2019 Vol.31(6)
Display Mode: |
2019, 31(6): 849-852.
doi: 10.21147/j.issn.1000-9604.2019.06.01
Abstract:
The aim of this mini-review is to compare and contrast the pros and cons of short-course and long-course neoadjuvant chemoradiation therapy regimens for stage II & III rectal adenocarcinoma. Multiple trials have demonstrated the equal efficacy and safety of short-course and long-course radiation therapy as a part of neoadjuvant regimens. Published data also shows that total neoadjuvant therapy could be more successful than neoadjuvant chemoradiation followed by adjuvant chemotherapy. This review points out future research directions for patients with locally advanced rectal adenocarcinoma such as comparing total neoadjuvant therapy that contains a short-course of radiation therapy to the standard of care, and evaluating how the sequence of short-course radiation therapy and chemotherapy in the total neoadjuvant therapy impacts the pathological complete response (pCR) rate, local control, and survival outcomes.
The aim of this mini-review is to compare and contrast the pros and cons of short-course and long-course neoadjuvant chemoradiation therapy regimens for stage II & III rectal adenocarcinoma. Multiple trials have demonstrated the equal efficacy and safety of short-course and long-course radiation therapy as a part of neoadjuvant regimens. Published data also shows that total neoadjuvant therapy could be more successful than neoadjuvant chemoradiation followed by adjuvant chemotherapy. This review points out future research directions for patients with locally advanced rectal adenocarcinoma such as comparing total neoadjuvant therapy that contains a short-course of radiation therapy to the standard of care, and evaluating how the sequence of short-course radiation therapy and chemotherapy in the total neoadjuvant therapy impacts the pathological complete response (pCR) rate, local control, and survival outcomes.
2019, 31(6): 853-861.
doi: 10.21147/j.issn.1000-9604.2019.06.02
Abstract:
Immunotherapy is one of the most promising treatments for multiple tumor types. The significant clinical benefits and durable responses of immunotherapy have led to the emergence of various immune-related clinical response patterns that extend beyond those achieved with cytotoxic agents. Various studies investigated the efficacy of immunotherapy, including the effect on tumor size, long-term survival benefits, and the ability to overcome the particularly challenging survival curves tailing phenomenon. The current immune-related methods guidelines, such as immune-related Response Criteria (irRC), immune-related Response Evaluation Criteria in Solid Tumors (irRECIST), immune Response Evaluation Criteria in Solid Tumors (iRECIST), and immune-modified Response Evaluation Criteria in Solid Tumors (imRECIST), could be well-adapted to identify the heterogeneity of responses that appear in patients receiving immunotherapy, such as pseudoprogression (PsPD) and hyperprogressive disease (HPD), and to some extent to overcome the limitation of evaluating the efficacy of immunotherapy on tumor size by imaging. Additionally, a second type of evaluation method was proposed based on survival, which includes milestone analysis and restricted mean survival time. Currently, milestone analysis is a complementary tool to summarize and interpret trial results along with more conventional measures of survival and other less established metrics. A golden standard evaluation method to distinguish the efficacy of immunotherapy may improve the process of imaging and aid survival-based efficacy evaluation in patients with solid tumors.
Immunotherapy is one of the most promising treatments for multiple tumor types. The significant clinical benefits and durable responses of immunotherapy have led to the emergence of various immune-related clinical response patterns that extend beyond those achieved with cytotoxic agents. Various studies investigated the efficacy of immunotherapy, including the effect on tumor size, long-term survival benefits, and the ability to overcome the particularly challenging survival curves tailing phenomenon. The current immune-related methods guidelines, such as immune-related Response Criteria (irRC), immune-related Response Evaluation Criteria in Solid Tumors (irRECIST), immune Response Evaluation Criteria in Solid Tumors (iRECIST), and immune-modified Response Evaluation Criteria in Solid Tumors (imRECIST), could be well-adapted to identify the heterogeneity of responses that appear in patients receiving immunotherapy, such as pseudoprogression (PsPD) and hyperprogressive disease (HPD), and to some extent to overcome the limitation of evaluating the efficacy of immunotherapy on tumor size by imaging. Additionally, a second type of evaluation method was proposed based on survival, which includes milestone analysis and restricted mean survival time. Currently, milestone analysis is a complementary tool to summarize and interpret trial results along with more conventional measures of survival and other less established metrics. A golden standard evaluation method to distinguish the efficacy of immunotherapy may improve the process of imaging and aid survival-based efficacy evaluation in patients with solid tumors.
2019, 31(6): 862-877.
doi: 10.21147/j.issn.1000-9604.2019.06.03
Abstract:
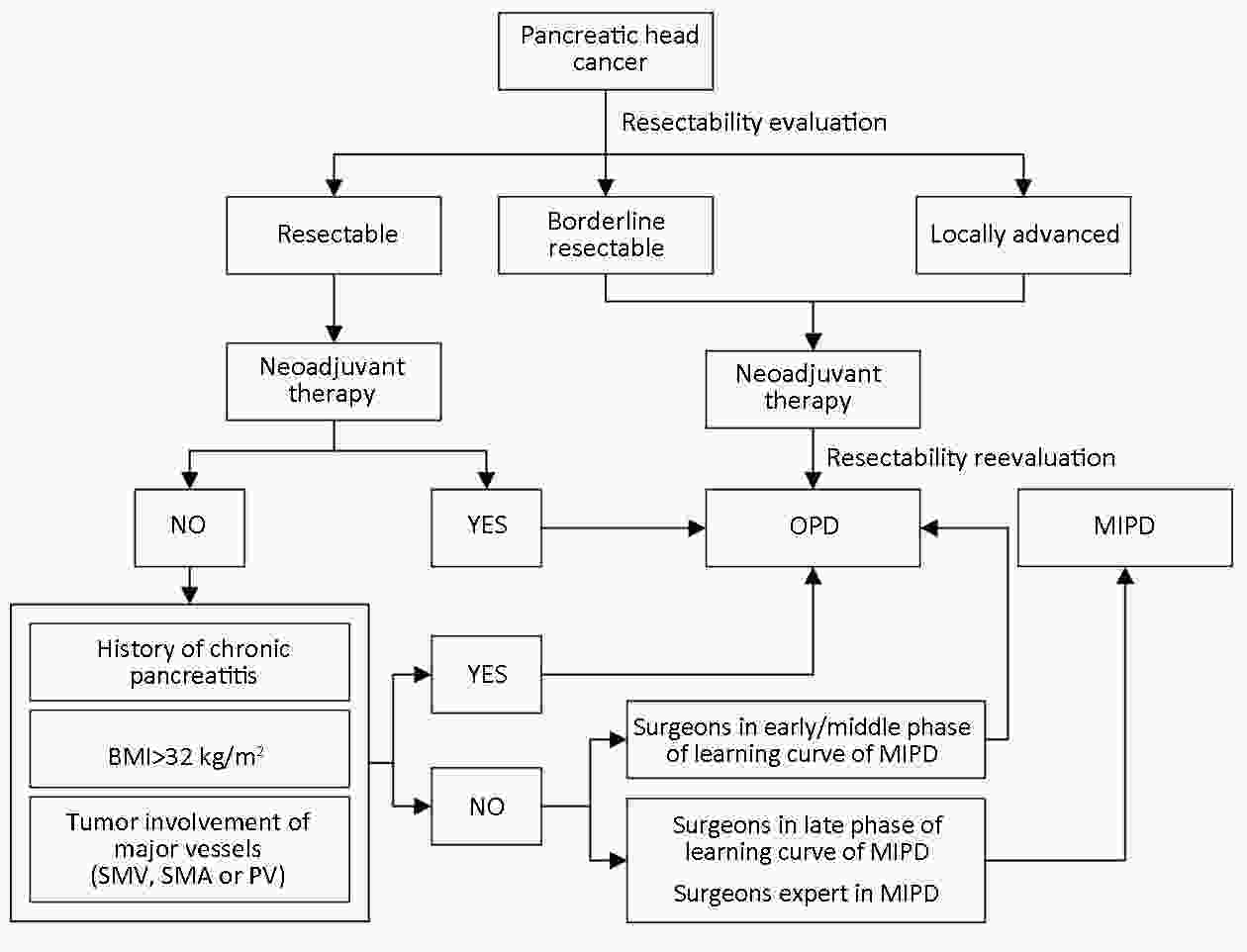
Pancreatic head cancer still represents an insurmountable barrier for patients and pancreatic surgeons. Pancreaticoduodenectomy (PD) continues to be the operative standard of care and potentially curative procedure for pancreatic head cancer. Despite the rapid development of minimally invasive techniques, whether the efficacy of minimally invasive pancreaticoduodenectomy (MIPD) is noninferior or superior to open pancreaticoduodenectomy (OPD) remains unclear. In this review, we summarized the history of OPD and MIPD and the latest staging and classification information for pancreatic head cancer as well as the proposed recommendations for MIPD indications for patients with pancreatic head cancer. By reviewing the MIPD- vs. OPD-related literature, we found that MIPD shows noninferiority or superiority to OPD in terms of safety, feasibility, enhanced recovery after surgery (ERAS) and several short-term and long-term outcomes. In addition, we analyzed and summarized the different MIPD outcomes in the USA, Europe and China. Certain debates over MIPD have continued, however, selection bias, the large number of low-volume centers, the steep MIPD learning curve, high conversion rate and administration of neoadjuvant therapy may limit the application of MIPD for pancreatic head cancer.
Pancreatic head cancer still represents an insurmountable barrier for patients and pancreatic surgeons. Pancreaticoduodenectomy (PD) continues to be the operative standard of care and potentially curative procedure for pancreatic head cancer. Despite the rapid development of minimally invasive techniques, whether the efficacy of minimally invasive pancreaticoduodenectomy (MIPD) is noninferior or superior to open pancreaticoduodenectomy (OPD) remains unclear. In this review, we summarized the history of OPD and MIPD and the latest staging and classification information for pancreatic head cancer as well as the proposed recommendations for MIPD indications for patients with pancreatic head cancer. By reviewing the MIPD- vs. OPD-related literature, we found that MIPD shows noninferiority or superiority to OPD in terms of safety, feasibility, enhanced recovery after surgery (ERAS) and several short-term and long-term outcomes. In addition, we analyzed and summarized the different MIPD outcomes in the USA, Europe and China. Certain debates over MIPD have continued, however, selection bias, the large number of low-volume centers, the steep MIPD learning curve, high conversion rate and administration of neoadjuvant therapy may limit the application of MIPD for pancreatic head cancer.
2019, 31(6): 878-891.
doi: 10.21147/j.issn.1000-9604.2019.06.04
Abstract:
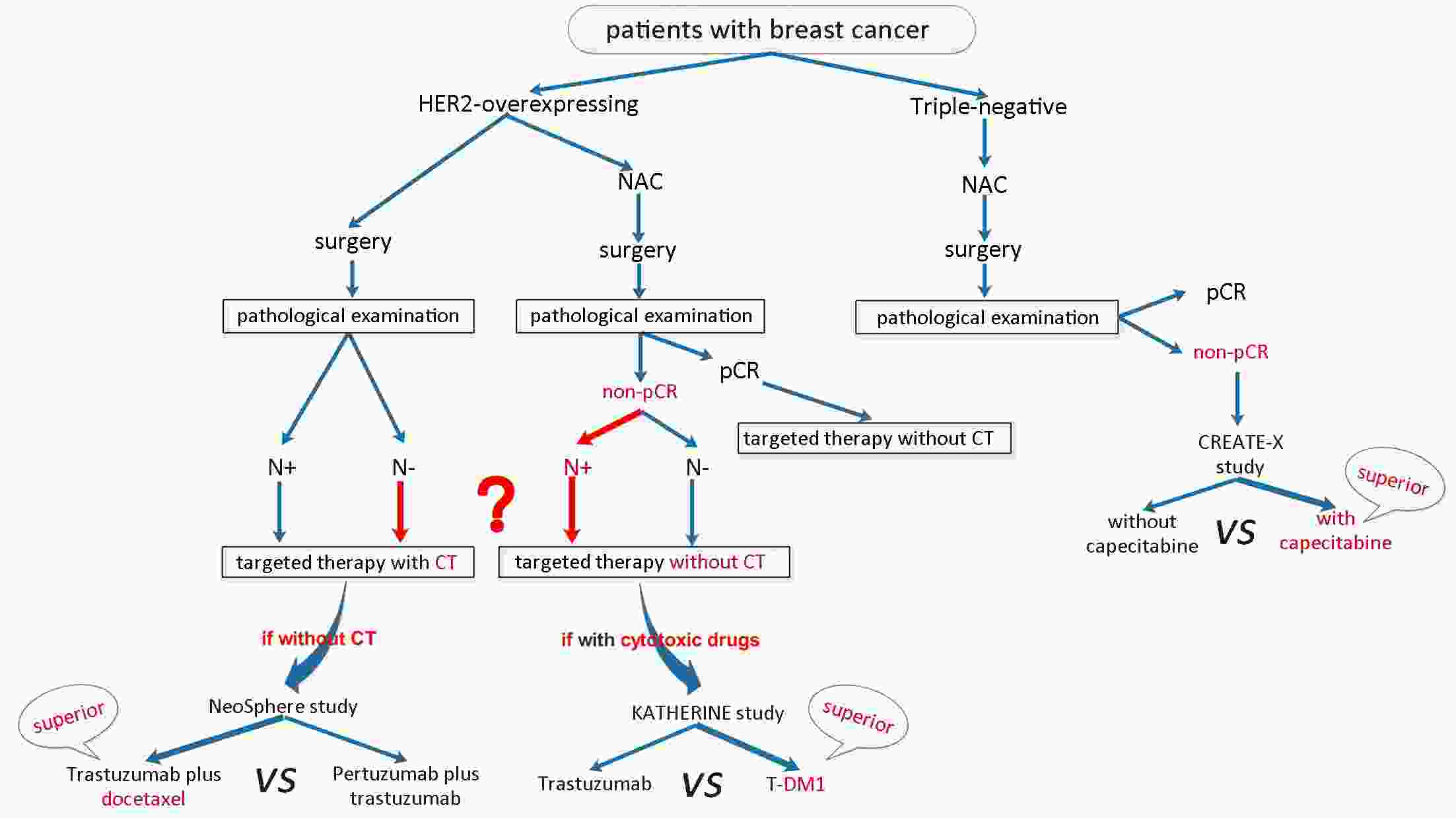
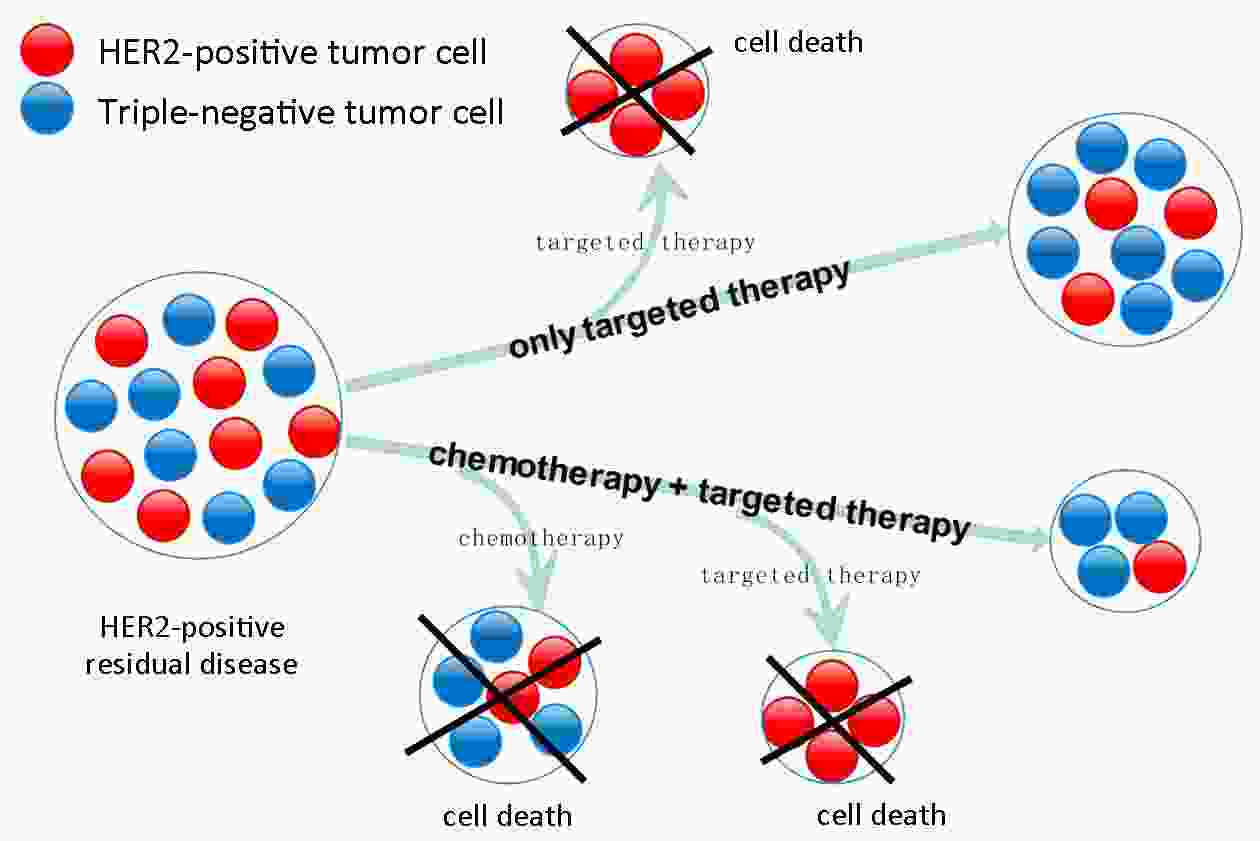
Human epidermal growth factor receptor 2 (HER2)-overexpressing breast cancer is an aggressive phenotype with a poor prognosis, and can easily metastasize and recur. Currently, chemotherapy plus HER2-targeted therapy is the standard systemic treatment for most of these patients. Given that neoadjuvant chemotherapy (NAC) has an efficacy equivalent to that of adjuvant chemotherapy and some additional benefits, many patients, especially those with more advanced tumors, prefer NAC and generally will not receive additional chemotherapy after surgery, irrespective of the pathological response. However, achieving pathological complete response to NAC is strongly correlated with prognosis, especially in triple-negative and HER2-overexpressing breast cancer. Therefore, postoperative treatment of these patients with residual diseases should be optimized to achieve favorable outcomes. The CREATE-X study has confirmed that additional chemotherapy can improve the outcomes of patients with HER2-negative residual disease after NAC. In addition, chemotherapy plays an indispensable role in the treatment of patients who receive surgery directly or who have recurrent lesions. Therefore, can additional chemotherapy improve prognosis of patients with HER2-overexpressing residual breast cancer? At present, no studies have compared the efficacy of additional chemotherapy plus trastuzumab with that of anti-HER2 therapy alone in residual cancer. The KATHERINE study revealed that trastuzumab emtansine (T-DM1) can reduce the risk of recurrence or death by 50% compared with trastuzumab in patients with HER2-positive residual invasive breast cancer after neoadjuvant therapy. T-DM1 is an antibody-drug conjugate of trastuzumab and the cytotoxic agent emtansine, and thus, to an extent, T-DM1 is equivalent to simultaneous application of chemotherapy and targeted therapy. However, high cost and low accessibility limit its use especially in low- and middle-income countries and regions. Hence, we proposed this perspective that additional chemotherapy plus trastuzumab should be given to HER2-overexpressing breast cancer patients with residual disease after NAC to improve their prognosis by discussing that the efficacy of additional chemotherapy plus trastuzumab is superior to that of anti-HER2 therapy alone and not inferior to T-DM1. Additional chemotherapy plus trastuzumab-based HER2-targeted therapy can be used as an alternative regimen to T-DM1 when T-DM1 is unavailable. However, further clinical research on the selection of chemotherapeutic agents is warranted.
2019, 31(6): 892-900.
doi: 10.21147/j.issn.1000-9604.2019.06.05
Abstract:
Postoperative adjuvant chemotherapy (ACT) confers superior gastric cancer (GC) survival in the Eastern cohort. However, is the current standard of ACT already excessive, or is it still necessary to increase its intensity for specific subgroups? Tailored ACT strategies for GC depend on gradual exploration by clinical trials in selected patients. Thus, understanding the implications of previous and current research can help us respond wisely and design effective, rational trials, save medical resources and make better decisions in clinical practice. After reviewing and analyzing studies on ACT for GC patients undergoing curative resection, we found that research strategies for conducting “addition” ACT for specific stages of the disease have achieved great progress in making ACT more tailored and personalized in consideration of pathology stages. Furthermore, trials indicate that “addition” ACT strategies for GC patient subgroups based on histological characteristics might be helpful to move toward a more specific tailored and personalized management approach. Designing ACT research focused on different node statuses should also be conducted according to the biological specificity of lymph node (LN) metastasis. Therefore, future trials designed to determine tailored treatment based on histological and biological characteristics for specific subgroups are urgently needed and conducted as the theme of the 2019 American Society of Clinical Oncology (ASCO): Caring for Every Patient, Learning from Every Patient.
Postoperative adjuvant chemotherapy (ACT) confers superior gastric cancer (GC) survival in the Eastern cohort. However, is the current standard of ACT already excessive, or is it still necessary to increase its intensity for specific subgroups? Tailored ACT strategies for GC depend on gradual exploration by clinical trials in selected patients. Thus, understanding the implications of previous and current research can help us respond wisely and design effective, rational trials, save medical resources and make better decisions in clinical practice. After reviewing and analyzing studies on ACT for GC patients undergoing curative resection, we found that research strategies for conducting “addition” ACT for specific stages of the disease have achieved great progress in making ACT more tailored and personalized in consideration of pathology stages. Furthermore, trials indicate that “addition” ACT strategies for GC patient subgroups based on histological characteristics might be helpful to move toward a more specific tailored and personalized management approach. Designing ACT research focused on different node statuses should also be conducted according to the biological specificity of lymph node (LN) metastasis. Therefore, future trials designed to determine tailored treatment based on histological and biological characteristics for specific subgroups are urgently needed and conducted as the theme of the 2019 American Society of Clinical Oncology (ASCO): Caring for Every Patient, Learning from Every Patient.
