2019 Vol.31(4)
Display Mode: |
2019, 31(4): 557-577.
doi: 10.21147/j.issn.1000-9604.2019.04.01
Abstract:
2019, 31(4): 578-585.
doi: 10.21147/j.issn.1000-9604.2019.04.02
Abstract:
2019, 31(4): 586-600.
doi: 10.21147/j.issn.1000-9604.2019.04.03
Abstract:
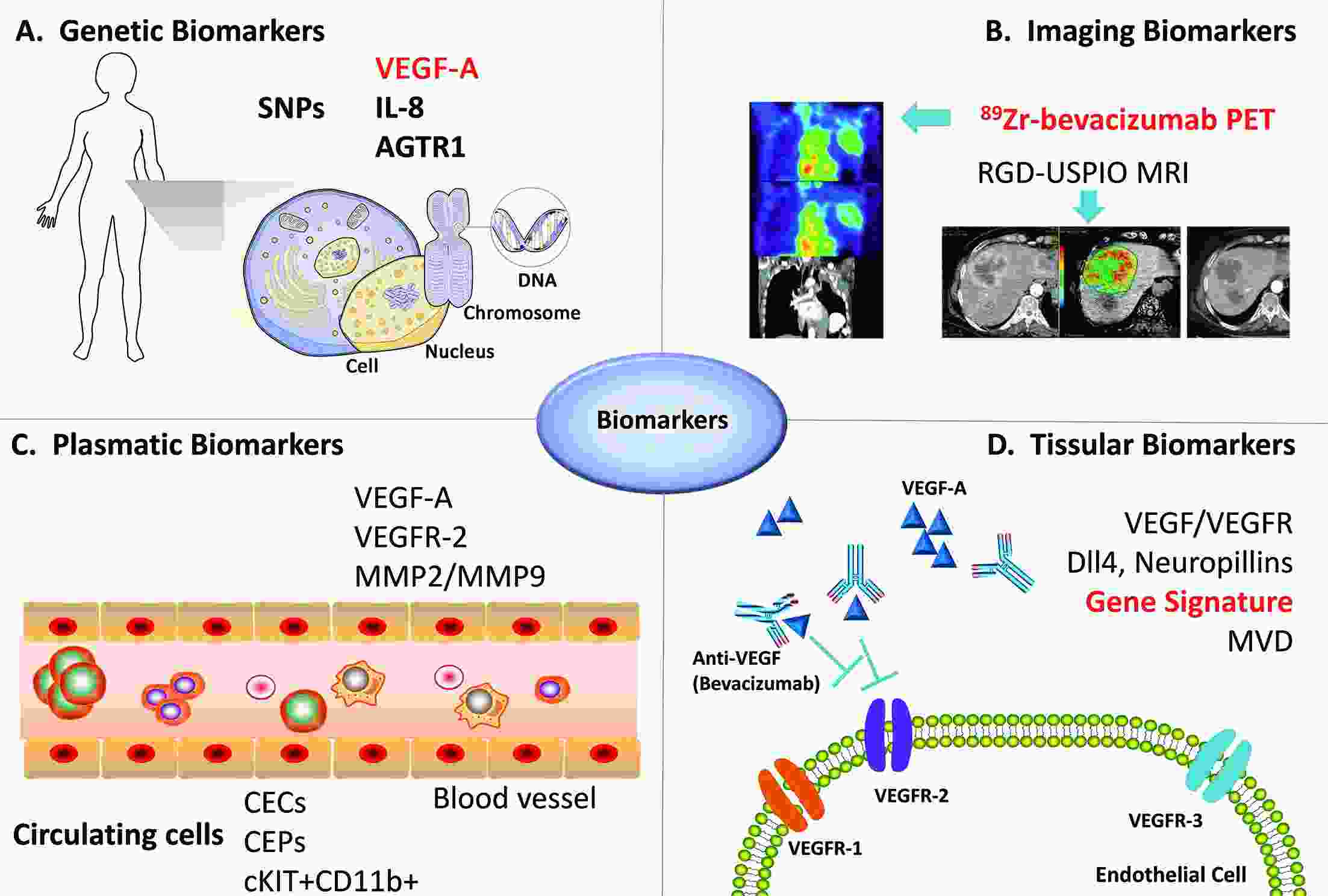
As the first monoclonal antibody against vascular endothelial growth factor (VEGF), bevacizumab (BEV) is a definitely controversial antiangiogenic therapy in breast cancer. The initial excitement over improvements in progression-free survival (PFS) with BEV was tempered by an absence of overall survival (OS) benefit and serious adverse effects. Missing targeted population urged us to identify the predictive biomarkers for BEV efficacy. In this review we focus on the research in breast cancer and provide recent investigations on clinical, radiological, molecular and gene profiling markers of BEV efficacy, including the new results from randomized phase III clinical trials evaluating the efficacy of BEV in combination with comprehensive biomarker analyses. Current evidences indicate some predictive values for genetic variants, molecular imaging, VEGF pathway factors or associated factors in peripheral blood and gene profiling. The current challenge is to validate those potential biomarkers and implement them into clinical practice.
As the first monoclonal antibody against vascular endothelial growth factor (VEGF), bevacizumab (BEV) is a definitely controversial antiangiogenic therapy in breast cancer. The initial excitement over improvements in progression-free survival (PFS) with BEV was tempered by an absence of overall survival (OS) benefit and serious adverse effects. Missing targeted population urged us to identify the predictive biomarkers for BEV efficacy. In this review we focus on the research in breast cancer and provide recent investigations on clinical, radiological, molecular and gene profiling markers of BEV efficacy, including the new results from randomized phase III clinical trials evaluating the efficacy of BEV in combination with comprehensive biomarker analyses. Current evidences indicate some predictive values for genetic variants, molecular imaging, VEGF pathway factors or associated factors in peripheral blood and gene profiling. The current challenge is to validate those potential biomarkers and implement them into clinical practice.
2019, 31(4): 601-608.
doi: 10.21147/j.issn.1000-9604.2019.04.04
Abstract:
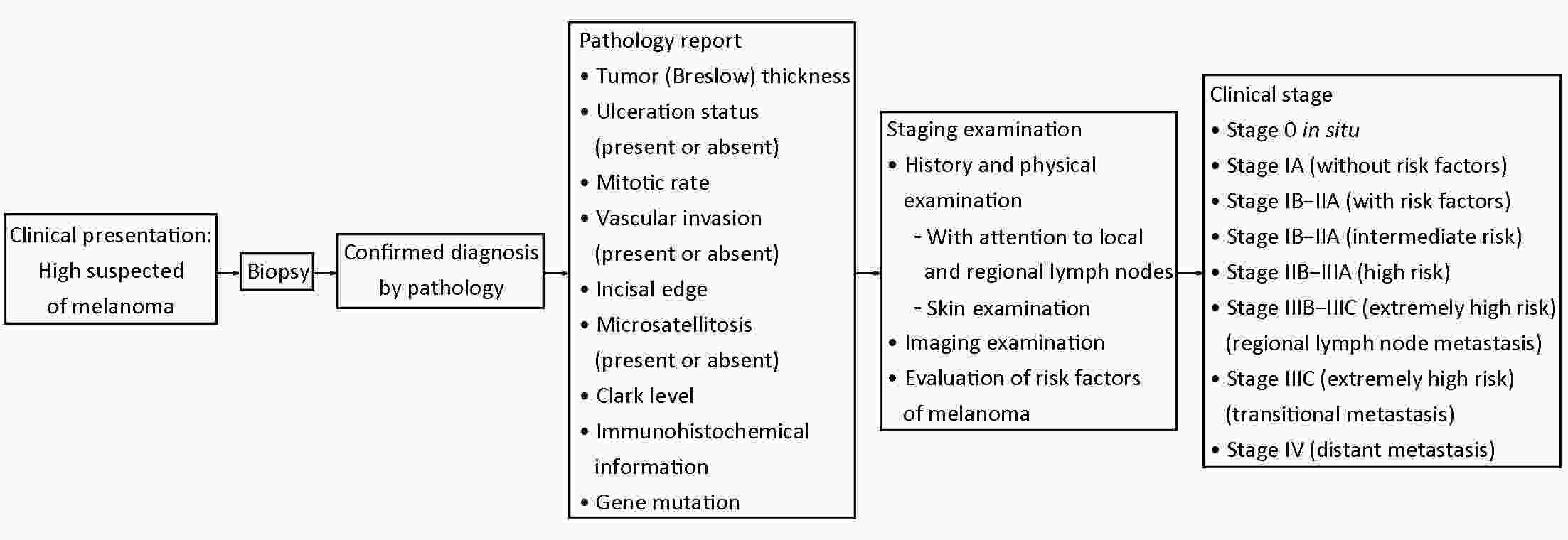
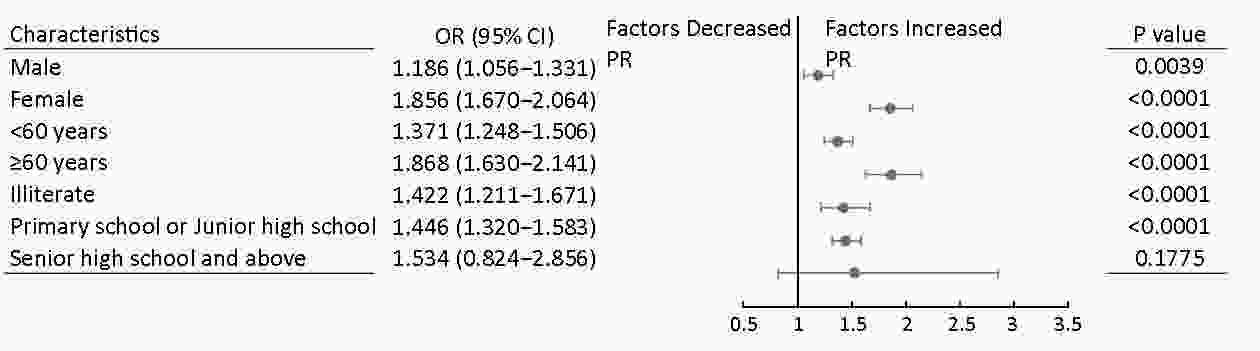
Objective China have implemented population-based esophageal cancer (EC) screening programs, however, the participant rates were relatively low. This study was conducted to examine the association between cancer prevention knowledge and EC screening participation rates (PRs). Methods Data in the analyses were obtained from a population-based cancer screening program in four provinces in China since 2007. In the course of 2007−2016, participants who were evaluated as high risk for EC and subsequently recommended for endoscopy examination were included in the final analysis. One-way analysis of variance test, Chi-square test and logistic regression analysis were applied. Results A total of 28,543 individuals assessed as high-risk population for EC were included in this study, with 13,036 males (45.67%) and 15,507 females (54.33%). The prevalence rates of current smoking and alcohol drinking were higher in males (58.25% and 44.22%, respectively) than in females (5.35% and 4.05%, respectively). Participants of females, and those who had older age, lower income, as well as higher education level and cancer prevention knowledge level were more likely to undergo endoscopy. Multivariable analysis showed that higher cancer prevention knowledge was associated with higher PR for endoscopic screening [adjusted odd ratio (aORQ4/Q1) =1.511, 95% confidence interval (95% CI): 1.398−1.632] among our study subjects. This association between cancer prevention knowledge and compliance with endoscopic screening also tends to be strong within subgroups of males, females, aged below 60 years, aged 60 years and above, and lower level of education (illiterate individuals and those with junior high education or less). Conclusions Our results displayed a positive relationship between cancer prevention knowledge and PRs for endoscopic screening, implying cancer prevention awareness being an independent influence factor for compliance with EC screening. Promoting public campaigns about comprehensive knowledge of cancer prevention seemed to be a reasonable and effective strategy to improve population PRs for EC screening.
