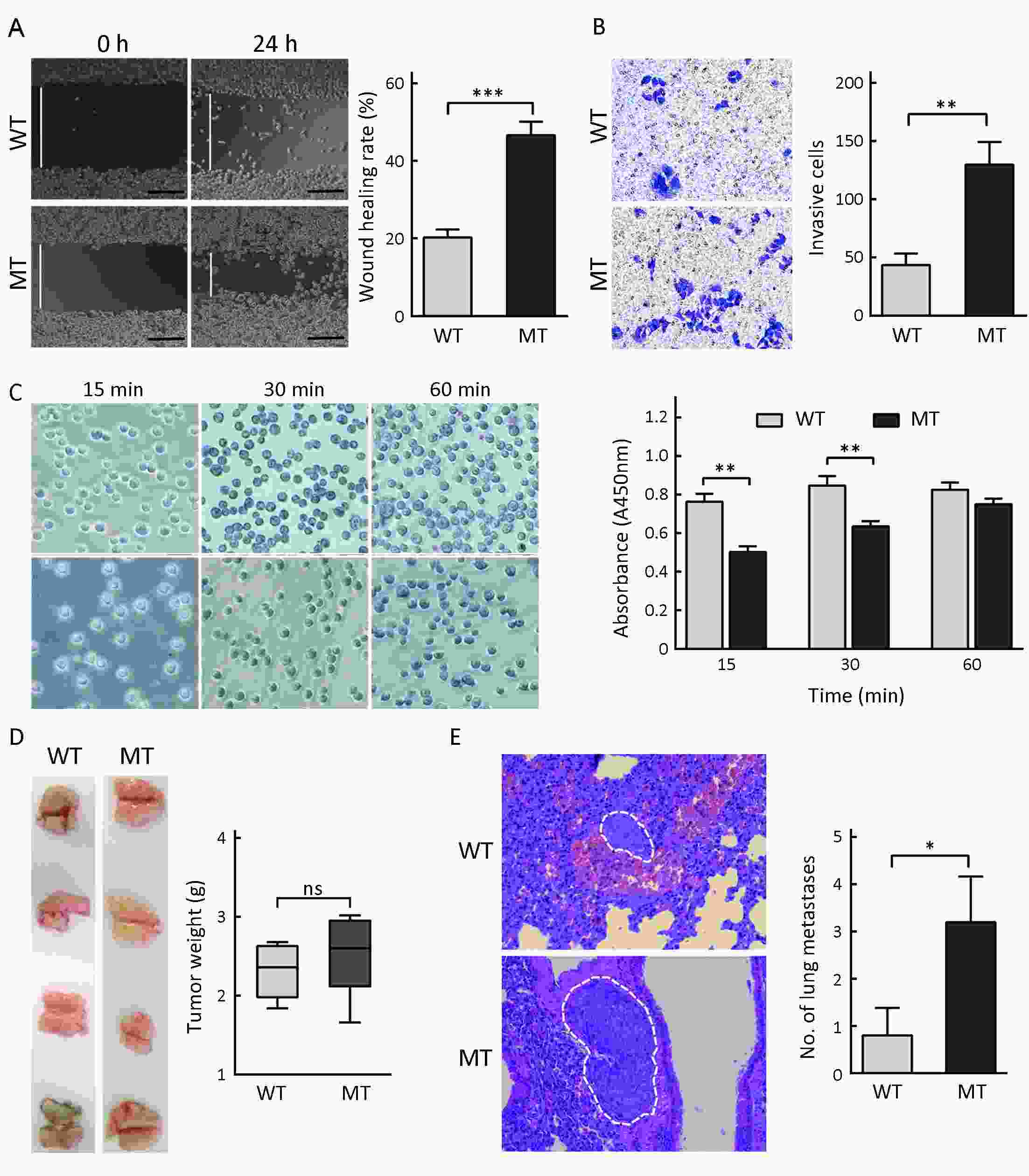
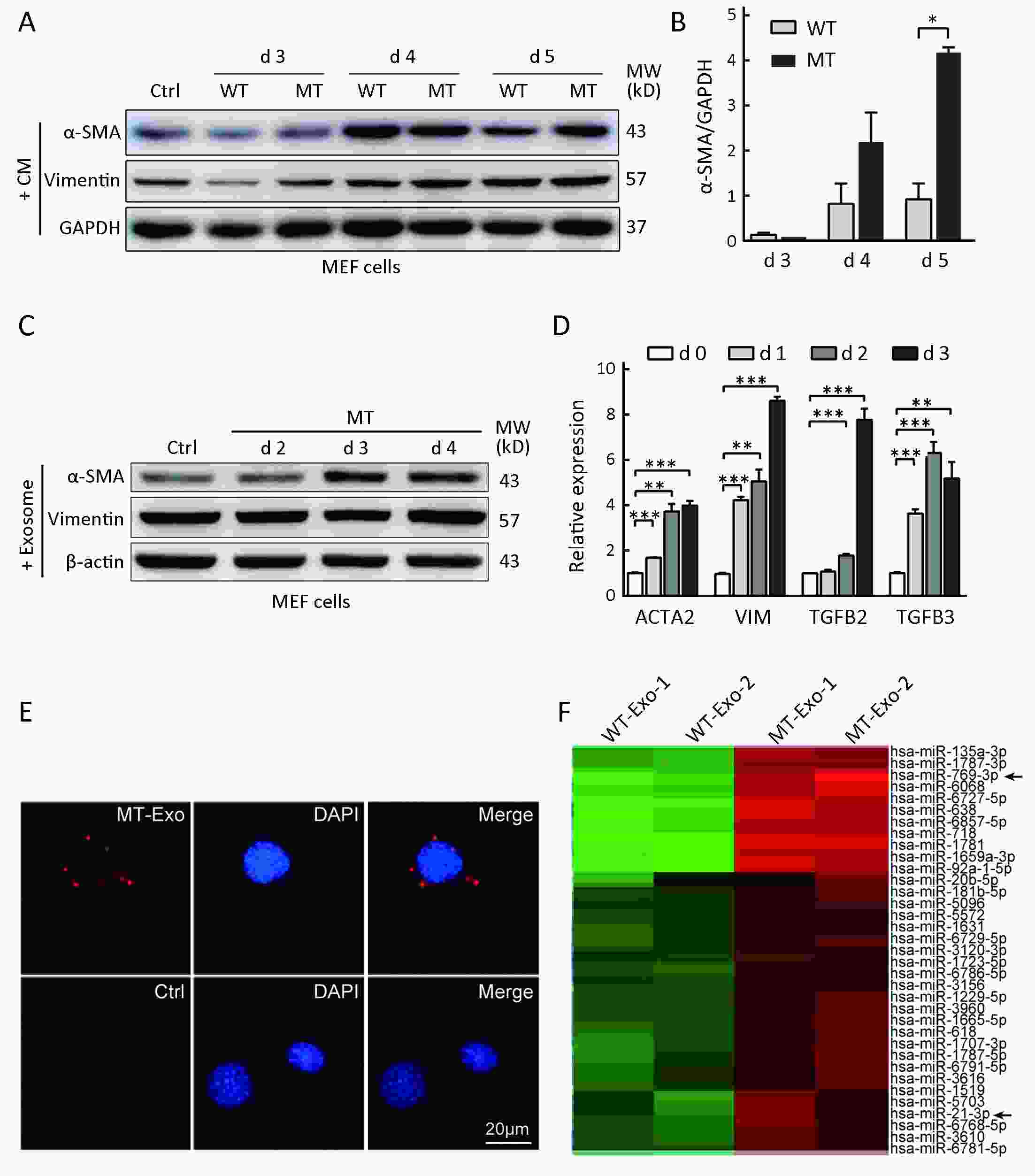
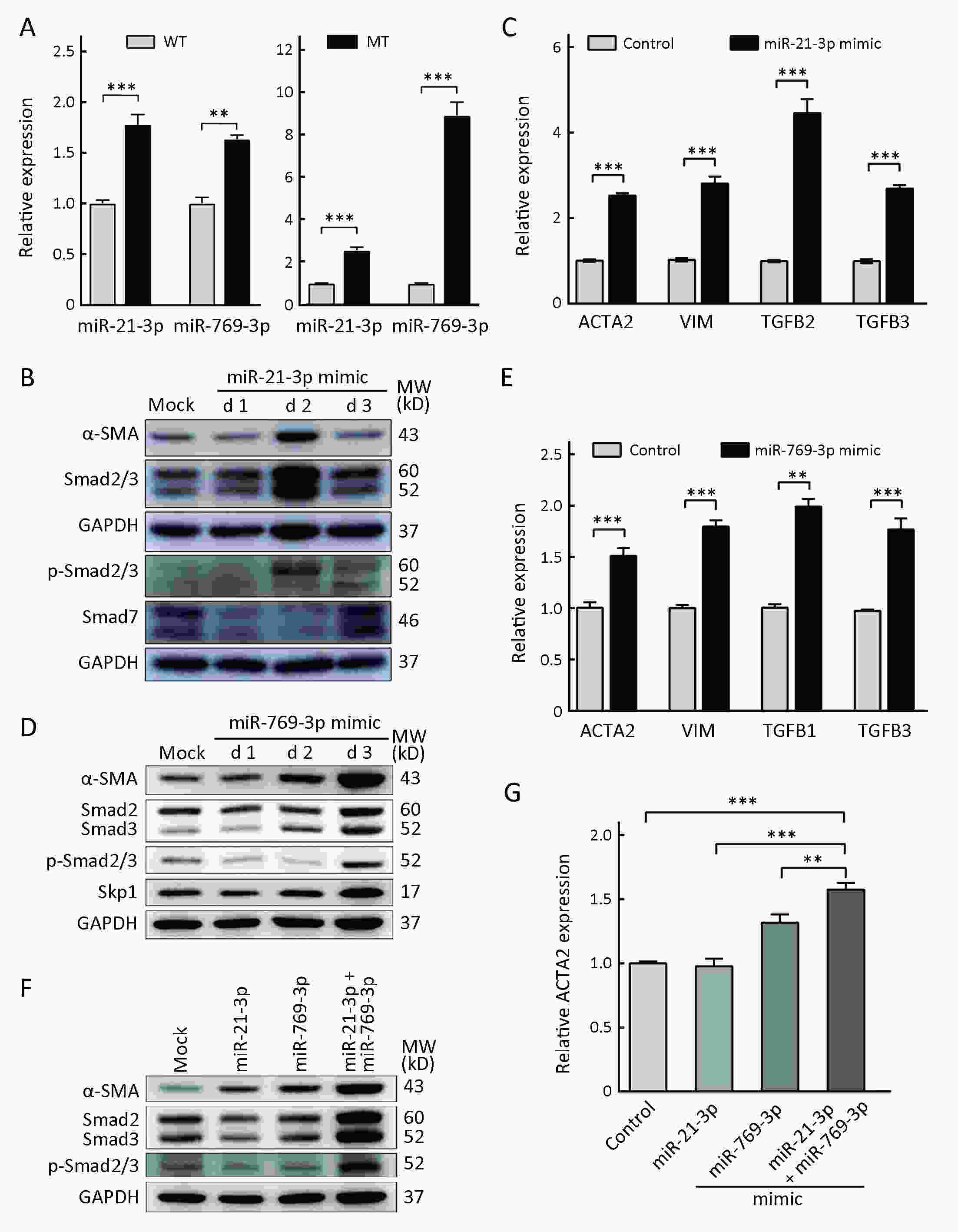
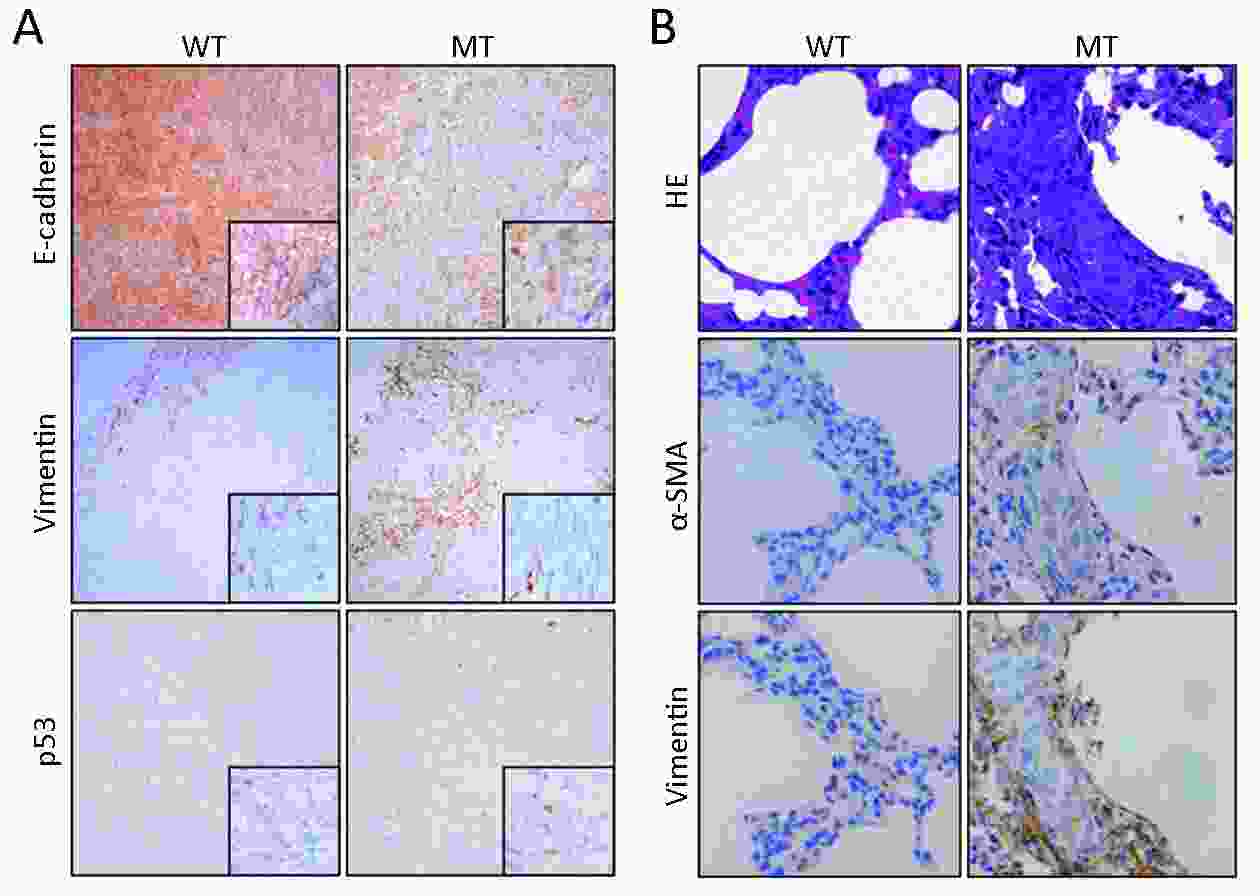
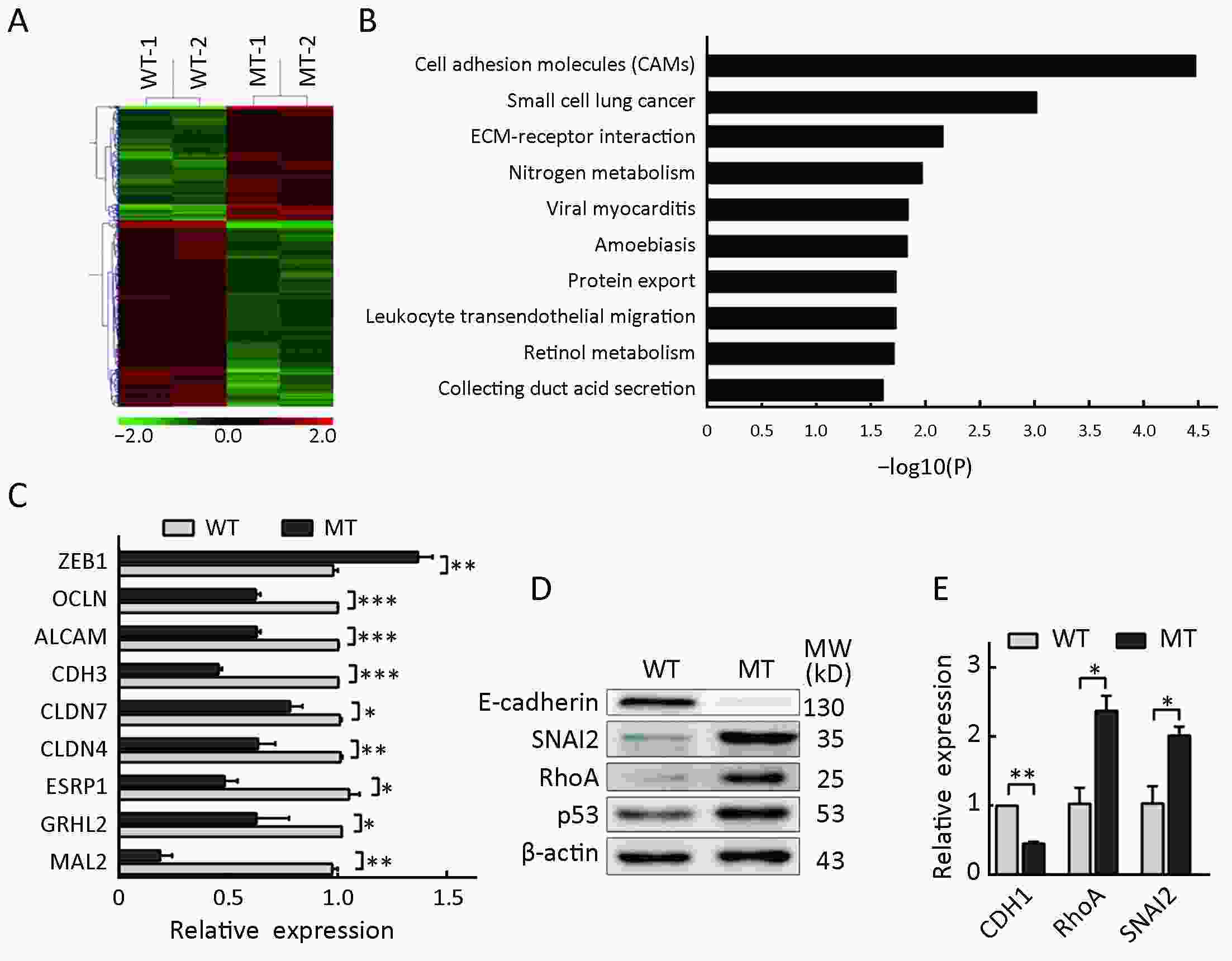
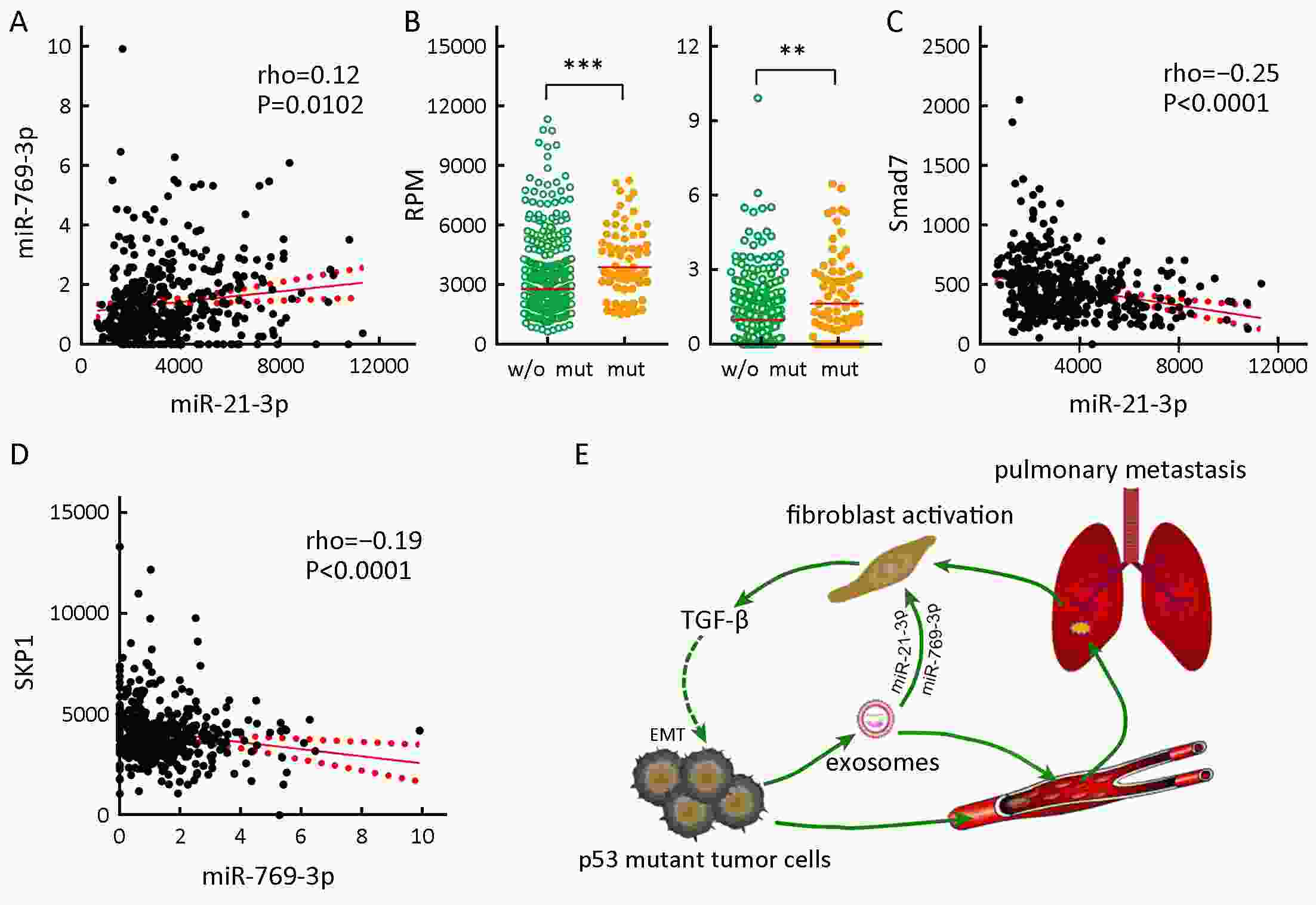
Objective Tumor metastasis is a complex, multistep process that depends on tumor cells and their communication with the tumor microenvironment. A p53 gain-of-function mutant has been shown to enhance the tumorigenesis, invasion, and metastasis abilities of tumor cells. This study aimed to investigate the roles of p53 R273H mutation in the tumor microenvironment. Methods