2020 Vol.32(1)
Display Mode: |
2020, 32(1): 1-9.
doi: 10.21147/j.issn.1000-9604.2020.01.01
Abstract:
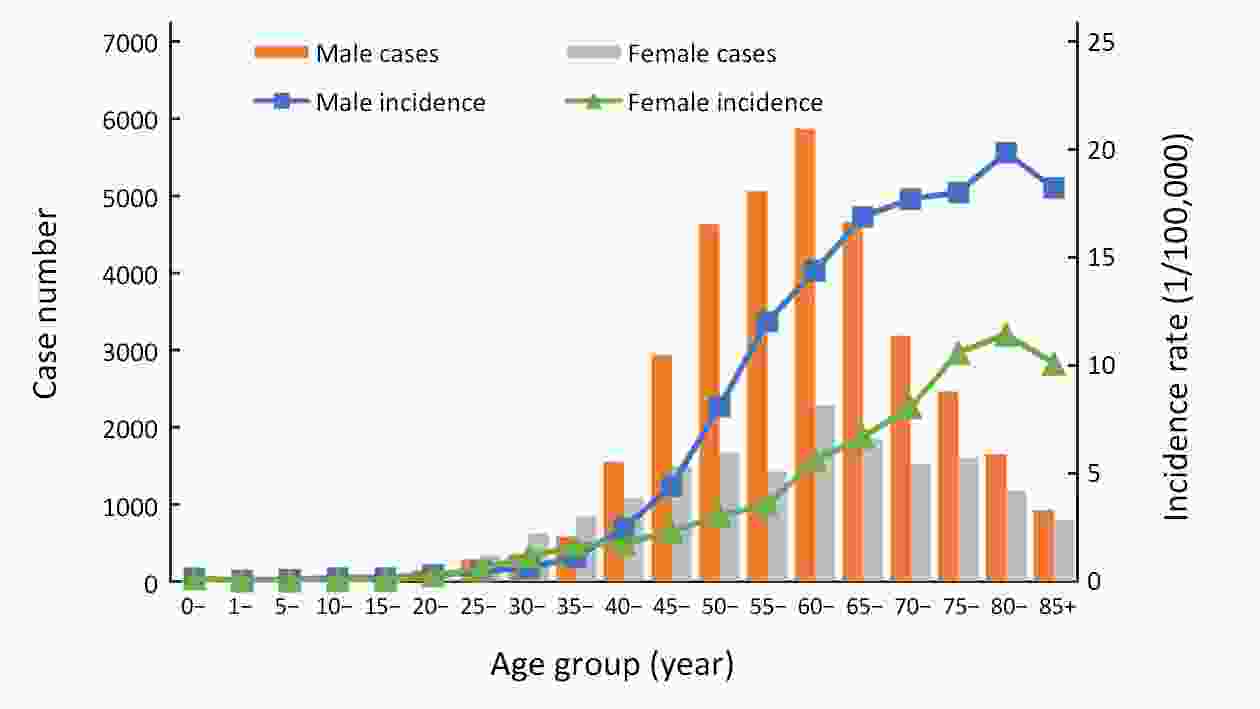
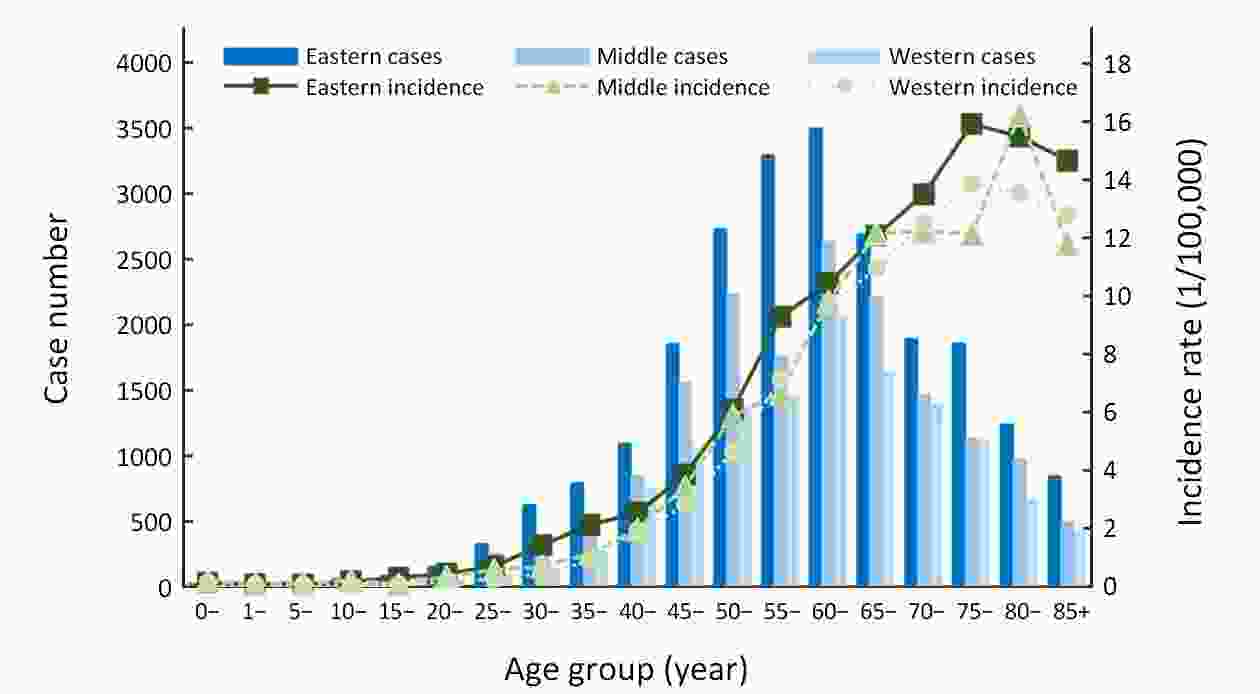
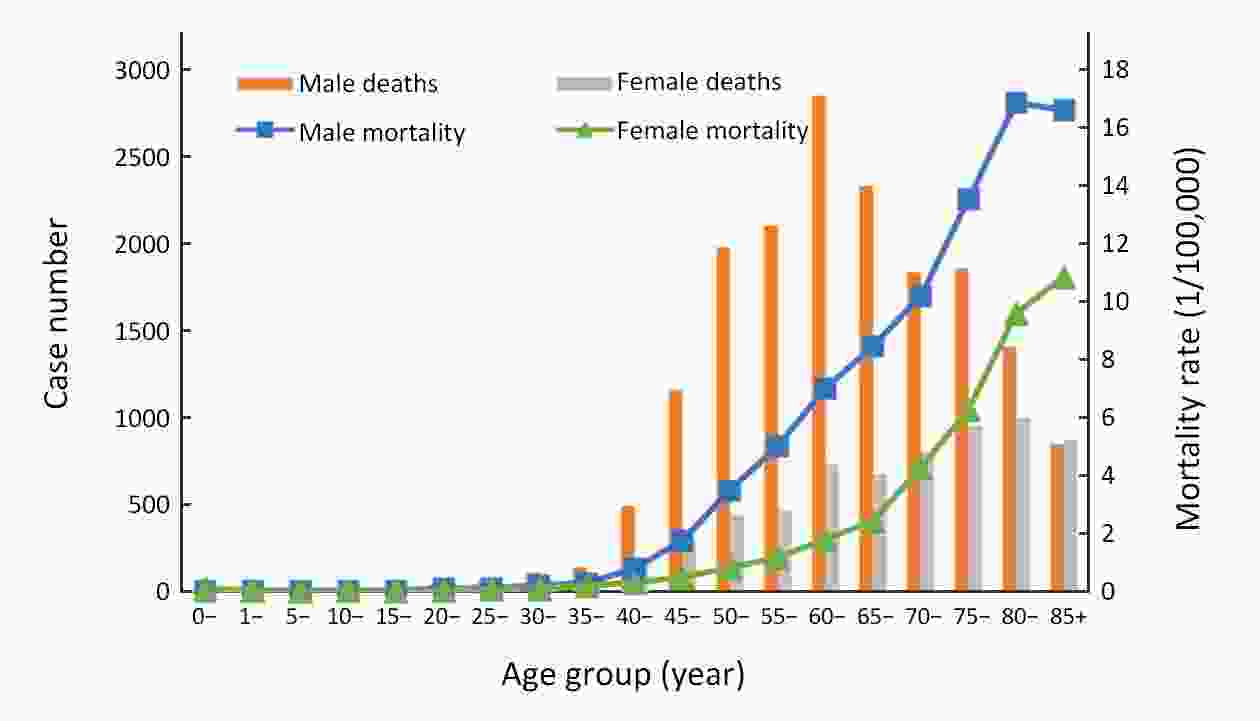
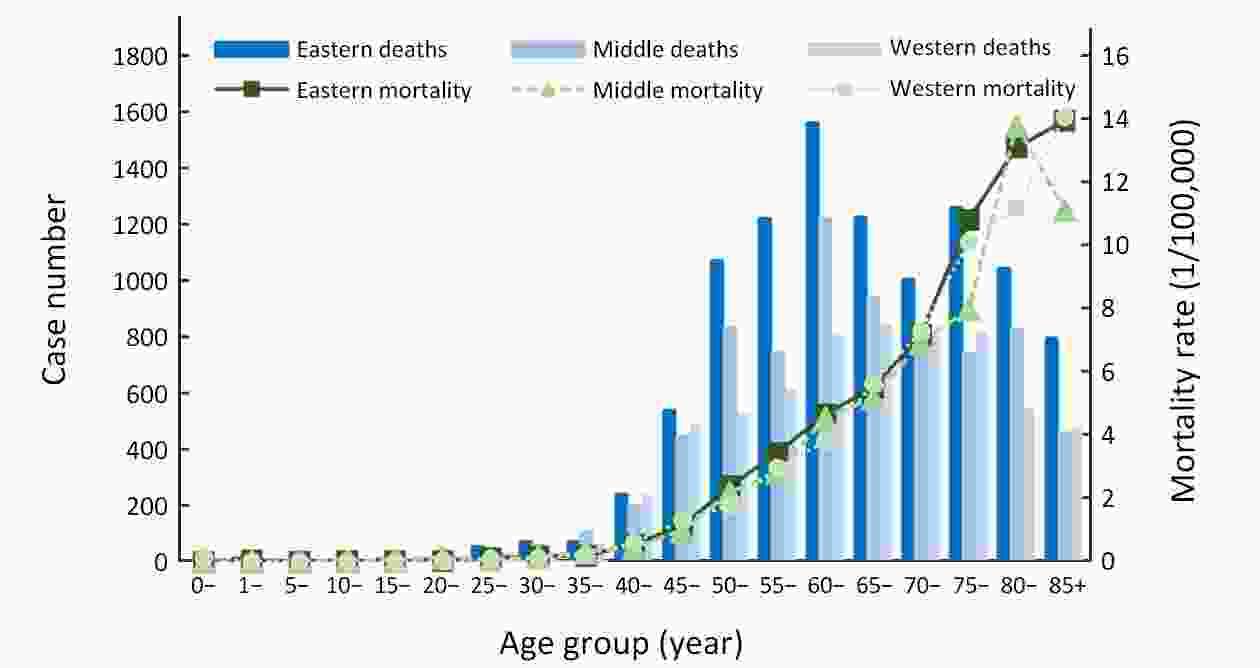
ObjectiveTo report the incidence and mortality rates of oral and oropharyngeal cancer in Chinese population. MethodsData were taken from a population-based cancer registry collected by the National Central Cancer Registry of China (NCCRC) in 2015. The data collected from 501 local cancer registries in China were assessed using NCCRC screening methods and criteria. Incidence and mortality rates of oral and oropharyngeal cancer were stratified by age group, gender, and area. Age-standardized incidence and mortality rates were adjusted using the Chinese standard population in 2000 and Segi’s world population. ResultsIn 2015, it was estimated that there were 51,765 oral and oropharyngeal cancer incident cases and 23,830 deaths in China. The crude incidence rate of oral and oropharyngeal cancer was 3.77/100,000, and the age-standardized incidence rate by Chinese standard population and by Segi’s world standard population were 2.55/100,000 and 2.49/100,000, respectively. The crude mortality rate and the age-standardized mortality rates by Chinese standard population and by Segi’s world standard population were 1.73/100,000, 1.09/100,000 and 1.08/100,000, respectively. Both incidence and mortality rates of oral and oropharyngeal cancer were higher in males and in urban areas. Residents in eastern areas had