2019, 31(4): 609-619.
doi: 10.21147/j.issn.1000-9604.2019.04.05
Abstract:
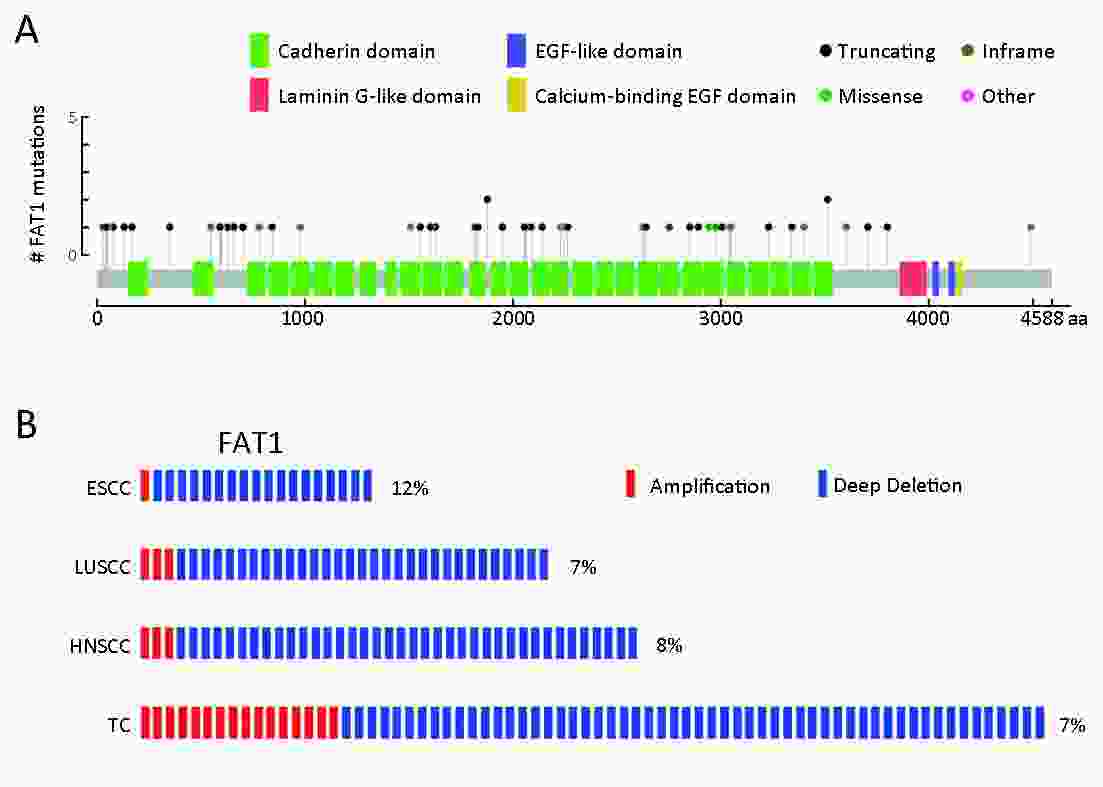
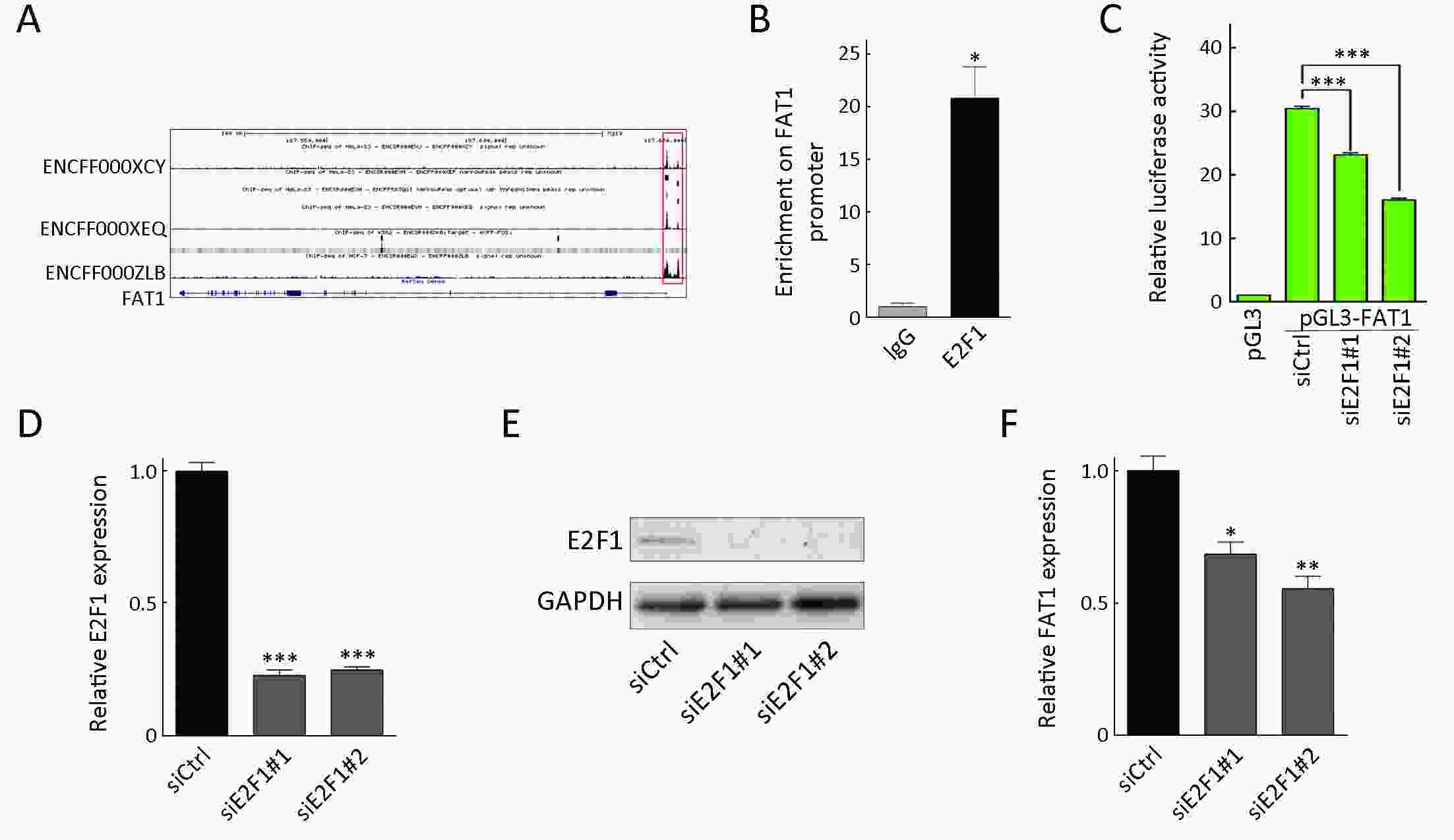
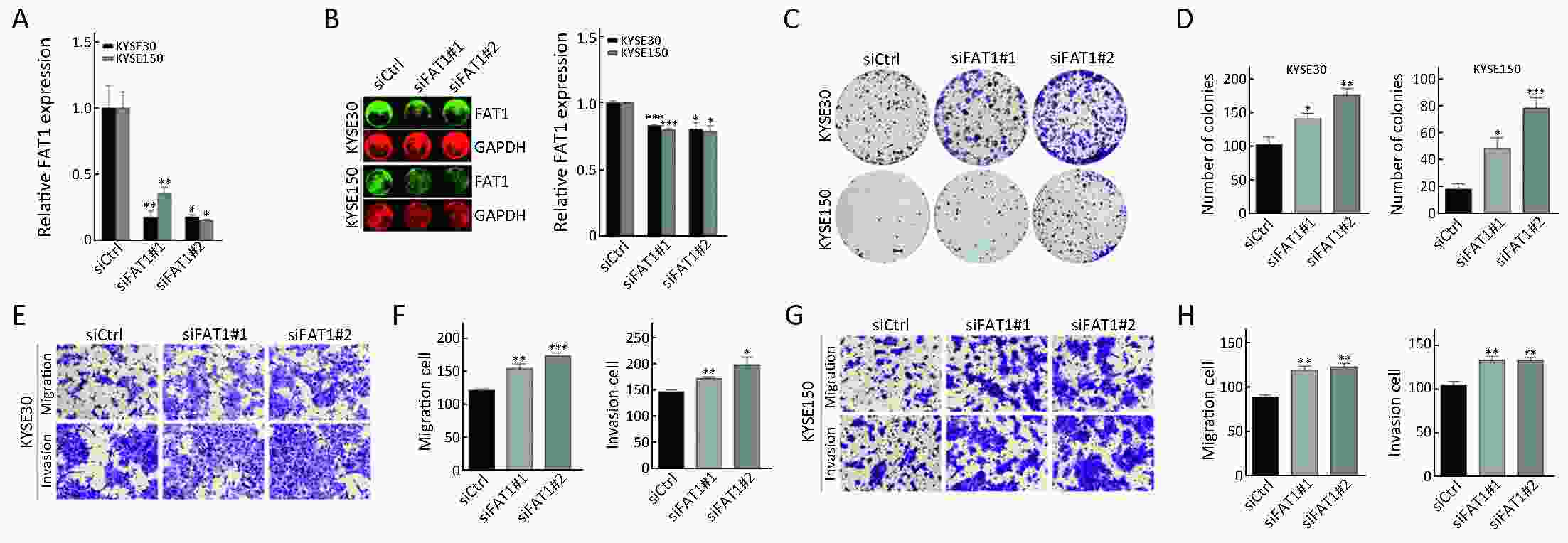
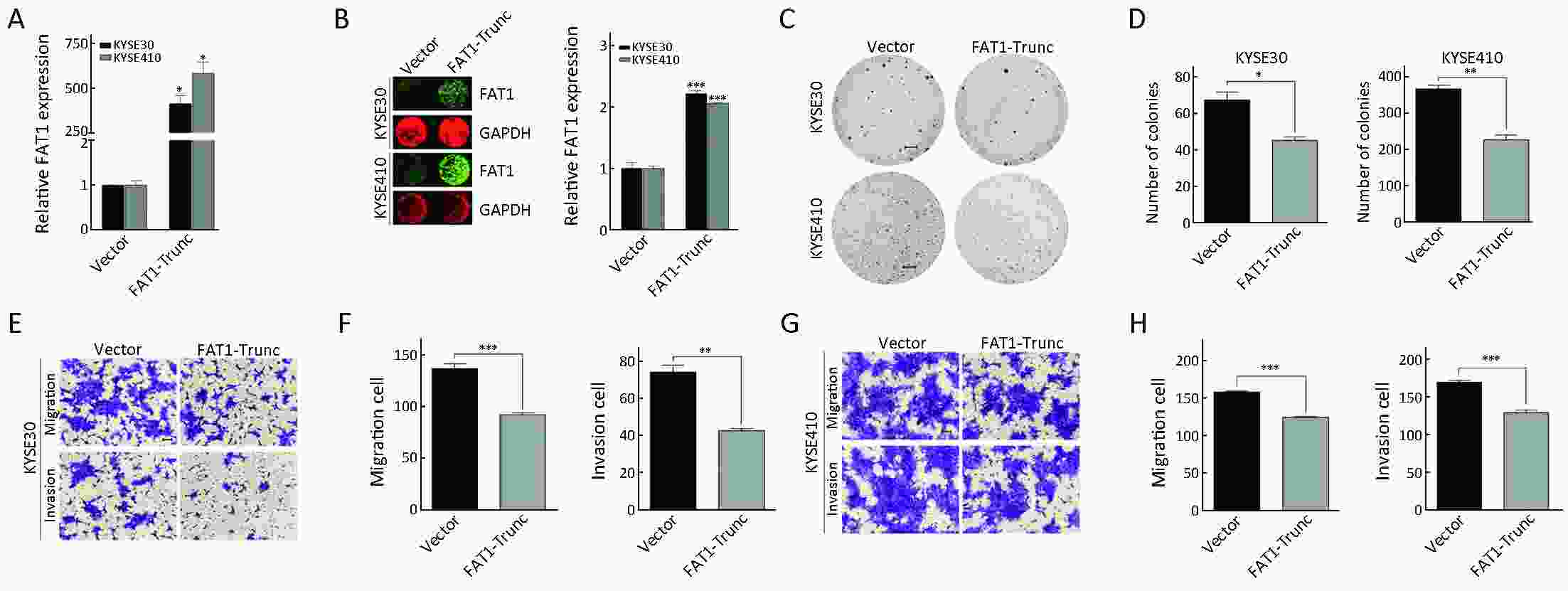
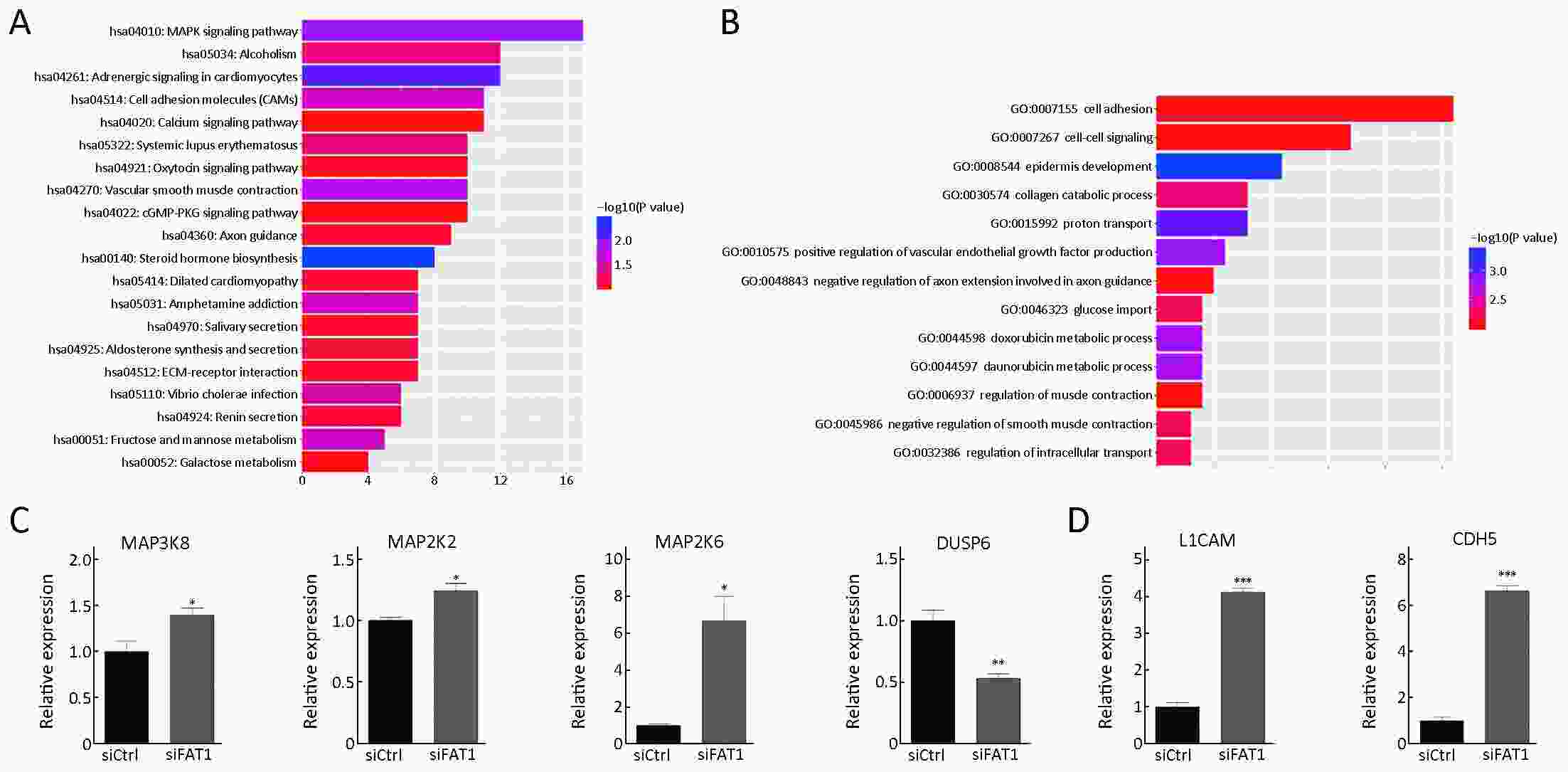
Objective Growing evidence indicates that FAT atypical cadherin 1 (FAT1) has aberrant genetic alterations and exhibits potential tumor suppressive function in esophageal squamous cell carcinoma (ESCC). However, the role of FAT1 in ESCC tumorigenesis remains not well elucidated. The aim of this study was to further investigate genetic alterations and biological functions of FAT1, as well as to explore its transcriptional regulation and downstream targets in ESCC. Methods The mutations of FAT1 in ESCC were achieved by analyzing a combined study from seven published genomic data, while the copy number variants of FAT1 were obtained from an analysis of our previous data as well as of The Cancer Genome Atlas (TCGA) and Cancer Cell Line Encyclopedia (CCLE) databases using the cBioPortal. The transcriptional regulation of FAT1 expression was investigated by chromatin immunoprecipitation (ChIP) and the luciferase reporter assays. In-cell western, Western blot and reverse transcription-quantitative polymerase chain reaction (RT-qPCR) were used to assess the indicated gene expression. In addition, colony formation and Transwell migration/invasion assays were employed to test cell proliferation, migration and invasion. Finally, RNA sequencing was used to study the transcriptomes. Results FAT1 was frequently mutated in ESCC and was deleted in multiple cancers. Furthermore, the transcription factor E2F1 occupied the promoter region of FAT1, and depletion of E2F1 led to a decrease in transcription activity and mRNA levels of FAT1. Moreover, we found that knockdown of FAT1 promoted KYSE30 and KYSE150 cell proliferation, migration and invasion; while overexpression of FAT1 inhibited KYSE30 and KYSE410 cell proliferation, migration and invasion. In addition, knockdown of FAT1 led to enrichment of the mitogen-activated protein kinase (MAPK) signaling pathway and cell adhesion process. Conclusions Our data provided evidence for the tumor suppressive function of FAT1 in ESCC cells and elucidated the transcriptional regulation of FAT1 by E2F1, which may facilitate the understanding of molecular mechanisms of the progression of ESCC.
2019, 31(4): 620-631.
doi: 10.21147/j.issn.1000-9604.2019.04.06
Abstract:
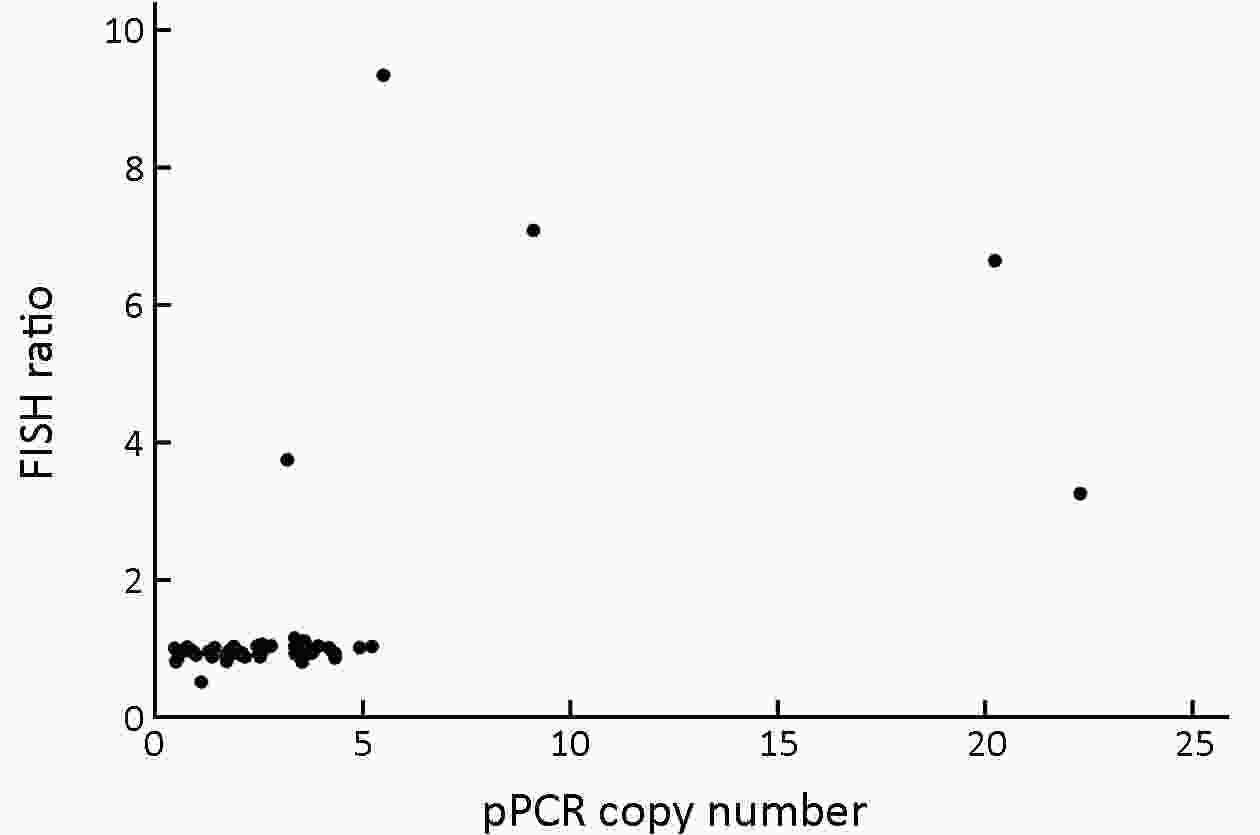
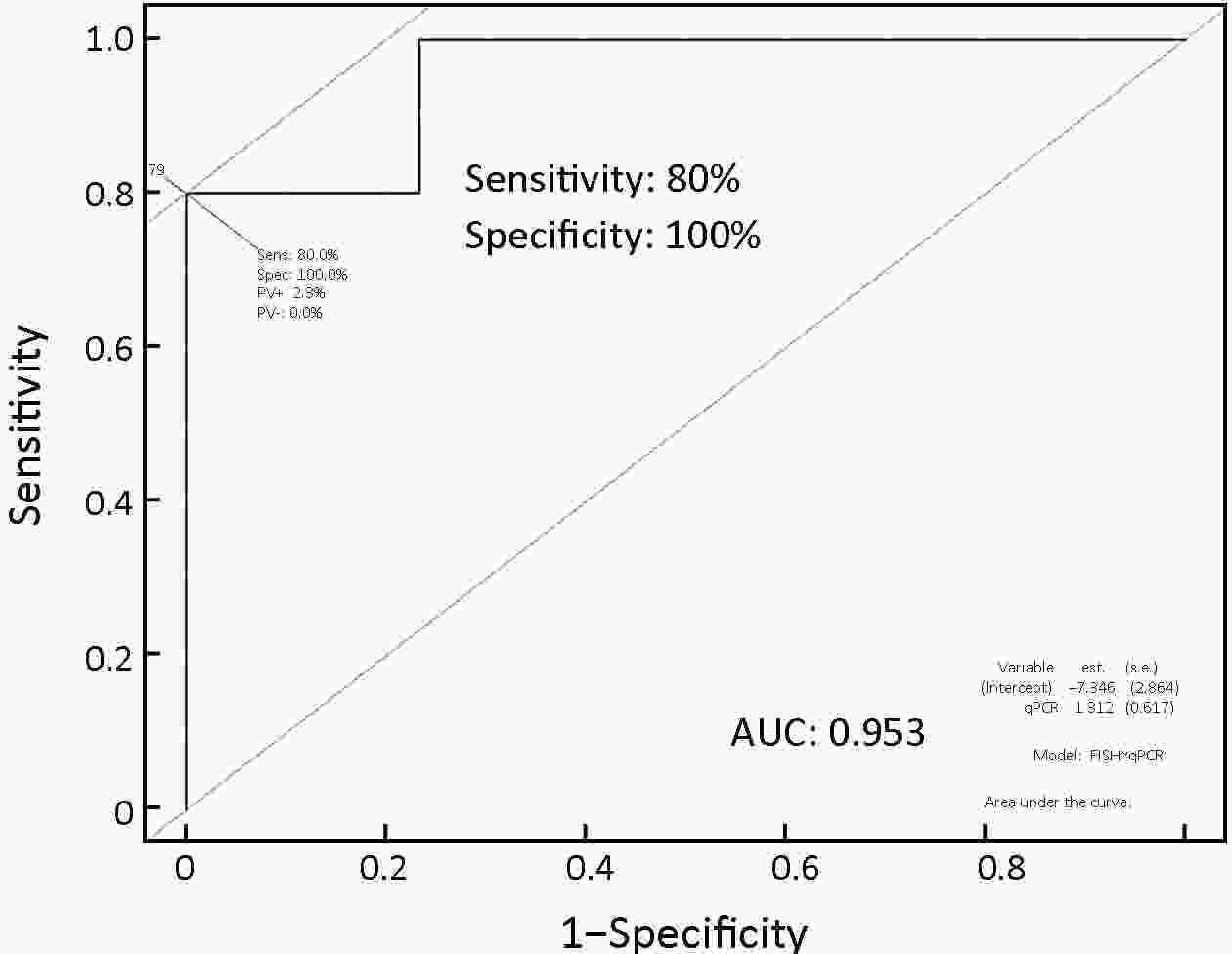
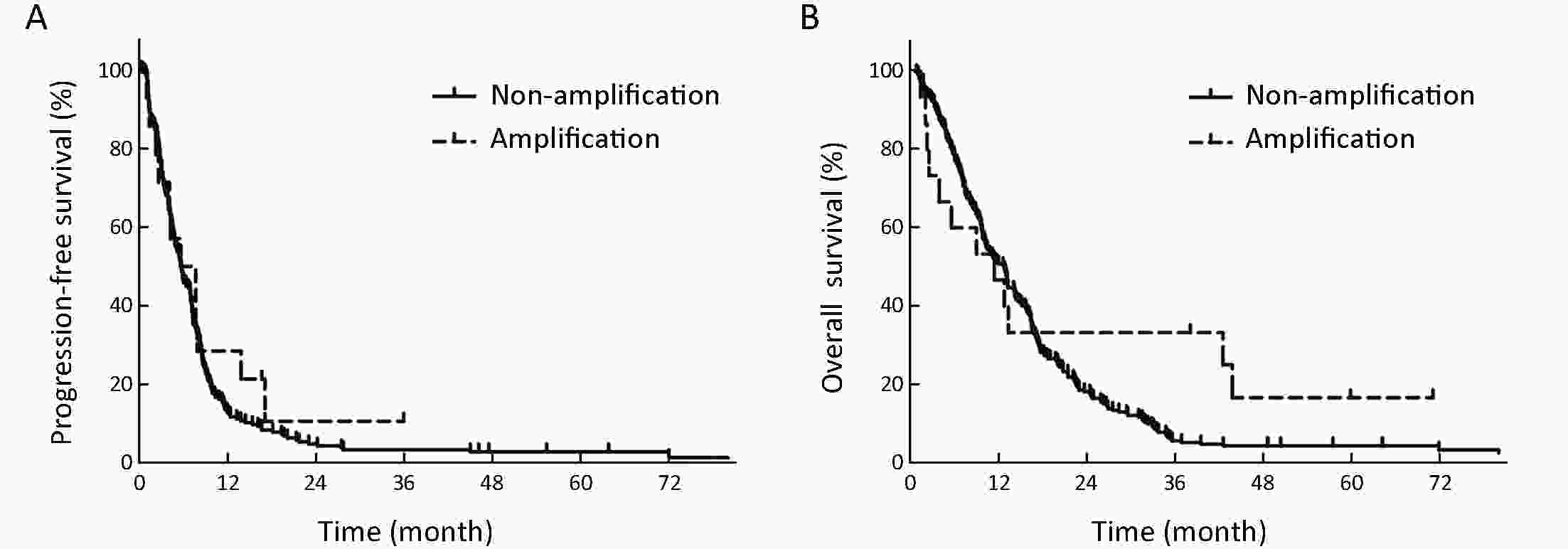
ObjectiveTo investigate the clinical significance of MET gene amplification in patients with gastric cancer in the palliative setting. MethodsMET amplification was assessed using fluorescence in situ hybridization (FISH) in 50 patients and quantitative polymerase chain reaction (qPCR) in 326 patients; 259 patients treated with first-line fluoropyrimidine and platinum were included for survival analysis. ResultsThe results of FISH and qPCR indicated that the c-MET/CEP7 ratio was correlated with gene copy number. The optimal cutoff value for the copy number using qPCR to detect MET gene amplification with FISH was 5 (κ=0.778, P<0.001). Twenty-one out of 326 patients (6.4%) were identified as MET amplification with a copy number of >5 detected by qPCR. MET-amplified gastric cancer was associated with an Eastern Cooperative Oncology Group (ECOG) performance status (PS) score of ≥2 (33.3% vs. 10.5% P=0.007), peritoneal metastasis (76.2% vs. 46.2%, P=0.008), and elevated bilirubin levels (28.6% vs. 7.3%, P=0.006). The median overall survival (OS) and progression-free survival (PFS) were 11.9 and 5.6 months, respectively. MET-amplified gastric cancer was not associated with survival outcomes [hazard ratio (HR)=0.68, 95% confidence interval (95% CI): 0.35−1.32, P=0.254 for PFS; HR=0.68, 95% CI: 0.35−1.32, P=0.251 for OS]. ConclusionsqPCR can be used to detect MET gene amplification. MET amplification was not a predictor of poor prognosis in patients with metastatic or unresectable gastric cancer.