2019, 31(6): 901-909.
doi: 10.21147/j.issn.1000-9604.2019.06.06
Abstract:
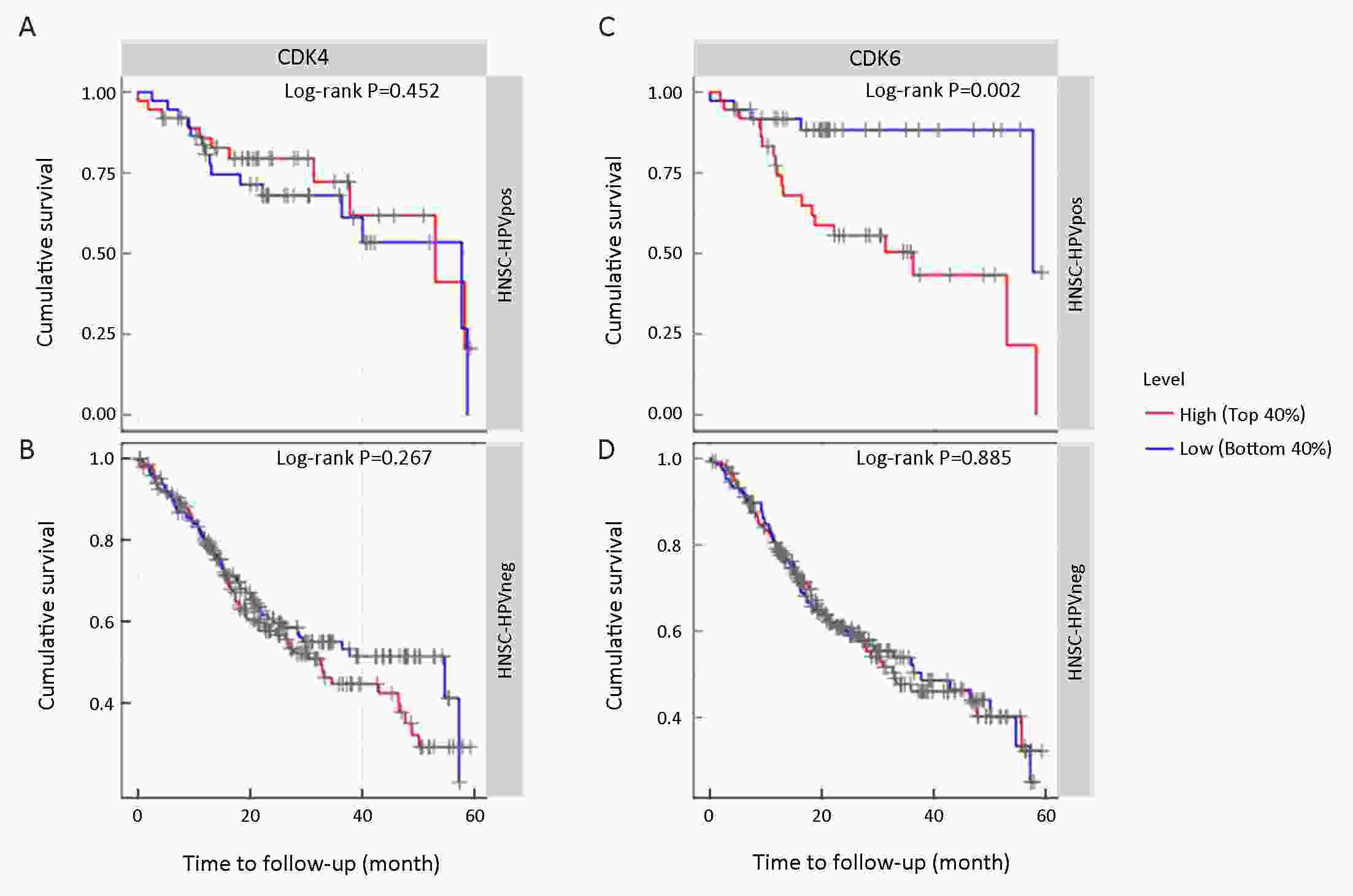
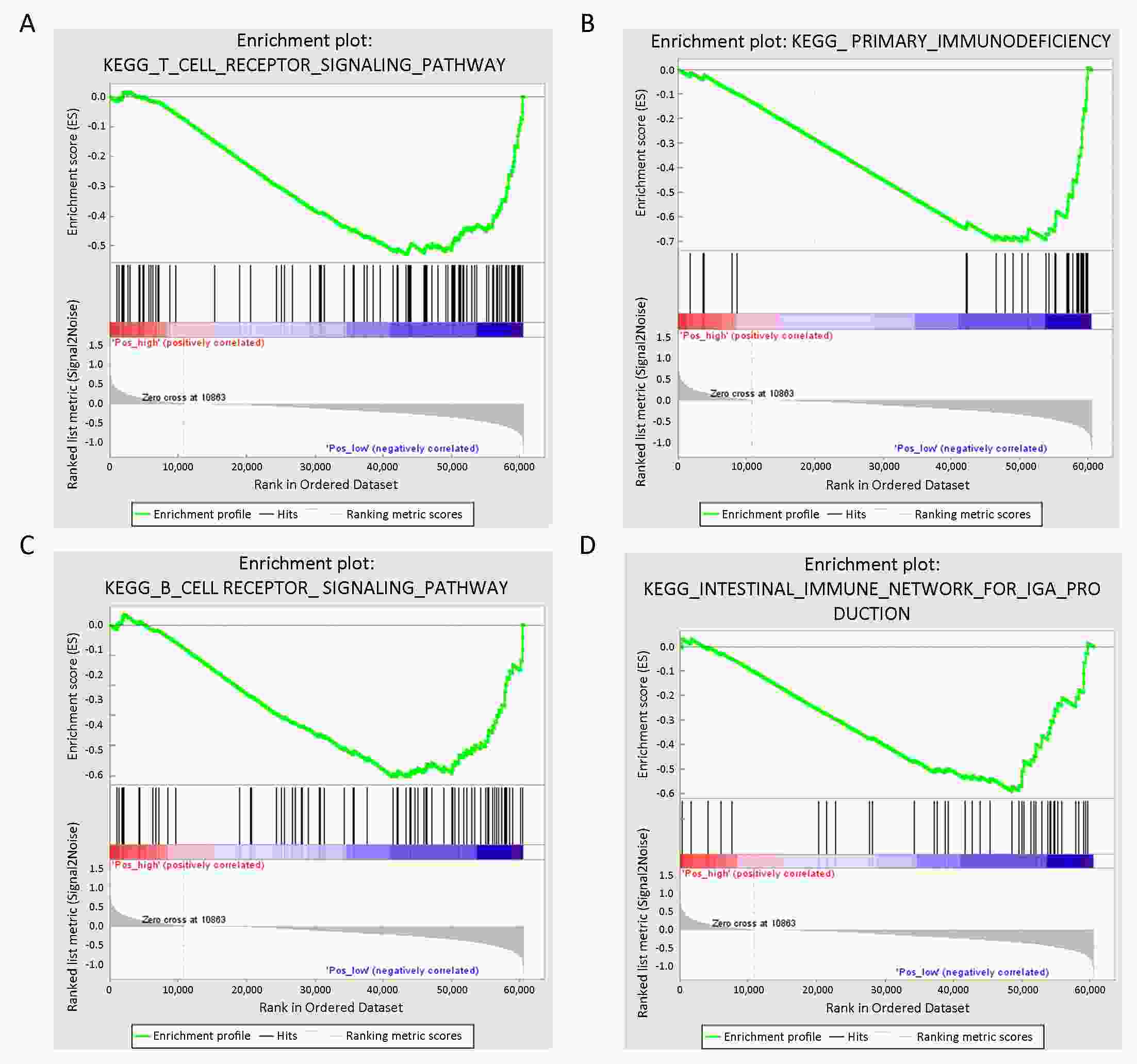
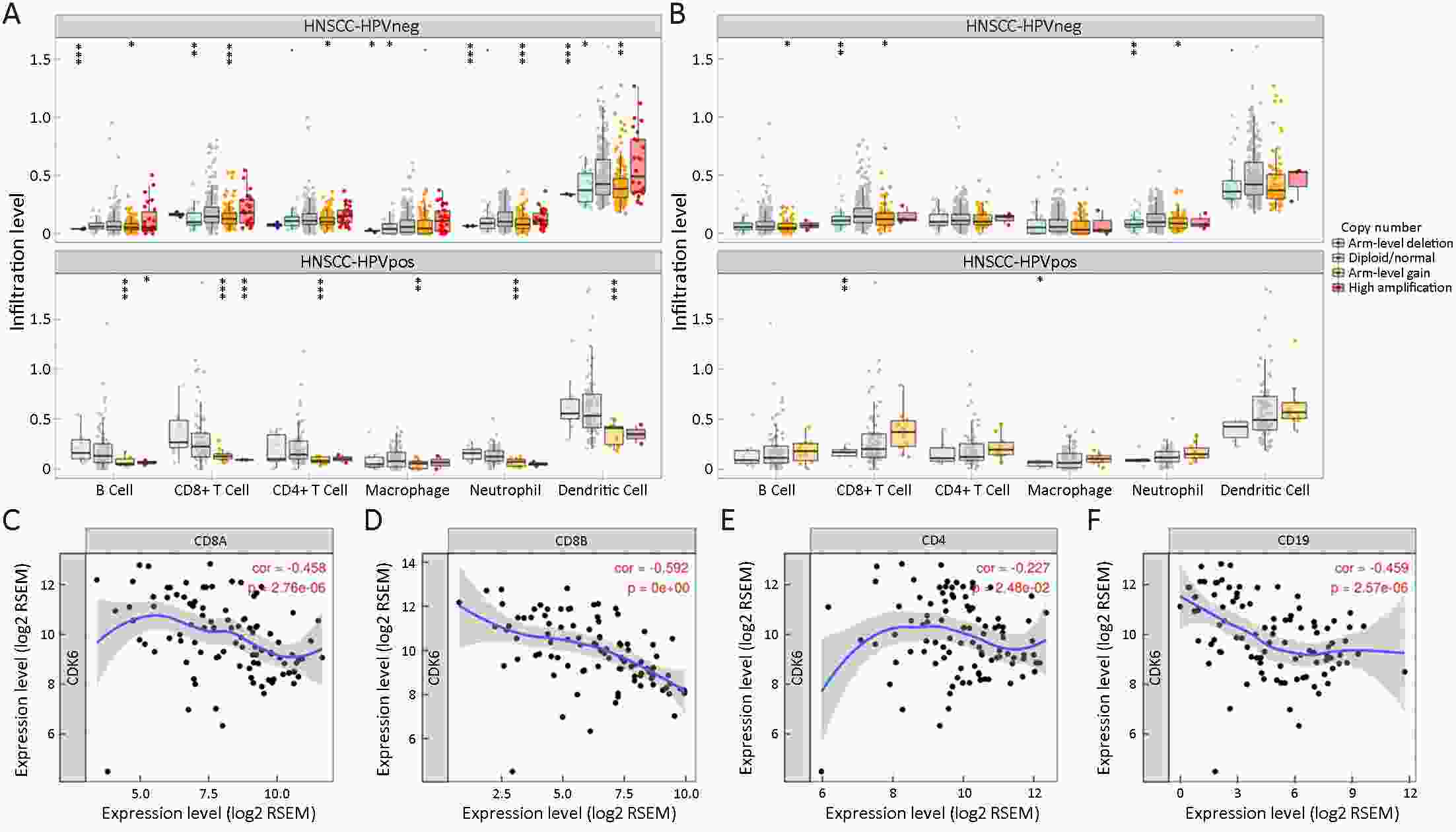
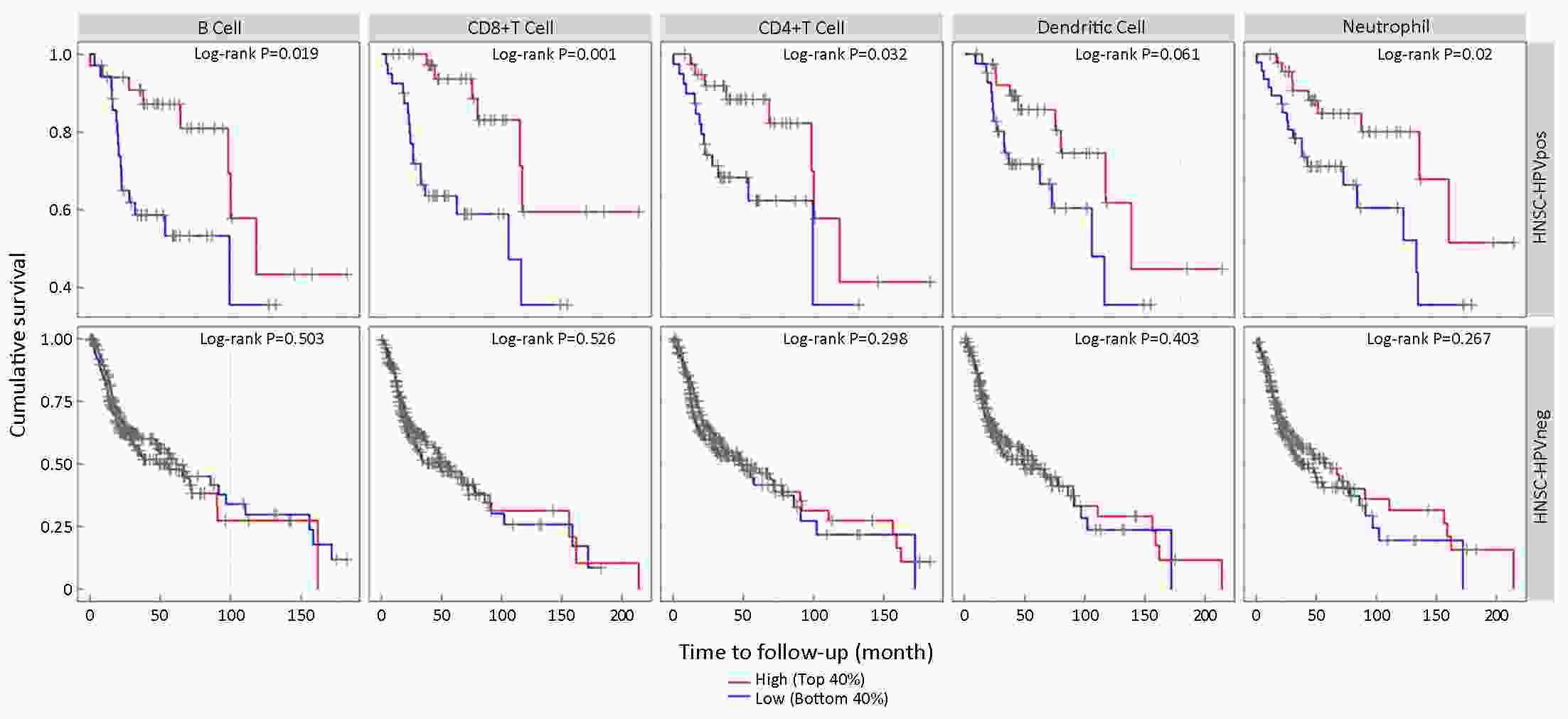
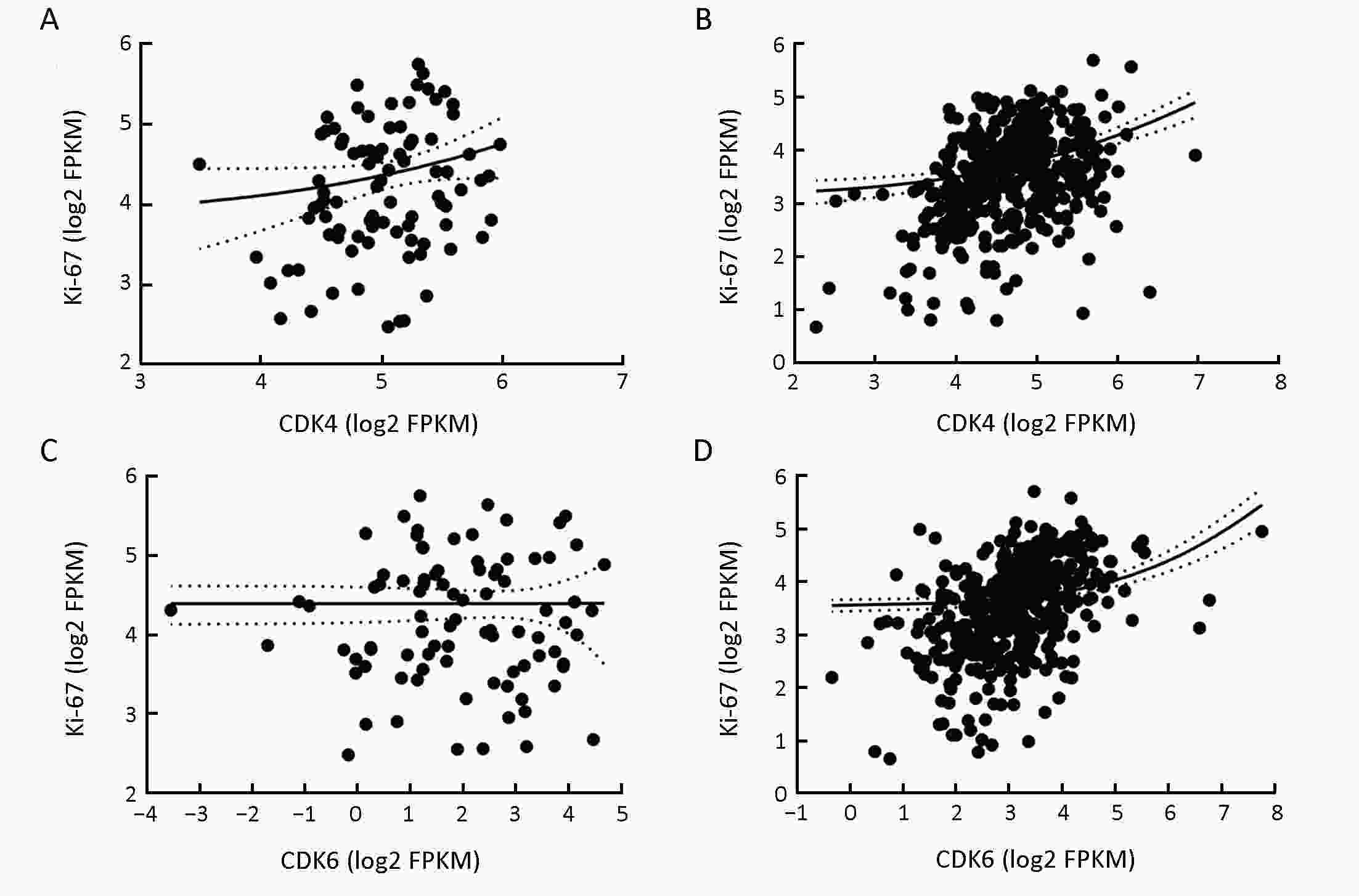
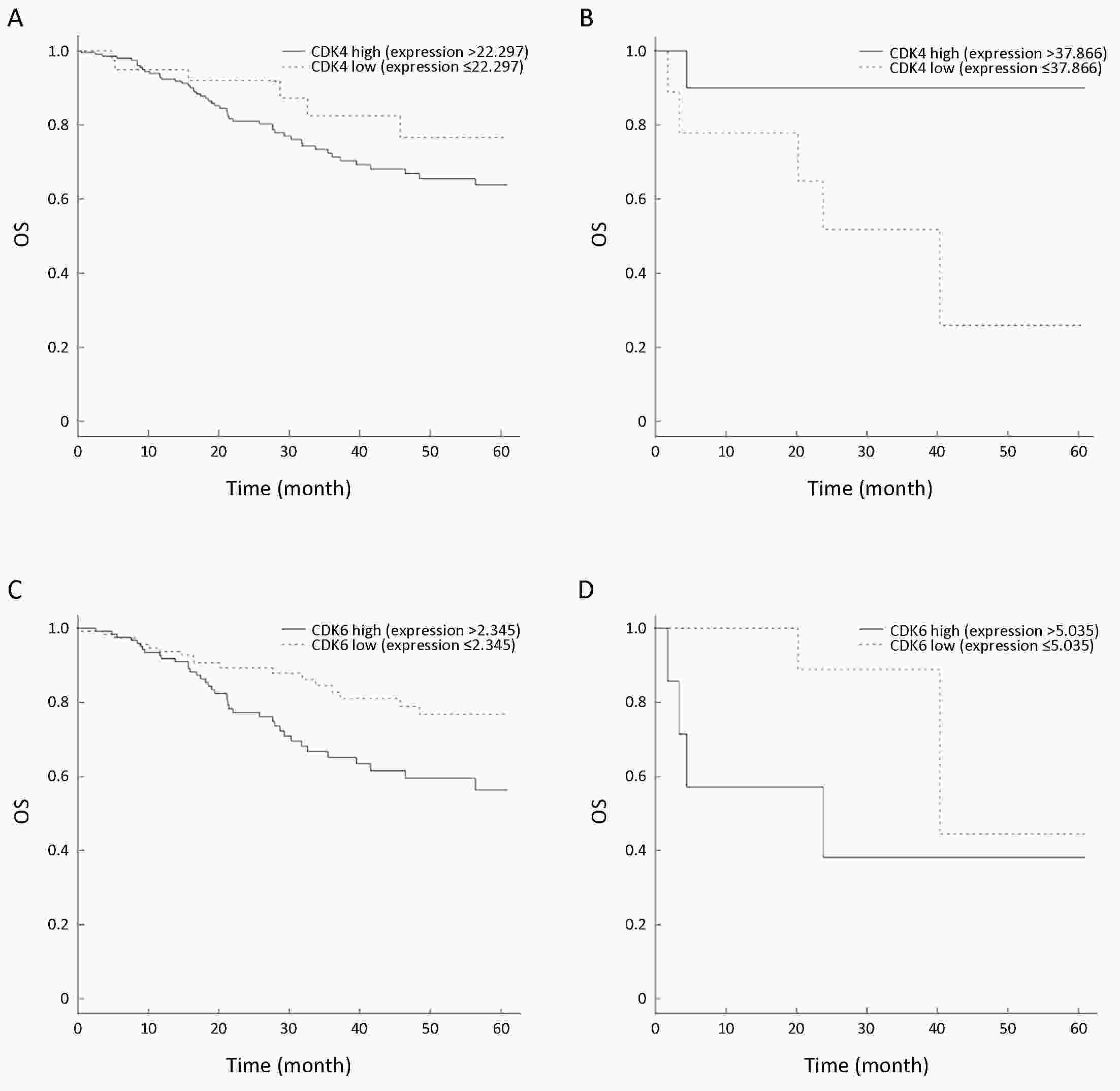
ObjectiveWe investigated the correlations between cyclin-dependent kinase 4/6 (CDK4/6) levels and human papillomavirus (HPV) infection state in head and neck squamous cell cancer (HNSCC). The aim was to explore the potential value of CDK4/6 inhibitors in the treatment of HNSCC. MethodsMultiomic sequencing data for HNSCC were obtained from The Cancer Genome Atlas (TCGA), and the mRNA levels and copy number variations (CNVs) of CDK4 and CDK6 were strictly analyzed. Overall survival (OS) curves were produced using the Kaplan-Meier method, and survival differences between groups were assessed by the log-rank test. Next, gene set enrichment analysis (GSEA) was applied to interrogate CDK4/6-associated molecular pathways in HPV-positive (HPV+) and HPV-negative (HPV−) HNSCC. Last, lymphoid cell infiltrates in each type of HNSCC were explored, and the correlations between CDK4/6 expression and lymphoid infiltrates were explored by Tumor Immune Estimation Resource (TIMER) analysis. ResultsOverexpression of either CDK6 or CDK4 was not a relevant factor for OS in HPV− HNSCC (CDK6: top 40% vs. bottom 40%, P=0.885; CDK4: top 40% vs. bottom 40%, P=0.267). In HPV+ HNSCC, CDK6 but not CDK4 was a relevant factor for OS (CDK6: top 40% vs. bottom 40%, P=0.002; CDK4: top 40% vs. bottom 40%, P=0.452). GSEA found that overexpressed CDK6 in HPV+ HNSCC inhibited pathways involved in the tumor immune response, suggesting its roles in antitumor immunity. TIMER analysis results revealed that CDK6 but not CDK4 accumulation was negatively correlated with the number of tumor-infiltrating lymphocytes specific for HPV+ HNSCC, which led to tumor response suppression. ConclusionsCDK6, but not CDK4, is a poor prognostic marker specific in HPV+ HNSCC patients. Overexpressed CDK6 might stimulate tumor progression by suppressing lymphocytes infiltration independent of its kinase activity. Only abrogating its kinase activity using current CDK4/6 inhibitors was not enough to block its tumor promotion function.