the highest incidence and mortality rates, followed by those from middle areas and western areas. The rates of oral and oropharyngeal cancer increased greatly with age, especially after the age of 40 years. ConclusionsThis study reports the latest incidence and mortality rates of oral and oropharyngeal cancer in China. Prevention intervention including early detection, treatment, and regular follow-ups is encouraged to be set up to reduce incidence and mortality rates of oral and oropharyngeal cancer in the future.
2020, 32(1): 10-17.
doi: 10.21147/j.issn.1000-9604.2020.01.02
Abstract:
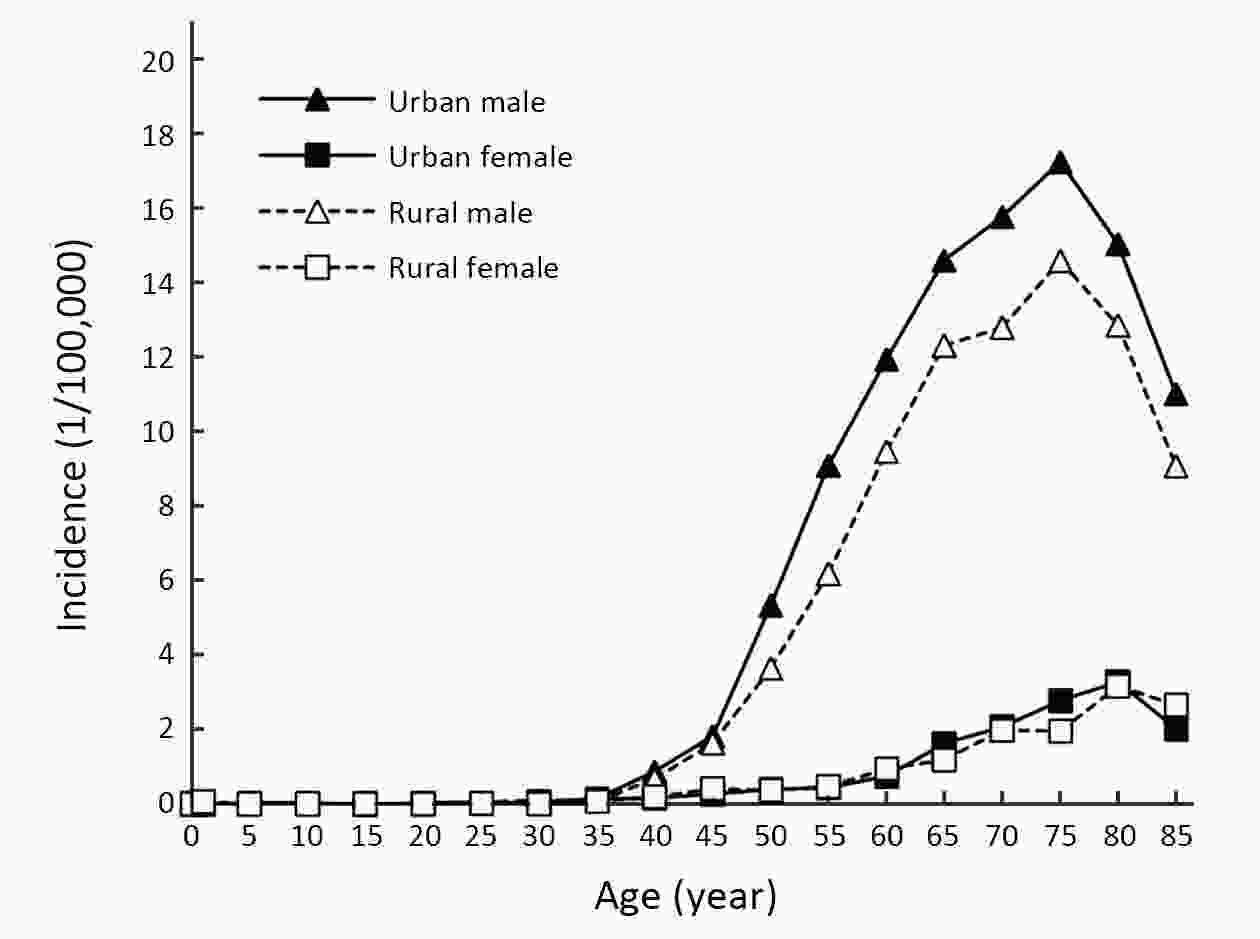
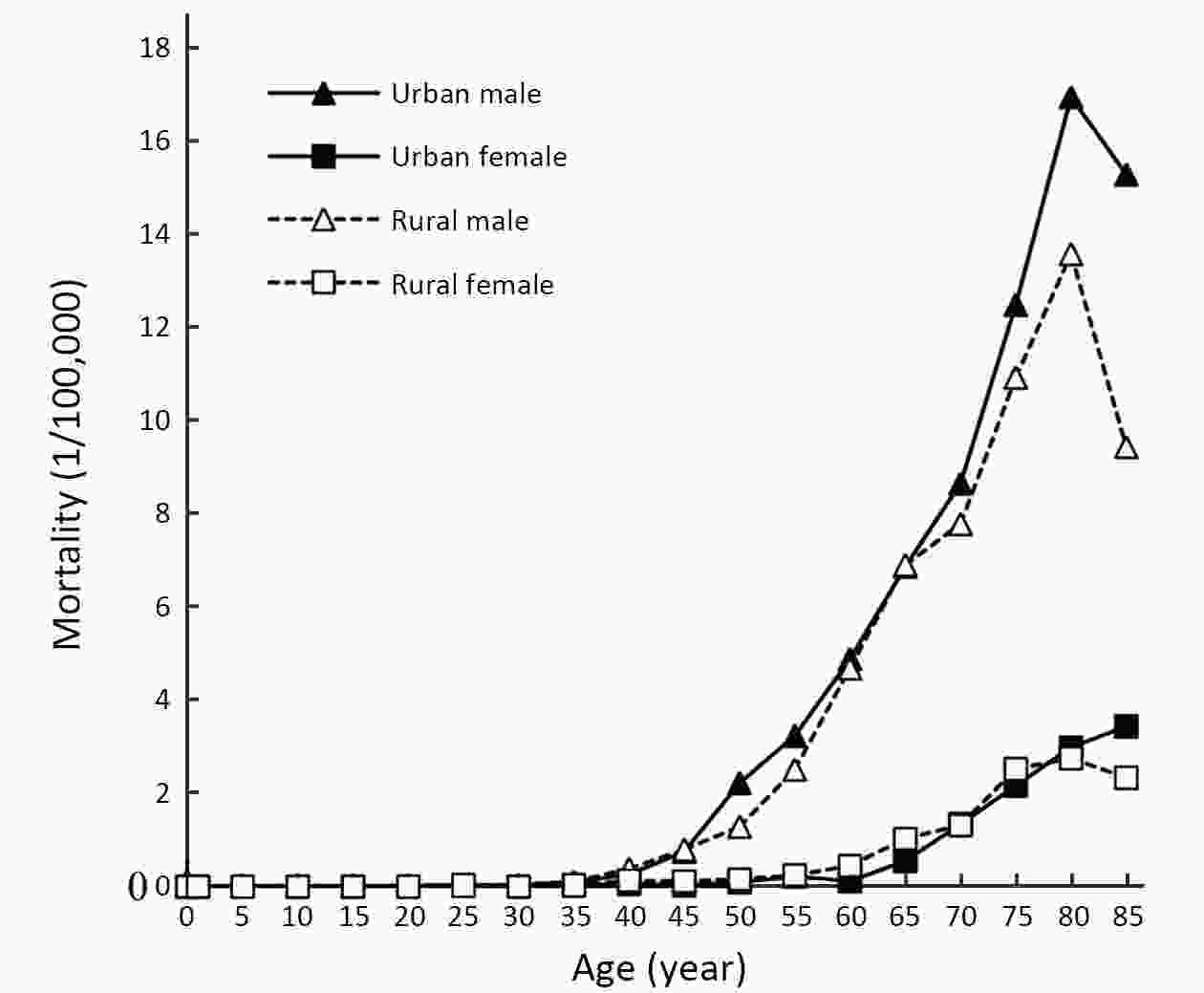
ObjectiveUsing data from cancer registries to estimate laryngeal cancer incidence and mortality in China, 2015. MethodsData submitted from 501 cancer registries were checked and evaluated according to the criteria of data quality control and 368 registries’ data were qualified for the final analysis. Data were stratified by area (urban/rural), sex, age group and combined with national population data to estimate laryngeal cancer incidence and mortality in China, 2015. China population census in 2000 and Segi’s population were used for age-standardized. ResultsThe percentage of cases morphological verified (MV%) of laryngeal cancer was 74.18%. The percentage of death certificate-only cases (DCO%) was 2.10%. And the mortality to incidence (M/I) ratio was 0.55. About 25,300 new cases of laryngeal cancer were diagnosed in 2015 and 13,700 deaths were reported. The crude rate of laryngeal cancer was 1.84 