2019, 31(4): 632-640.
doi: 10.21147/j.issn.1000-9604.2019.04.07
Abstract:
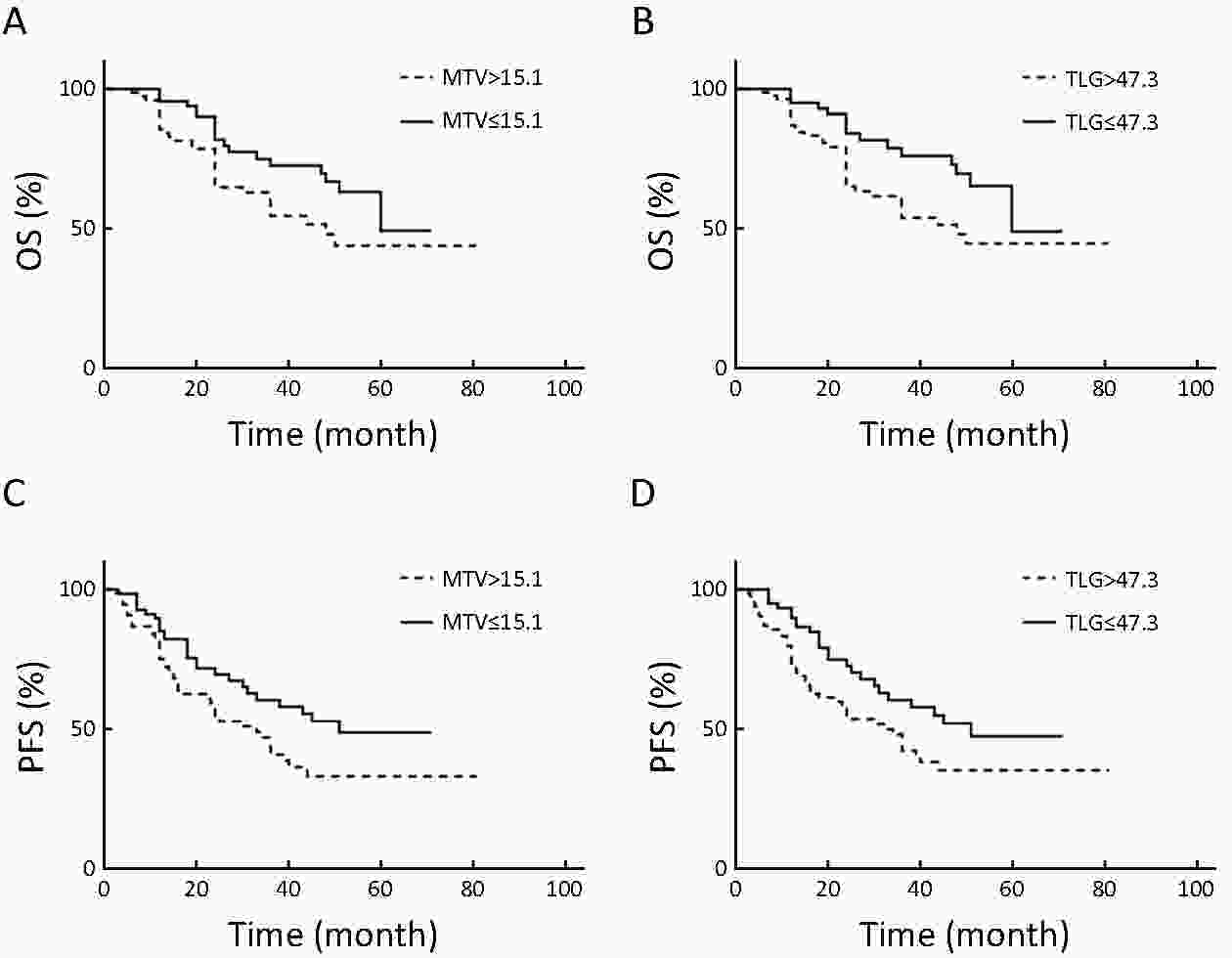
Objective The present study investigated the prognosis value of preoperative fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) in patients with local advanced gastric cancer (LAGC). Methods In total, 144 patients [median age 63 (range: 48−80) years old] with LAGC underwent 18F-FDG PET/CT prior to any treatment. The maximum standardized uptake values (SUVmax), mean standardized uptake values (SUVmean), metabolic tumor volume (MTV) and total lesion glycolysis (TLG) of the primary lesion were measured on PET/CT and correlated with clinicopathological features and survival. Results Significant differences in SUVmean, SUVmax, MTV and TLG were found according to Lauren’s classification, histologic grade and T category (P<0.05). During the 26.5-month follow-up, 51 (35.4%) patients died and 70 (48.6%) exhibited disease progression. The optimal thresholds of MTV and TLG were 15.1 cm3 and 47.3 cm3, respectively. The 3-year progression-free survival (PFS) and overall survival (OS) for patients with high TLG values were 30% and 38% compared to 38% and 47% for low TLG values, respectively (P<0.05). Univariate and multifactor analyses demonstrated that lymph node metastasis and T stage were independent prognostic factors for PFS; T stage, histologic grade and TLG were independent prognostic factors for OS (P<0.05). Molecular markers had no relationship with patient’s outcomes. Conclusions Metabolic activity of primary gastric tumors from 18F-FDG PET/CT is a prognostic factor in patients with LAGC.
2019, 31(4): 641-652.
doi: 10.21147/j.issn.1000-9604.2019.04.08
Abstract:
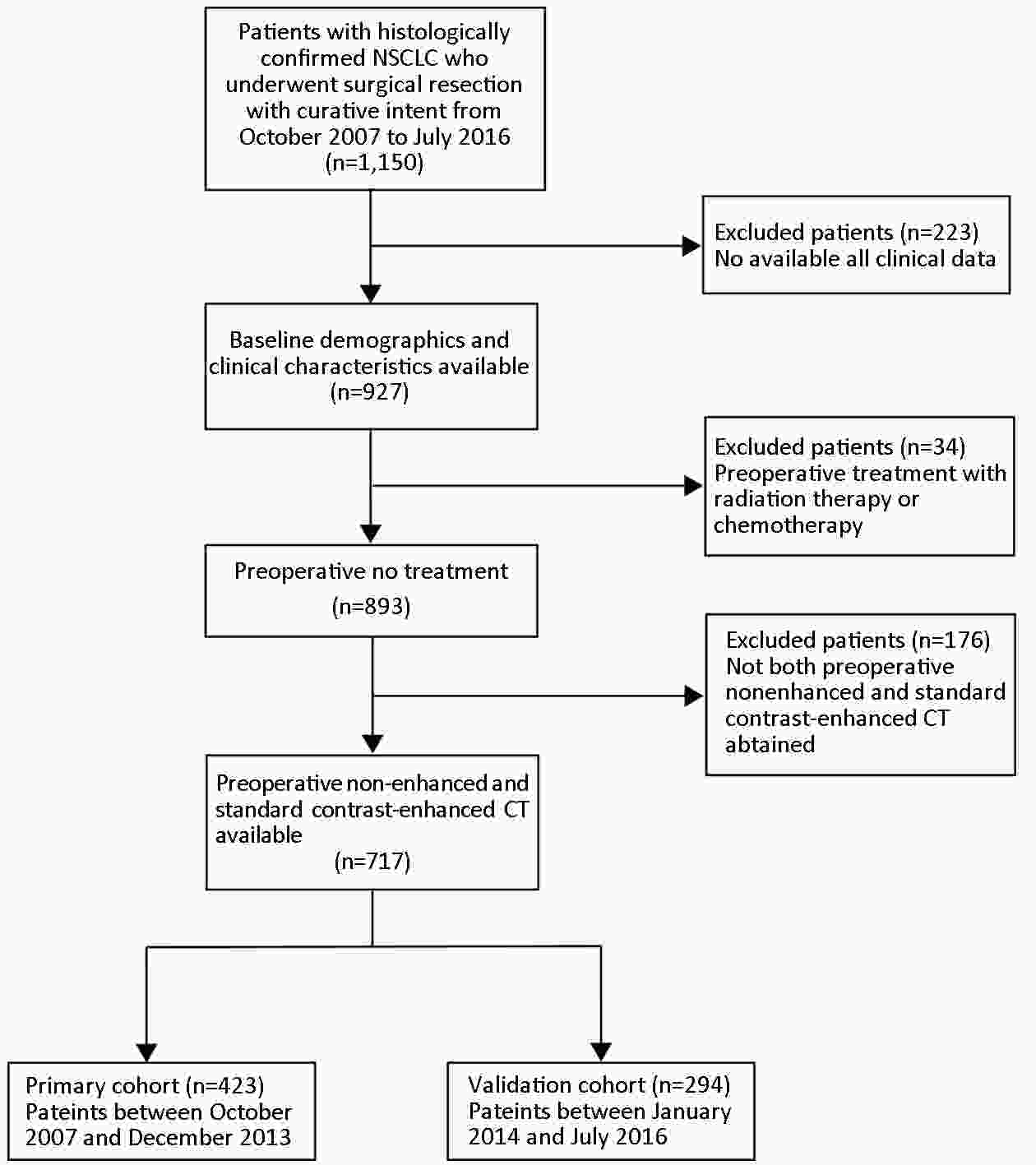
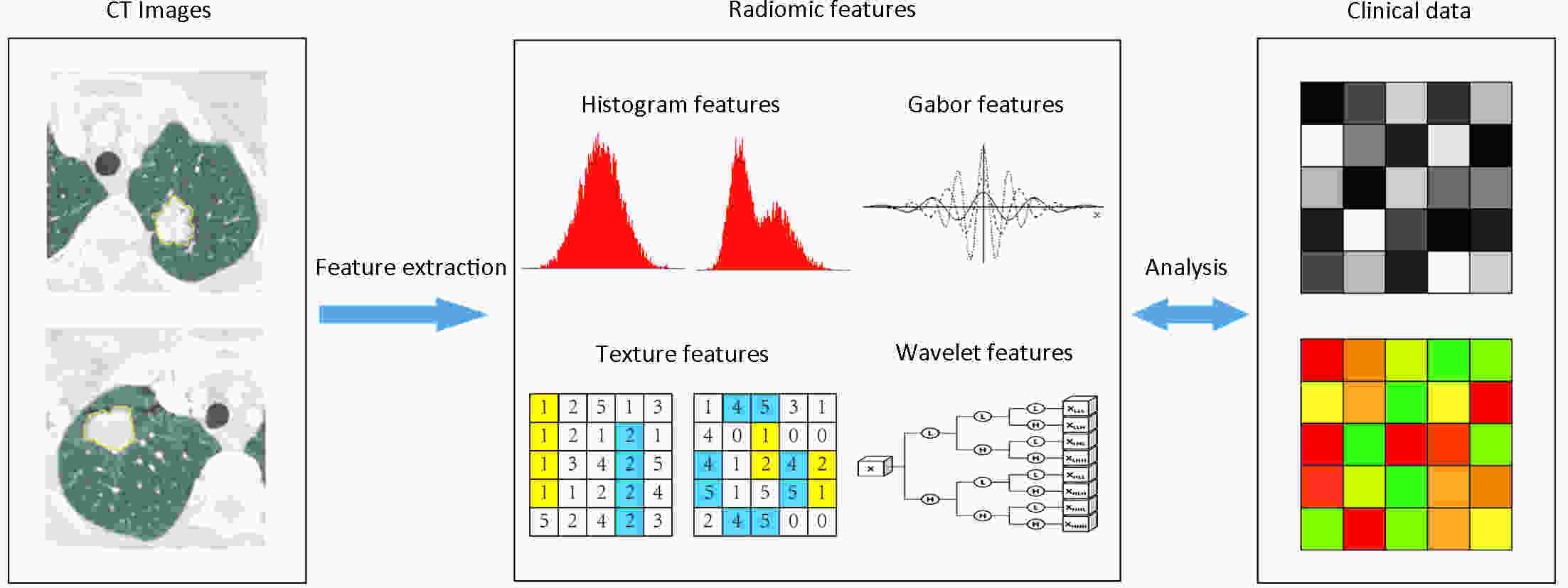
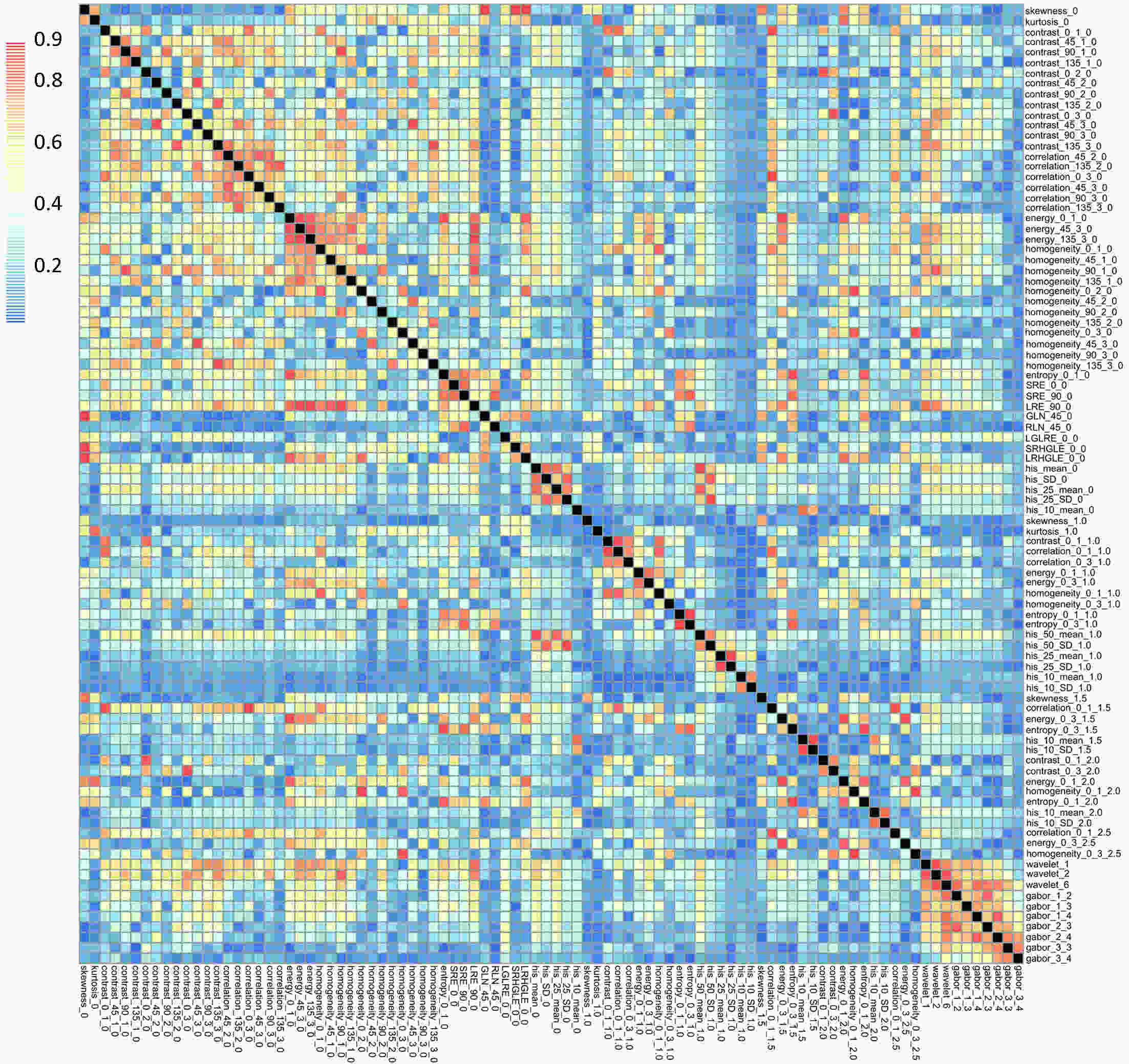
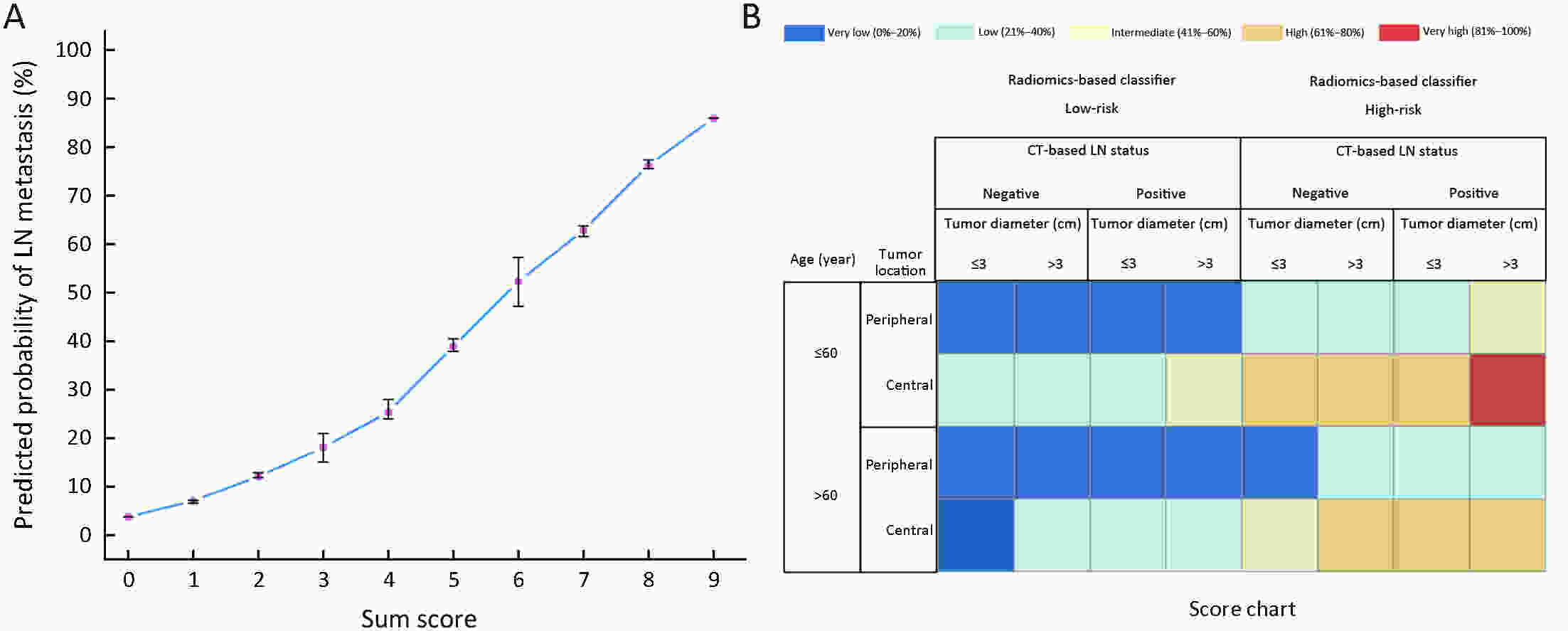
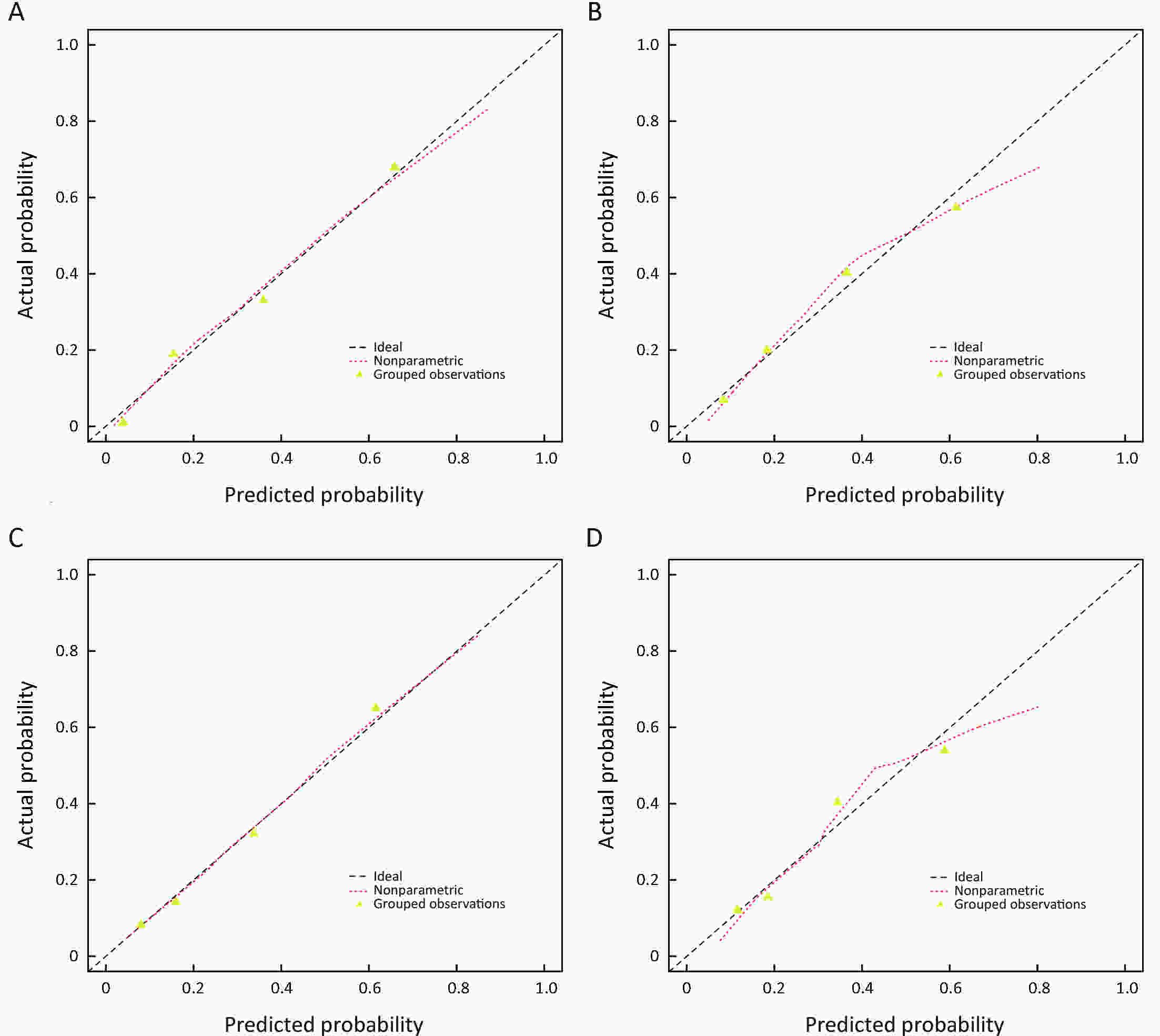
ObjectiveTo develop and validate a radiomics-based predictive risk score (RPRS) for preoperative prediction of lymph node (LN) metastasis in patients with resectable non-small cell lung cancer (NSCLC). MethodsWe retrospectively analyzed 717 who underwent surgical resection for primary NSCLC with systematic mediastinal lymphadenectomy from October 2007 to July 2016. By using the method of radiomics analysis, 591 computed tomography (CT)-based radiomics features were extracted, and the radiomics-based classifier was constructed. Then, using multivariable logistic regression analysis, a weighted score RPRS was derived to identify LN metastasis. Apparent prediction performance of RPRS was assessed with its calibration, discrimination, and clinical usefulness. ResultsThe radiomics-based classifier was constructed, which