2019, 31(6): 910-917.
doi: 10.21147/j.issn.1000-9604.2019.06.07
Abstract:
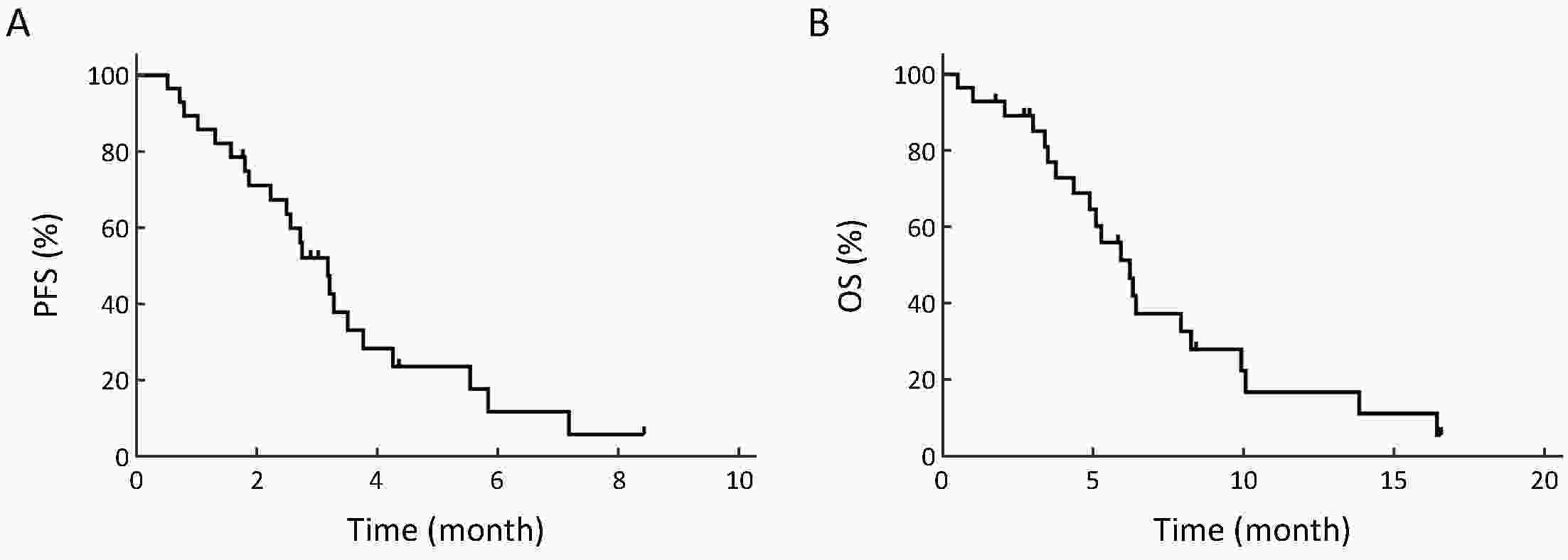
ObjectiveSeveral anti-programmed cell death 1 (anti-PD-1) antibodies have demonstrated potential efficacy in the treatment of advanced esophageal squamous cell cancer (ESCC). However, the response to subsequent chemotherapy after the failure of PD-1 blockade in ESCC patients has not been reported, and the optimal sequencing of immunotherapy and chemotherapy remains controversial. The aim of the present study was to evaluate responses to irinotecan-based subsequent chemotherapy in advanced ESCC patients who had progressed after treatment with camrelizumab (SHR-1210), a novel anti-PD-1 antibody. MethodsWe retrospectively reviewed the medical records of patients with advanced ESCC treated with camrelizumab at a single institution. Consecutive patients who received subsequent irinotecan-based chemotherapy were selected for data collection and analysis. ResultsOverall, a total of 28 patients were included. All patients had received at least two lines of systemic treatment prior to irinotecan salvage. The most common regimen that was administered after PD-1 blockade was irinotecan in combination with 5-fluorouracil (5-Fu) (or its derivatives), which was given to 19 patients. The objective response rate (ORR) and disease control rate (DCR) were 17.9% (5/28) and 64.3% (18/28), respectively, with 5 (17.9%) patients achieving a partial response and 13 (46.4%) having stable disease. The median progression-free survival (PFS) was 3.18 [95% confidence interval (95% CI), 2.48−3.88] months and the median overall survival (OS) was 6.23 (95% CI, 4.71−7.75) months. No new safety issues, either immune-related or otherwise, were observed. ConclusionsOur results suggested that the response to irinotecan-based chemotherapy after PD-1 blockade in advanced ESCC patients appeared similar to that previously observed in patients who had not received PD-1 antibodies, and further study in larger cohorts or randomized trials is warranted to verify our observation.
2019, 31(6): 918-929.
doi: 10.21147/j.issn.1000-9604.2019.06.08
Abstract:
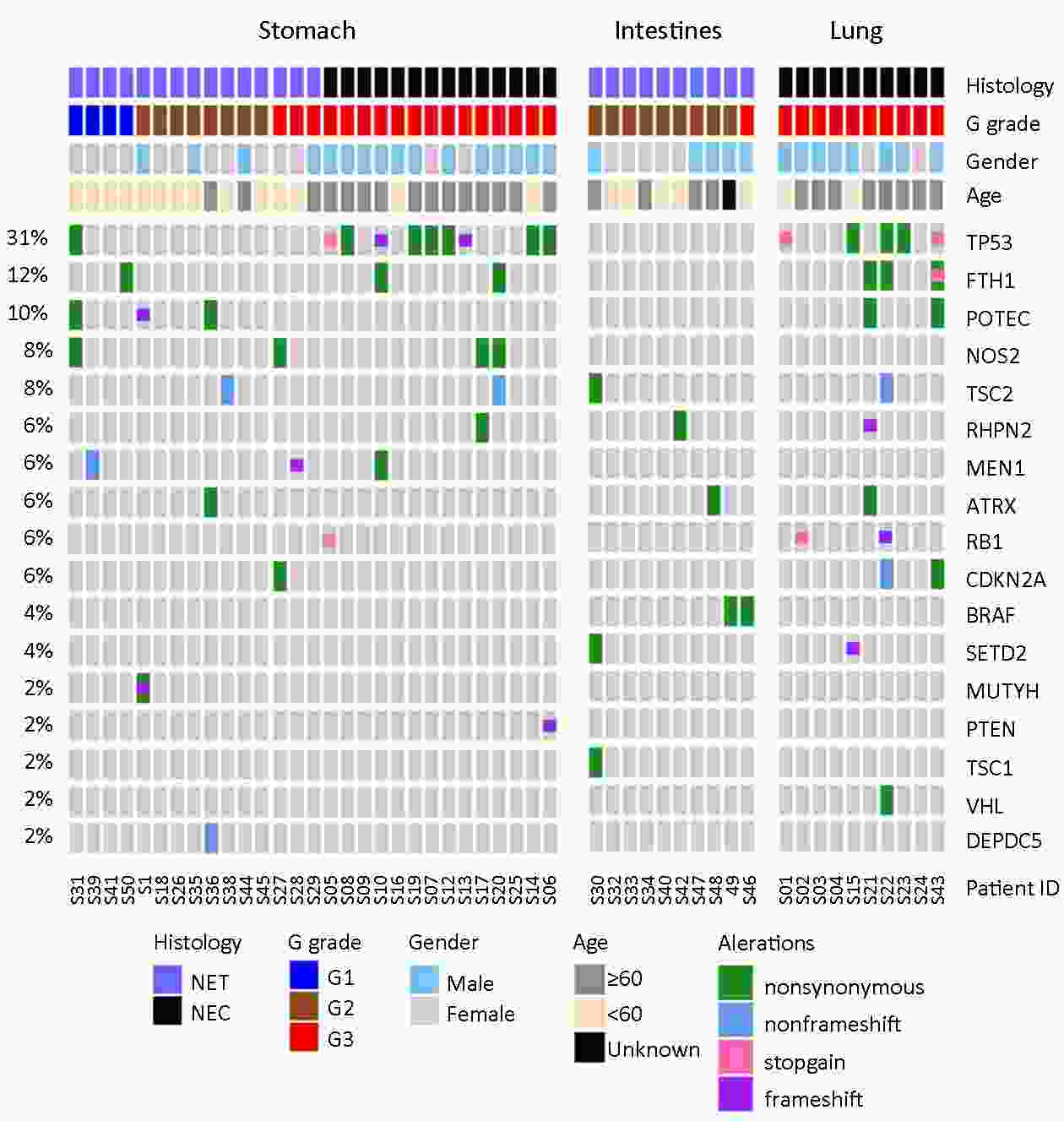
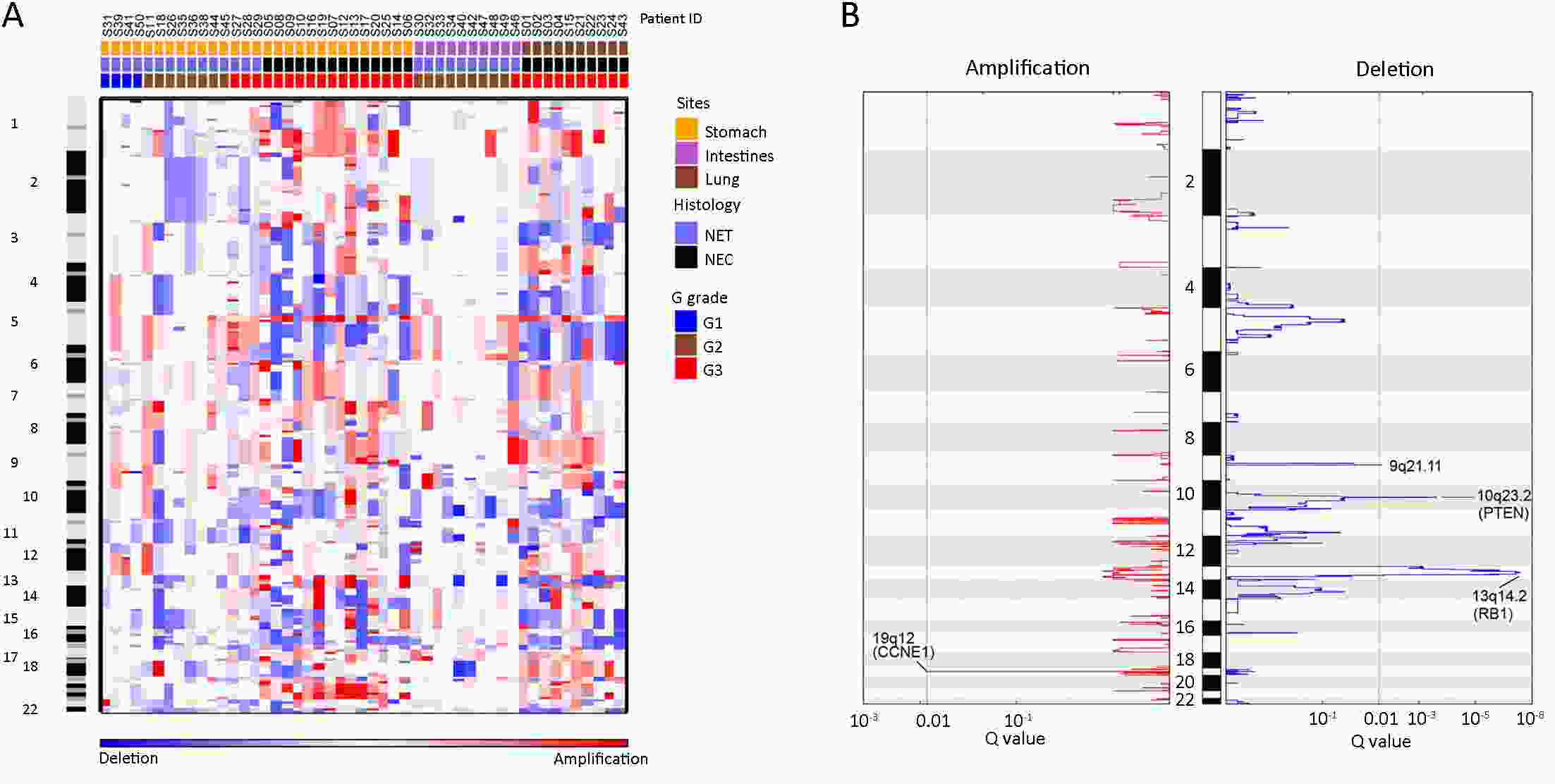
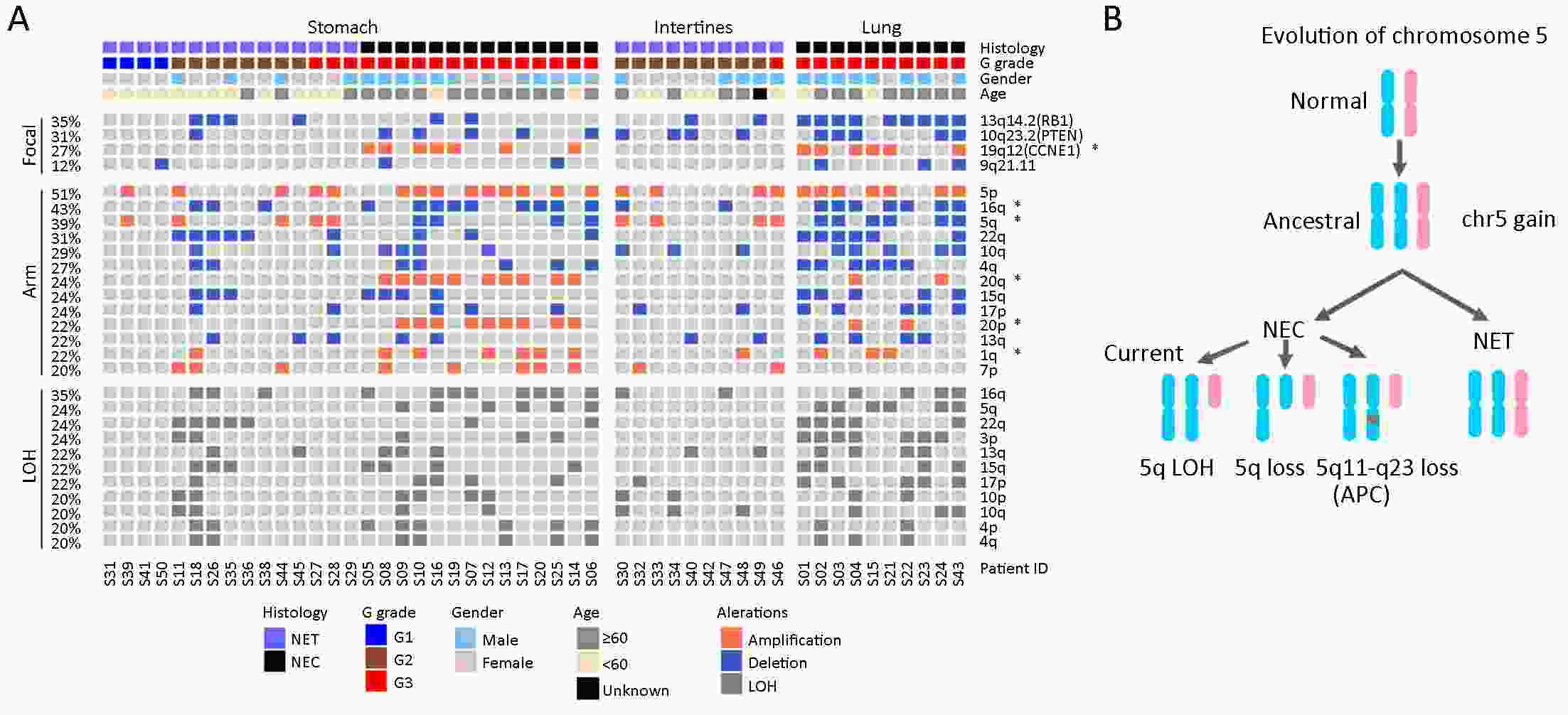
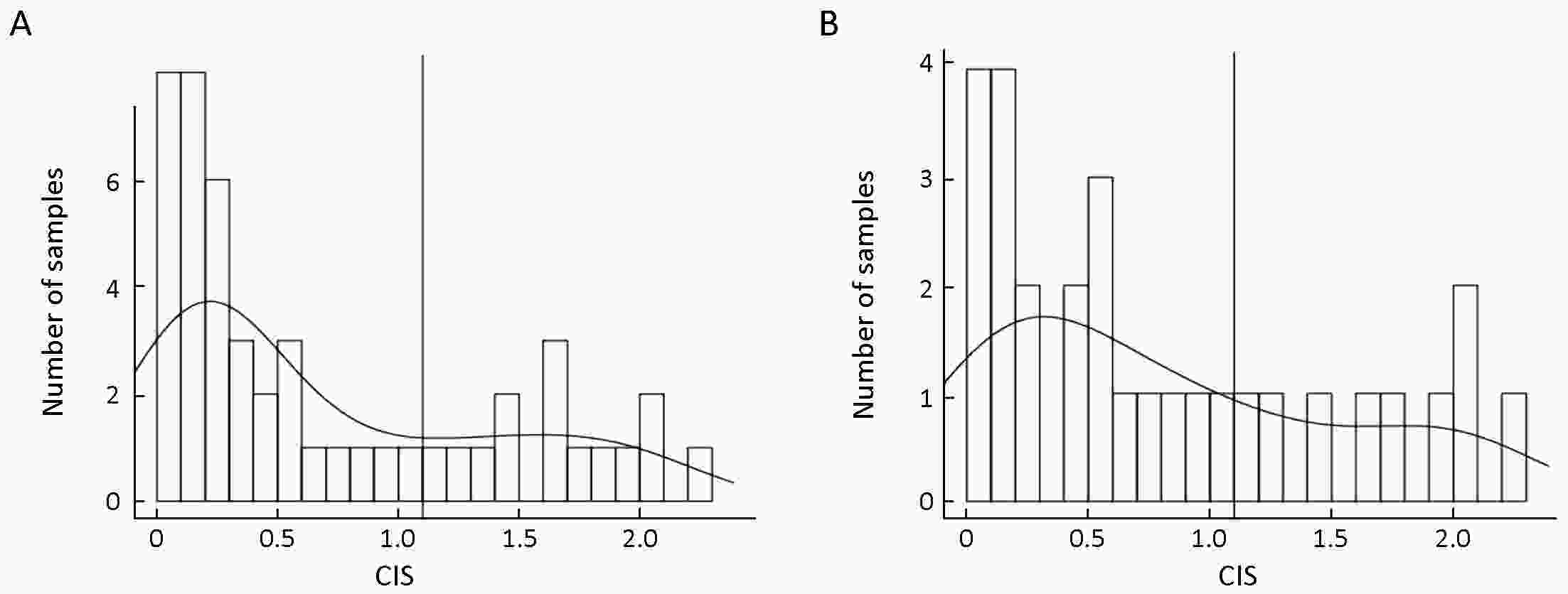
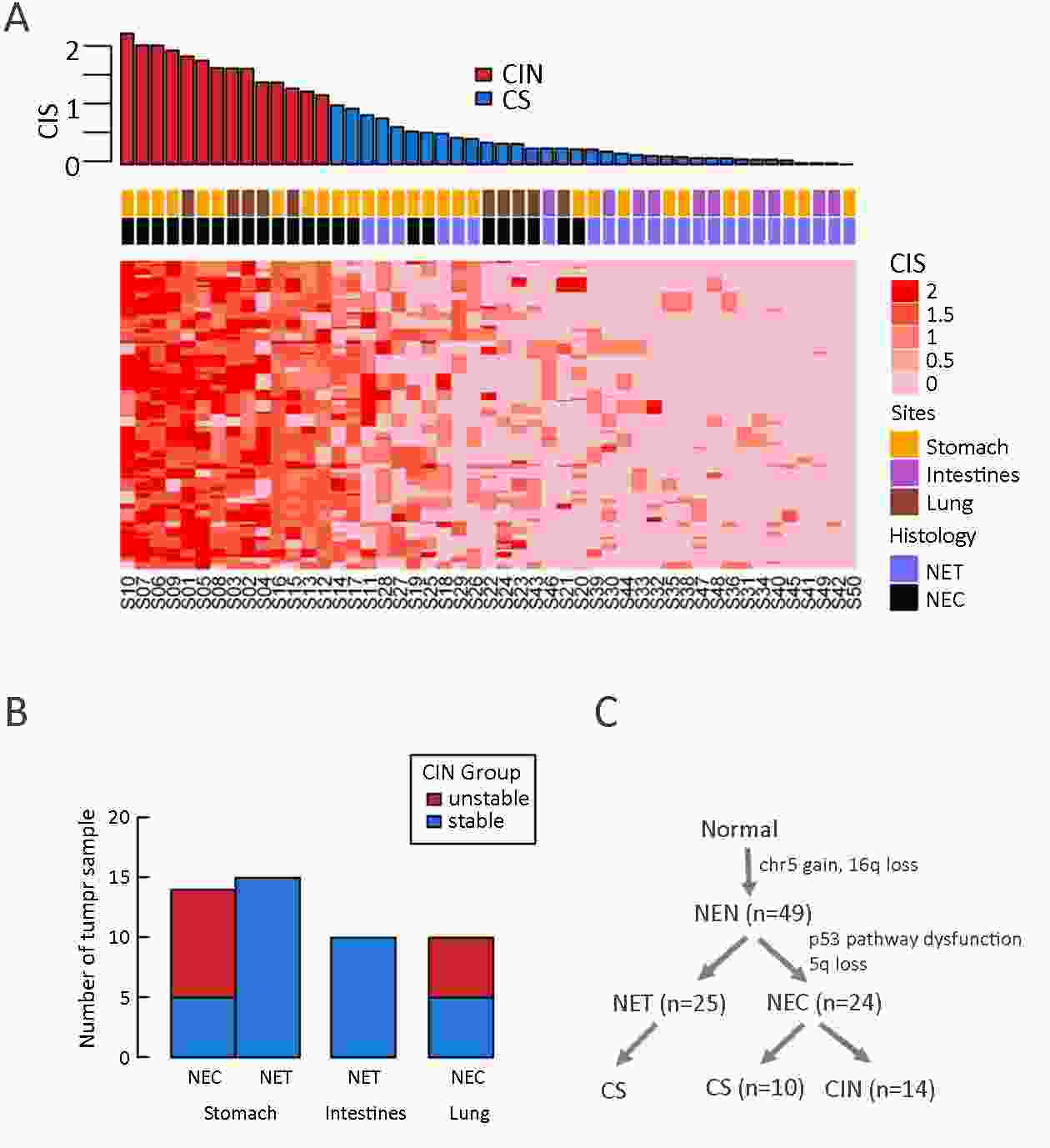
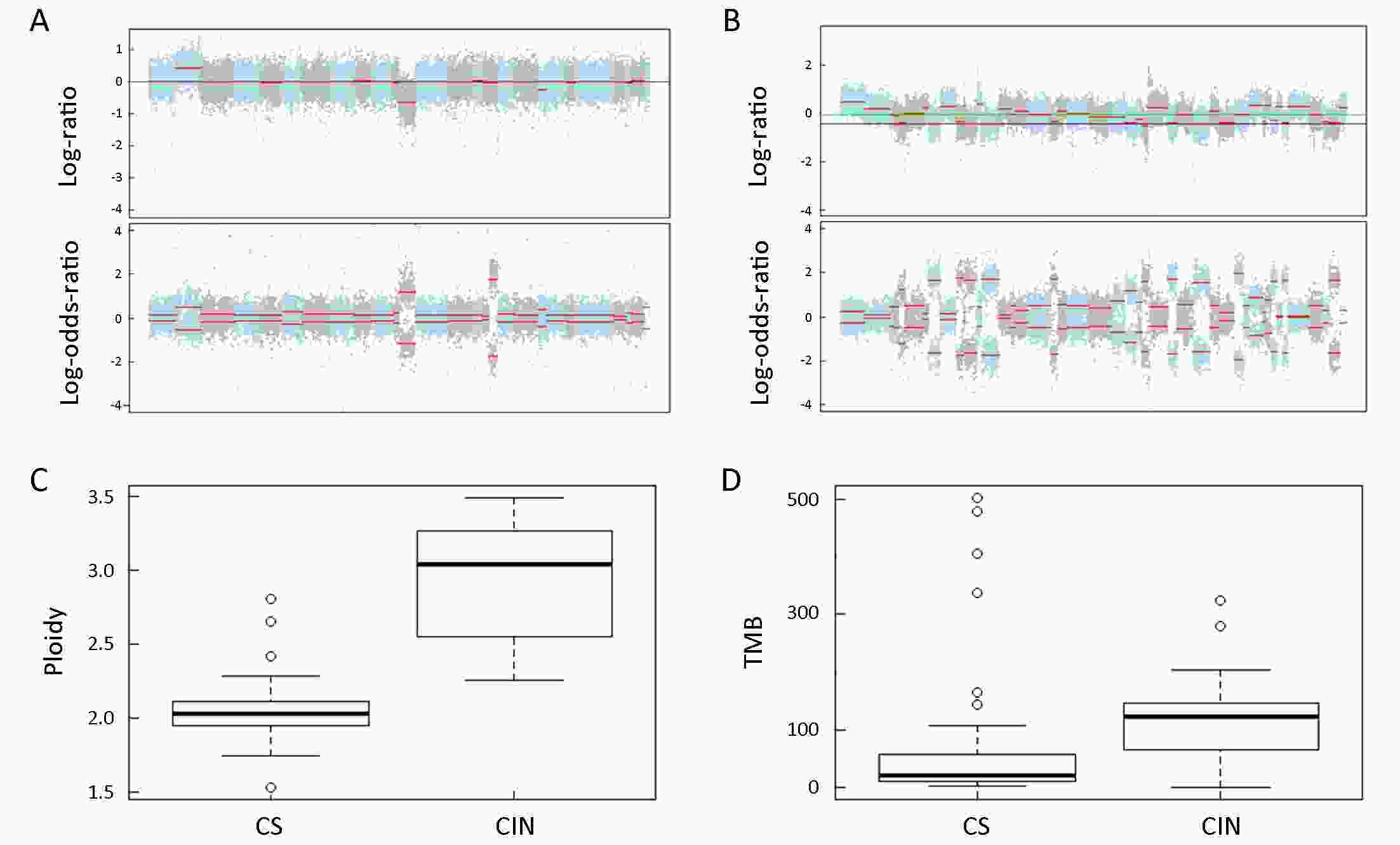
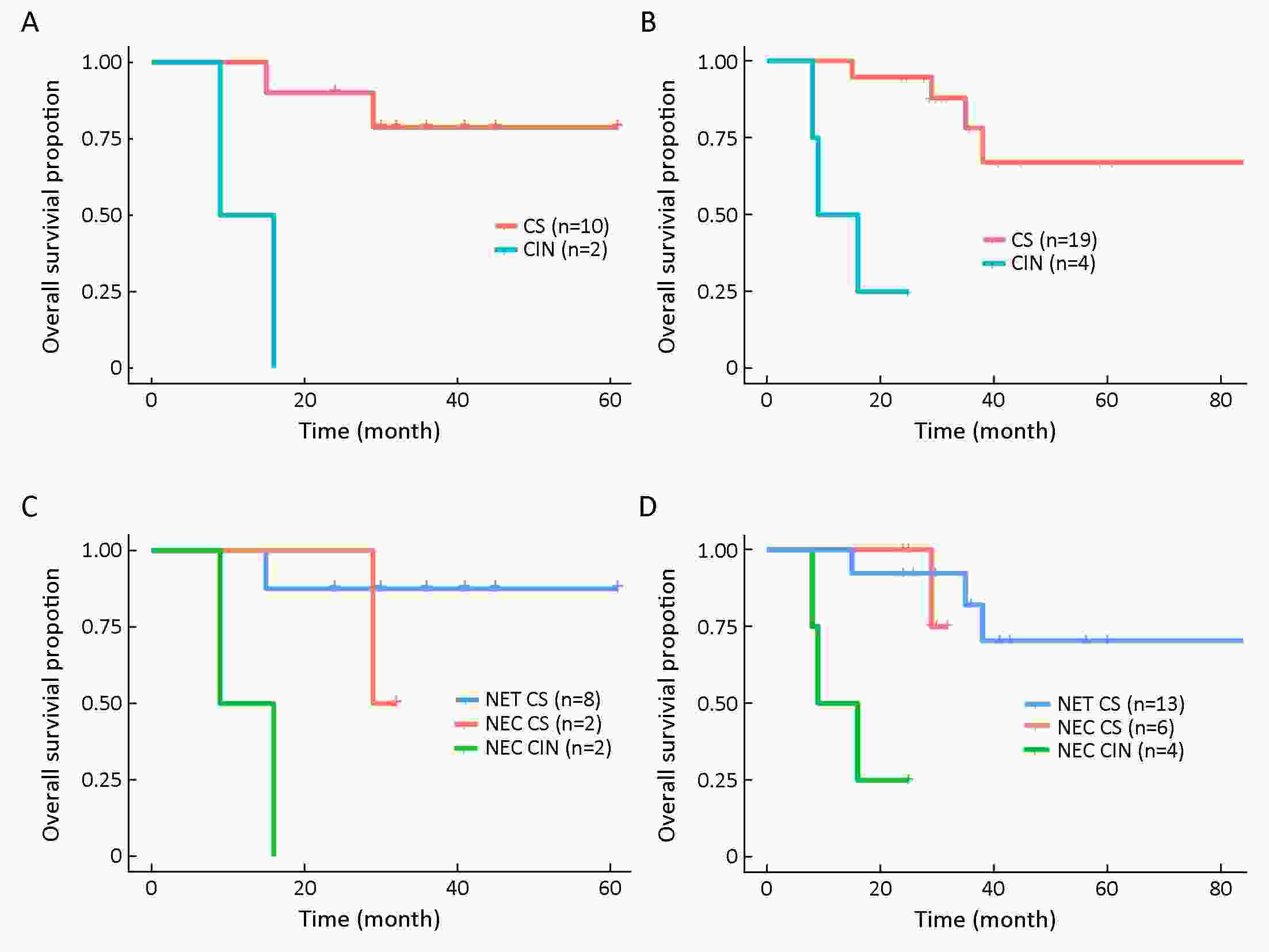
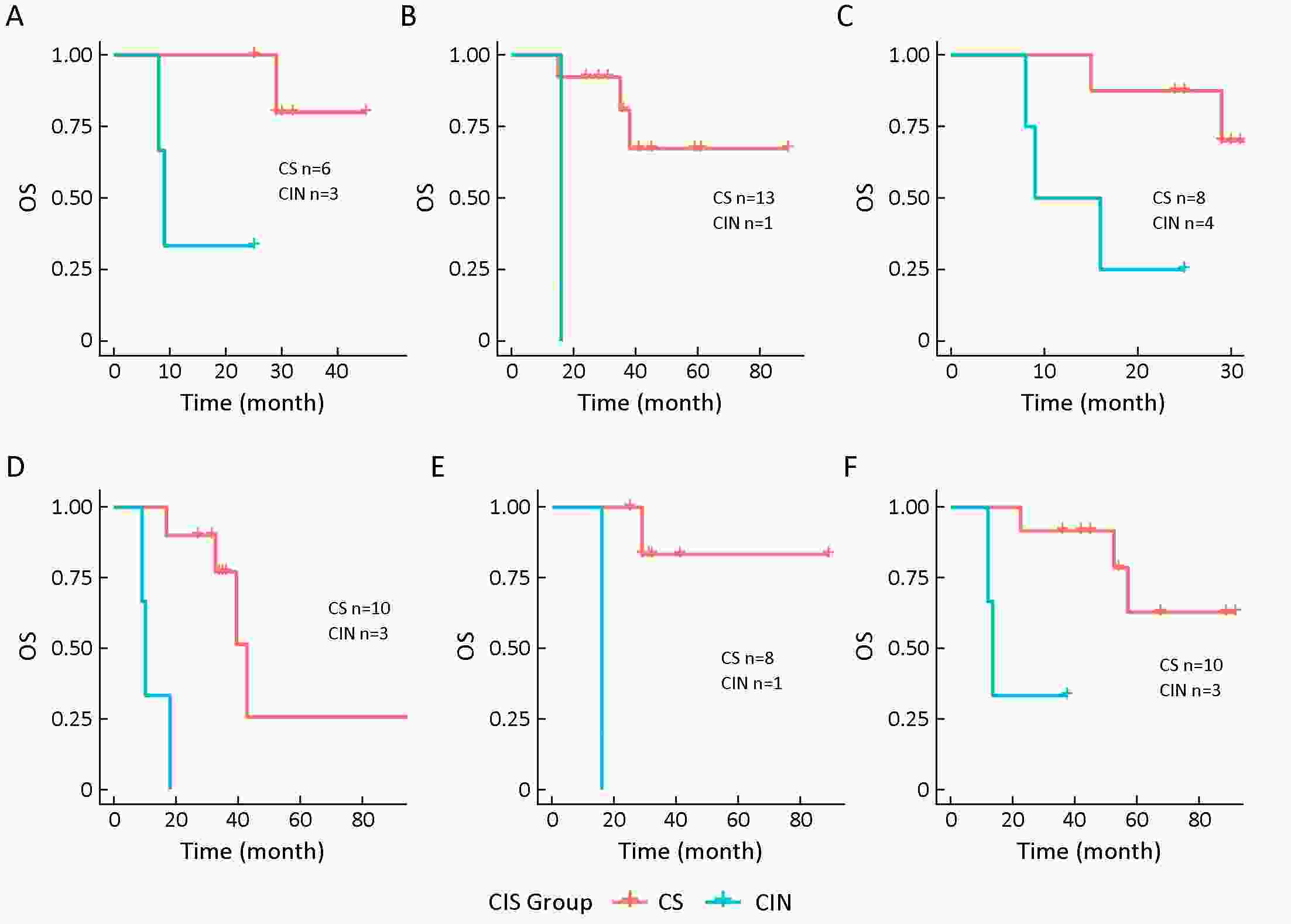