per 100,000 (males and females were 3.20 and 0.42 per 100,000, respectively). Age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 1.18 and 1.19 per 100,000, respectively. The cumulative incidence rate (0−74 years old) was 0.15%. The crude mortality rate was 1.00 per 100,000. Age-standardized mortality rates by Chinese standard population (ASMRC) and by world standard population (ASMRW) were 0.61 and 0.61 per 100,000, respectively, with the cumulative rate (0−74 years old) was 0.07%. Incidence and mortality of laryngeal cancer in males were higher than those in females. And the rates in urban areas were higher than those in rural areas. ConclusionsThe incidence and mortality of laryngeal cancer in China were low. And the rates were significantly higher in males than in females. Risk factor control and targeted prevention should be strengthened.
2020, 32(1): 18-25.
doi: 10.21147/j.issn.1000-9604.2020.01.03
Abstract:
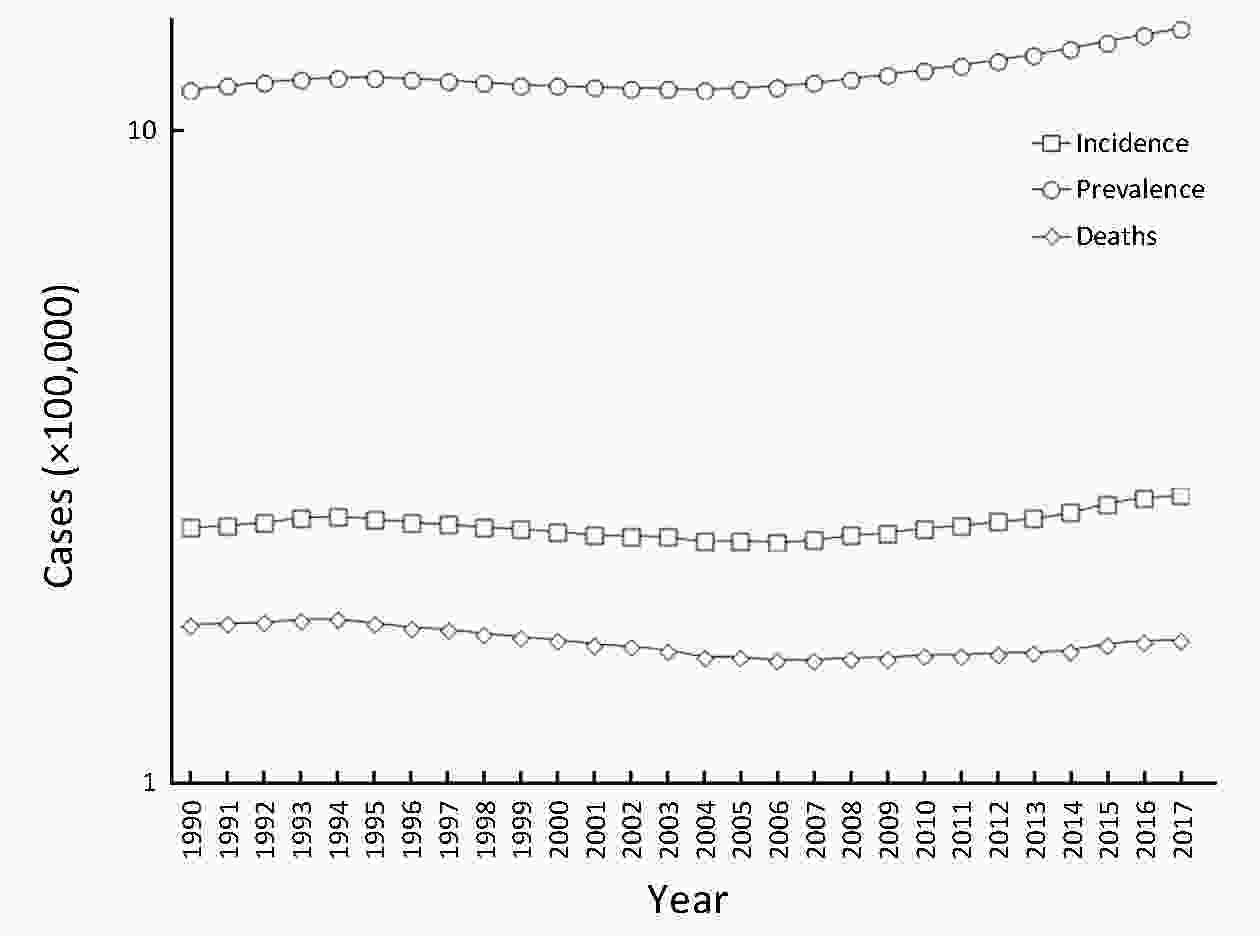
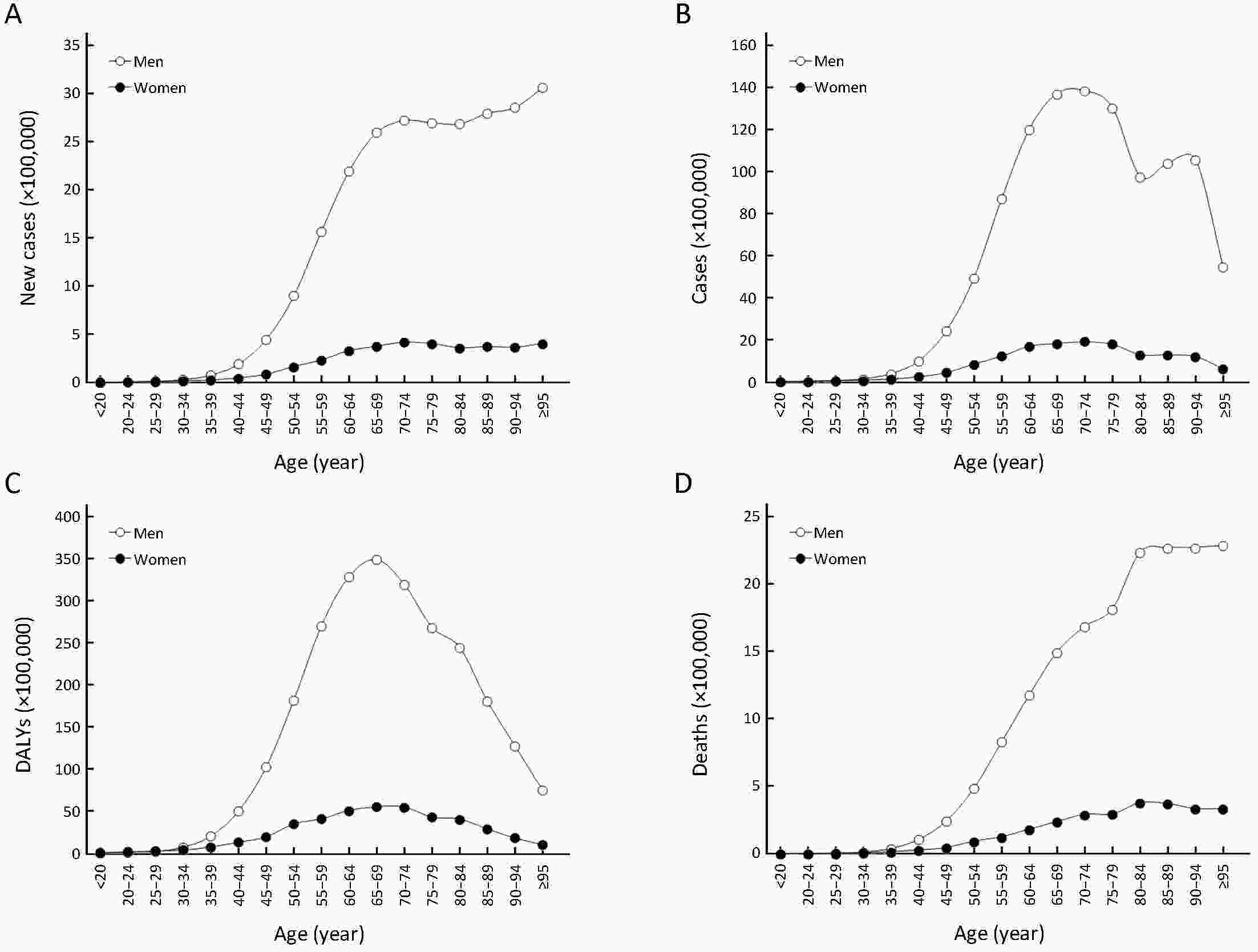
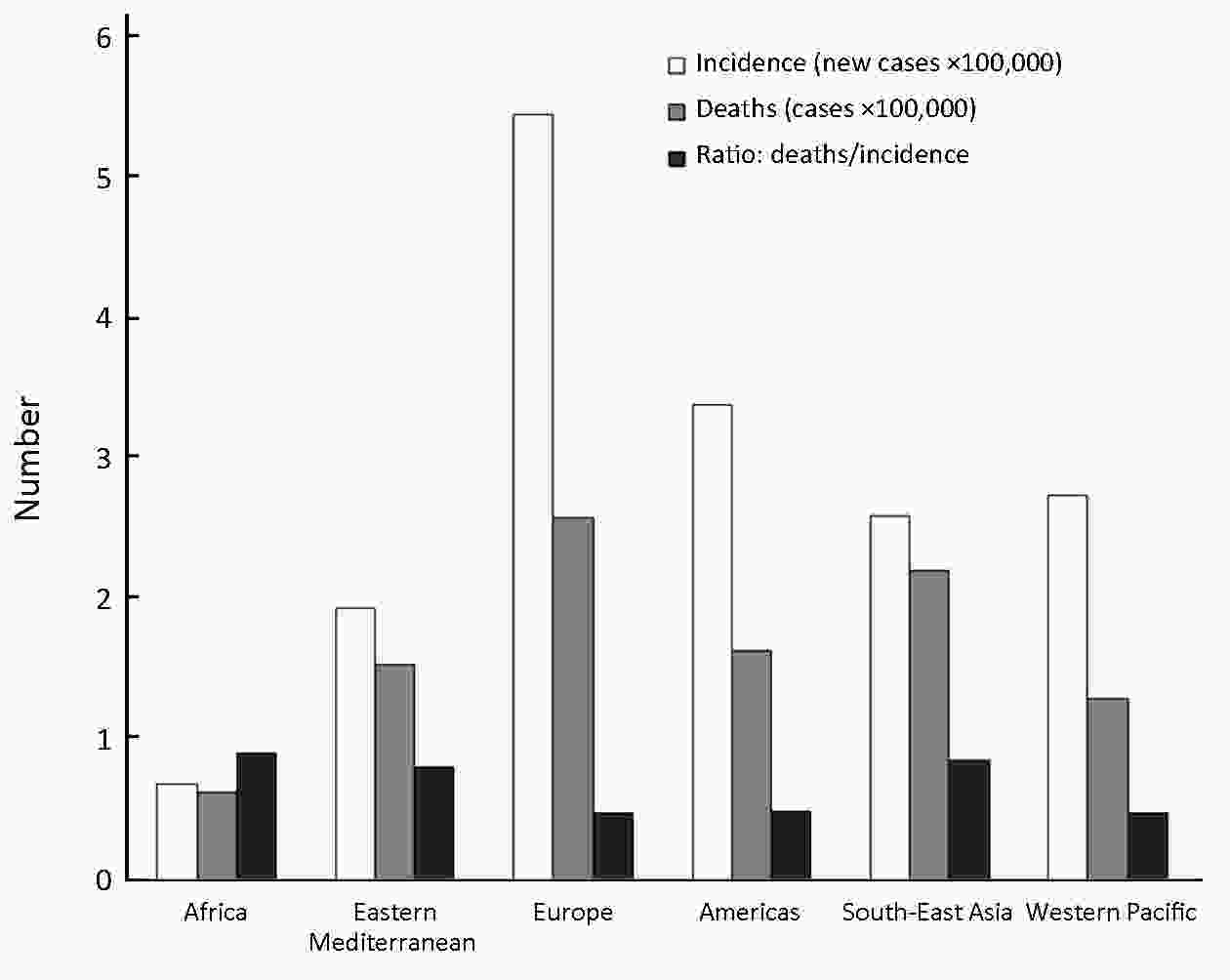
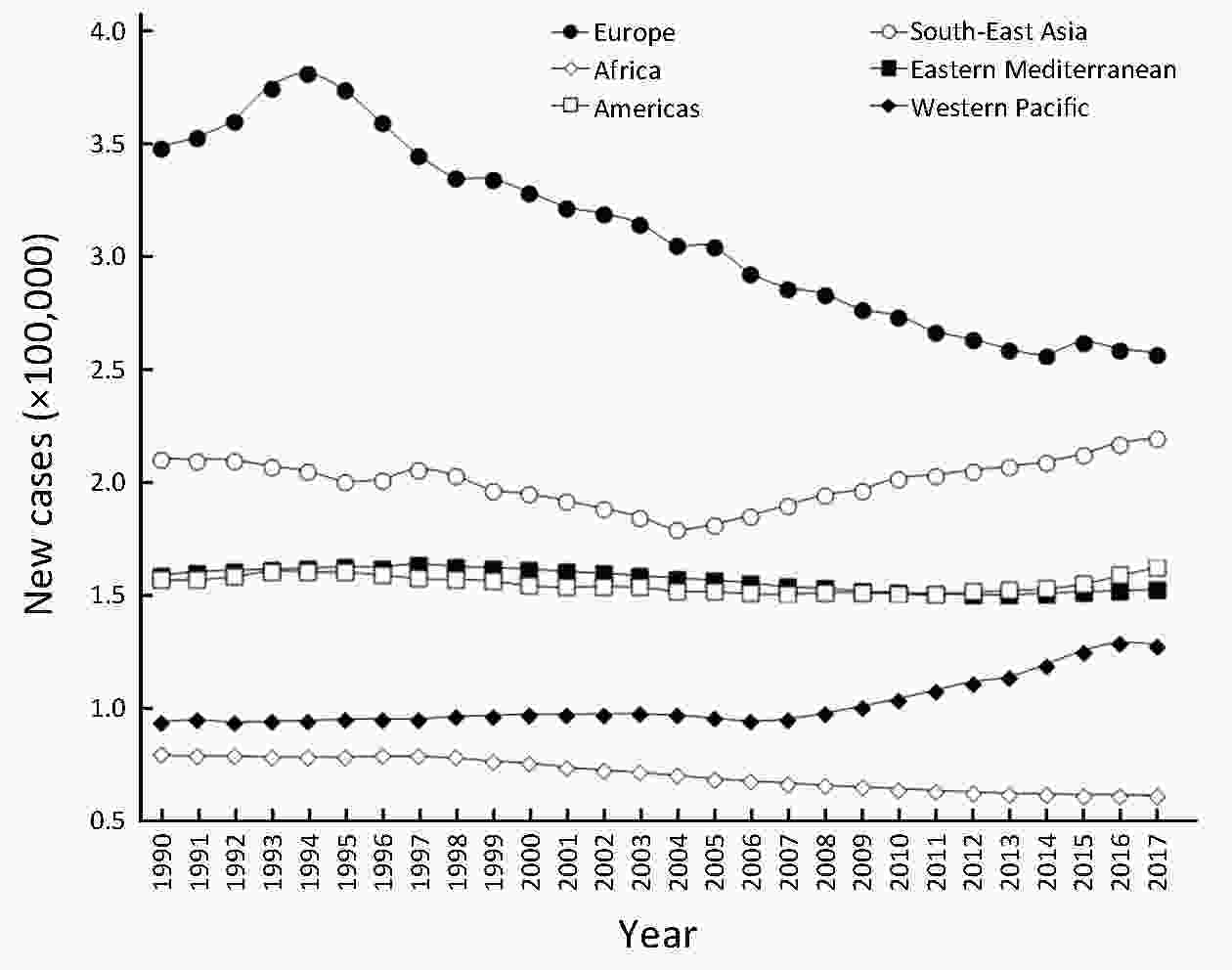
ObjectiveLaryngeal cancer is an important oncologic entity, whose prognosis depends on establishing appropriate preventive and diagnostic measures, especially in populations at higher risk. MethodsEpidemiologic information including worldwide incidence, prevalence, burden of health loss (disability-adjusted life year; DALYs) and mortality of larynx cancer was obtained from the Global Health Data Exchange (GHDx) database. ResultsThe current incidence, prevalence and mortality of laryngeal