The in vitro and in vivo effects of the p53 R273H mutant on the invasion and metastasis of HCT116 cells were investigated. Exosomes from wild-type and HCT116-TP53(R273H) cells were cocultured with mouse embryonic fibroblasts (MEFs). The roles of differentially expressed exosomal microRNAs identified by microarray analysis were investigated. The functions of the p53 R273H mutant in tumor cells were also investigated via gene expression microarray and quantitative polymerase chain reaction (qPCR) analyses. Results Introducing p53 R273H mutant into HCT116 cells significantly potentiated pulmonary metastasis in vivo. In the presence of exosomes derived from HCT116-TP53(R273H) cells, the exosomes were taken up by MEFs and became activated. Microarray analysis showed that the p53 R273H mutation increased the exosomal levels of miR-21-3p and miR-769-3p. Intriguingly, in clinical samples, miR-21-3p and miR-769-3p levels were significantly higher in patients with a p53 mutation than in those without this mutation. Furthermore, both miR-21-3p and miR-769-3p activated fibroblasts and exerted a synergistic effect via their target genes on the transforming growth factor-β (TGF-β)/Smad signaling pathway. The activated fibroblasts excreted cytokine TGF-β and may have reciprocally induced cancer cells to undergo epithelial-mesenchymal transition (EMT). Indeed, HCT116-TP53(R273H) cells showed increased expression of ZEB1 and SNAI2 and decreased transcription of several cell adhesion molecules. Conclusions The mutant p53-exosomal miR-21-3p/miR-769-3p-fibroblast-cytokine circuit appears to be responsible for communication between tumor and stromal cells, with exosomal miRNAs acting as a bridge. miR-21-3p and miR-769-3p are potential predictive markers of pulmonary metastasis and candidate targets for therapeutic interventions.
2019, 31(3): 547-556.
doi: 10.21147/j.issn.1000-9604.2019.03.16
Abstract:
Accumulating evidence suggests that periostin is frequently upregulated in tissue injury, inflammation, fibrosis and tumor progression. Periostin expression in cancer cells can promote metastatic potential of colorectal cancer (CRC) via activating PI3K/Akt signaling pathway. Moreover, periostin is observed mainly in tumor stroma and cytoplasm of cancer cells, which may facilitate aggressiveness of CRC. In this review, we summarize information regarding periostin to emphasize its role as a prognostic marker of CRC.
Accumulating evidence suggests that periostin is frequently upregulated in tissue injury, inflammation, fibrosis and tumor progression. Periostin expression in cancer cells can promote metastatic potential of colorectal cancer (CRC) via activating PI3K/Akt signaling pathway. Moreover, periostin is observed mainly in tumor stroma and cytoplasm of cancer cells, which may facilitate aggressiveness of CRC. In this review, we summarize information regarding periostin to emphasize its role as a prognostic marker of CRC.

 Abstract
Abstract FullText HTML
FullText HTML PDF 94KB
PDF 94KB