ObjectiveNeuroendocrine neoplasms (NENs) are relatively rare and heterogeneous malignancies with two major subtypes: low-grade neuroendocrine tumor (NET) and high-grade neuroendocrine carcinoma (NEC). Comprehensive molecular characterization of NENs is needed to refine our understanding of the biological underpinnings of different NEN subtypes and to predict disease progression more accurately. MethodsWe performed whole-exome sequencing (WES) of NEN samples from 49 patients (25 NETs and 24 NECs) arising from the stomach, intestines or lung. Clinicopathologic features were assessed and associated with molecular events. ResultsNENs generally harbor a low mutation burden, with TP53 being the top mutated gene found in 31% of patients. Consistent with other studies, p53 signaling pathway dysfunction is significantly enriched in NECs compared to NETs (P<0.01). Other than TP53, tissue type-specific mutation profiles of NENs were observed in our cohort compared to those reported in pancreatic NETs. Importantly, we observed significant genomic instability, with increased copy number alterations observed across the NEN genome, which was more profound in NECs and independently correlated with poor overall survival (OS) (P<0.001). NECs could be further stratified into two molecular subtypes based on OS (P<0.001) and the chromosomal instability score (CIS). Interestingly, we discovered that the gain of whole chromosome 5 occurred at the early stage of NEN development, followed by the loss of 5q exclusively in NECs (P<0.001). ConclusionsThese findings provide novel insights into the molecular characteristics of NENs and highlight the association of genomic stability with clinical outcomes.
2019, 31(6): 930-944.
doi: 10.21147/j.issn.1000-9604.2019.06.09
Abstract:
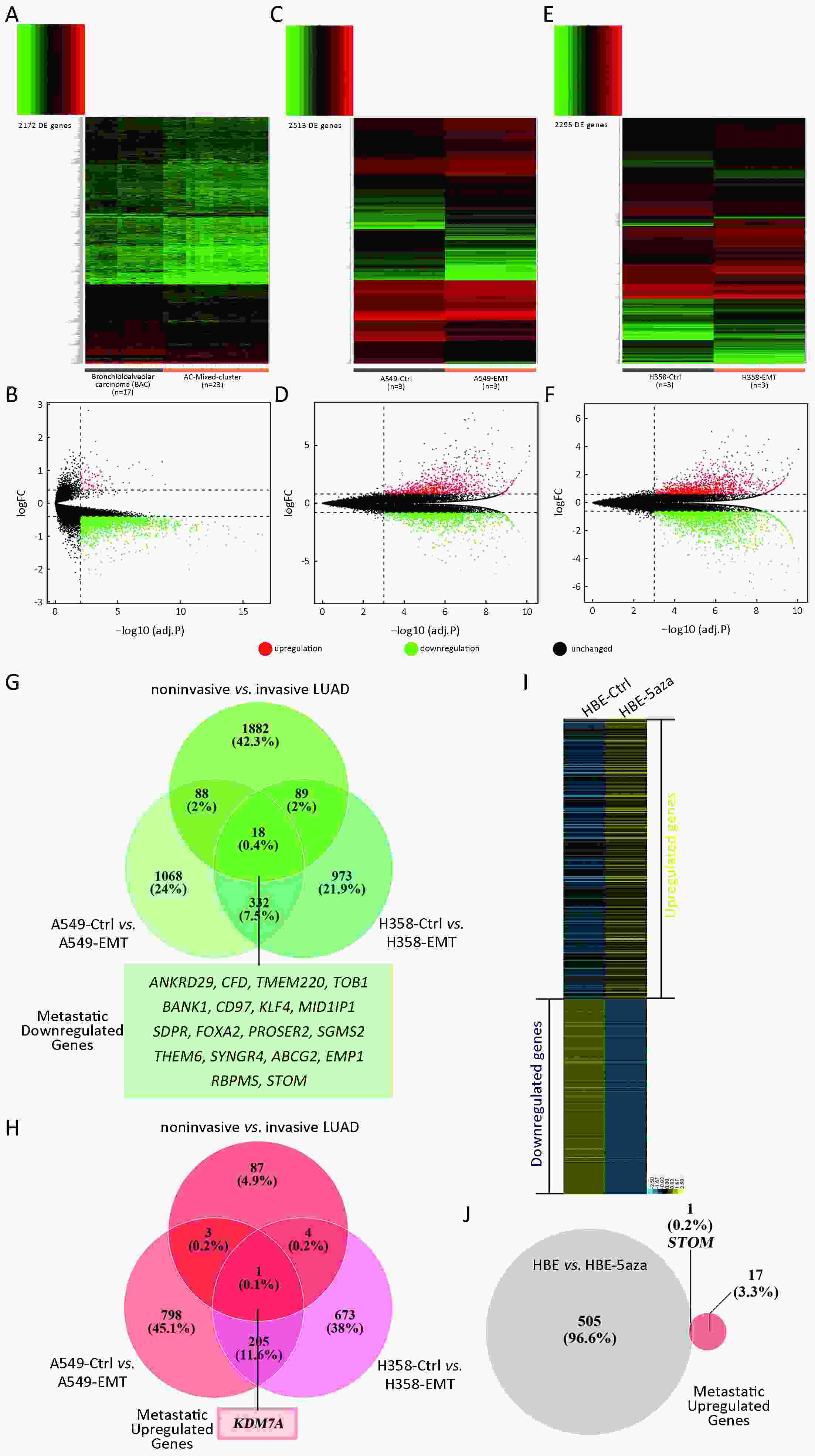
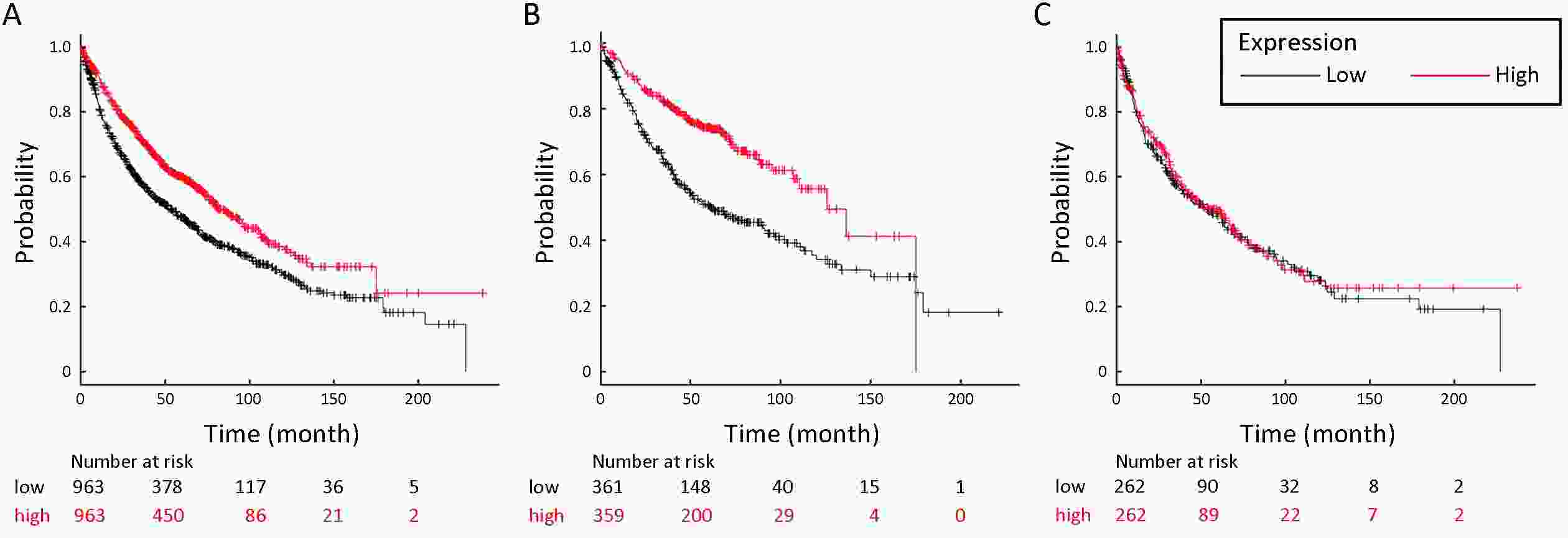
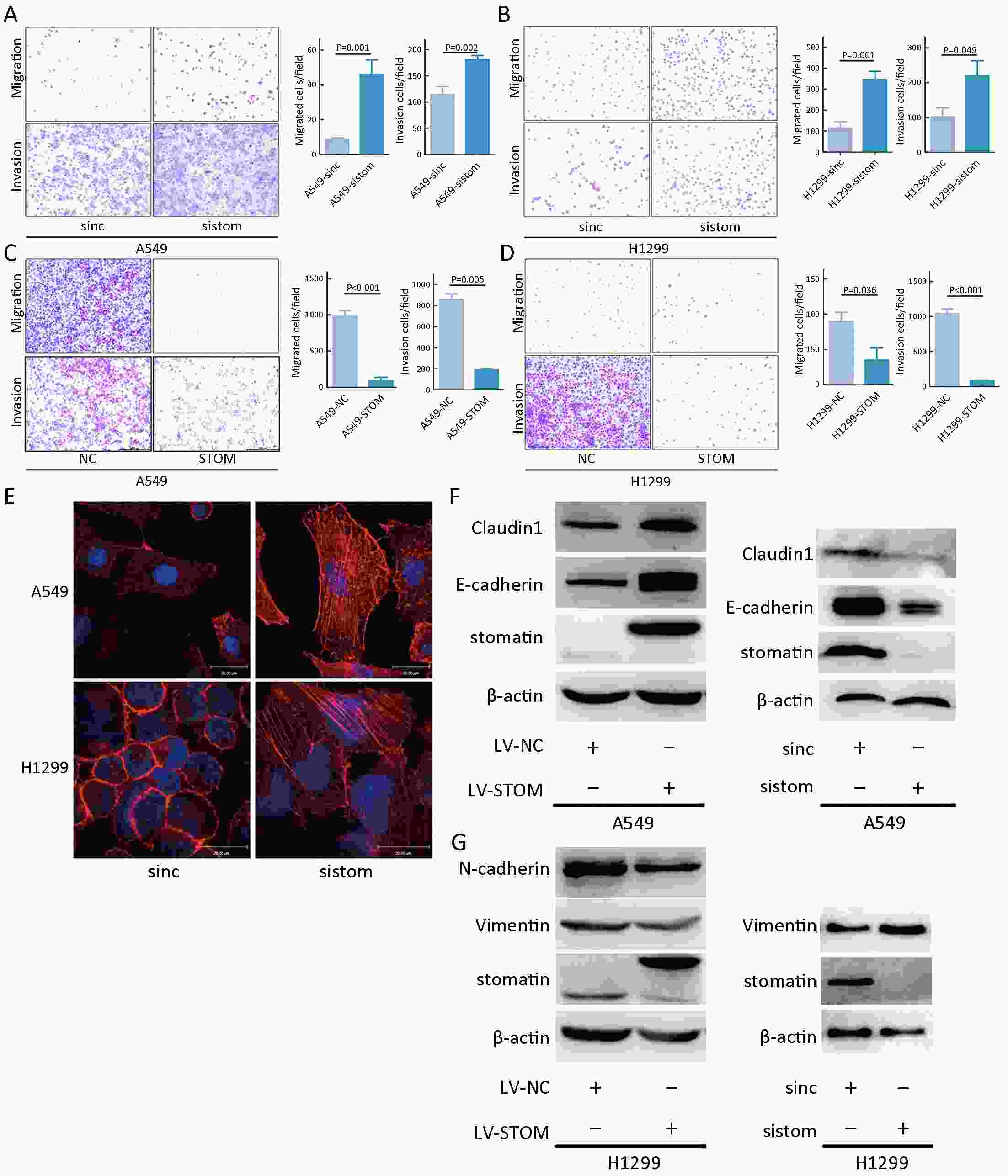
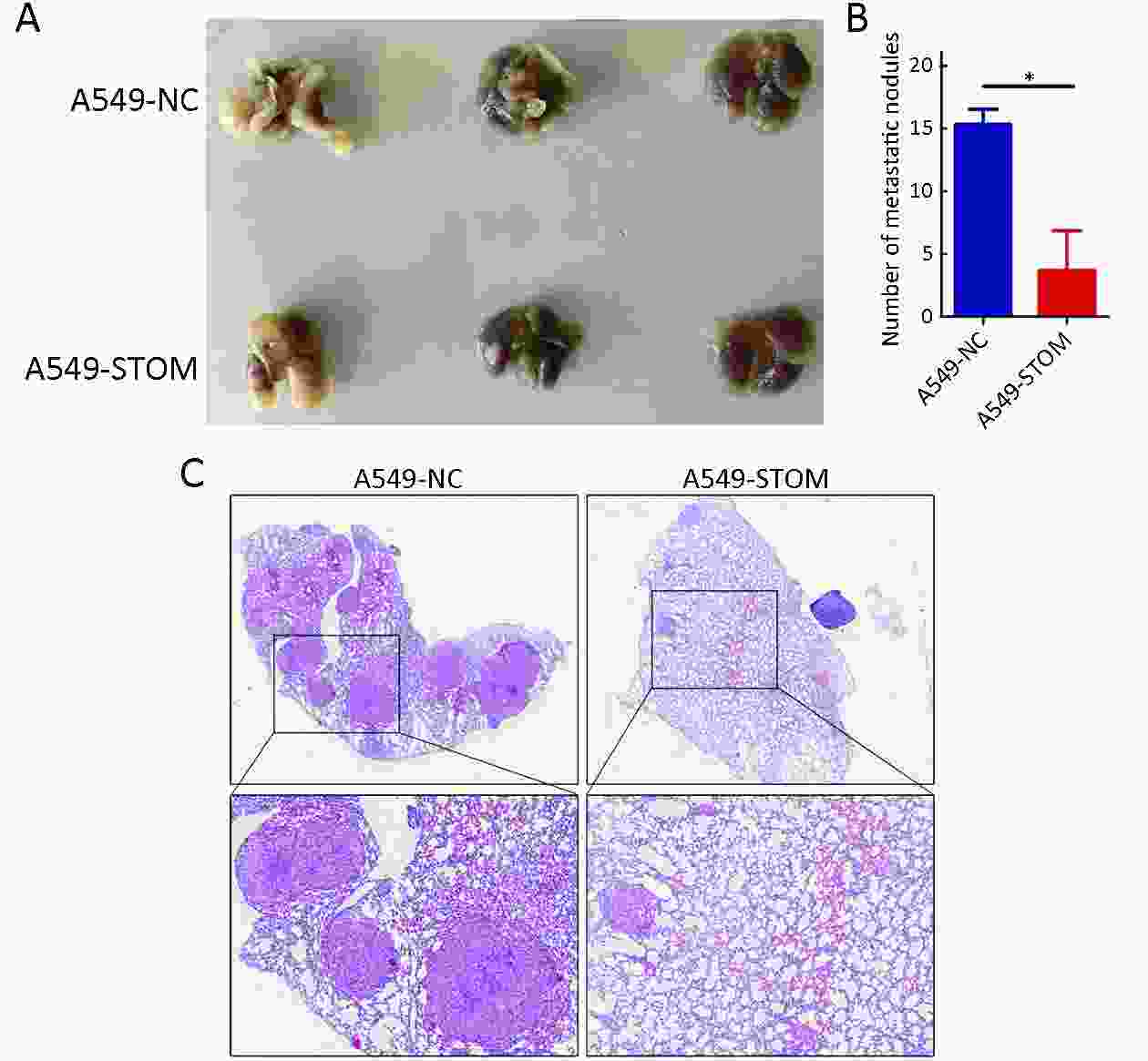
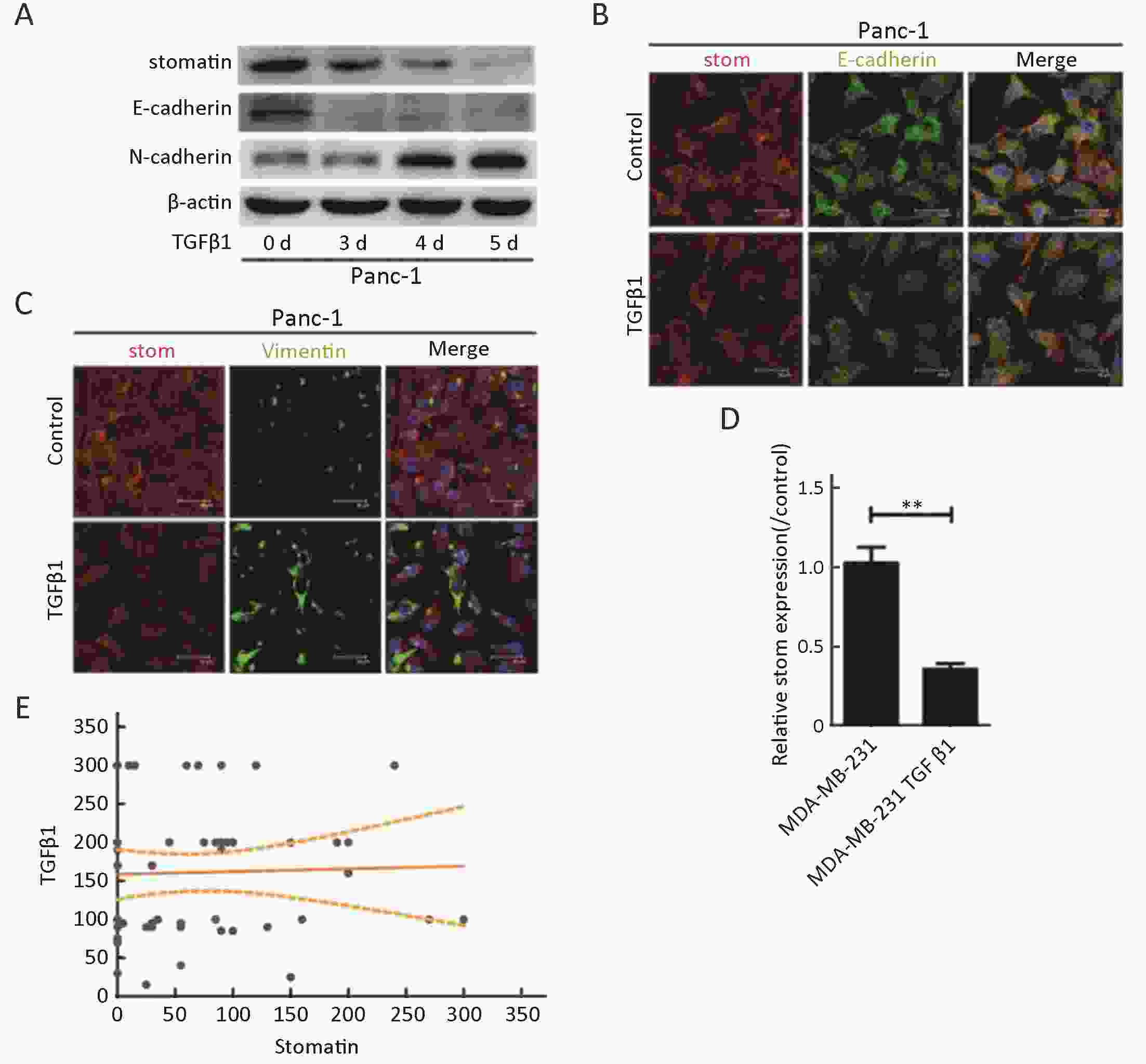
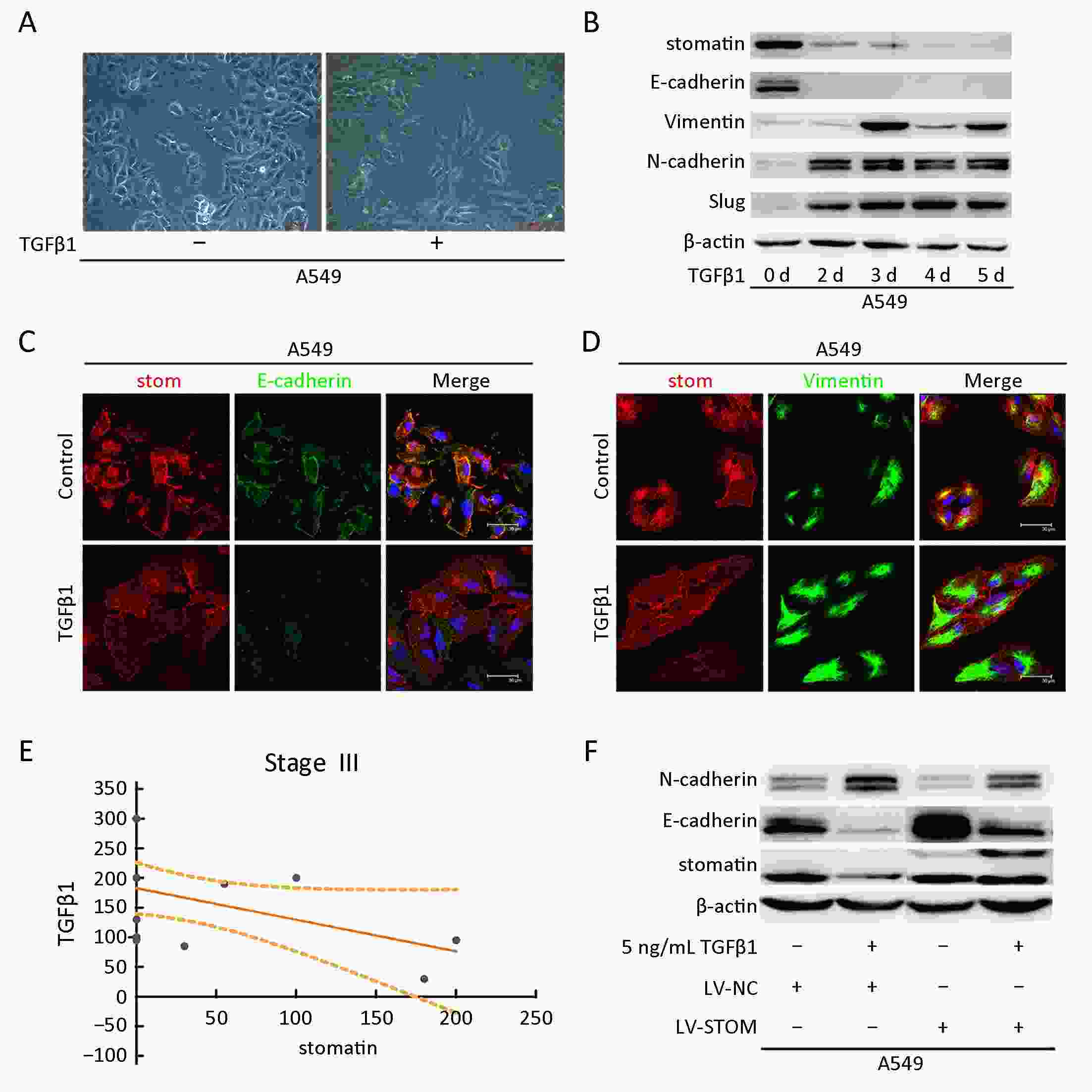
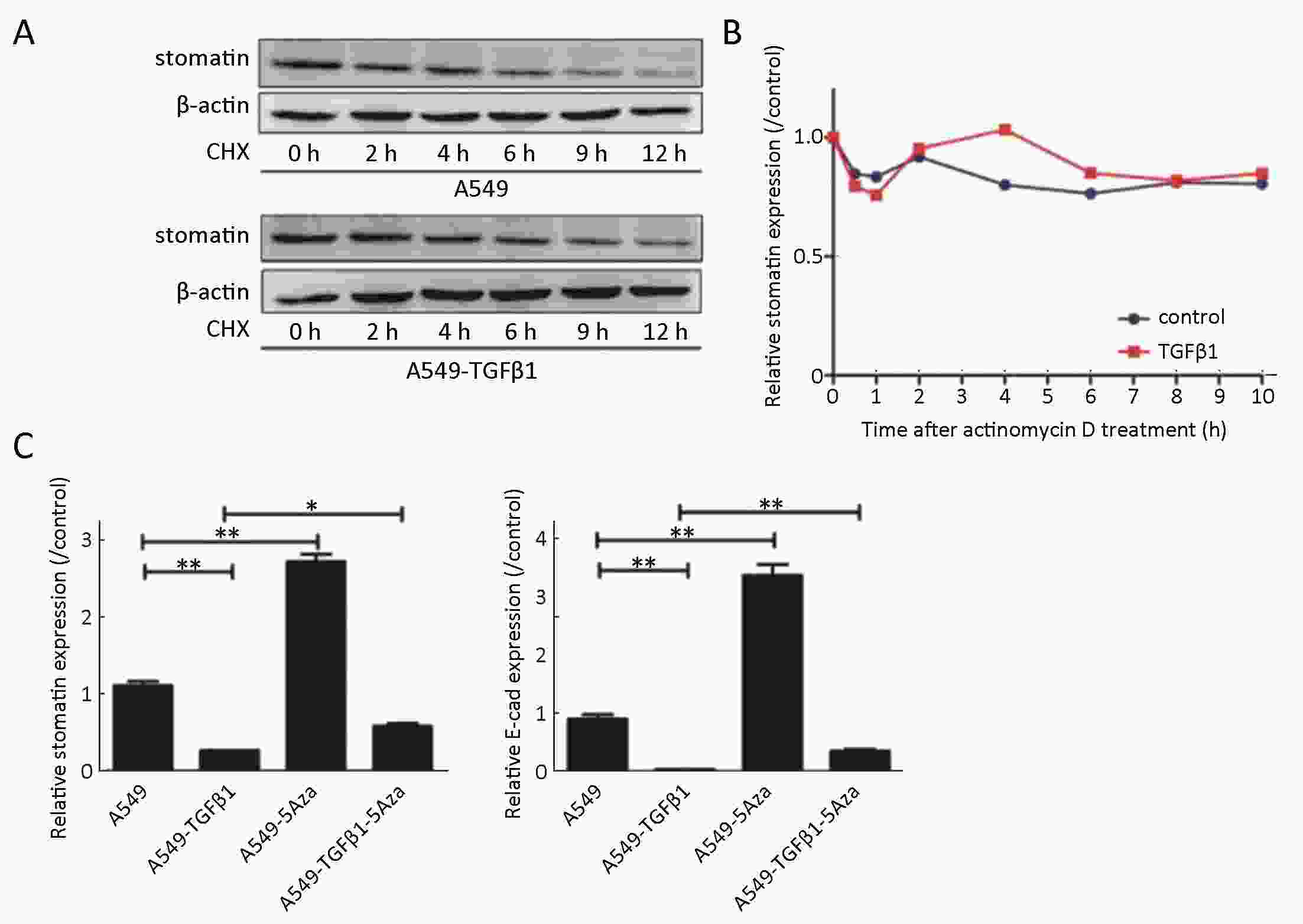
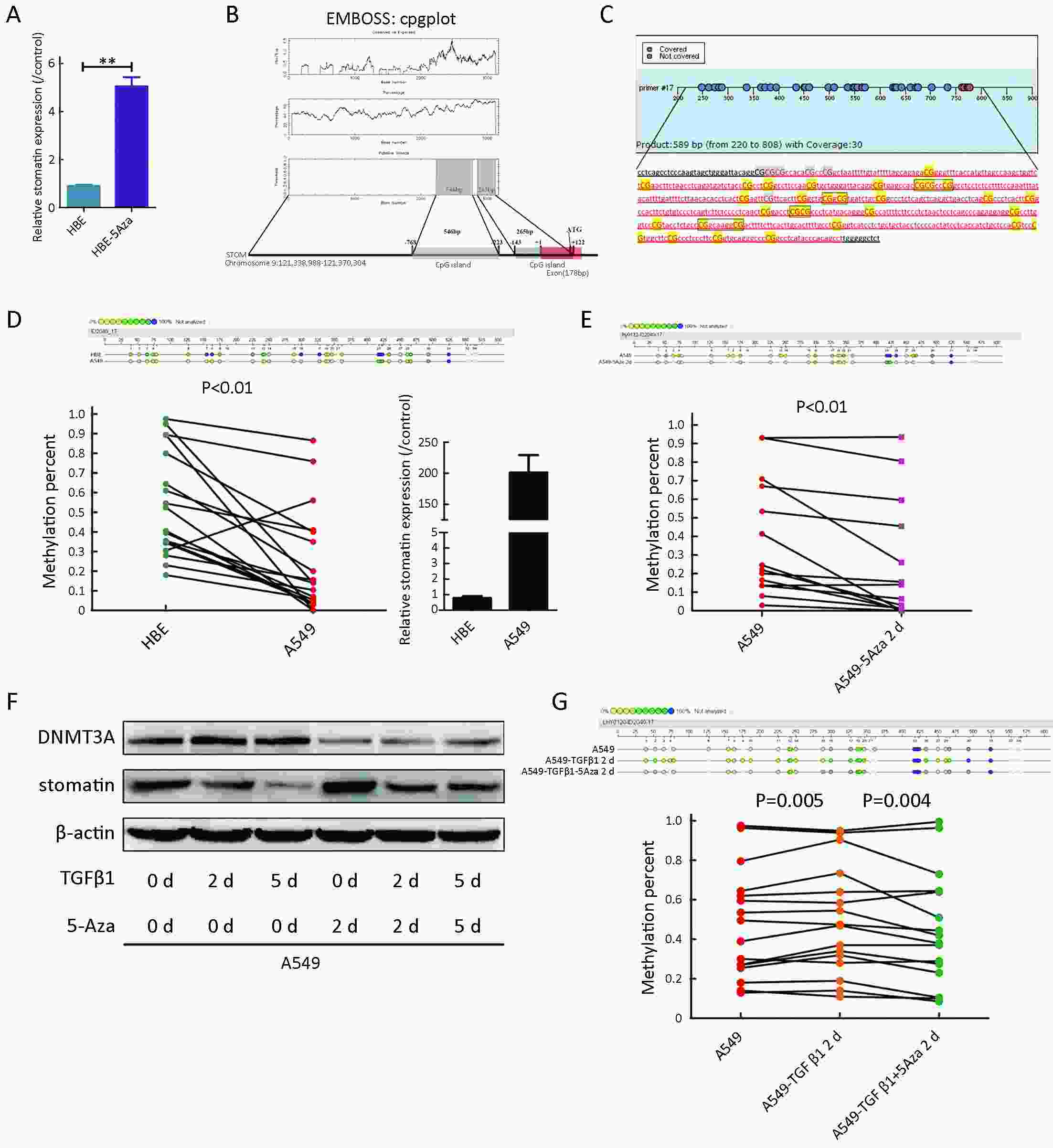
ObjectiveMetastasis is one of the key causes of high mortality in lung cancer. Aberrant DNA methylation is a common event in metastatic lung cancer. We aimed to identify new epigenetic regulation of metastasis-associated genes and characterize their effects on lung cancer progression. MethodsWe screened genes associated with non-small cell lung cancer (NSCLC) metastasis by integrating datasets from the Gene Expression Omnibus (GEO) database. We obtained epigenetic-regulated candidate genes by analyzing the expression profile of demethylation genes. By overlapping analysis, epigenetically modulated metastasis-associated genes were obtained. Kaplan-Meier plotter (KM plotter) was utilized to assess the overall survival (OS) of stomatin in lung cancer. Immunohistochemistry (IHC) was conducted to determine the association between stomatin and metastasis-associated clinical indicators. Both in vitro and in vivo assays were performed to investigate the potential role of stomatin in metastasis. The regulation mechanisms of transforming growth factor β1 (TGFβ1) on stomatin were determined by Sequenom MassARRAY quantitative methylation and western blot assays. ResultsA