cancer are estimated at 2.76 cases/year per 100,000 inhabitants, 14.33 cases/year per 100,000 inhabitants and 1.66 deaths/year per 100,000 inhabitants, respectively, averaging 3.28 million DALYs each year. Incidence and prevalence have increased by 12% and 24%, respectively during the past 3 decades, whilst mortality has declined by around 5%. The epidemiologic burden of this malignancy is approximately 5-fold higher in males and increases in parallel with ageing, peaking after 65 years of age. Both incidence and mortality rates are higher in Europe and lower in Africa, but the ratio between deaths and incidence is the highest in Africa. Incidence has gradually declined in Europe during the past 3 decades, whilst it has increased in South-East Asia and Western Pacific. Cigarette smoking and alcohol abuse contribute for about 90% of overall worldwide mortality for laryngeal cancer. ConclusionsLaryngeal cancer still poses a high clinical and societal burden, with an escalating temporal trend not expected to reverse soon.
2020, 32(1): 26-35.
doi: 10.21147/j.issn.1000-9604.2020.01.04
Abstract:
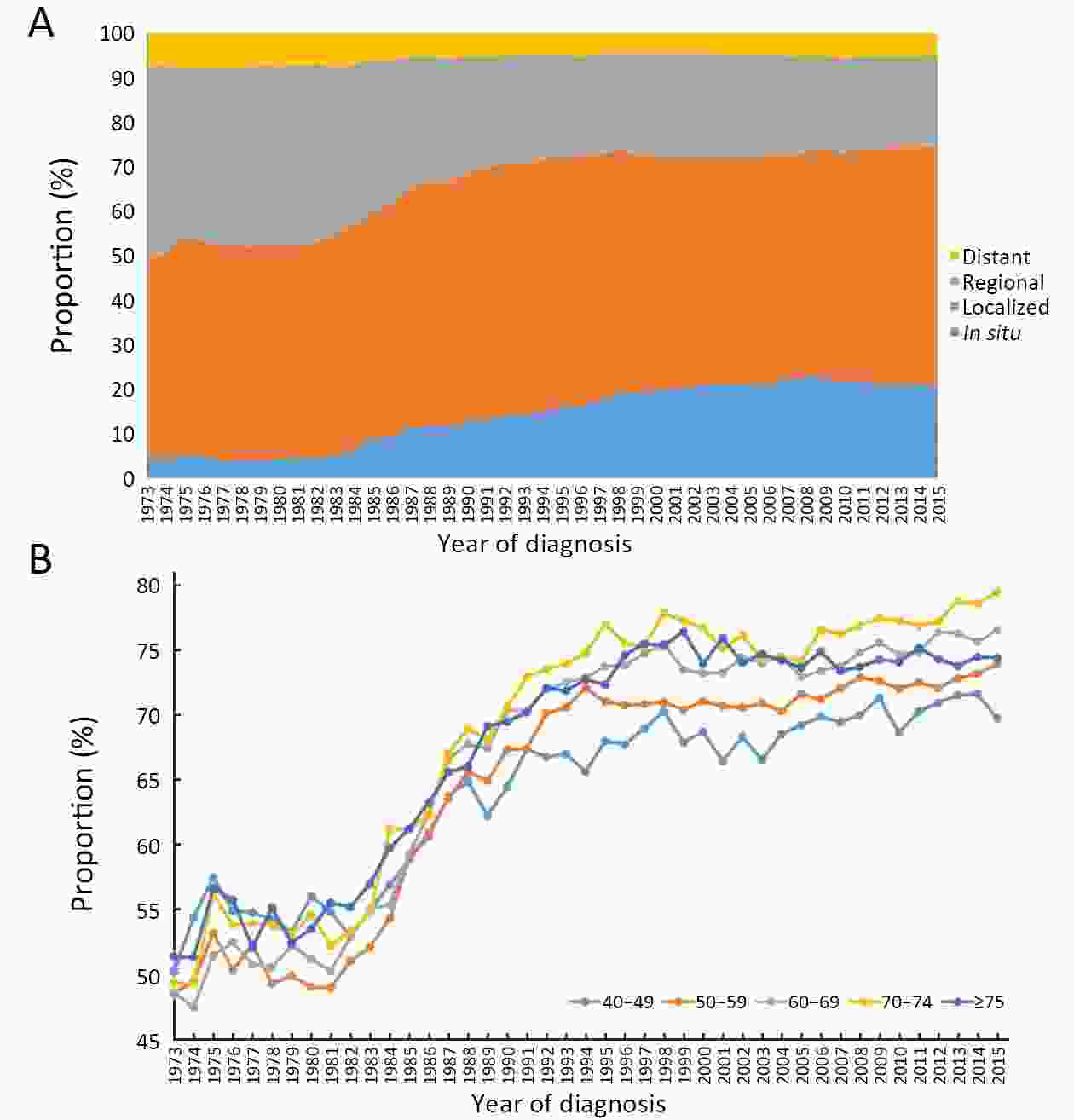
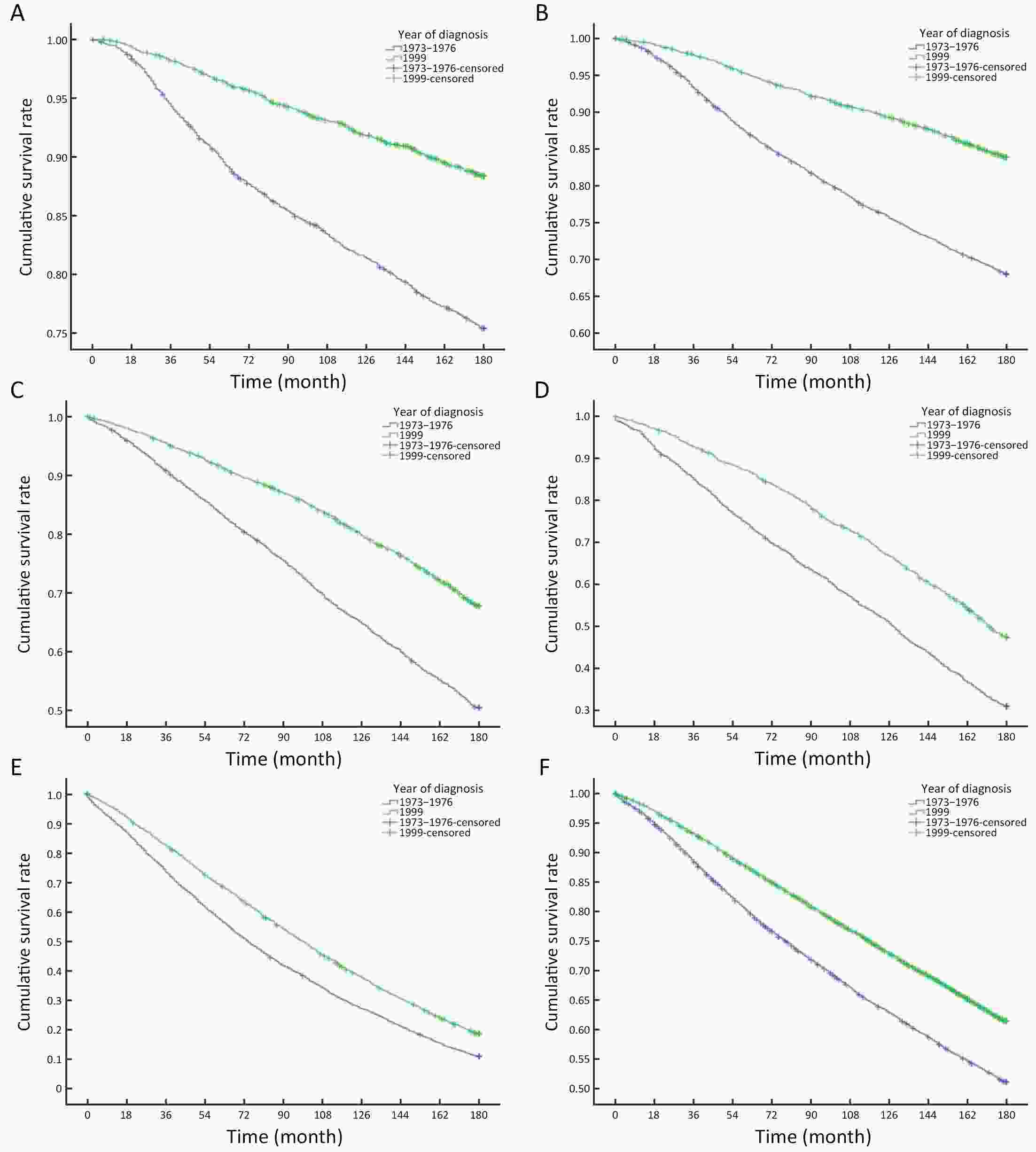
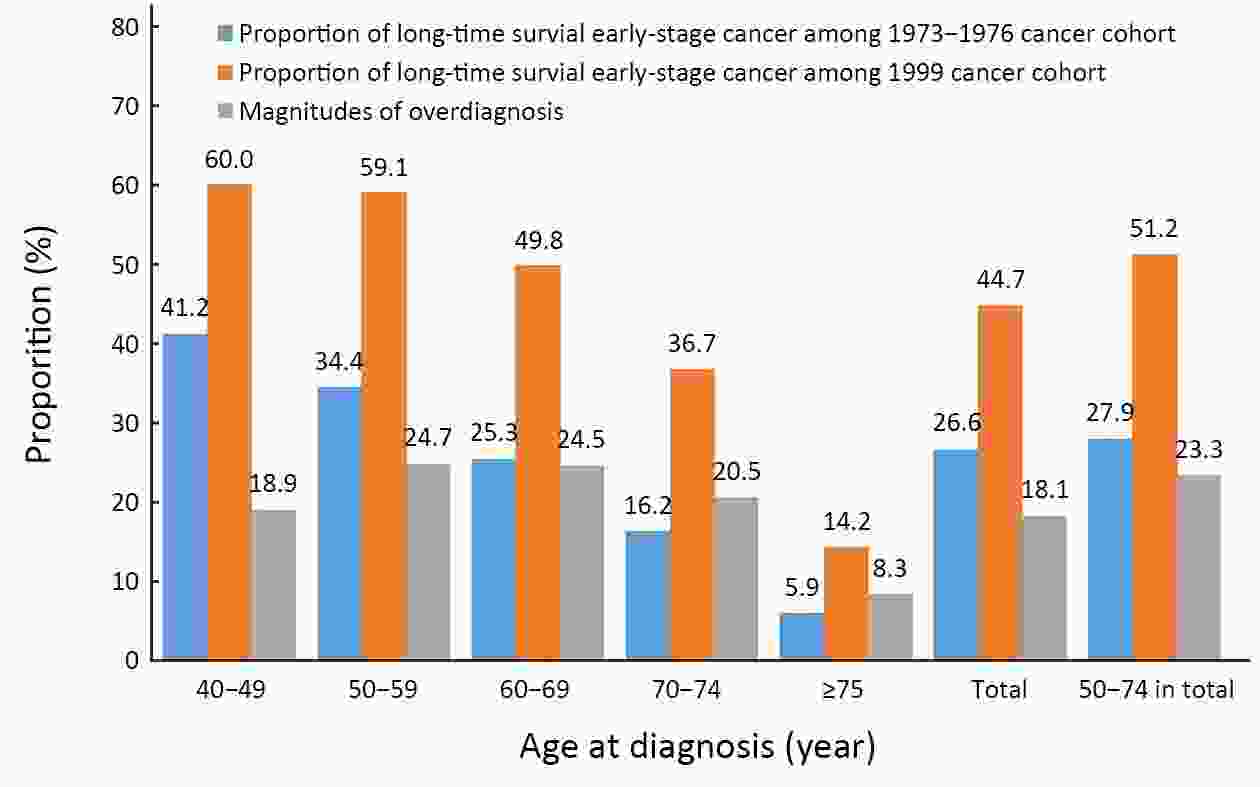
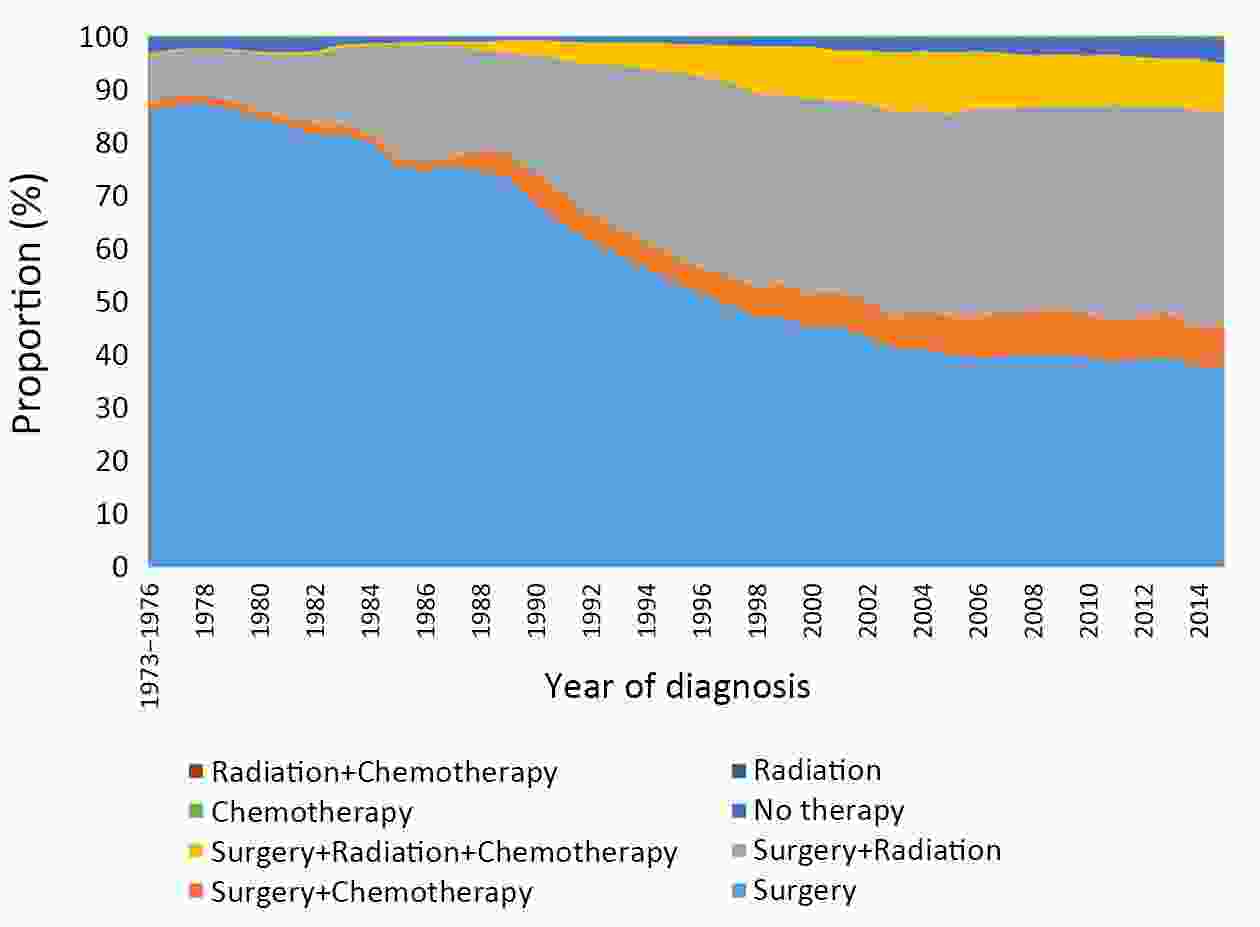
ObjectiveTo redefine overdiagnosis and reestimate the proportion of overdiagnosis of breast cancer caused by screening based on the Surveillance, Epidemiology, and End Results (SEER, 1973−2015) Program data. MethodsThe breast cancer diagnosed before 1977 was defined as the no-screening cohort since America had