consisted of 13 selected radiomics features. Multivariate models demonstrated that radiomics-based classifier, age group, tumor diameter, tumor location, and CT-based LN status were independent predictors. When we assigned the corresponding score to each variable, patients with RPRSs of 0−3, 4−5, 6, 7−8, and 9 had distinctly very low (0%−20%), low (21%−40%), intermediate (41%−60%), high (61%−80%), and very high (81%−100%) risks of LN involvement, respectively. The developed RPRS showed good discrimination and satisfactory calibration [C-index: 0.785, 95% confidence interval (95% CI): 0.780−0.790]. Additionally, RPRS outperformed the clinicopathologic-based characteristics model with net reclassification index (NRI) of 0.711 (95% CI: 0.555−0.867). ConclusionsThe novel clinical scoring system developed as RPRS can serve as an easy-to-use tool to facilitate the preoperatively individualized prediction of LN metastasis in patients with resectable NSCLC. This stratification of patients according to their LN status may provide a basis for individualized treatment.
2019, 31(4): 653-662.
doi: 10.21147/j.issn.1000-9604.2019.04.09
Abstract:
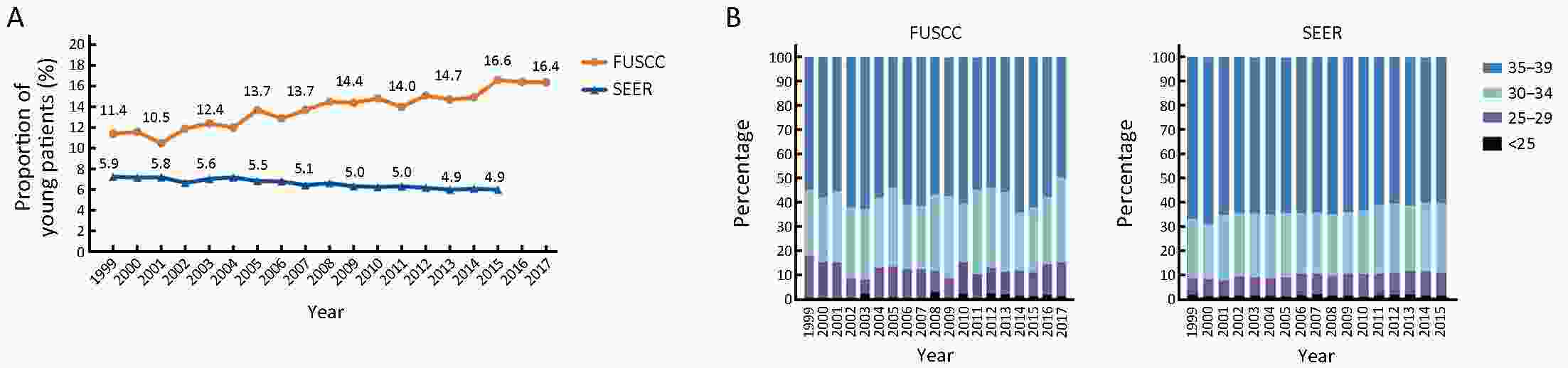
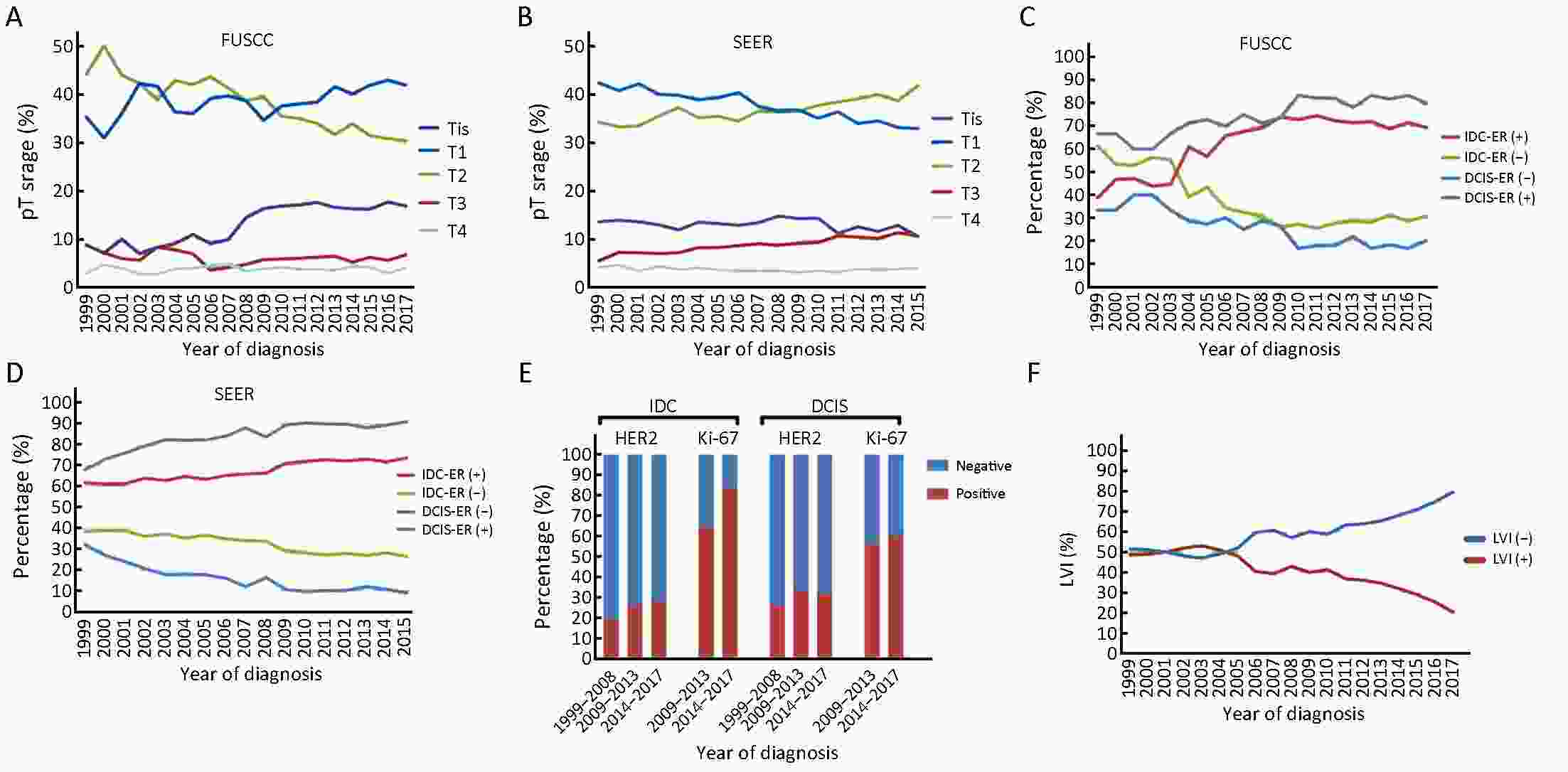
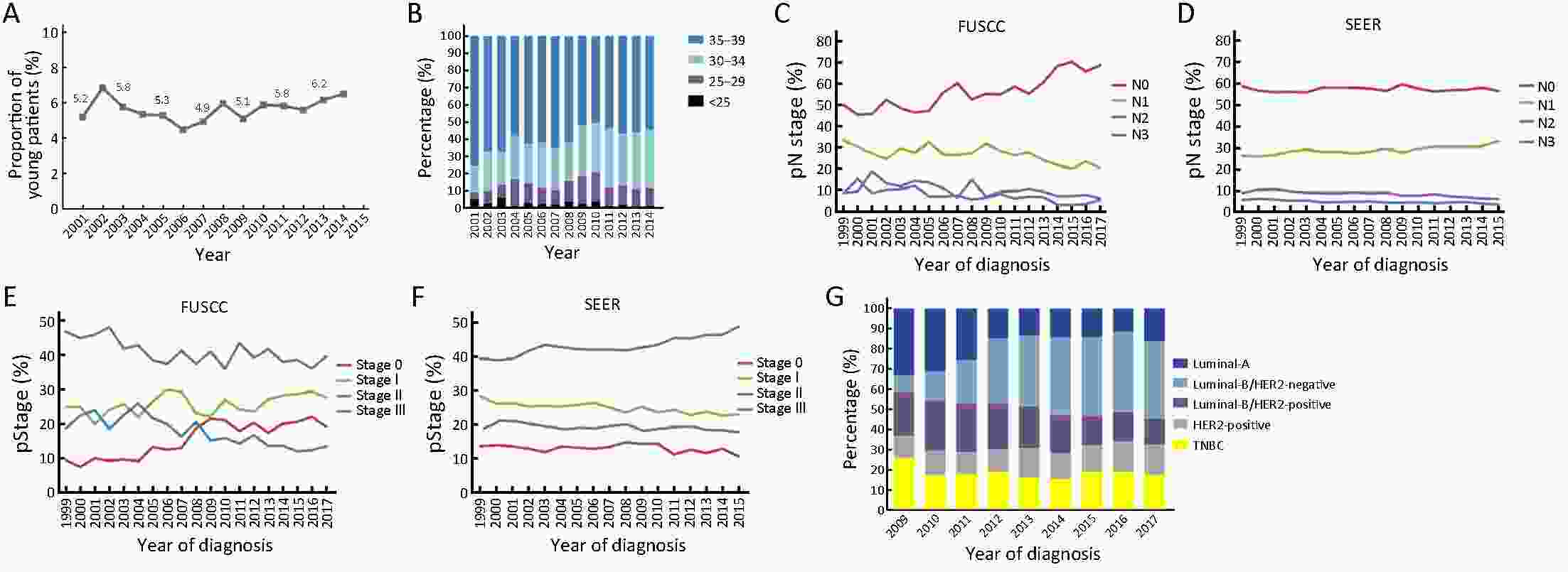
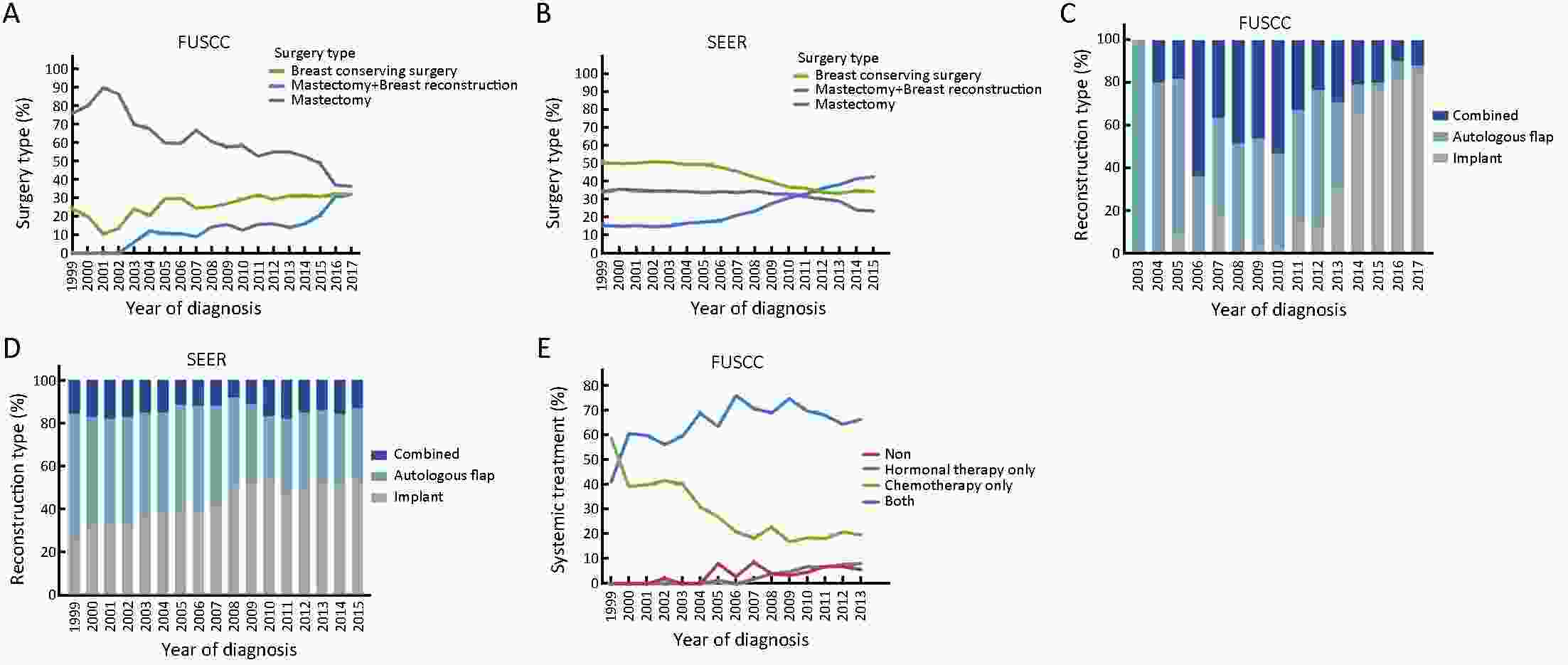
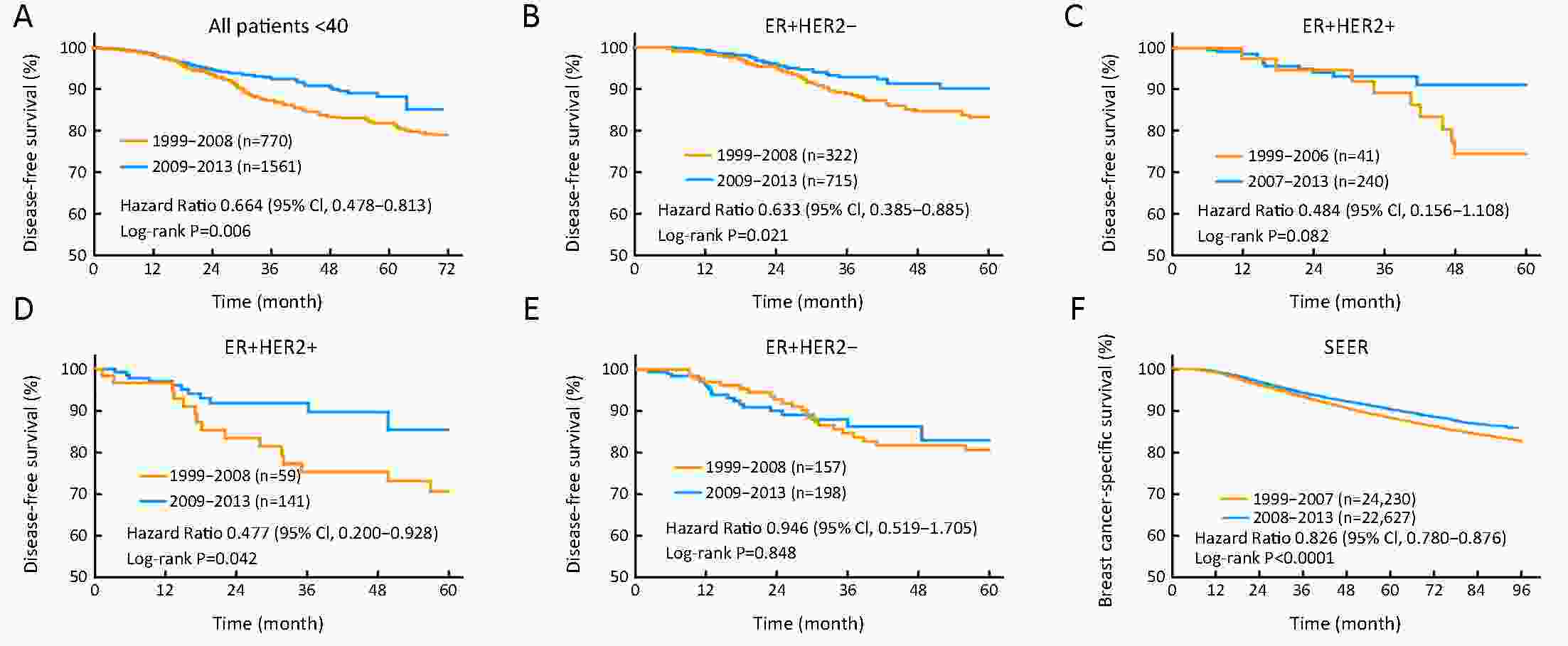
ObjectiveBreast cancer in young females was usually considered more aggressive and requires aggressive therapy. We investigated whether early detection and improved treatments changed the patterns of characteristics, management and outcomes of young breast cancer patients over time. MethodsFemales under 40 years of age diagnosed with breast cancer during the periods 1999−2017 and 1999−2015 were identified in the Fudan University Shanghai Cancer Center (FUSCC) and the population-based Surveillance, Epidemiology, and End Results (SEER) registry, respectively. Clinicopathologic characteristics and treatment information were collected. Patients diagnosed before 2013 were followed up. ResultsThe proportions of young breast cancer patients were 15.0% and 5.3% in the FUSCC and SEER cohorts, respectively. In the FUSCC cohort, there was a significant increase in the proportion of ductal carcinoma in situ (DCIS) (from 8.8% to 16.9%; P<0.0001) and it remained stable in SEER cohort. The proportion of T1-stage tumors increased dramatically in the FUSCC cohort (from 35.3% to 41.9%; P=0.008), whereas it decreased in SEER cohort (from 42.4% to 33.0%; P<0.0001). The percentage of estrogen receptor (ER)-positive cancers was consistently increased in both the invasive ductal carcinoma (IDC) and DCIS patients in the two cohorts. Breast-conserving surgery and