series of bioinformatic analyses revealed stomatin as the metastasis-associated gene regulated by DNA methylation. The KM plotter analysis showed a positive association between stomatin and the OS of lung cancer. IHC analysis indicated that the decreased stomatin expression is linked with advanced TNM stage. Loss- and gain-of-function experiments displayed that stomatin could inhibit the migration and invasion of NSCLC cells. Furthermore, TGFβ1 repressed stomatin expression during epithelial-to-mesenchymal transition (EMT). The negative correlation between stomatin and TGFβ1 was also validated in advanced stage III lung tumor samples. The underlying mechanism by which TGFβ1 inhibits stomatin is due in part to DNA methylation. ConclusionsOur results suggest that stomatin may be a target for epigenetic regulation and can be used to prevent metastatic diseases.
2019, 31(6): 945-954.
doi: 10.21147/j.issn.1000-9604.2019.06.10
Abstract:
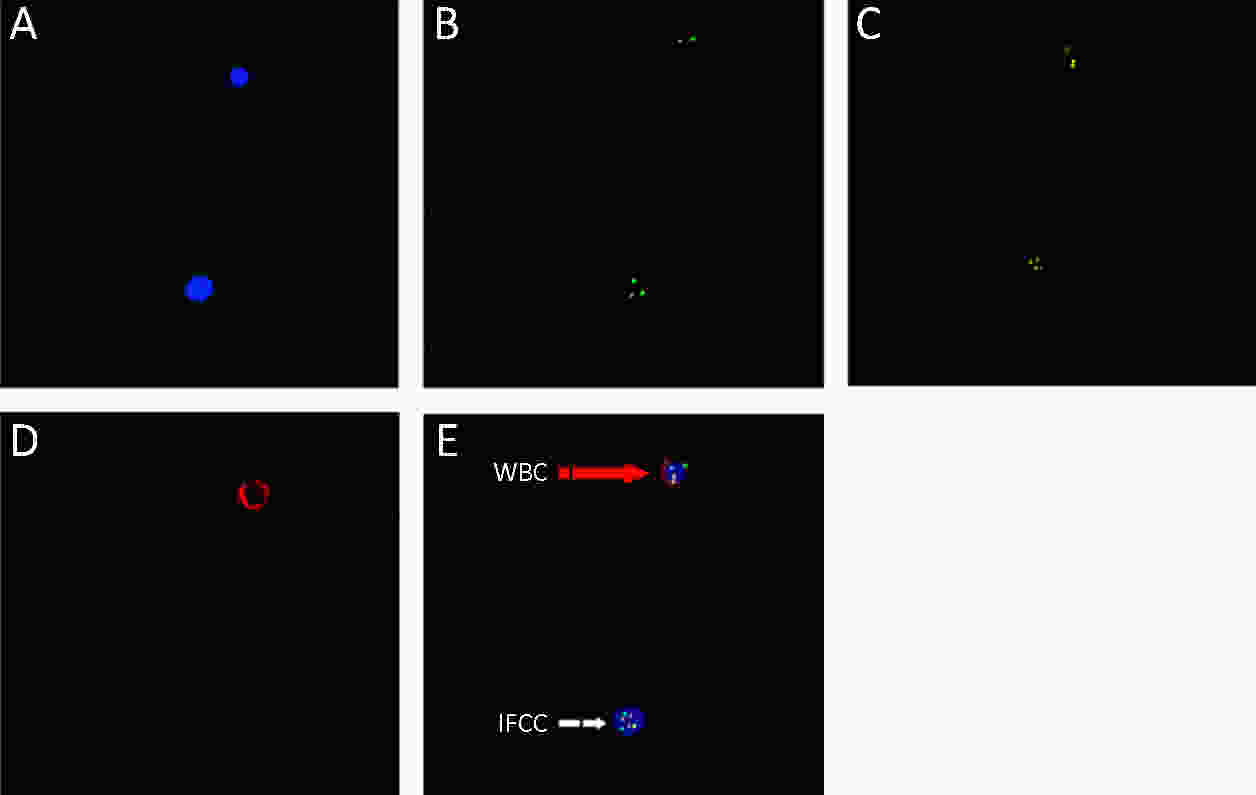
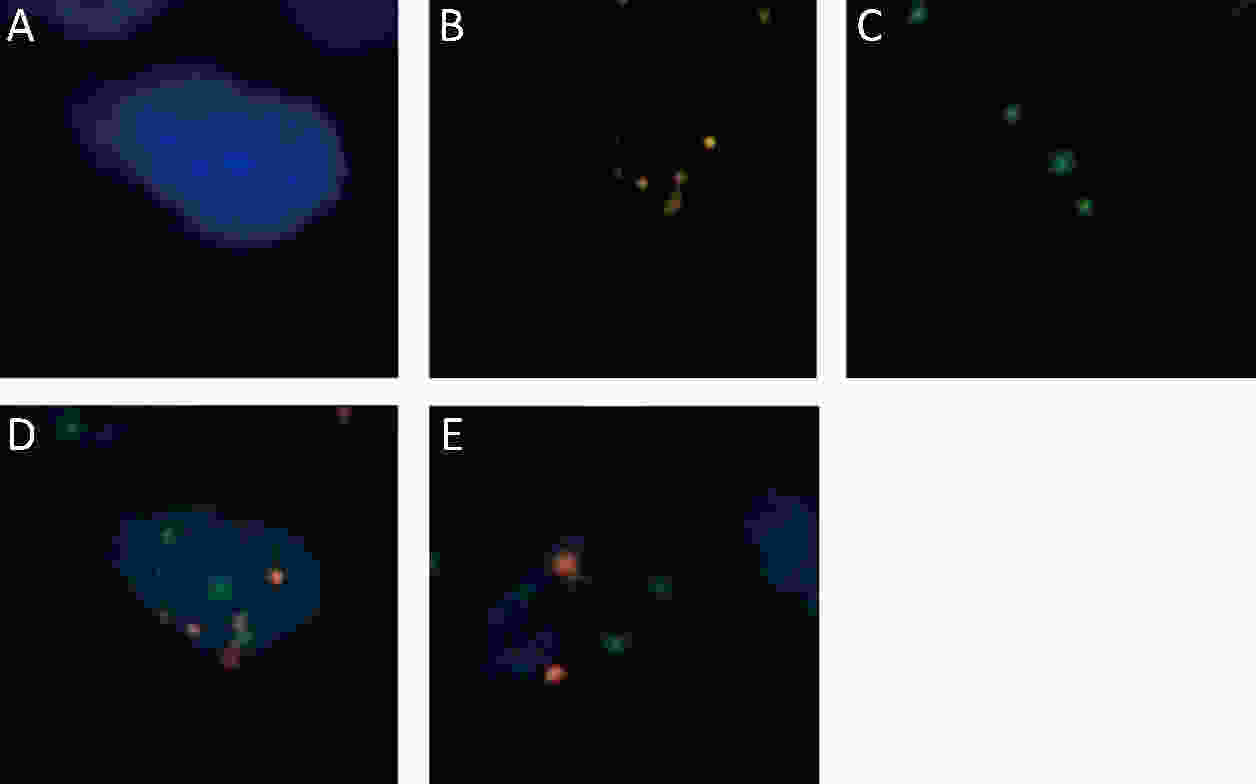
ObjectiveTo explore the intraperitoneal free cancer cell (IFCC) detection value of negative enrichment and immune fluorescence in situ hybridization (NEimFISH) on chromosomes (CEN) 8/17. MethodsTo verify the reliability of NEimFISH, 29 gastric cancer tumors, their adjacent tissues and greater omental tissues were tested. Our study then included 105 gastric cancer patients for IFCC. We defined patients as IFCC-positive if a signal was detected, regardless of the detailed cancer cell numbers. A comparison of clinicopathological features was conducted among IFCC groups. We also compared the diagnosis value and peritoneal recurrence predictive value among different detection methods. The comparison of IFCC number was also conducted among different groups. ResultsA cutoff of 2.5 positive cells could distinguish all benign tissue samples and 97% of malignant tissue samples in our study. Compared to intestinal gastric cancer, patients with diffuse gastric cancer tended to have more IFCCs (6 vs. 4, P=0.002). The IFCC counts were often higher in the lymphovascular invasion positive group than negative group (3 vs. 1, P=0.022). All IFCC samples that were considered positive using conventional cytology were also found to be positive using NEimFISH. When compared to conventional cytology and paraffin pathology, NEimFISH had a higher IFCC positive rate (68.9%) and higher one-year peritoneal recurrence predictive value with area under the curve (AUC) of 0.922. ConclusionsGastric cancer could be effectively diagnosed by NEimFISH. The IFCC number found using NEimFISH on CEN8/17 is closely associated with Lauren type and vascular invasion of cancer. NEimFISH is a reliable detection modality with a higher positive detection rate, higher one-year peritoneal recurrence predictive value and quantitative features for IFCC of gastric cancer.