initiated breast cancer screening from 1977. The breast cancer diagnosed in 1999 was defined as the screening cohort due to no increases in both the proportion of early-stage breast cancer until 1999 and the overall survival of early-stage breast cancer diagnosed over the three years since 1999. The magnitude of overdiagnosis was calculated as the difference in the proportions of early-stage breast cancer patients with long-time (15-year) survival to all breast cancer patients between two cohorts. ResultsOver 23 years before and after widespread screening in America, the proportion of early-stage breast cancer patients increased from 52.1% (16,891/32,443) to 72.7% (16,021/22,025) (P<0.001). The 15-year survival rate of early-stage breast cancer patients increased from 51.1% to 61.5% (P<0.001), while the proportions of early-stage breast cancer patients with long-time survival to all breast cancer patients increased from 26.6% (52.1%×51.1%) to 44.7% (72.7%×61.5%). Assuming no improvements in cancer screening technology and treatment technology, 18.1% (44.7%−26.6%) of breast cancer patients were overdiagnosed associated with screening. The age-specific overdiagnosis rates were 18.9%, 24.7%, 24.5%, 20.5%, and 8.3% for breast cancer patients aged 40−49, 50−59, 60−69, 70−74, and ≥75 years old, respectively. ConclusionsOverdiagnosis caused by mammographic screening is probably overestimated in current screening practices. Further trials with more sophisticated designs and analyses are needed to validate our findings in the future.
2020, 32(1): 36-42.