immediate implant reconstruction after mastectomy both exhibited increased use over time in the FUSCC cohort. Both the FUSCC and SEER cohorts showed a significantly better prognosis in the recent time period. ConclusionsWith the increased early-stage and ER-positive diseases in young patients as well as better systemic treatment strategies, improved survival has been observed in recent years. There has been a substantial de-escalation in surgical therapies in young breast cancer patients.
2019, 31(4): 663-672.
doi: 10.21147/j.issn.1000-9604.2019.04.10
Abstract:
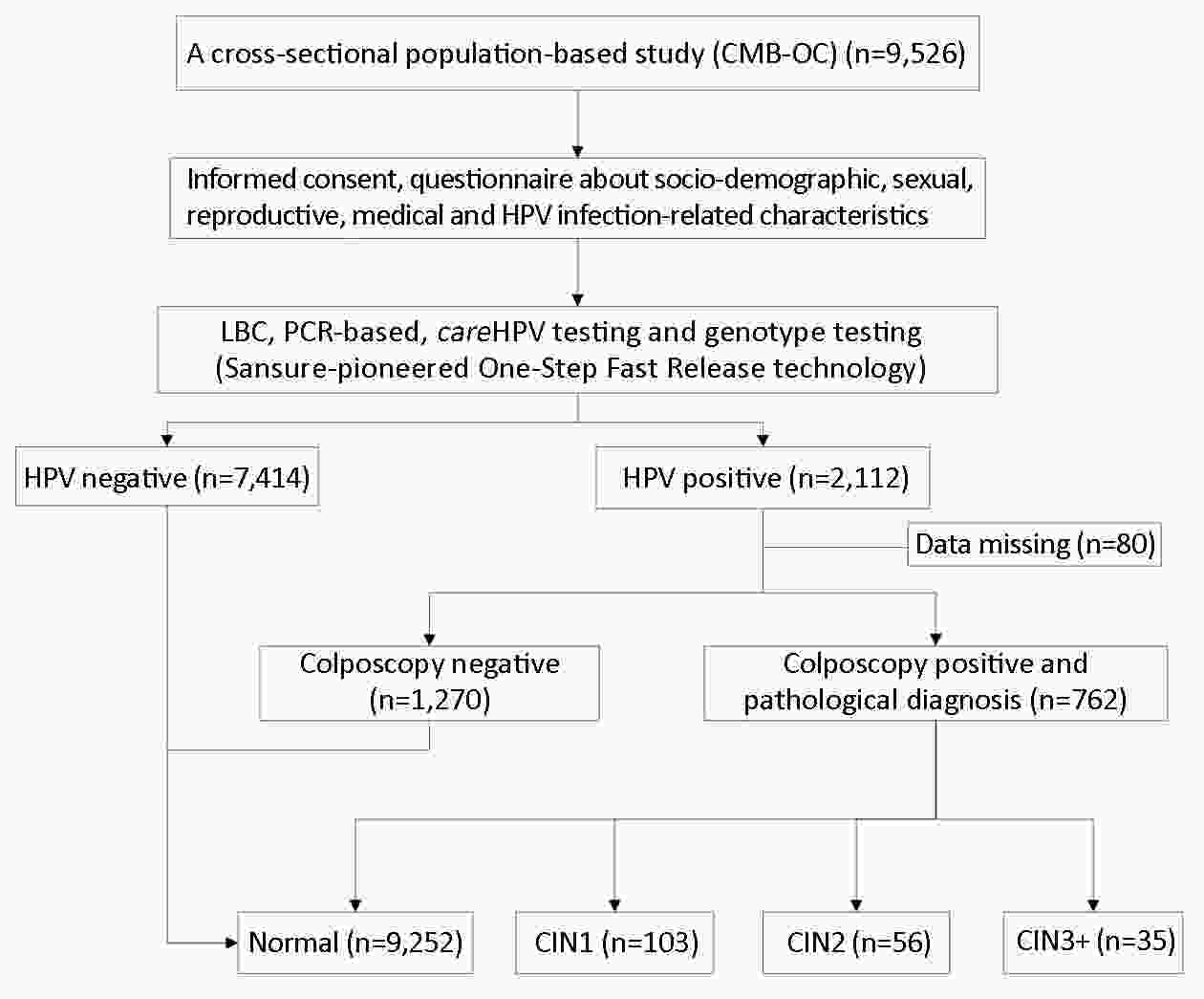
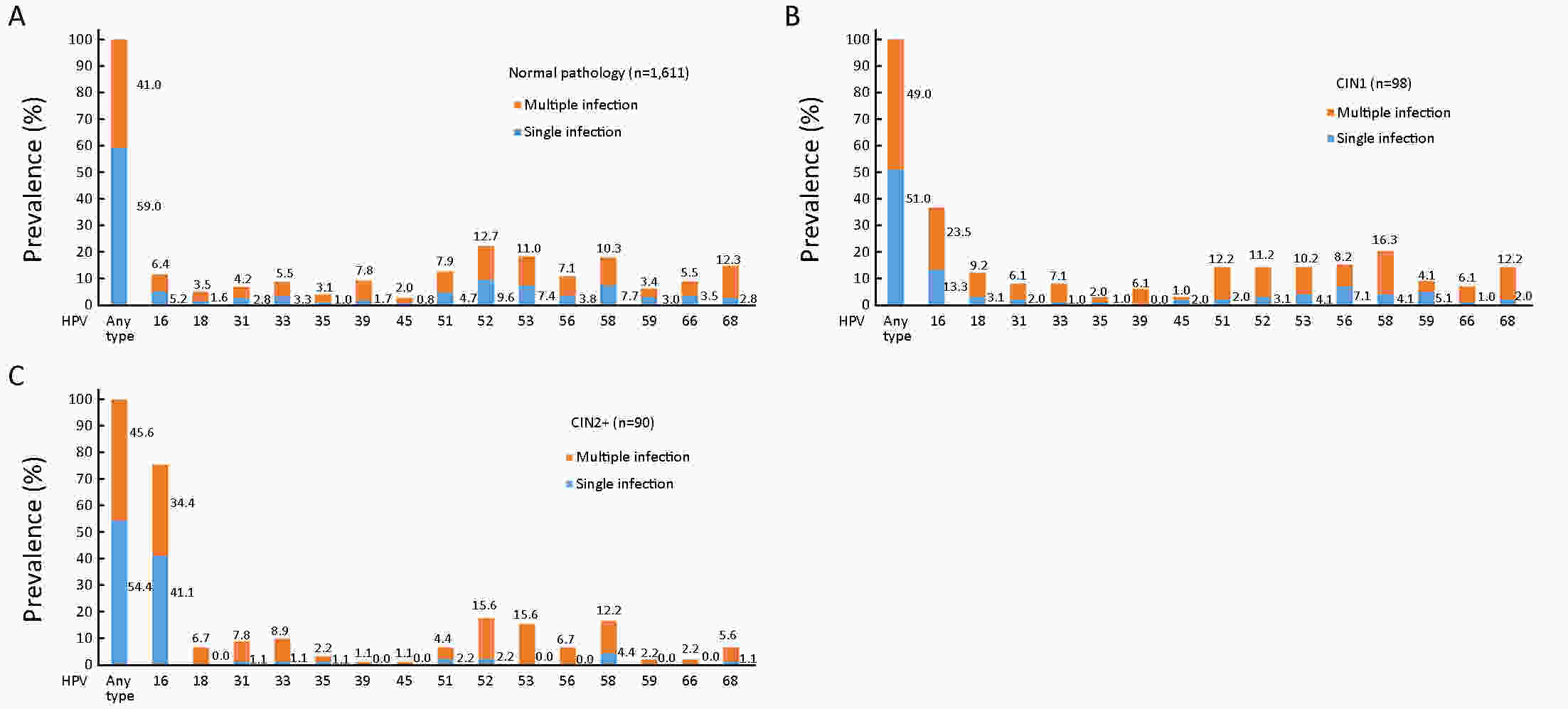
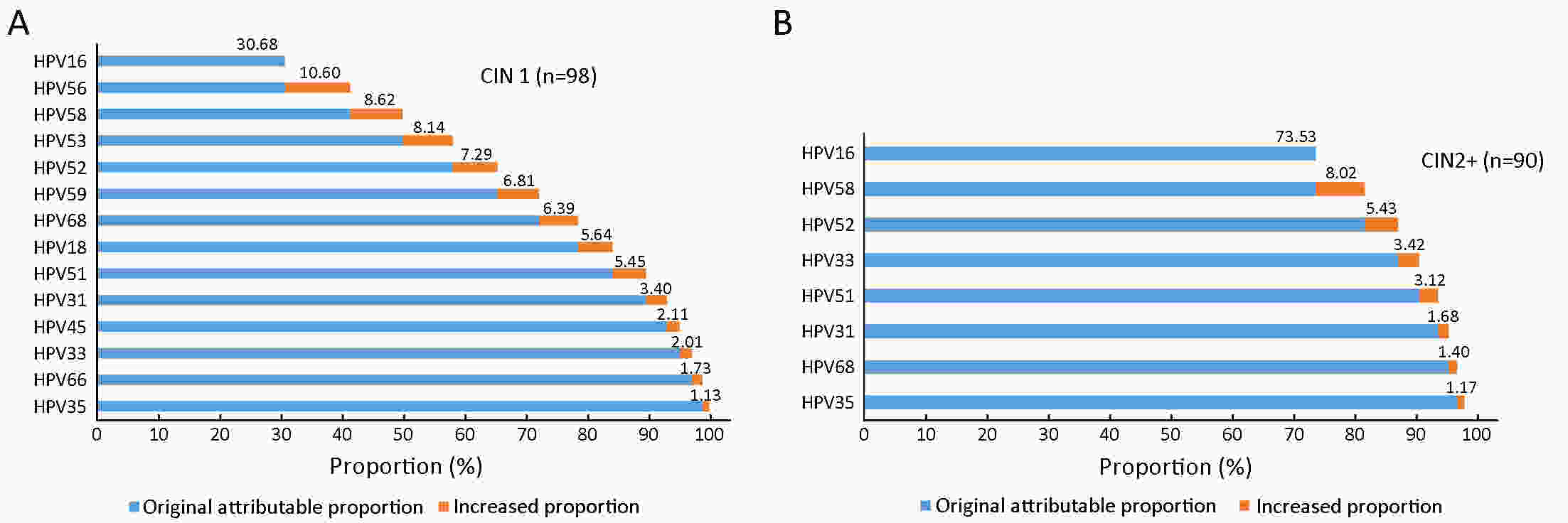
ObjectivePrecise prevention is more desired for cervical cancer due to the huge population, high prevalence of human papillomavirus (HPV) infection in China and the vision of screen-and-treat strategies in low- and middle-income countries (LMICs). Considerations of combining type-specific prevalence and attribution proportion to high-grade cervical intraepithelial neoplasia are informative to more precise and effective region-specific cervical cancer prevention and control programs. The aim of the current study was to determine the genotype distribution of HPV and attribution to cervical precancerous lesions among women from rural areas in North China. MethodsA total of 9,526 women participated in the cervical cancer screening project in rural China. The samples of women who tested positive for HPV were retested with a polymerase chain reaction (PCR)-based HPV genotyping test. The attribution proportion of specific high-risk human papillomavirus (HR-HPV) types for different grades of cervical lesions was calculated by using the type contribution weighting method. ResultsA total of 22.2% (2,112/9,526) of women were HR-HPV positive and HPV52 (21.7%) was the most common HR-HPV genotype, followed by HPV58 (18.2%), HPV53 (18.2%) and HPV16 (16.2%). The top three genotypes detected in HR-HPV-positive cervical intraepithelial neoplasia (CIN)1 were HPV16 (36.7%), HPV58 (20.4%), HPV56 (15.3%). Among CIN2+, the most frequent genotypes were HPV16 (75.6%), HPV52 (17.8%), HPV58 (16.7%). HPV16, 56, 58, 53, 52, 59, 68, and 18 combined were attributed to 84.17% of all CIN1 lesions, and HPV16, 58, and 52 combined were attributed to 86.98% of all CIN2+ lesions. ConclusionsThe prevalence of HR-HPV infection among women from rural areas in North China was high and HPV16, HPV58, HPV52 had paramount attributable fraction in CIN2+. Type-specific HPV prevalence and attribution proportion to cervical precancerous lesions should be taken into consideration in the development of vaccines and strategy for screening in this population.