2019, 31(6): 955-964.
doi: 10.21147/j.issn.1000-9604.2019.06.11
Abstract:
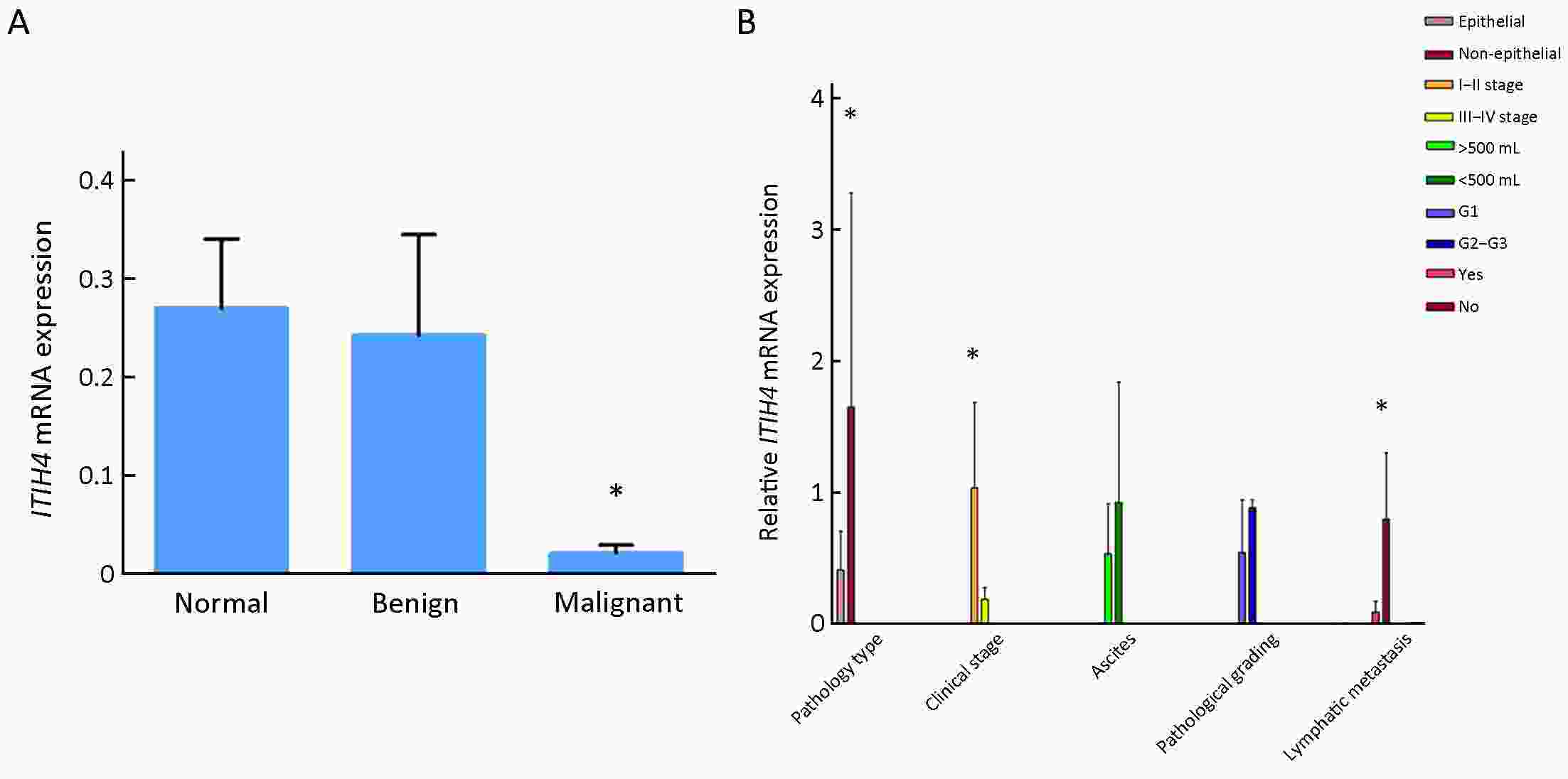
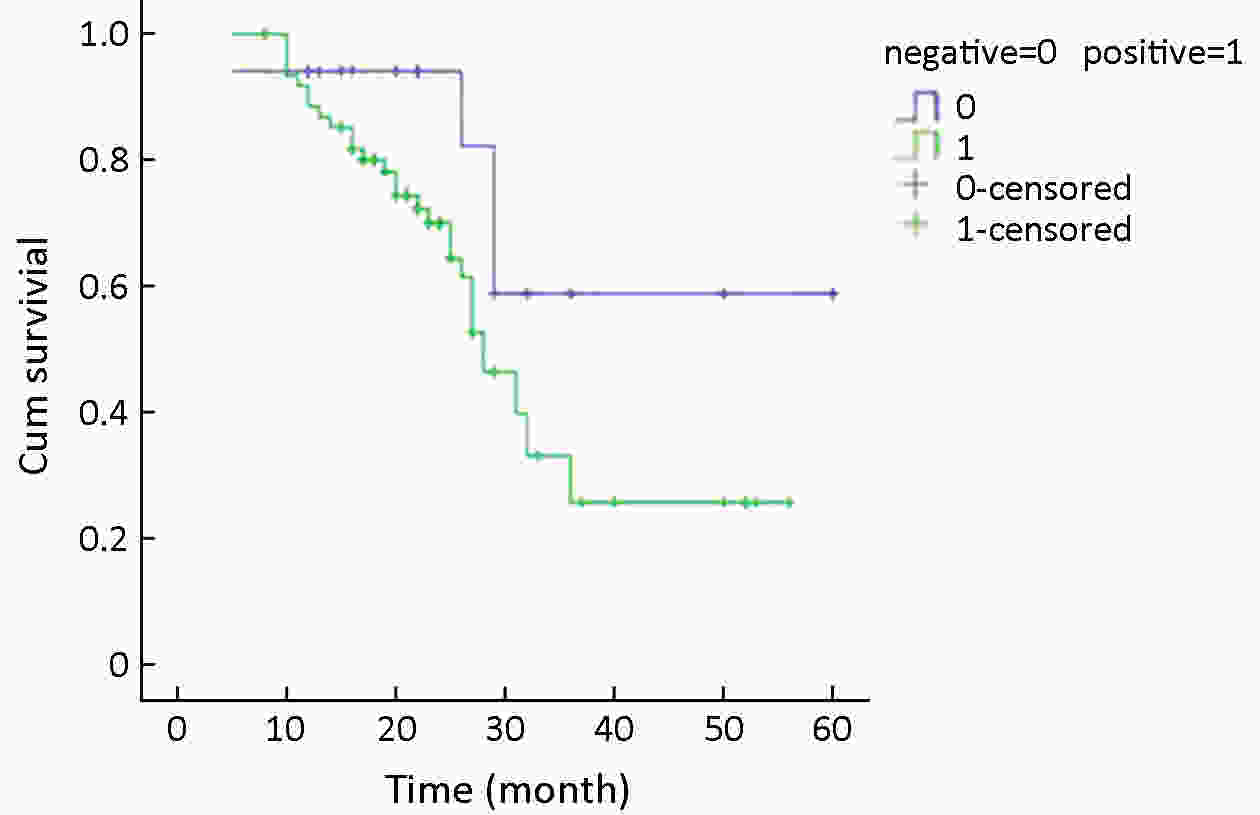
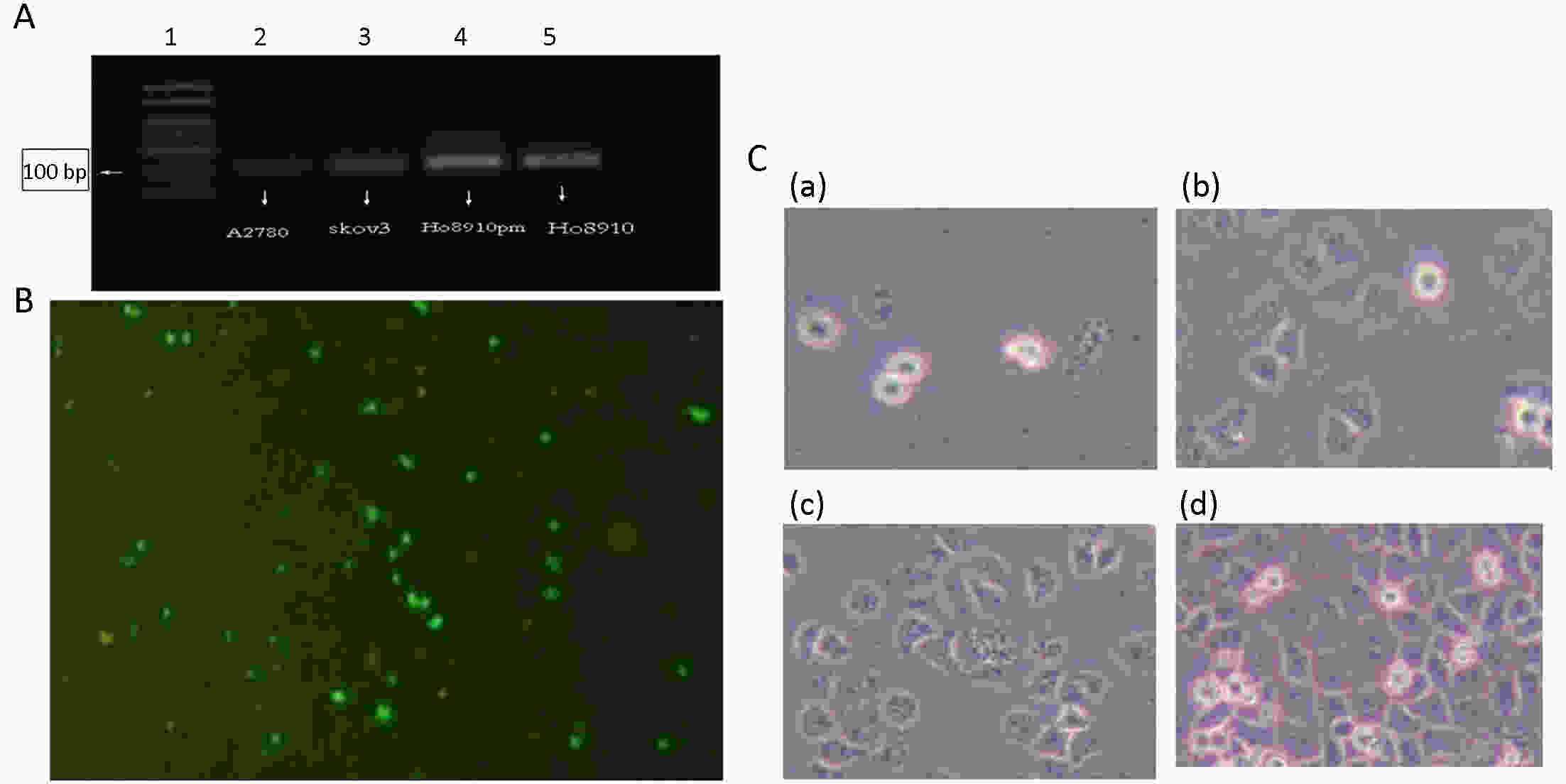
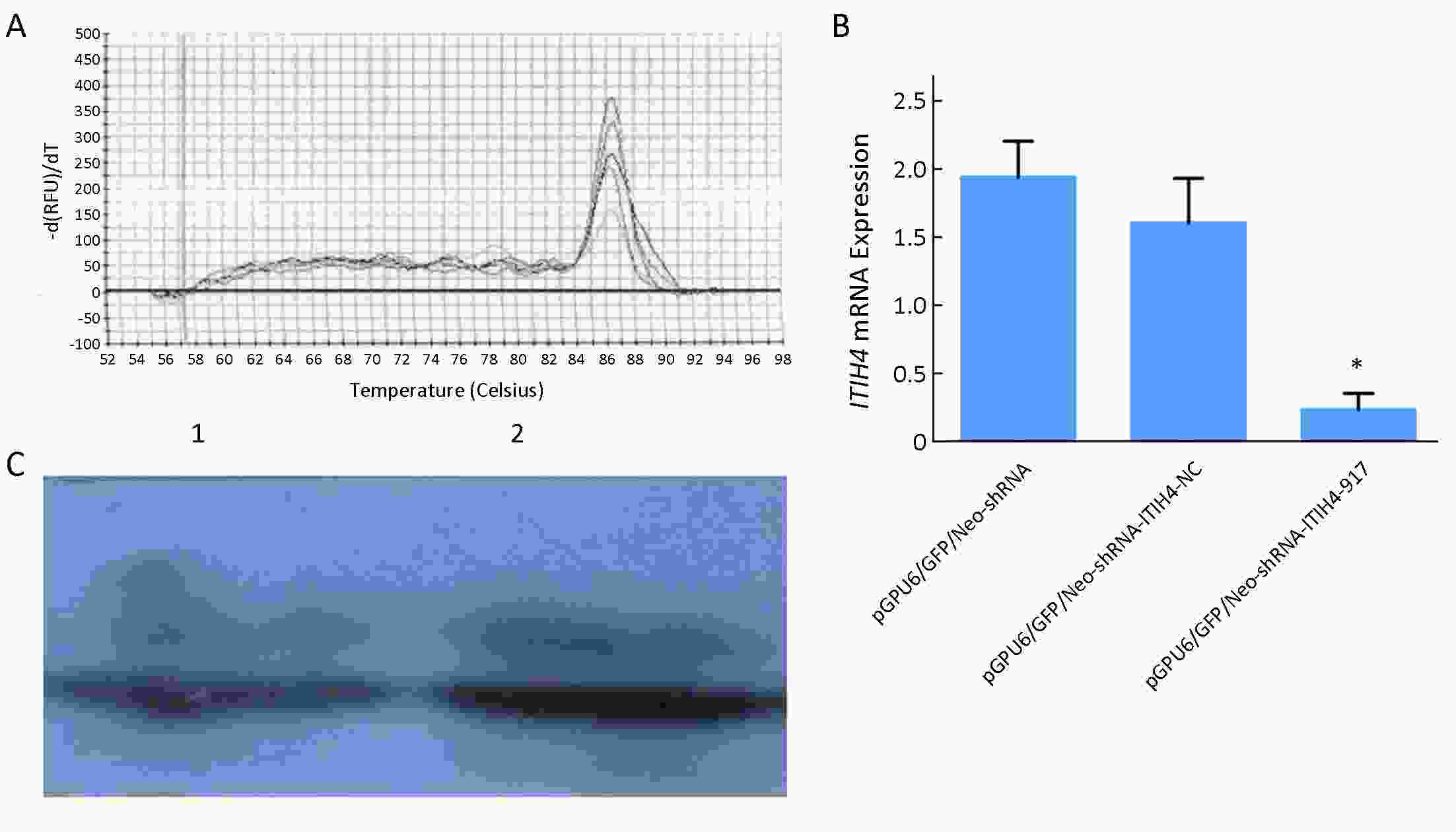
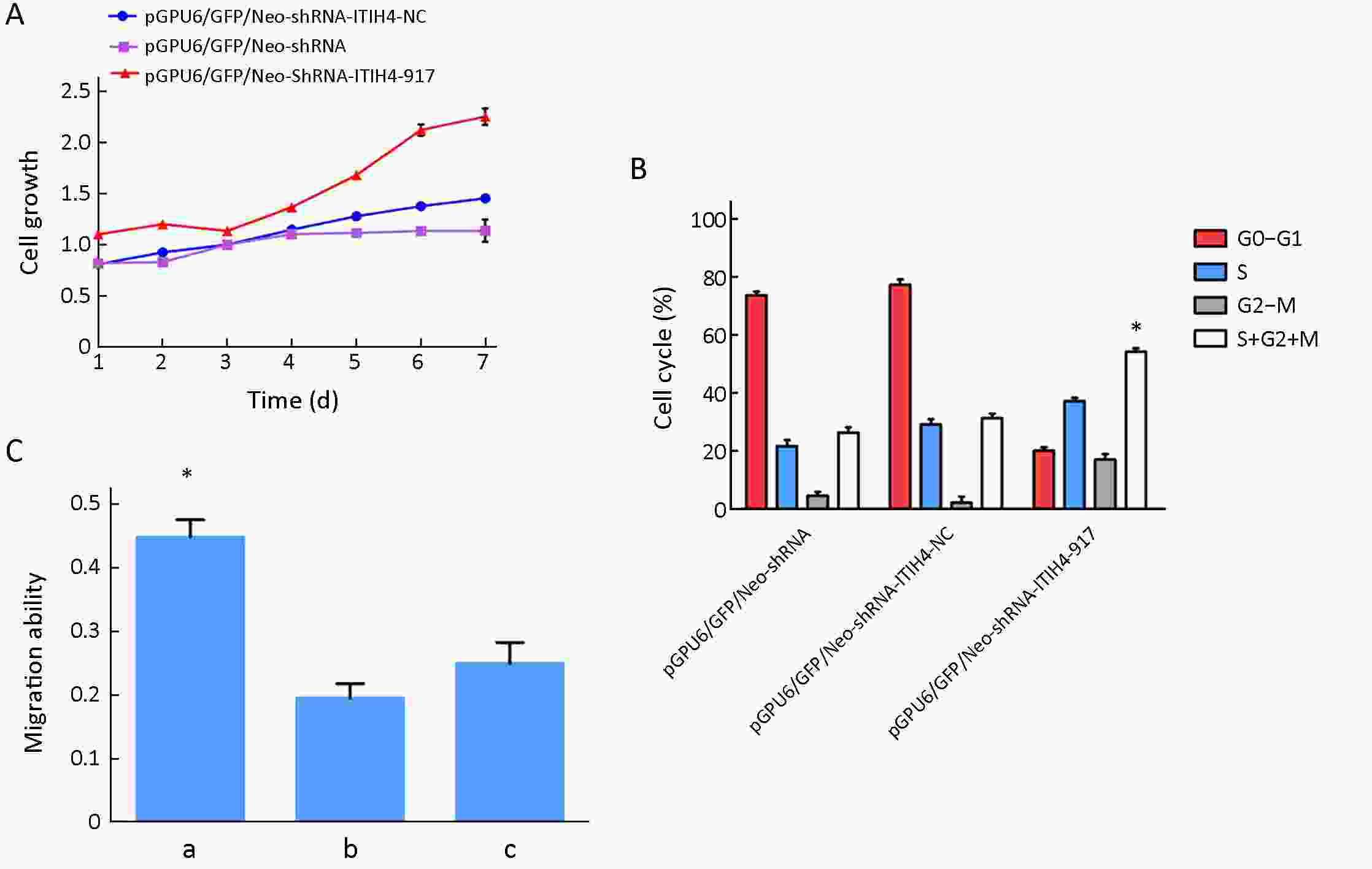
ObjectiveThe inter-α-trypsin inhibitor heavy chain 4 (ITIH4) protein is involved in the development of tumors. However, the relationship between ITIH4 and ovarian cancer (OC) has not been extensively examined. This study aimed to explore the effect of ITIH4 on OC and to identify its underlying mechanism. MethodsExpressions of ITIH4 in OC tissues and cells were determined using quantitative reverse transcription polymerase chain reaction (RT-qPCR) and western blots. The function of ITIH4 in the OC cell line HO8910pm was tested via ITIH4 knockdown. The cell growth rate was measured using MTT and colony formation assays. Flow cytometry was performed to evaluate cell cycle progression. Cell migration and invasion abilities were observed using the transwell migration assay. ResultsITIH4 was downregulated in OC tissues and cells. ITIH4 knockdown promoted cell growth and cell cycle progression. Consistent with these results, inhibition of ITIH4 in OC cells significantly increased cell migration and invasion abilities. Cox regression analysis suggests that ITIH4 expression alone is not a good predictor of the prognosis of malignant ovarian tumors in patients. ConclusionsITIH4 inhibits the progression of OC, suggesting that ITIH4 may be a useful biomarker for OC. This study may provide a potential novel target for the treatment of OC.