doi: 10.21147/j.issn.1000-9604.2020.01.05
Abstract:
ObjectiveTo evaluate changes in chest X-rays, pulmonary function tests (PFTs) and quality of life in female breast cancer patients who had been treated with four cycles of neoadjuvant chemotherapy consisting of a regimen of cyclophosphamide, epirubicin and 5-fluorouracil (CEF regimen), and to determine the correlation between pulmonary function parameters and declined quality of life. MethodsTwenty-nine eligible female patients diagnosed with breast cancer at the first visit who were 20−60 years old, were classified as the American Society of Anesthesiologists (ASA) I−II and patients whose body mass index (BMI) <30 kg/m2 were recruited and subjected to chest X-ray examinations, PFTs and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire C30 (EORTC QLQ-C30) questionnaire before and after receiving 4 cycles of the CEF regimen. ResultsIn this study, chest X-rays showed no abnormal changes after chemotherapy, but significant decreases in carbon monoxide diffusing capacity (DLCO) and percentage of the DLCO predicted value (DLCO%) (P<0.001). A significant increase in maximal ventilatory volume (MVV) (P=0.004) was observed, and most patients experienced dyspnea (P=0.031) and fatigue (P<0.001). However, there was no significant correlation between the changes in these PFTs parameters and the results of the EORTC QLQ-C30 (P>0.05). ConclusionsNeoadjuvant chemotherapy can reduce lung diffusion function and quality of life in females with breast cancer.
2020, 32(1): 43-50.
doi: 10.21147/j.issn.1000-9604.2020.01.06
Abstract:
ObjectiveThe revised Japanese treatment guideline for gastric cancer recommends dissection of the superior mesenteric vein lymph node (No. 14v LN) if there is metastasis in infrapyloric lymph node (No. 6 LN). However, it is still controversial whether LN dissection is necessary. The aim of this study was to investigate the factors associated with metastasis in No. 14v LN. MethodsPatients who underwent D2 lymphadenectomy between 2003 and 2010 were included. We excluded patients who underwent total gastrectomy, had multiple lesions, or had missing data about the status of metastasis in the LNs that were included in D2 lymphadenectomy. Clinicopathologic characteristics and the metastasis in regional LNs were compared between patients with No. 14v LN metastasis (14v+) and those without (14v−). ResultsFive hundred sixty patients were included in this study. Univariate analysis showed that old age, larger tumor size, tumor location, differentiation, lymphatic invasion, venous invasion, perineural invasion, T classification, and N classification were related to metastasis in No. 14v LN. Multivariate analysis showed differentiation (P=0.027) and N classification (P<0.001) were independent related factors. Metastasis in infrapyloric lymph node (No. 6 LN) and proxiaml splenic lymph node (No. 11p LN) was independently associated with metastasis in No. 14v LN. ConclusionsDifferentiation and N classification were independent factors associated with No. 14v LN metastasis, and No. 6 and No. 11p LN metastasis were independent risk factors for No. 14v LN metastasis.
2020, 32(1): 51-61.