2019, 31(4): 673-685.
doi: 10.21147/j.issn.1000-9604.2019.04.11
Abstract:
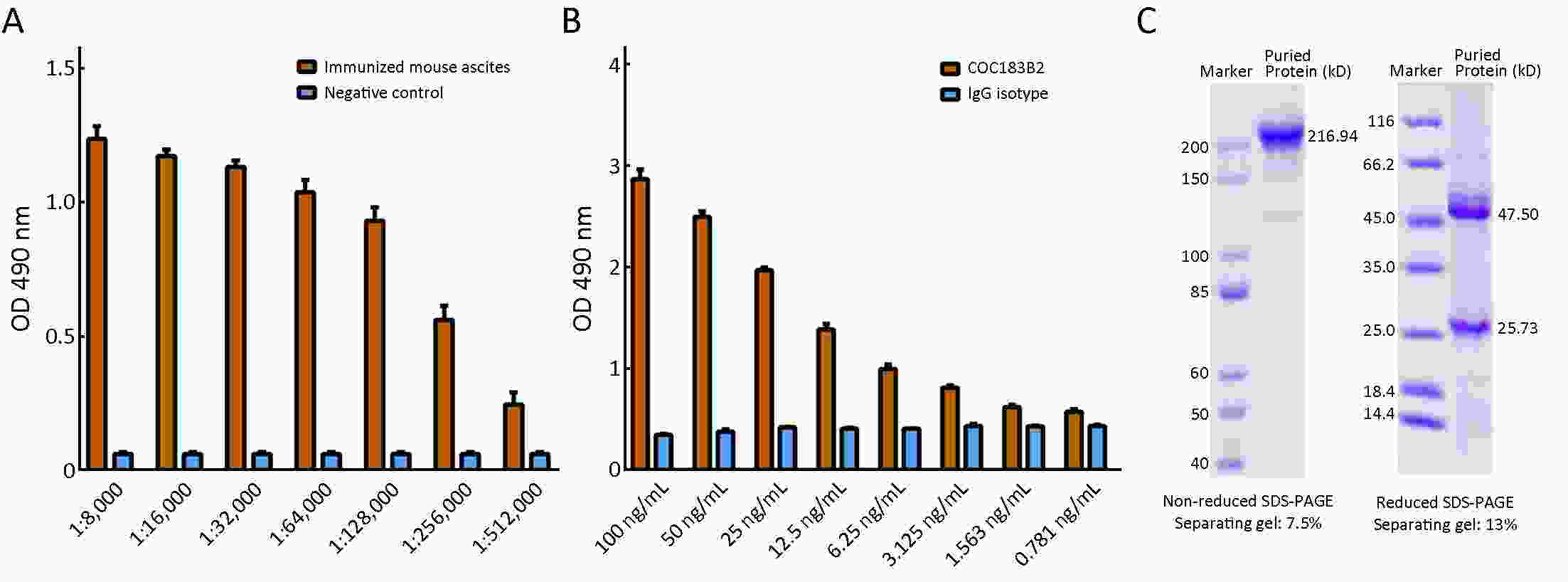
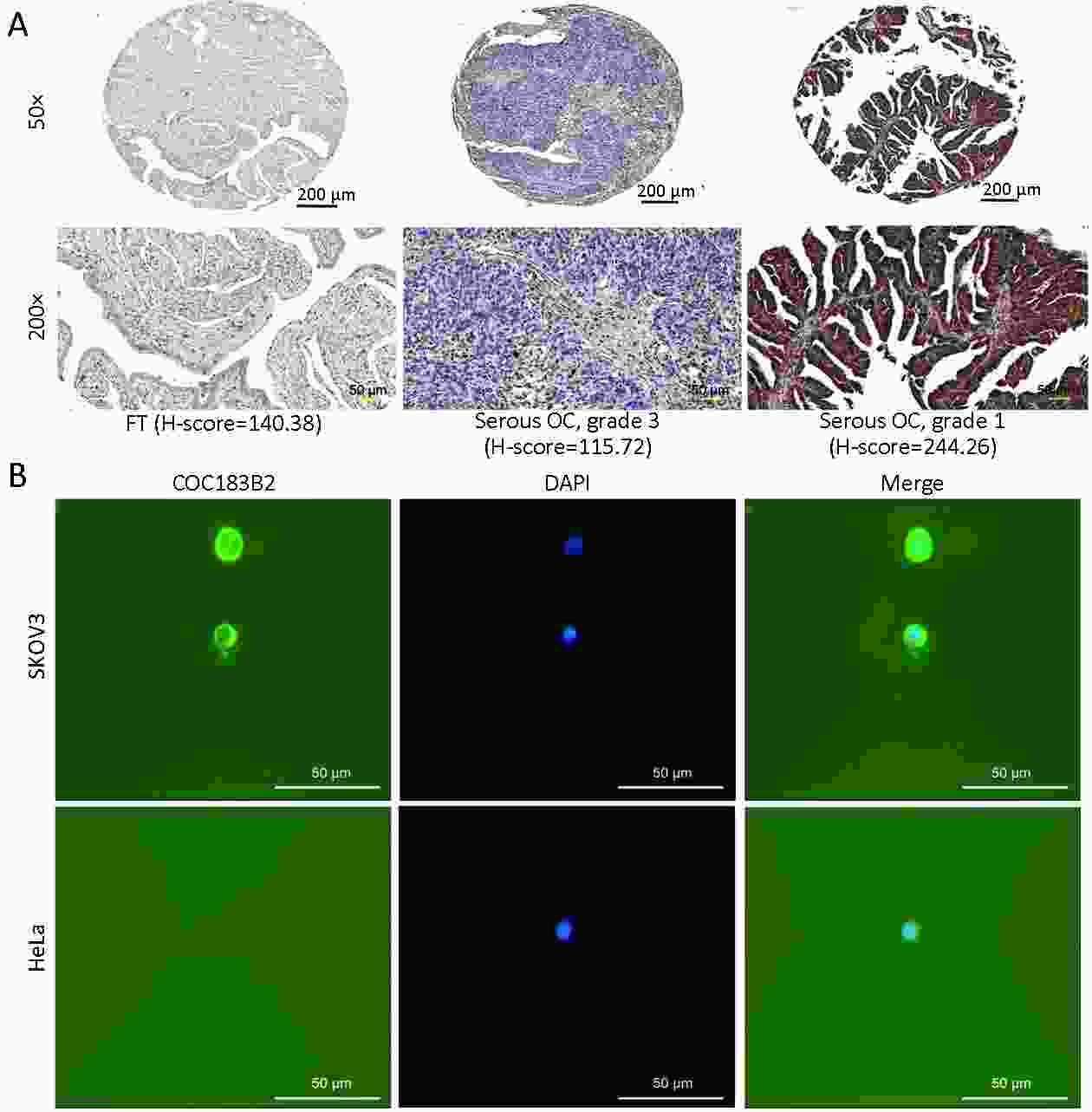
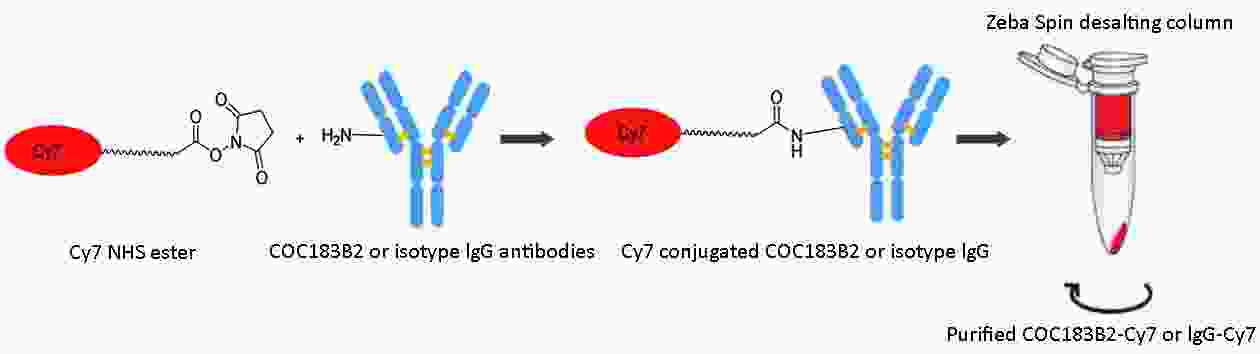
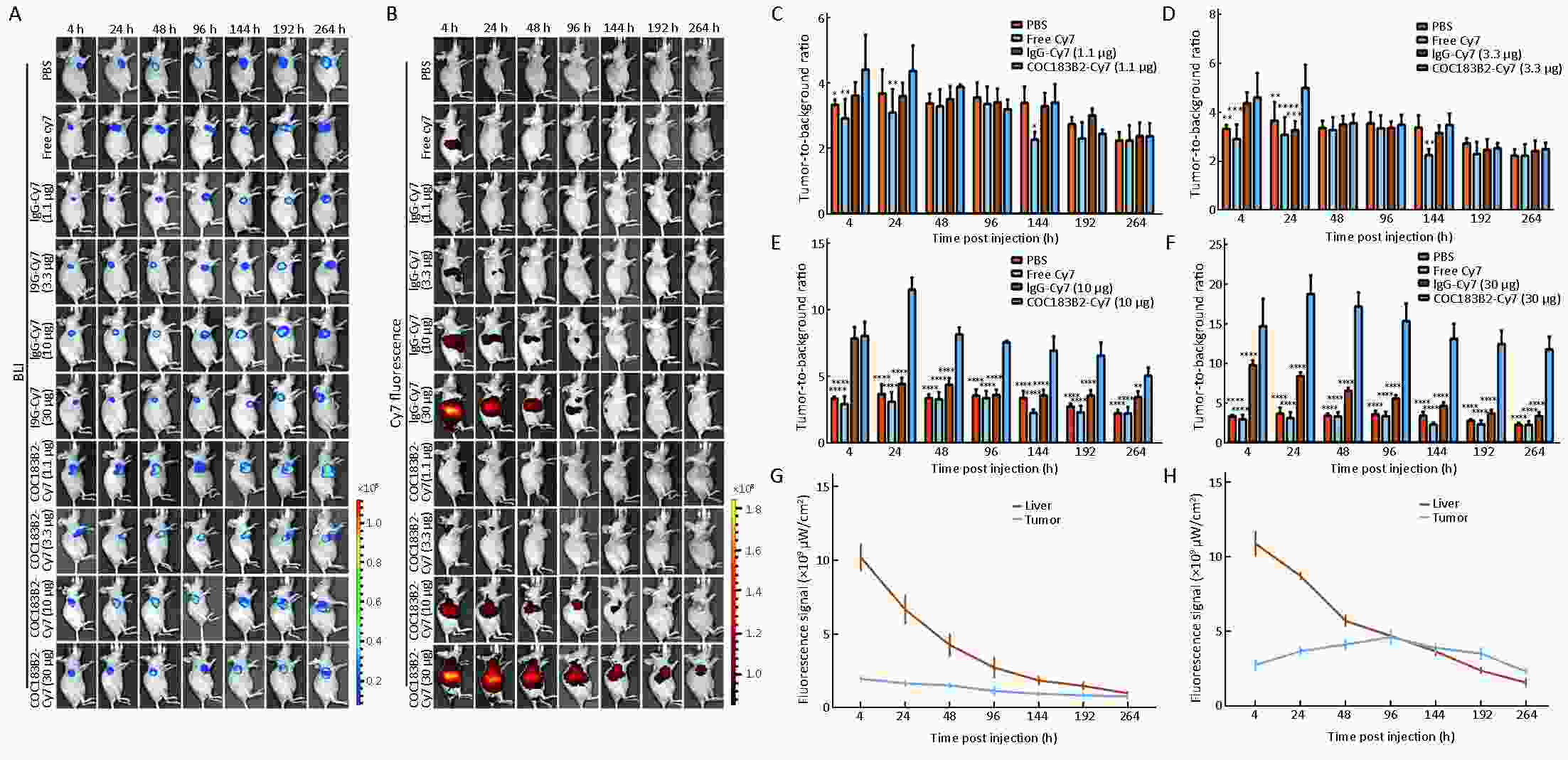
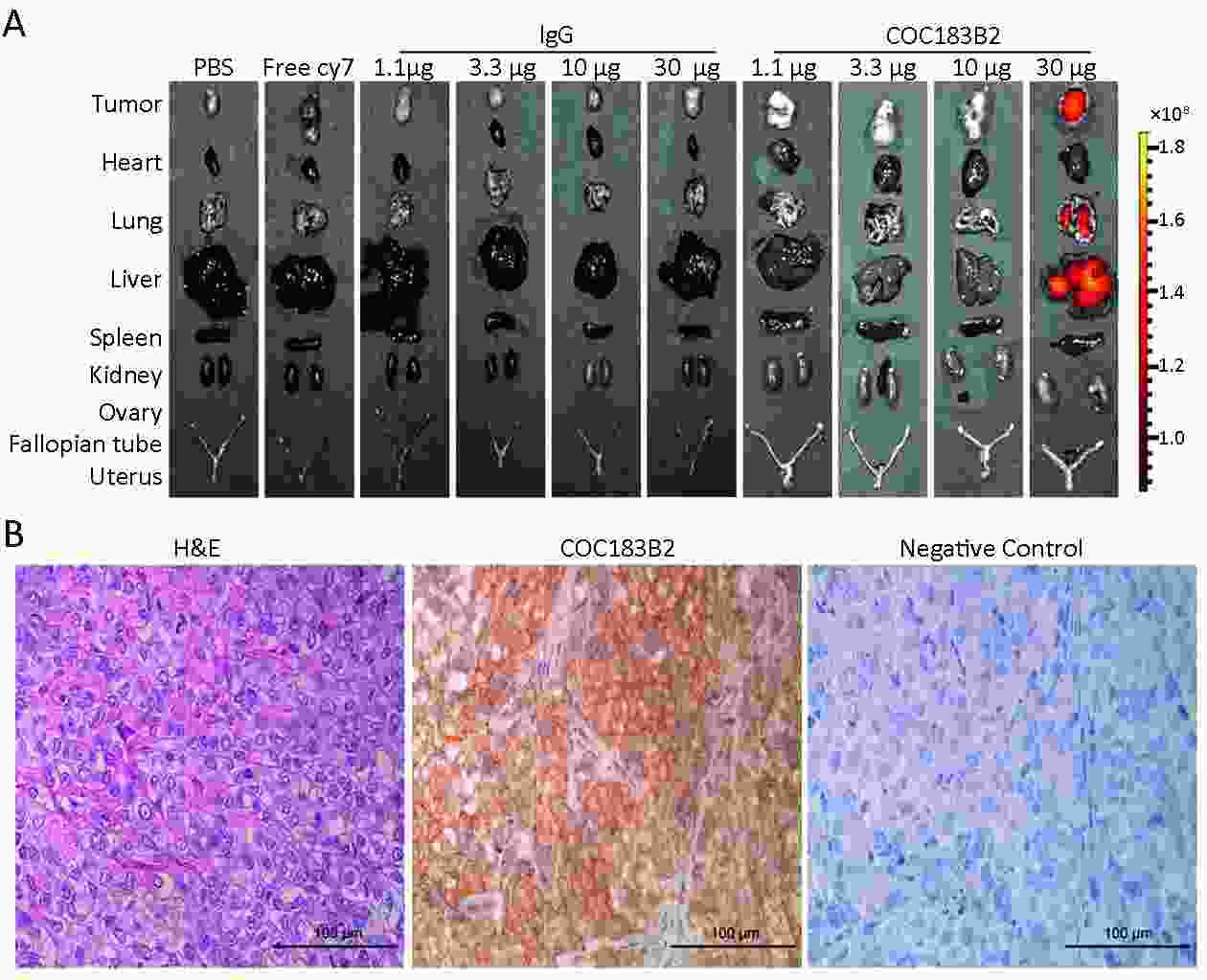
Objective To evaluate the imaging potential of a novel near-infrared (NIR) probe conjugated to COC183B2 monoclonal antibodies (MAb) in ovarian cancer (OC). Methods The expression of OC183B2 antigen in OC was determined by immunohistochemical (IHC) staining using tissue microarrays with the H-score system and immunofluorescence (IF) staining of tumor cell lines. Imaging probes with the NIR fluorescent dye cyanine 7 (Cy7) conjugated to COC183B2 Mab were chemically engineered. OC183B2-positive human OC cells (SKOV3-Luc) were injected subcutaneously into BALB/c nude mice. Bioluminescent imaging (BLI) was performed to detect tumor location and growth. COC183B2-Cy7 at 1.1, 3.3, 10, or 30 μg were used for in vivo fluorescence imaging, and phosphate-buffered saline (PBS), free Cy7 dye and mouse isotype immunoglobulin G (IgG)-Cy7 (delivered at the same doses as COC183B2-Cy7) were used as controls. Results The expression of OC183B2 with a high H-score was more prevalent in OC tissue than fallopian tube (FT) tissue. Among 417 OC patients, the expression of OC183B2 was significantly correlated with the histological subtype, histological grade, residual tumor size, relapse state and survival status. IF staining demonstrated that COC183B2 specifically expressed in SKOV3 cells but not HeLa cells. In vivo NIR fluorescence imaging indicated that COC183B2-Cy7 was mainly distributed in the xenograft and liver with optimal tumor-to-background (T/B) ratios in the xenograft at 30 μg dose. The highest fluorescent signals in the tumor were observed at 96 h post-injection (hpi). Ex vivo fluorescence imaging revealed the fluorescent signals mainly from the tumor and liver. IHC analysis confirmed that xenografts were OC183B2 positive. Conclusions COC183B2 is a good candidate for NIR fluorescence imaging and imaging-guided surgery in OC.