2019, 31(6): 965-973.
doi: 10.21147/j.issn.1000-9604.2019.06.12
Abstract:
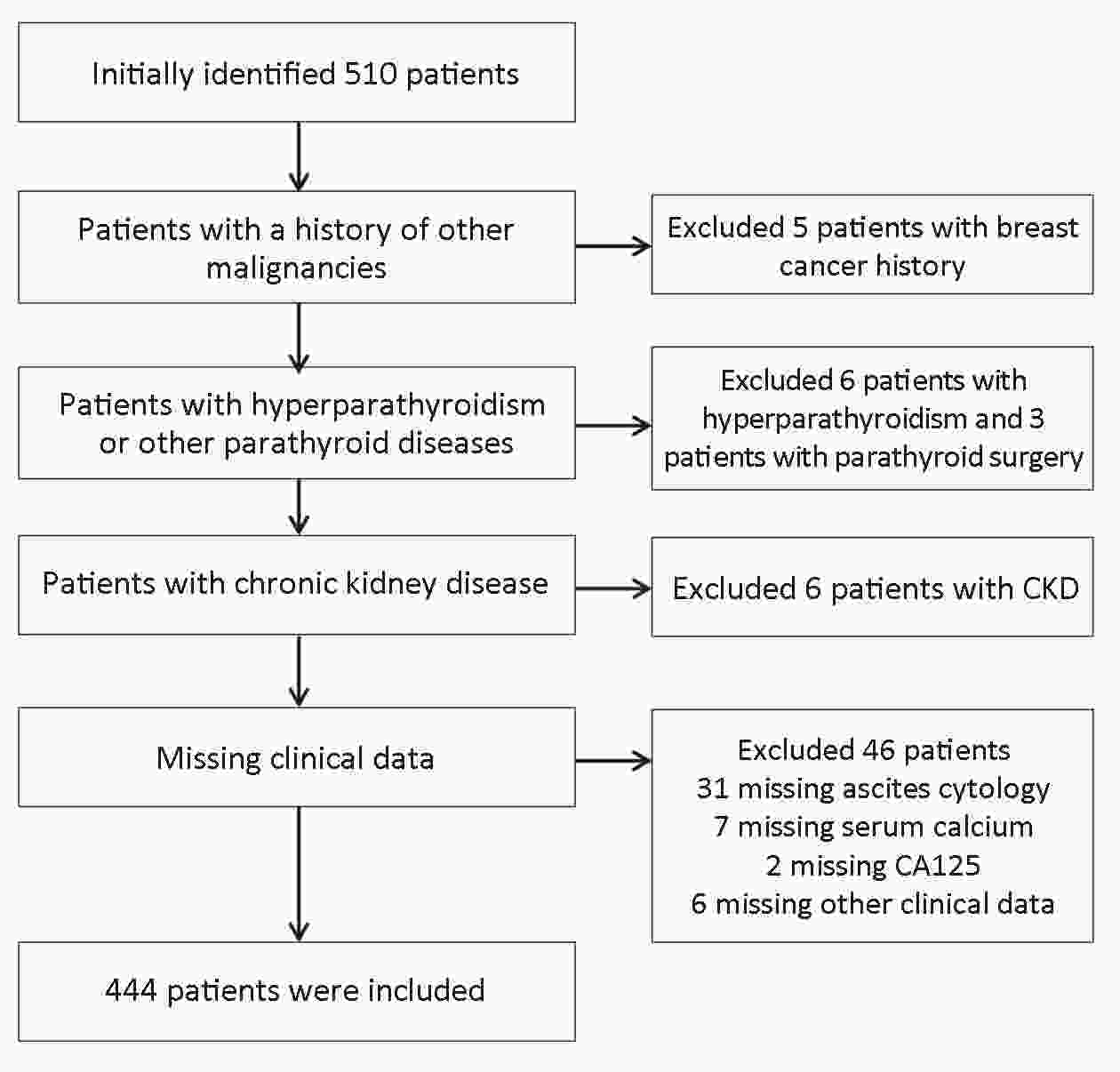
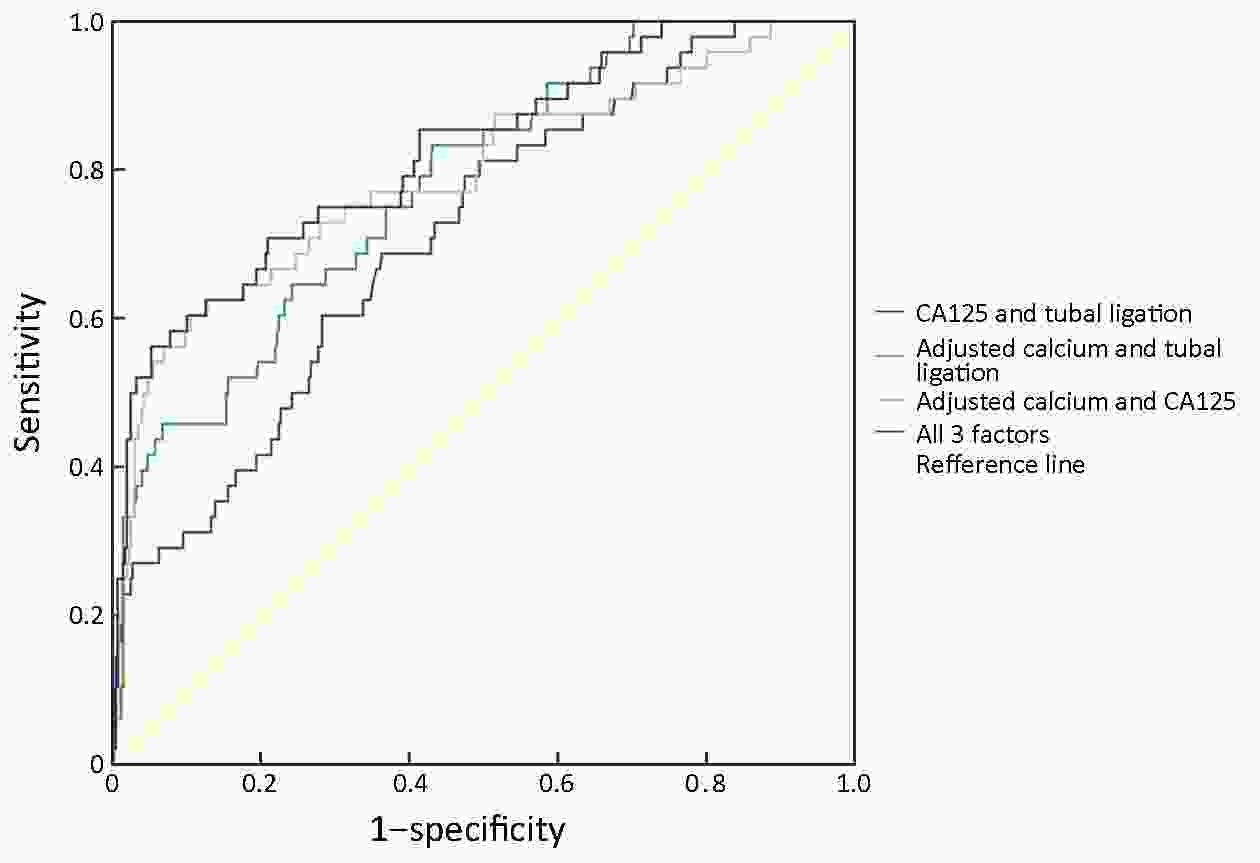
ObjectiveTo evaluate preoperative serum calcium concentration and investigate the association between calcium level and positive peritoneal cytology in endometrial carcinoma (EC). MethodsA total of 510 patients who were diagnosed with EC and had surgery were initially enrolled in this study at Peking University People’s Hospital between January 2012 and December 2016. Clinical characteristics and preoperative serum calcium, albumin, carbohydrate antigen (CA)125, CA19-9, carcinoembryonic antigen (CEA) were extracted from patient records and evaluated according to postoperative peritoneal cytology. Predictive factors were assessed with Cox univariate and multivariate analyses. Factors selected from multivariate analysis results were used to build a predictive model. ResultsA total of 510 patients are identified in our database and 444 patients who fulfilled inclusion and exclusion criteria are included in this study. Univariate analysis revealed that ionized calcium concentration was closely related to positive peritoneal cytology, tumor grade and lymph-vascular space invasion (LVSI). Moreover, peritoneal cytology was significantly associated with hypertension, tubal ligation, serum CA125, CA19-9, CEA and ionized calcium level. Multivariate analysis revealed that albumin-adjusted calcium level, CA125 and tubal ligation were independent predictive factors of positive peritoneal cytology (P<0.05). A combination of ionized calcium level with the other two indexes yielded significantly great area under the curve (AUC=0.824). ConclusionsThis study enhanced the value of preoperative ionized calcium level. We also identified several potential biomarkers to predict positive peritoneal cytology in EC patients before surgery.
2019, 31(6): 974-983.
doi: 10.21147/j.issn.1000-9604.2019.06.13
Abstract:
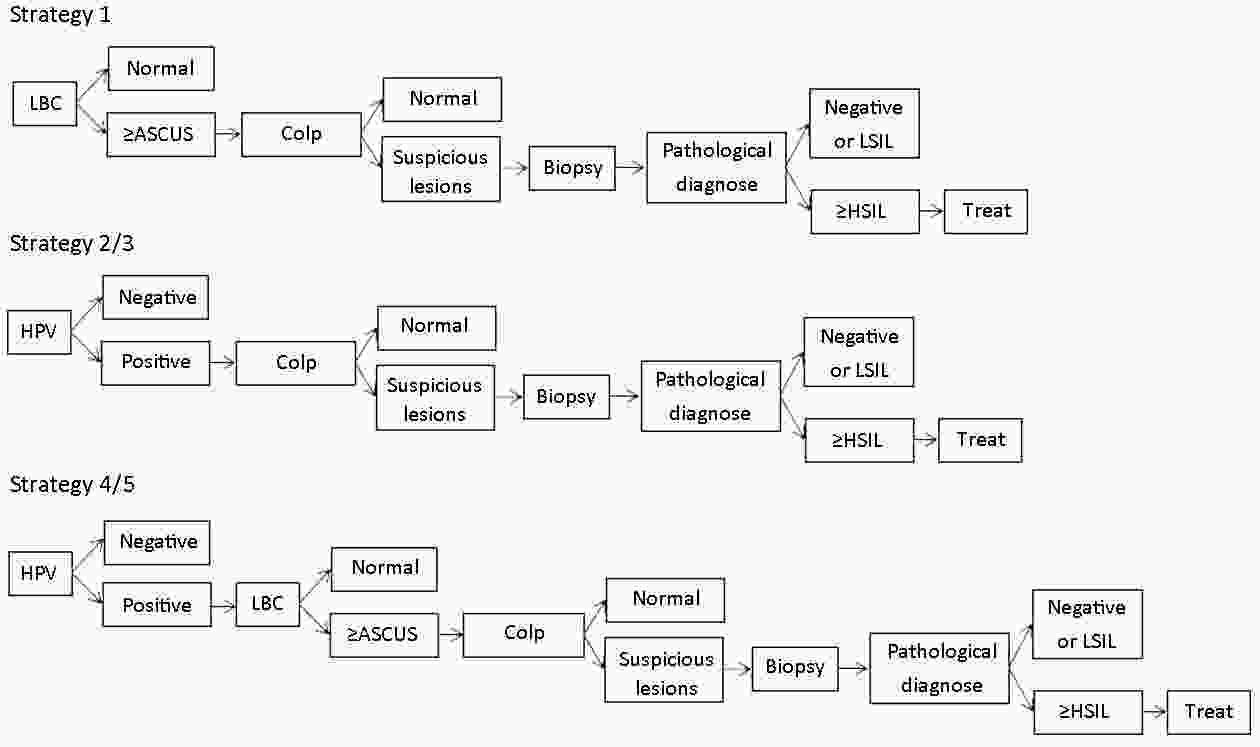
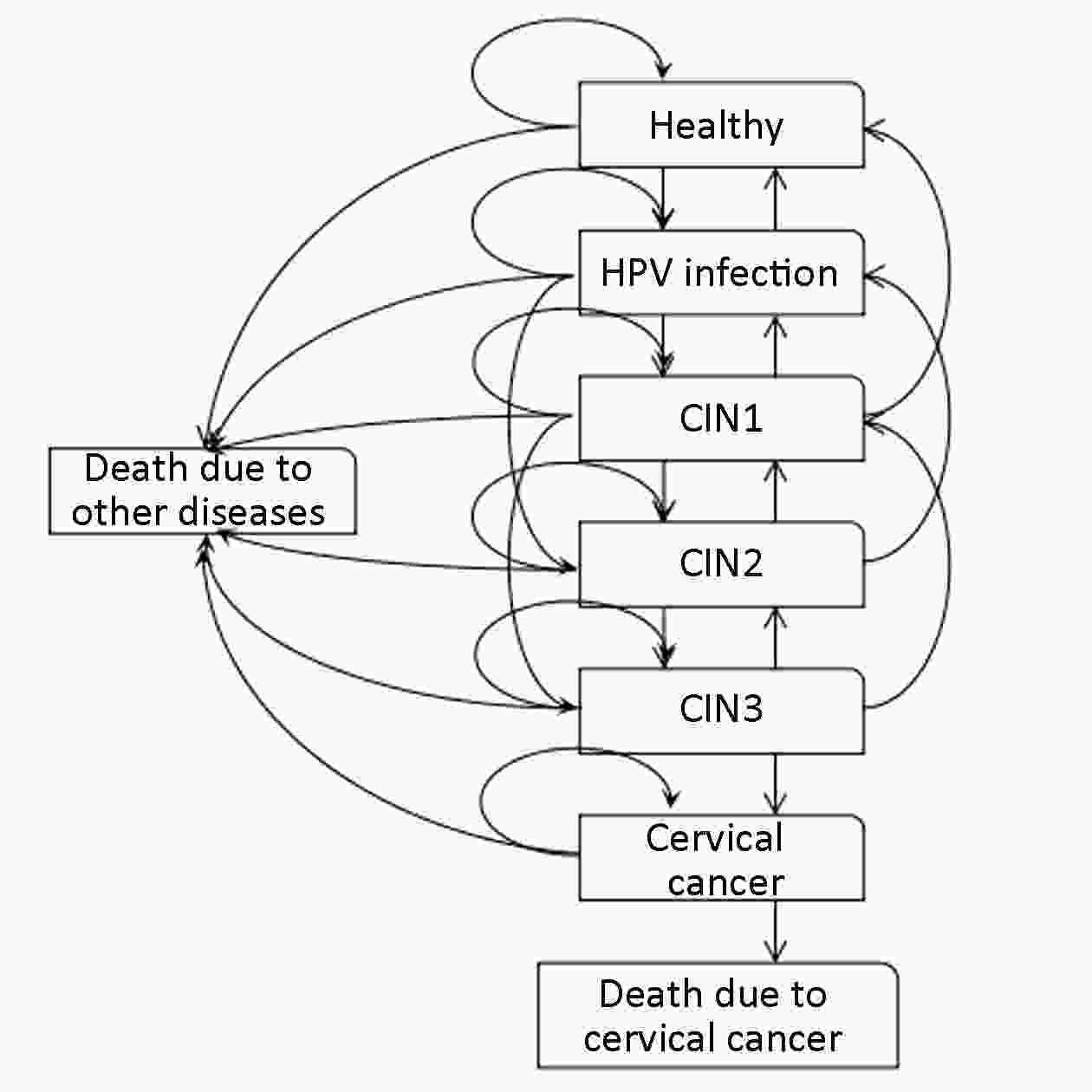
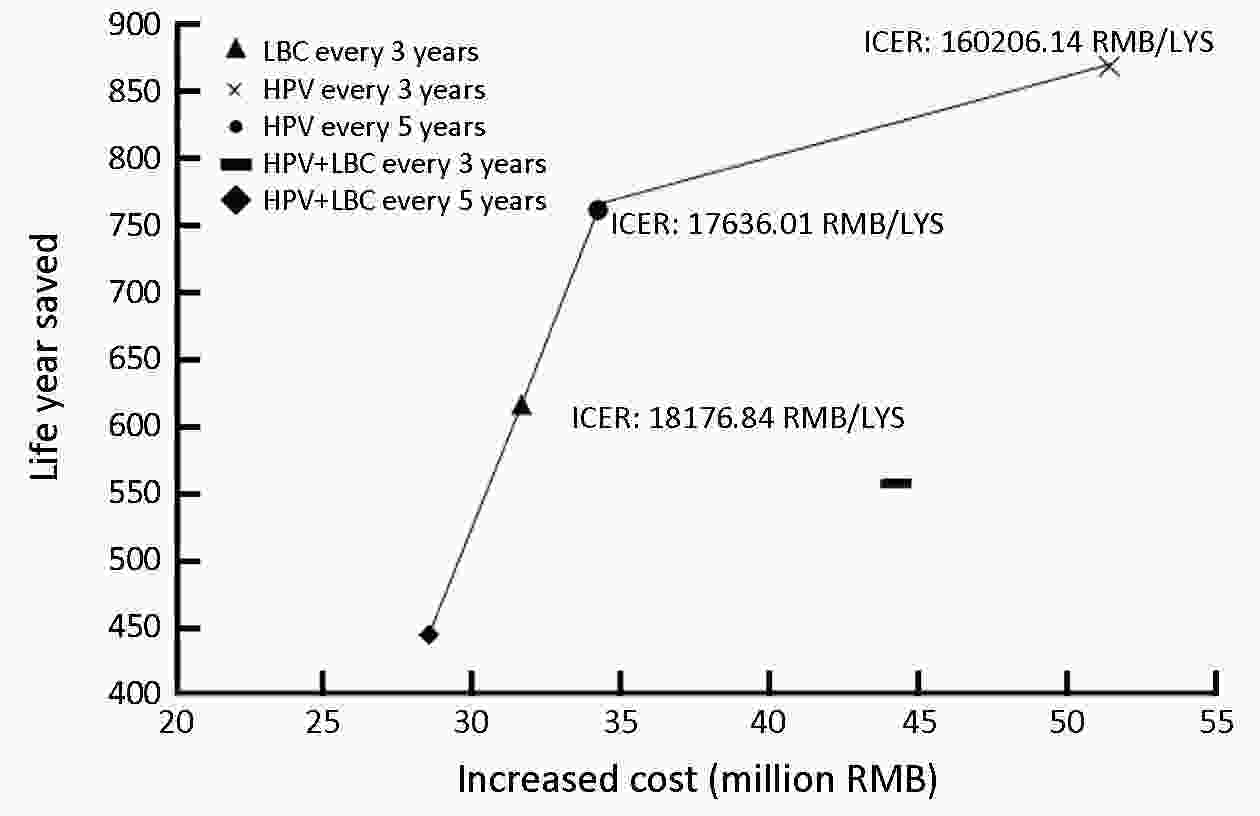
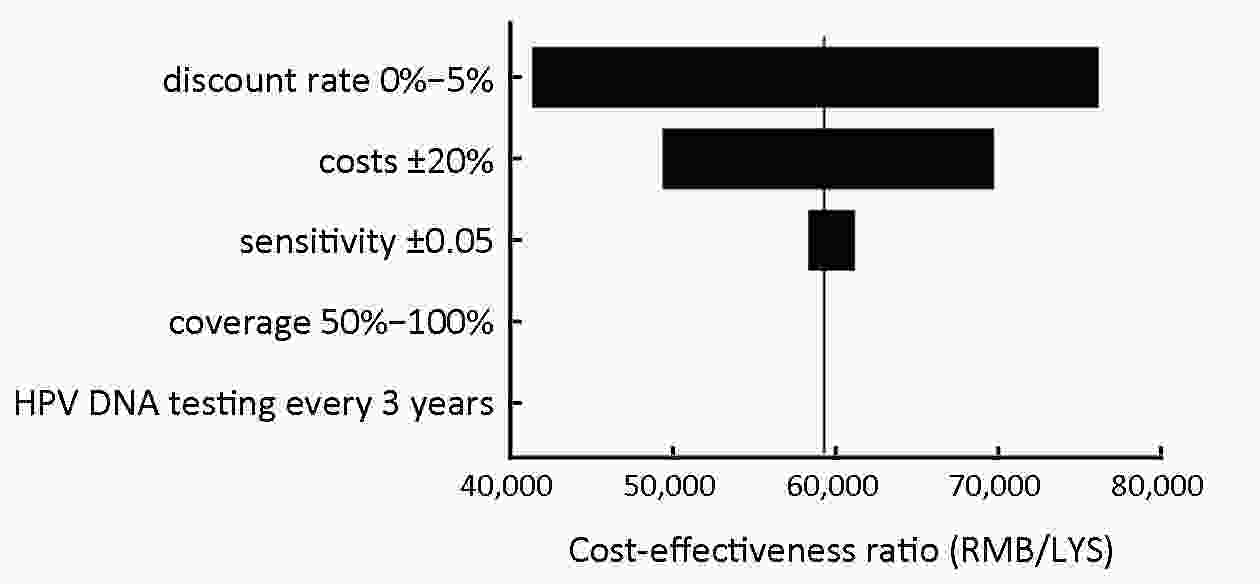
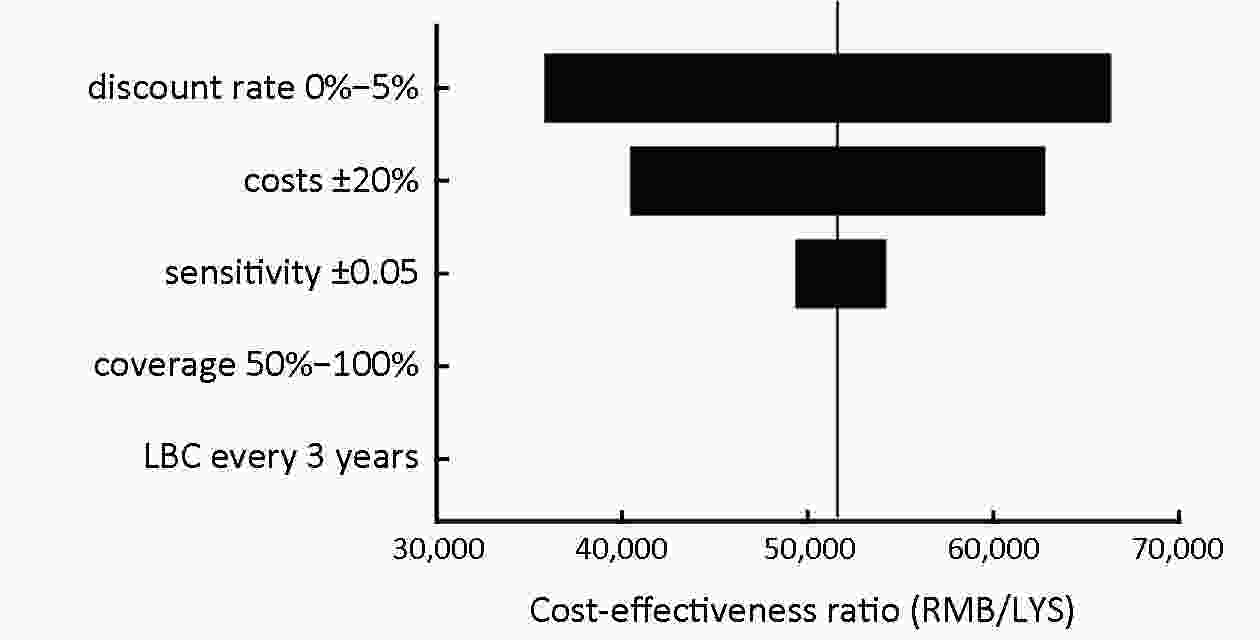
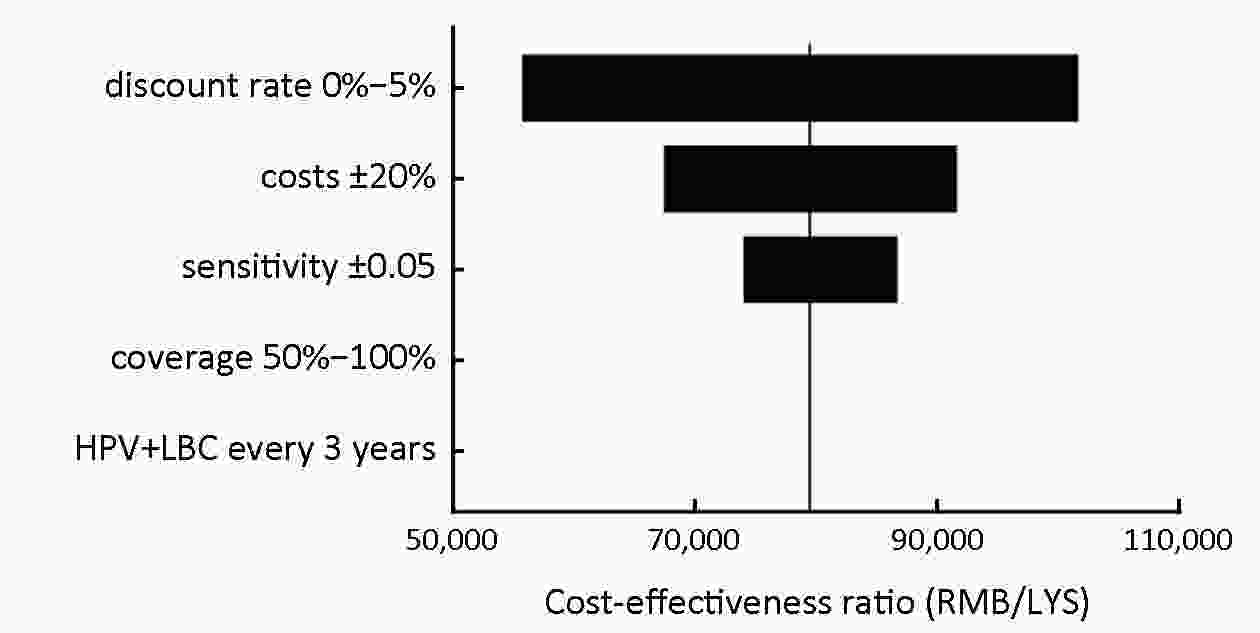
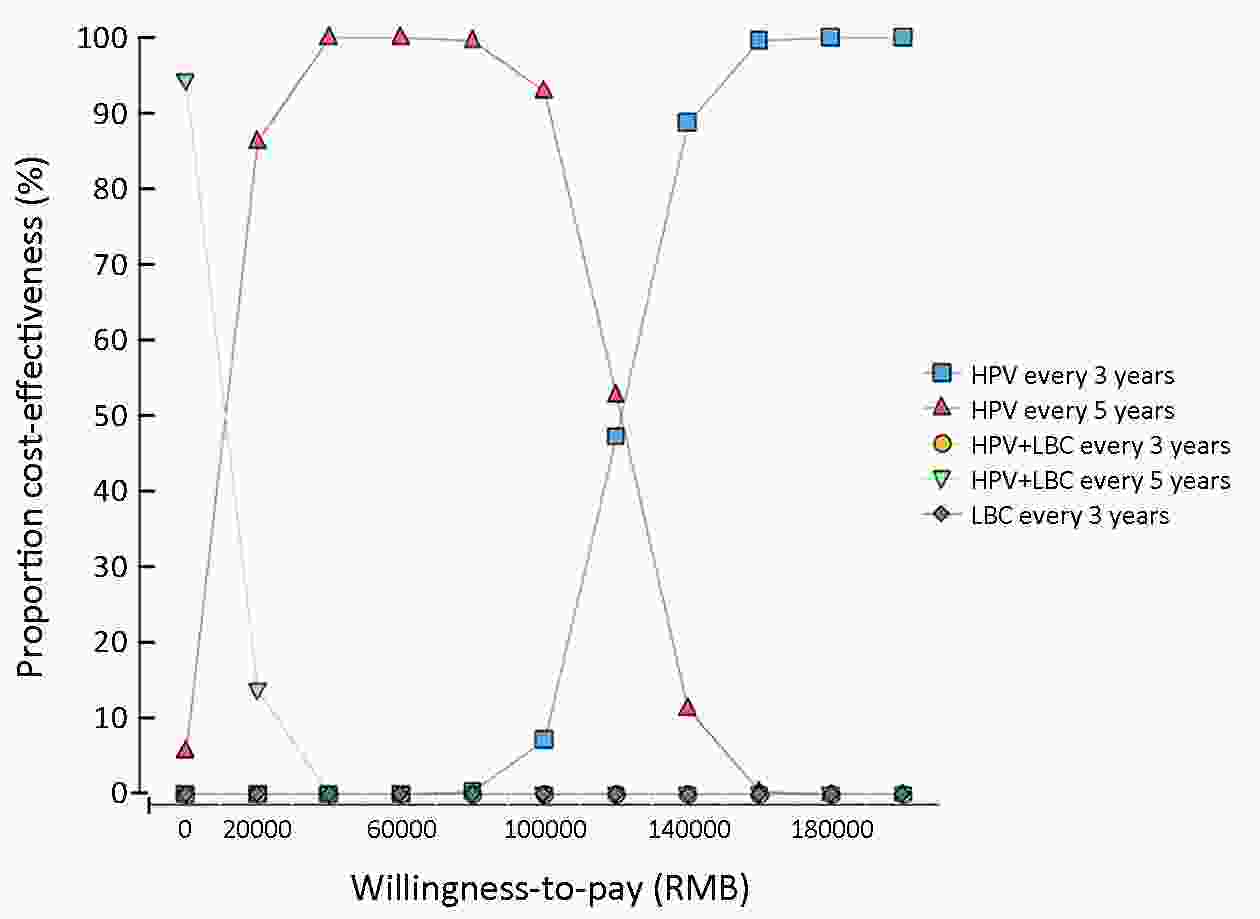
ObjectiveThis study evaluated the feasibility of different cervical cancer screening strategies in urban China. MethodsA Markov model was constructed to simulate a hypothetical cohort of 100,000 females aged 30−59 years in a 20-year period. Screening strategies included liquid-based cytology (LBC) every three years, human papillomavirus (HPV) DNA testing every three and five years, respectively, and a combination of HPV DNA testing and LBC (HPV+LBC) every three and five years, respectively. Model outcomes included cumulative incidence over 20 years, cumulative risk of cervical cancer, costs, life year saved (LYS), quality-adjusted life years (QALYs) and benefits. The cost-effectiveness ratios (CERs), incremental cost-effectiveness ratios (ICERs), cost-utility ratios (CURs), and benefit-cost ratios (BCRs) were used as outcomes