2019, 31(4): 686-698.
doi: 10.21147/j.issn.1000-9604.2019.04.12
Abstract:
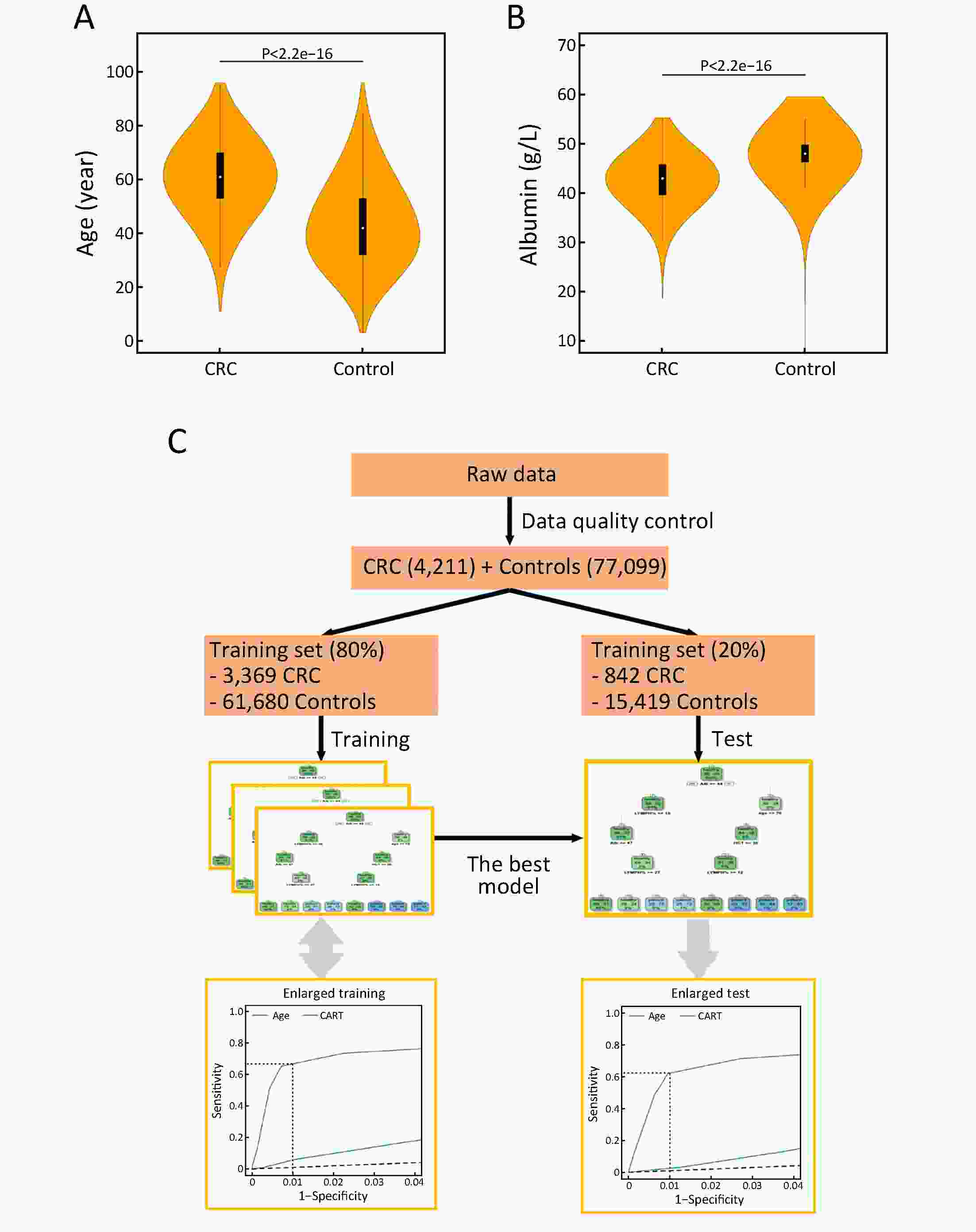
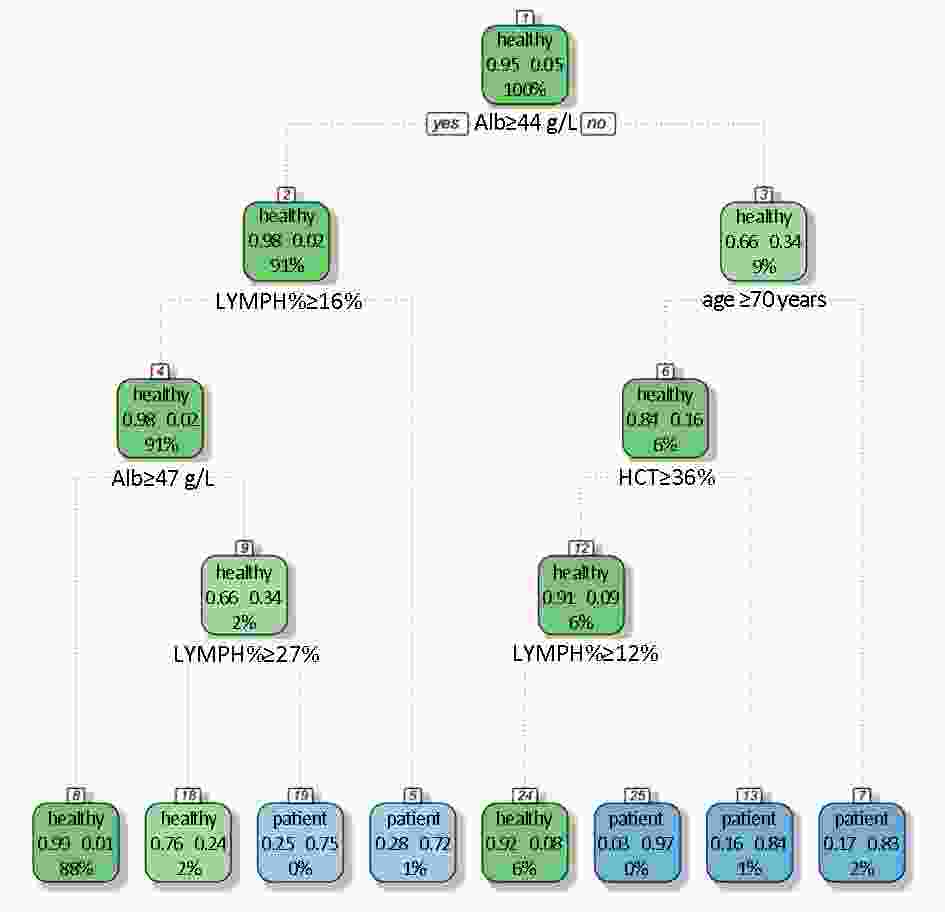
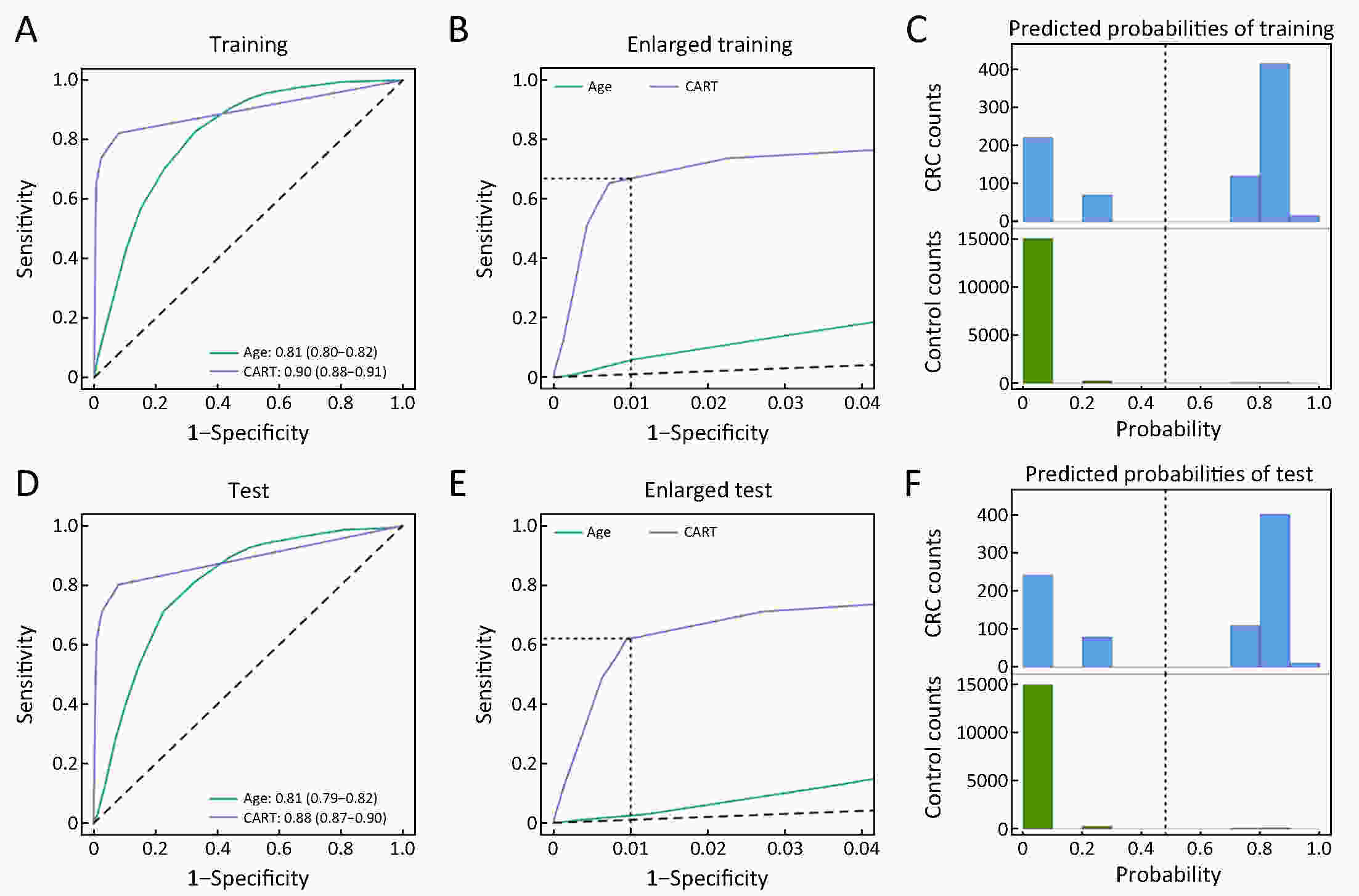
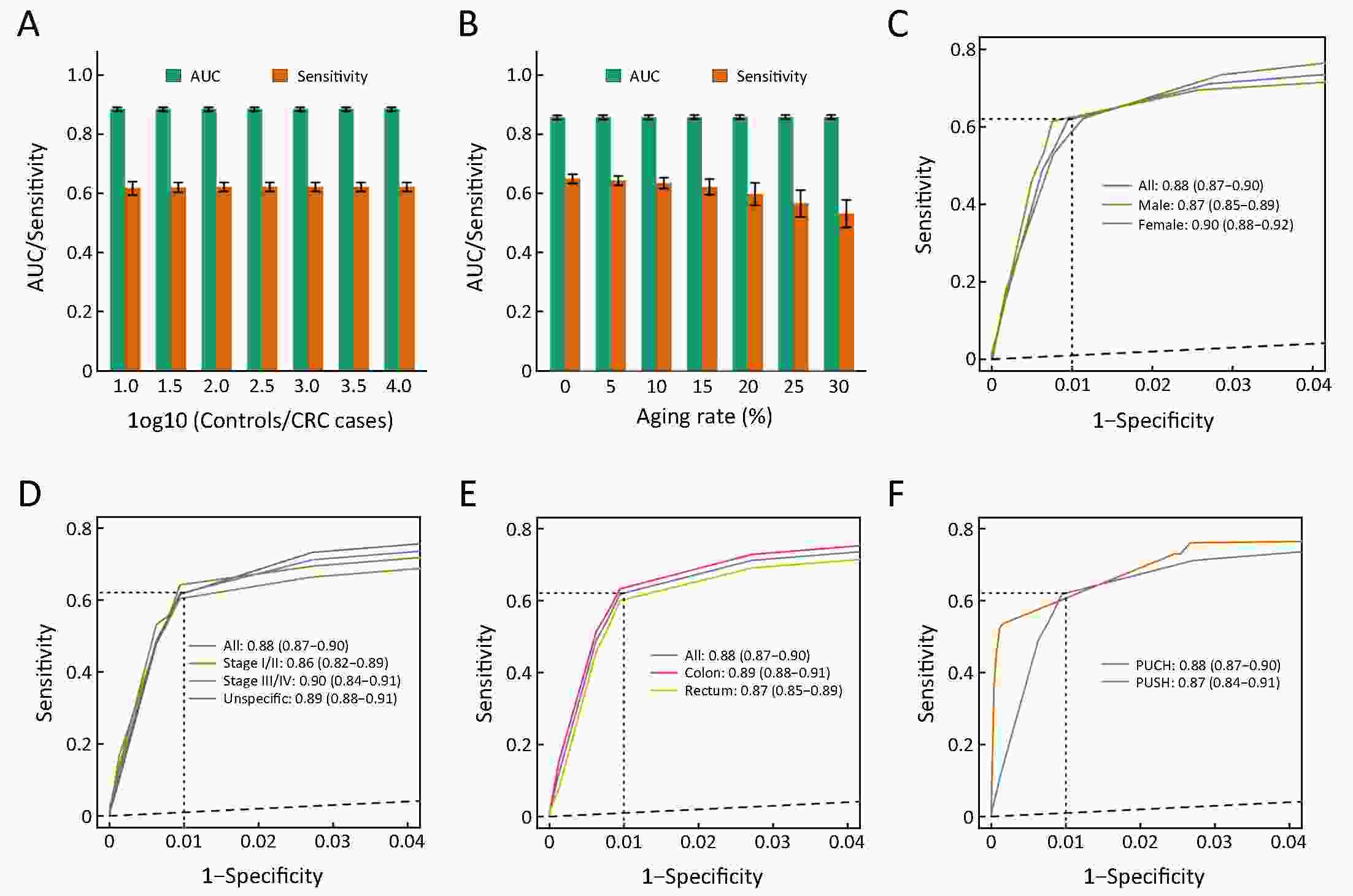
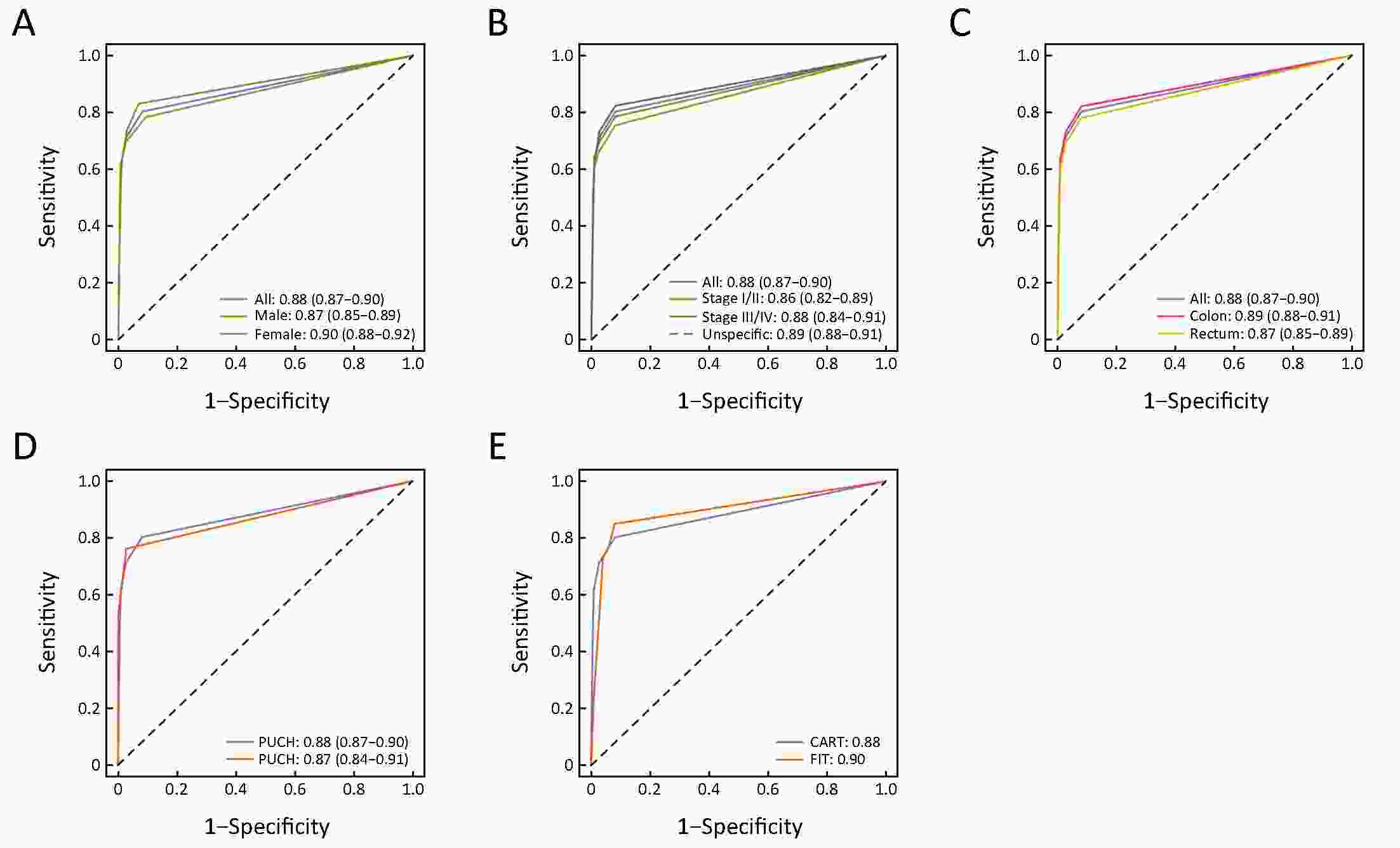
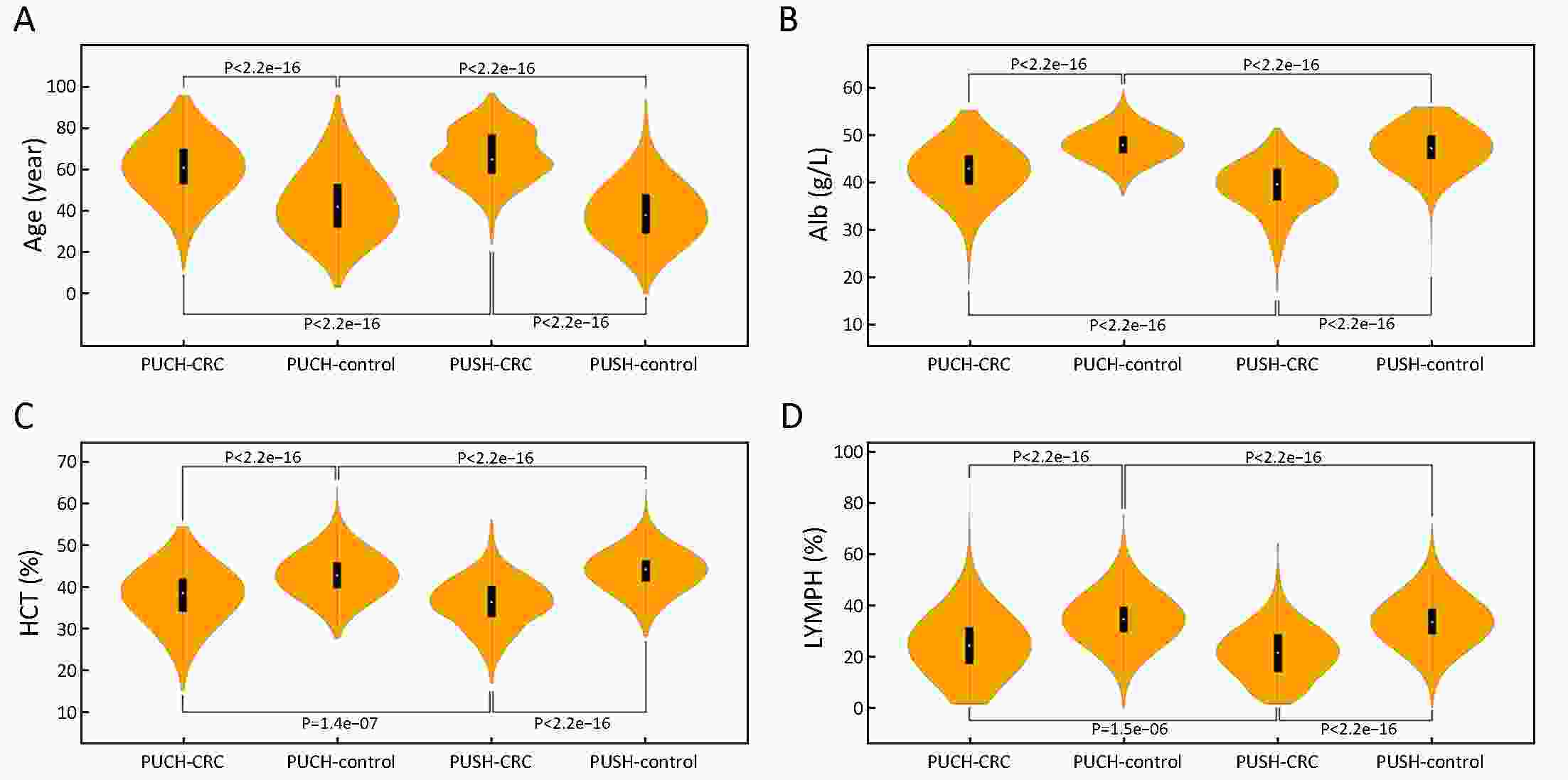
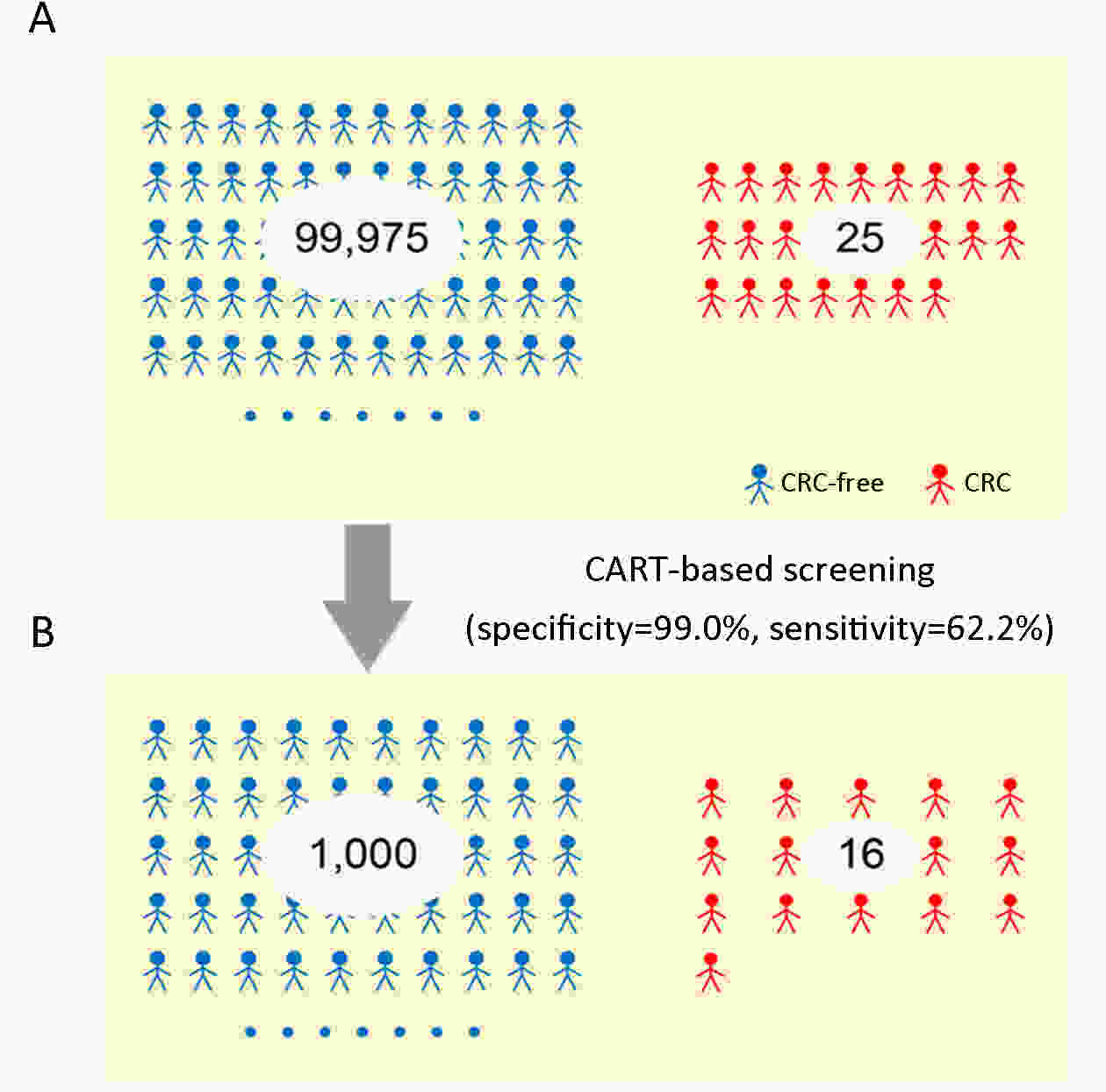
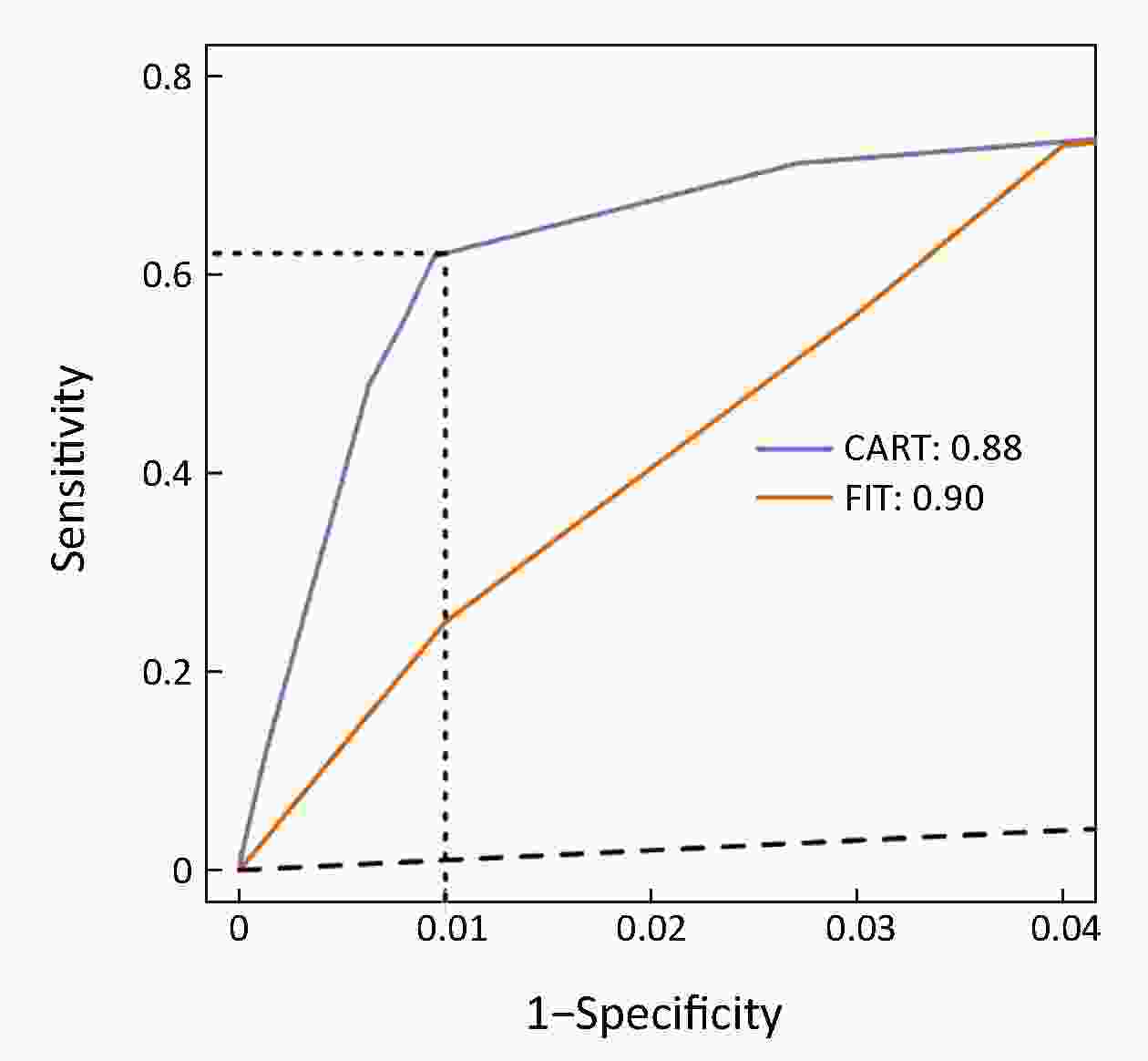
ObjectiveChallenges remain in current practices of colorectal cancer (CRC) screening, such as low compliance, low specificities and expensive cost. This study aimed to identify high-risk groups for CRC from the general population using regular health examination data. MethodsThe study population consist of more than 7,000 CRC cases and more than 140,000 controls. Using regular health examination data, a model detecting CRC cases was derived by the classification and regression trees (CART) algorithm. Receiver operating characteristic (ROC) curve was applied to evaluate the performance of models. The robustness and generalization of the CART model were validated by independent datasets. In addition, the effectiveness of CART-based screening was compared with stool-based screening. ResultsAfter data quality control, 4,647 CRC cases and 133,898 controls free of colorectal neoplasms were used for downstream analysis. The final CART model based on four biomarkers (age, albumin, hematocrit and percent lymphocytes) was constructed. In the test set, the area under ROC curve (AUC) of the CART model was 0.88 [95% confidence interval (95% CI), 0.87−0.90] for detecting CRC. At the cutoff yielding 99.0% specificity, this model’s sensitivity was 62.2% (95% CI, 58.1%−66.2%), thereby achieving a 63-fold enrichment of CRC cases. We validated the robustness of the method across subsets of test set with diverse CRC incidences, aging rates, genders ratio, distributions of tumor stages and locations, and data sources. Importantly, CART-based screening had the higher positive predictive value (1.6%) than fecal immunochemical