in the health economic evaluation analysis. Univariate sensitivity analyses were performed to examine the stability of the results. ResultsThe cumulative incidence of the five screening strategies ranged from 833.02 to 1,158.07 cases per 100,000 females. HPV DNA testing was most effective in reducing the cumulative risk of cervical cancer, saving life years and QALYs and gaining benefits. The CERs of HPV DNA testing every three and five years, and LBC every three years were considered to be very cost-effective if they were below China’s GDP per capita. The CERs of HPV+LBC were considered to be cost-effective if they were below three times GDP per capita. The incremental cost-effectiveness analysis showed that HPV DNA testing every three and five years, LBC every three years and HPV+LBC every five years were dominant strategies. ConclusionsThe findings of this study indicated that HPV DNA testing every five years or LBC every three years should be recommended in urban China.
2019, 31(6): 984-992.
doi: 10.21147/j.issn.1000-9604.2019.06.14
Abstract:
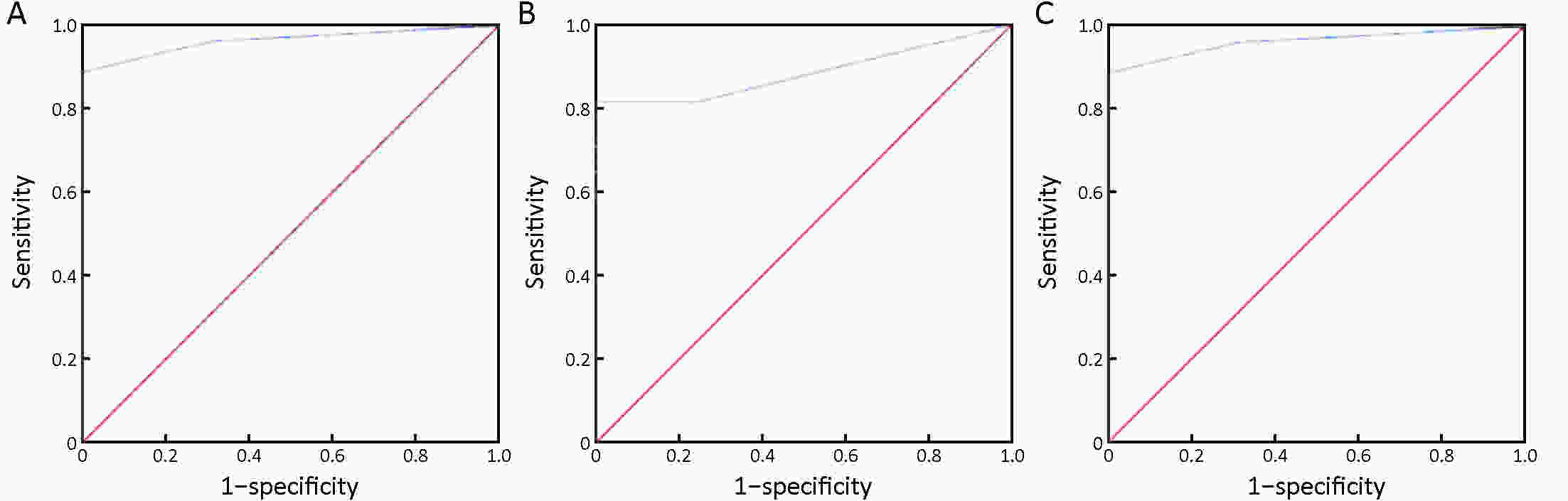
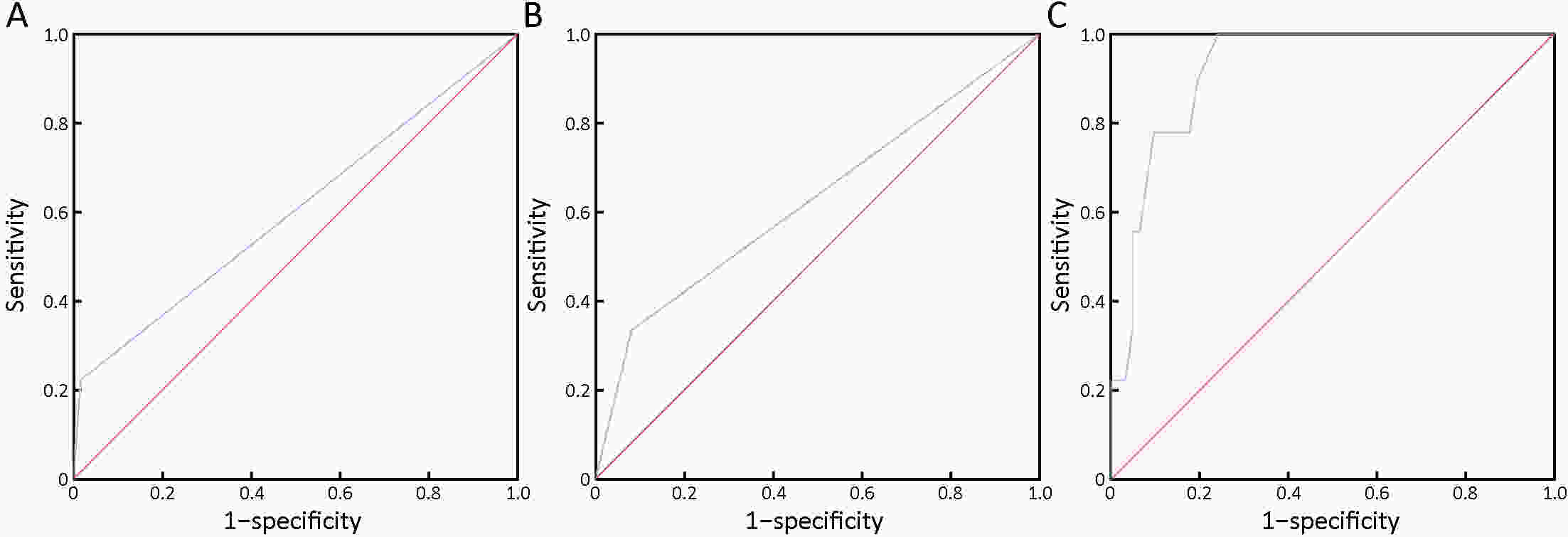
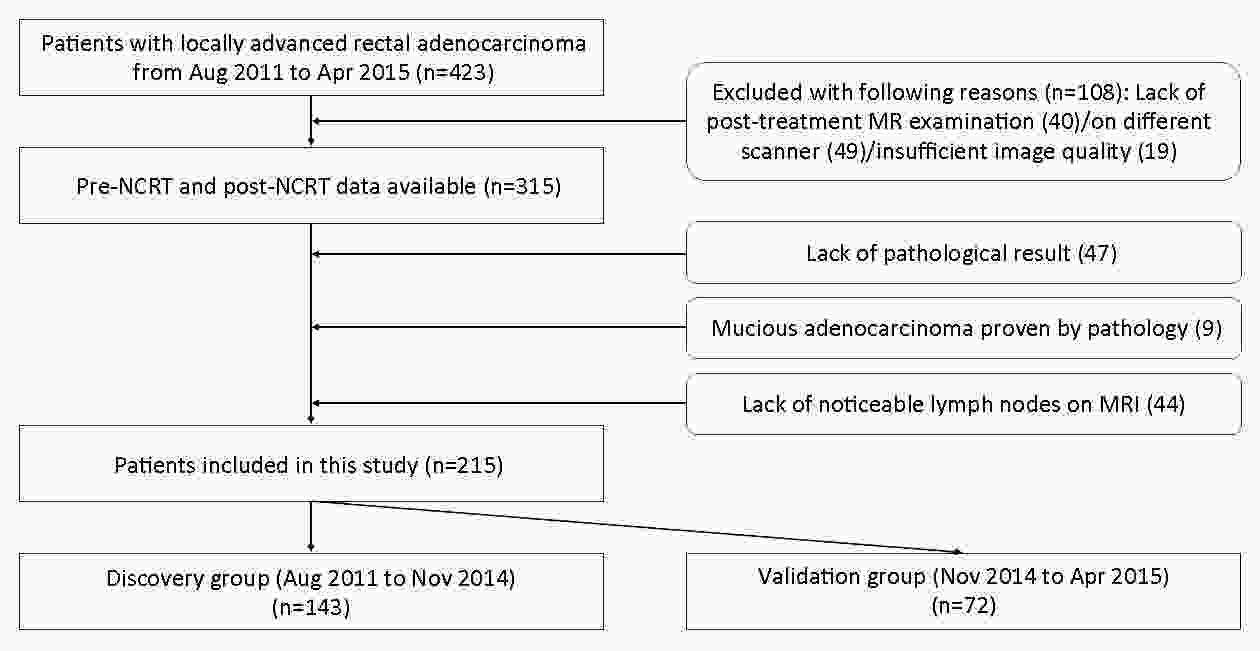
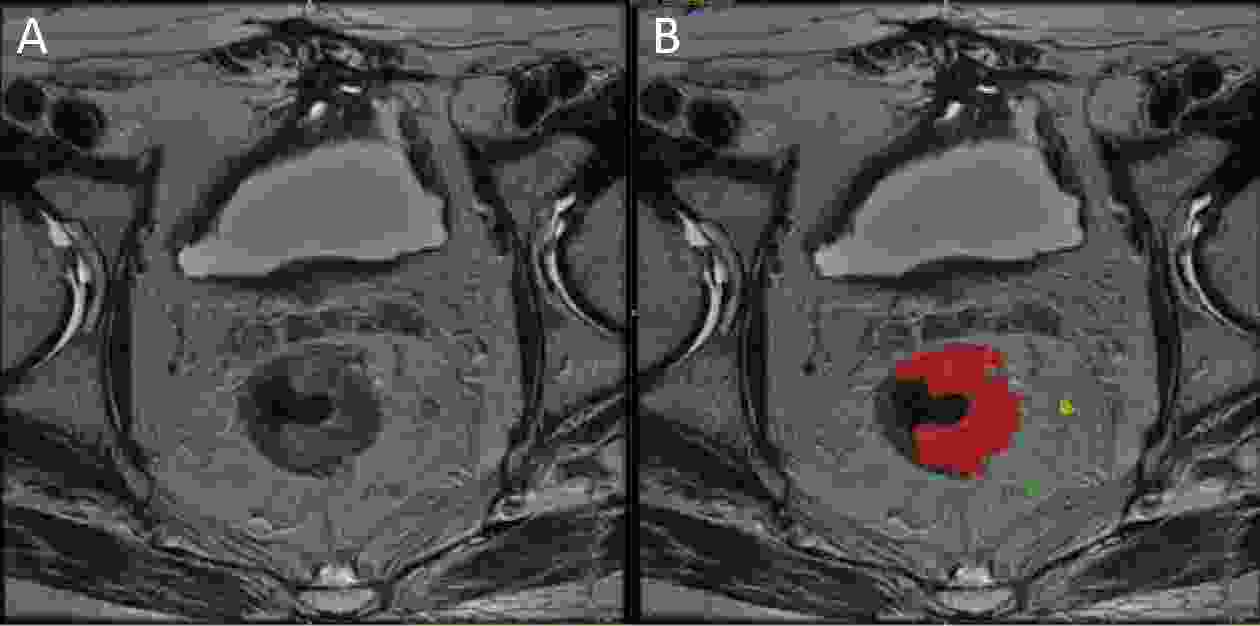
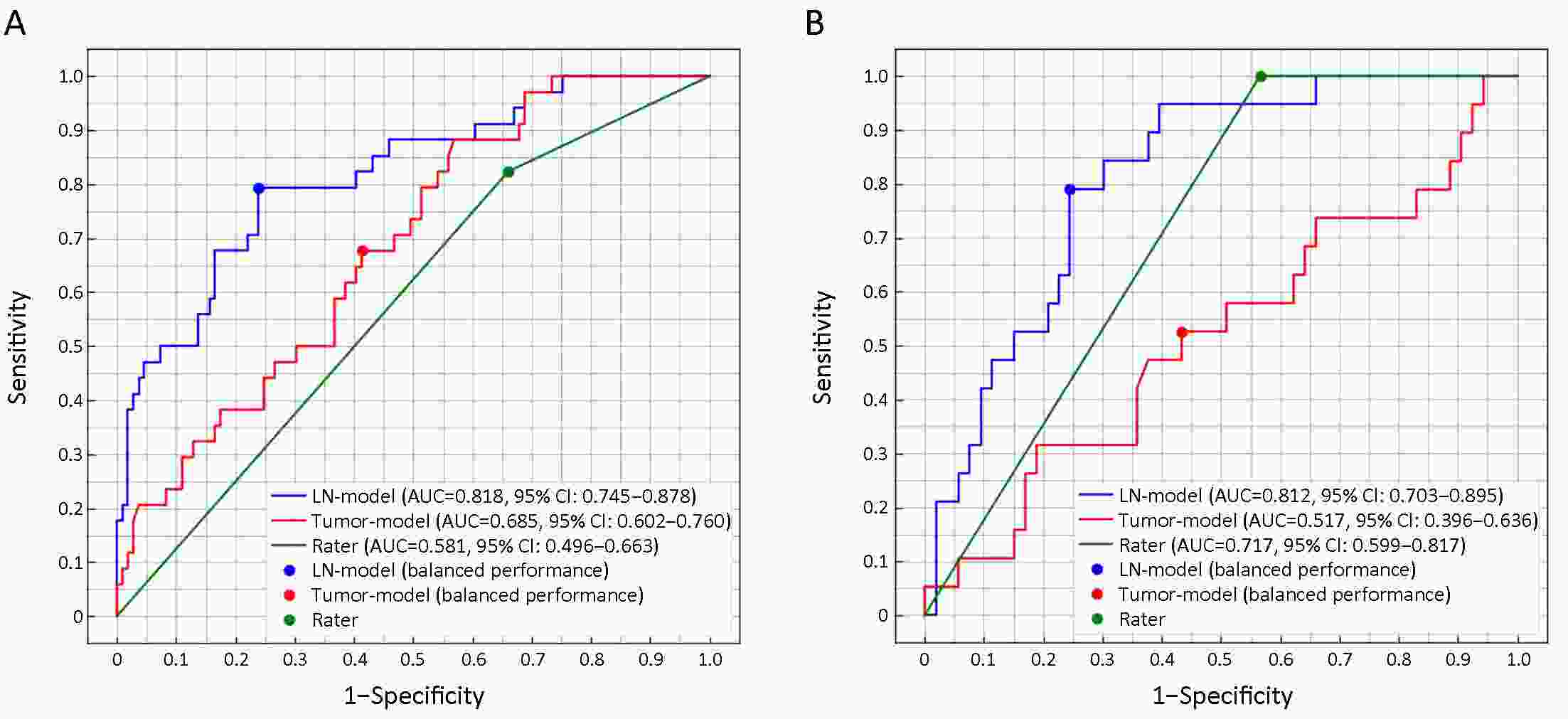
ObjectiveTo predict pathological nodal stage of locally advanced rectal cancer by a radiomic method that uses collective features of multiple lymph nodes (LNs) in magnetic resonance images before and after neoadjuvant chemoradiotherapy (NCRT). MethodsA total of 215 patients were included in this study and chronologically divided into the discovery cohort (n=143) and validation cohort (n=72). In total, 2,931 pre-NCRT LNs and 1,520 post-NCRT LNs were delineated from all visible rectal LNs in magnetic resonance images. Geometric, first-order and texture features were extracted from each LN before and after NCRT. Collective features are defined as the maximum, minimum, mean, median value and standard deviation of each feature from all delineated LNs of each participant. LN-model is constructed from collective LN features by logistic regression model with L1 regularization to predict pathological nodal stage (ypN0 or ypN+). Tumor-model is constructed from tumor features for comparison by using DeLong test. ResultsThe LN-model selects 7 features from 412 LN features, and the tumor-model selects 7 features from 82 tumor features. The area under the receiver operating characteristic curve (AUC) of LN-model in the discovery cohort is 0.818 [95% confidence interval (95% CI): 0.745−0.878], significantly (Z=2.09, P=0.037) larger than 0.685 (95% CI: 0.602−0.760) of the tumor-model. The AUC of LN-model in validation cohort is 0.812 (95% CI: 0.703−0.895), significantly (Z=3.106, P=0.002) larger than 0.517 (95% CI: 0.396−0.636) of the tumor-model. ConclusionsThe usage of collective features from all visible rectal LNs performs better than the usage of tumor features for the prediction of pathological nodal stage of locally advanced rectal cancer.

 Abstract
Abstract FullText HTML
FullText HTML PDF 118KB
PDF 118KB