test (0.3%). ConclusionsAs an alternative approach for the early detection of CRC, this study provides a low-cost method using regular health examination data to identify high-risk individuals for CRC for further examinations. The approach can promote early detection of CRC especially in developing countries such as China, where annual health examination is popular but regular CRC-specific screening is rare.
2019, 31(4): 699-706.
doi: 10.21147/j.issn.1000-9604.2019.04.13
Abstract:
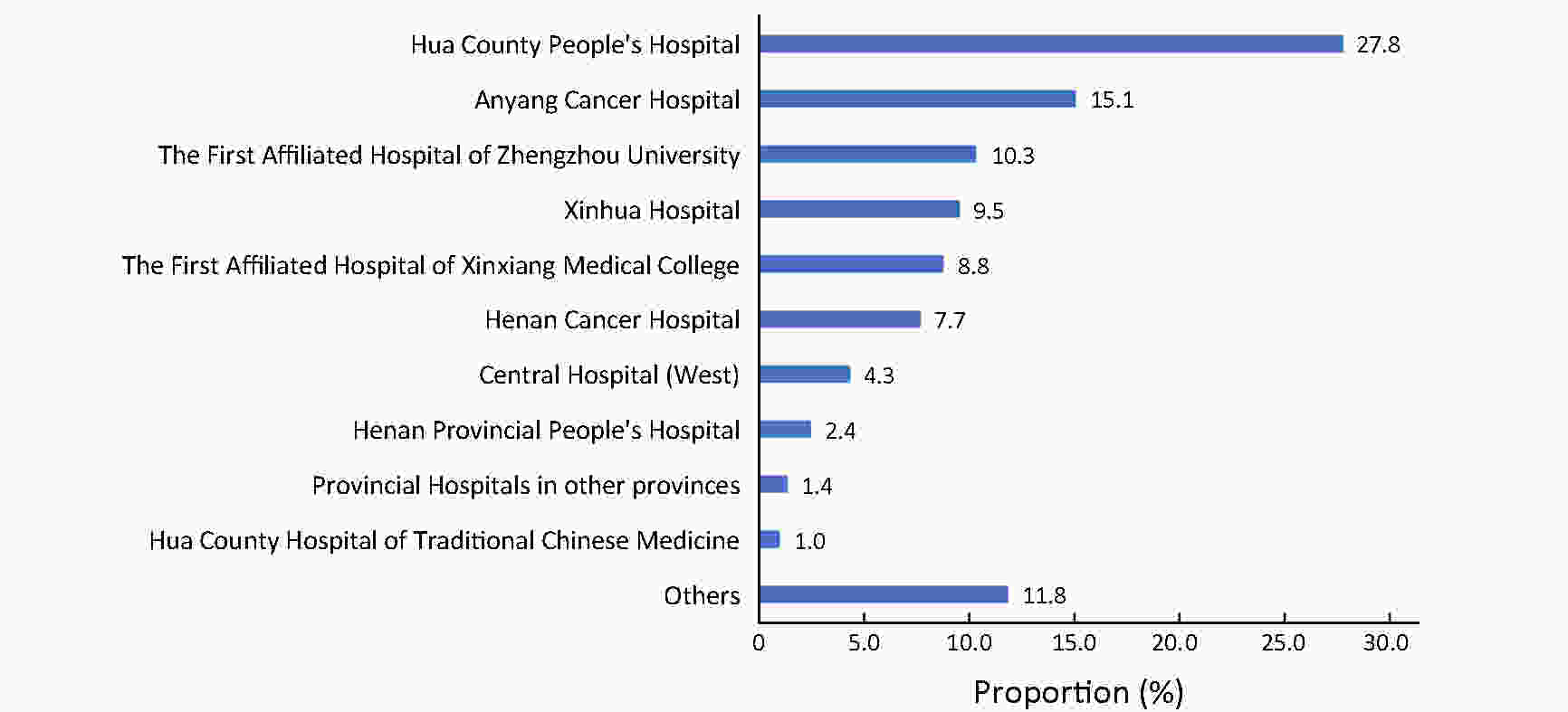
ObjectiveTo evaluate the accuracy of identifying cancer patients by use of medical claims data in a health insurance system in China, and provide the basis for establishing the claims-based cancer surveillance system in China. MethodsWe chose Hua County, Henan Province as the study site, and randomly selected 300 and 1,200 qualified inpatient electronic medical records (EMRs) as well as the New Rural Cooperative Medical Scheme (NCMS) claims records for cancer patients in Hua County People’s Hospital (HCPH) and Anyang Cancer Hospital (ACH) in 2017. Diagnostic information for NCMS claims was evaluated on an individual level, and sensitivity and positive predictive value (PPV) were calculated taking the EMRs as the gold standard. ResultsThe sensitivity of NCMS was 95.2% (93.8%−96.3%) and 92.0% (88.3%−94.8%) in ACH and HCPH, respectively. The PPV of the NCMS was 97.8% (96.7%−98.5%) in ACH and 89.0% (84.9%−92.3%) in HCPH. Overall, the weighted and combined sensitivity and PPV of NCMS in Hua County was 93.1% and 92.1%, respectively. Significantly higher sensitivity and PPV in identifying patients with common cancers than non-common cancers were detected in HCPH and ACH separately (P<0.01). ConclusionsIdentification of cancer patients by use of the NCMS is accurate on individual level, and it is therefore feasible to conduct claims-based cancer surveillance in areas not covered by cancer registries in China.

 Abstract
Abstract FullText HTML
FullText HTML PDF 402KB
PDF 402KB