doi: 10.21147/j.issn.1000-9604.2020.01.07
Abstract:
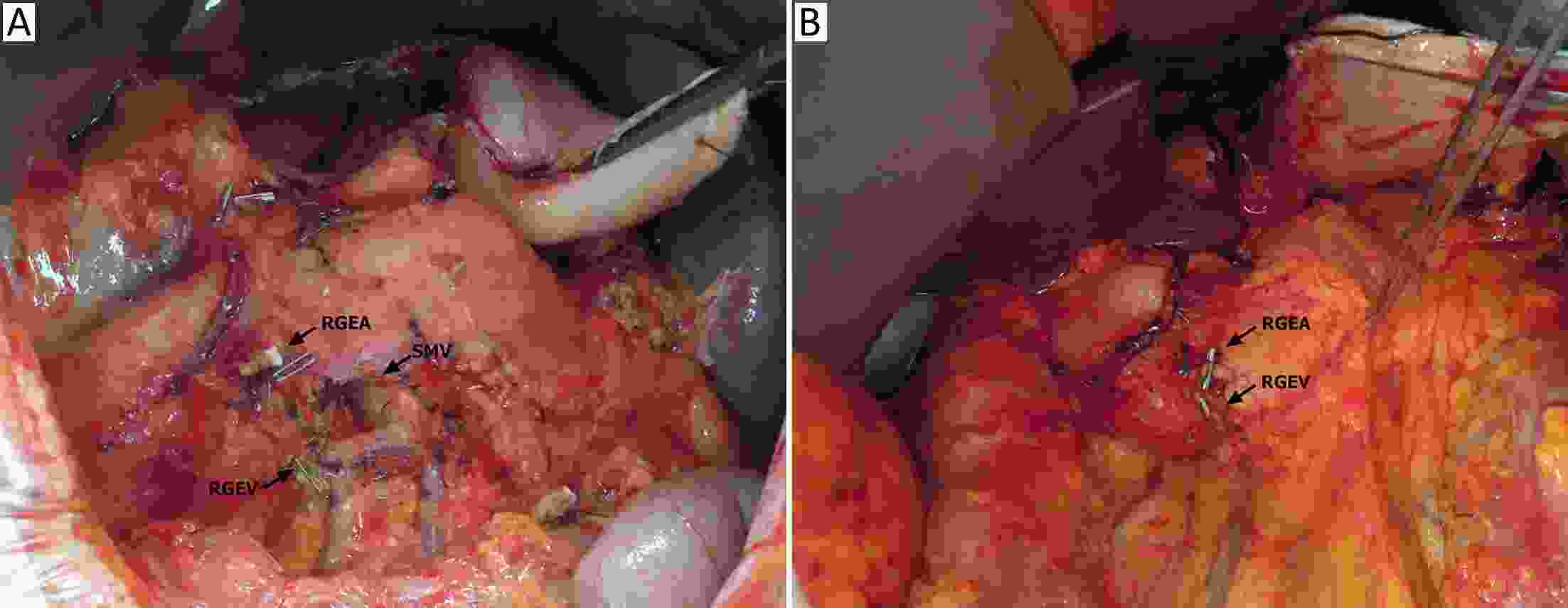
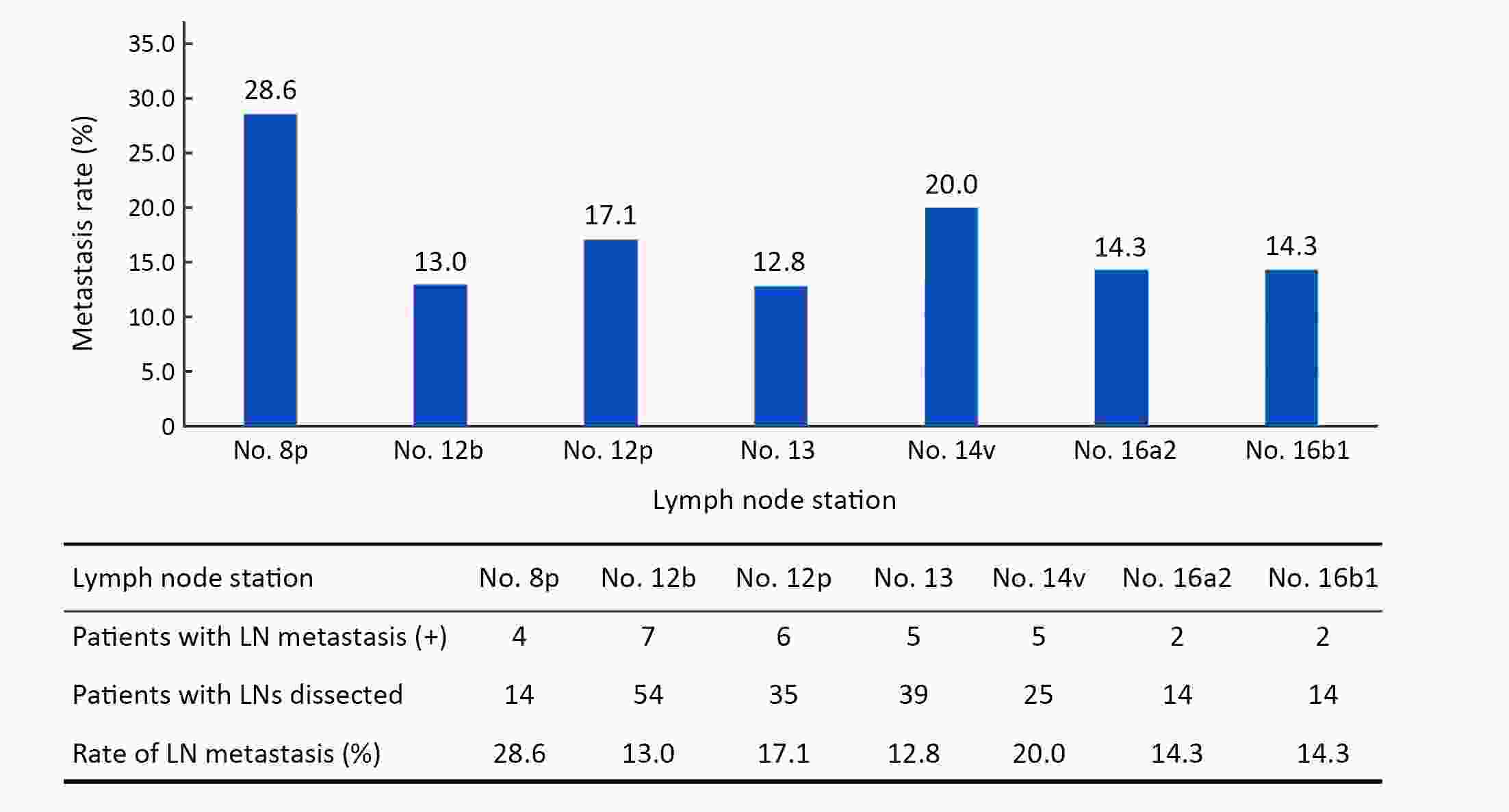
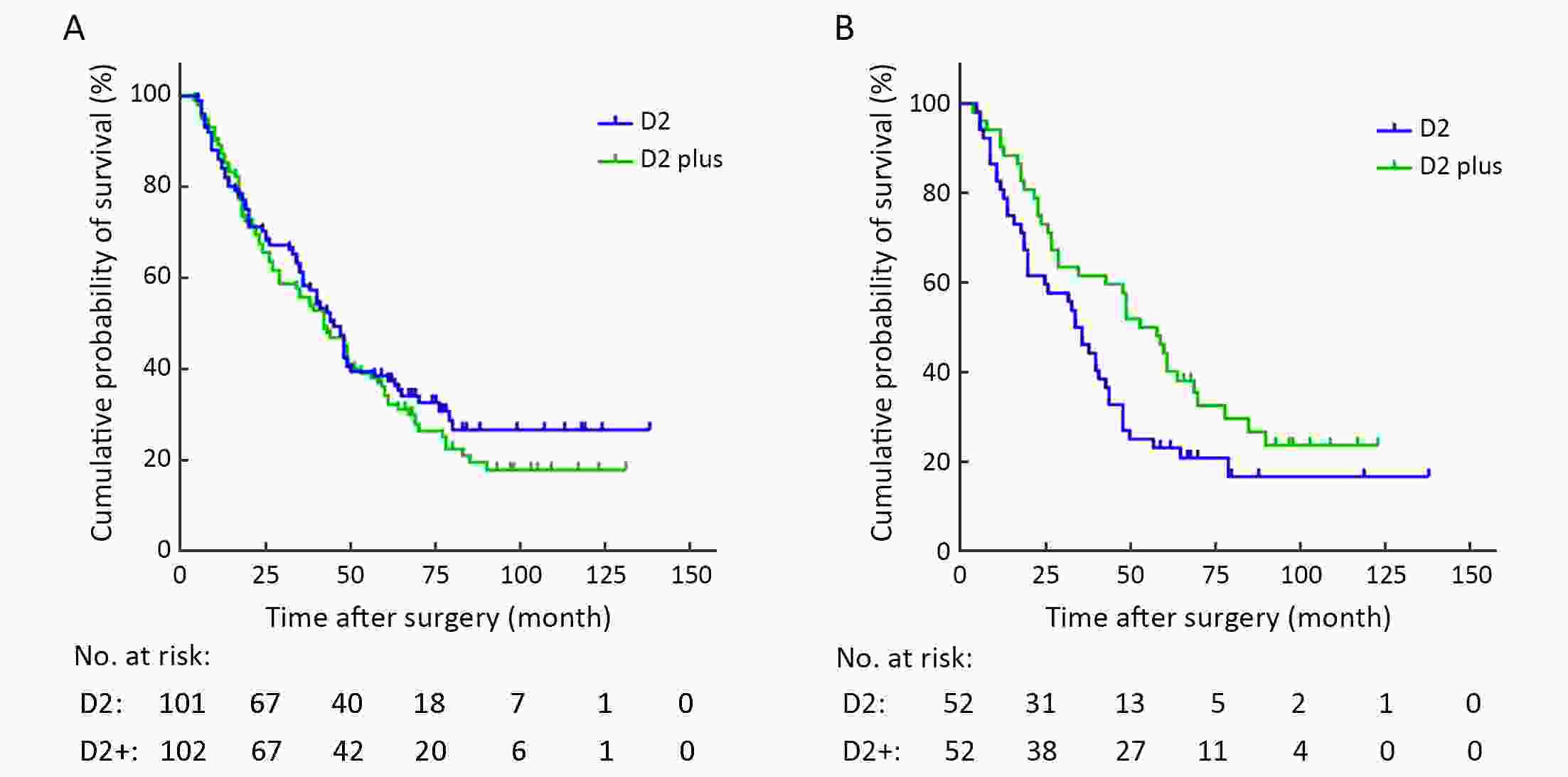
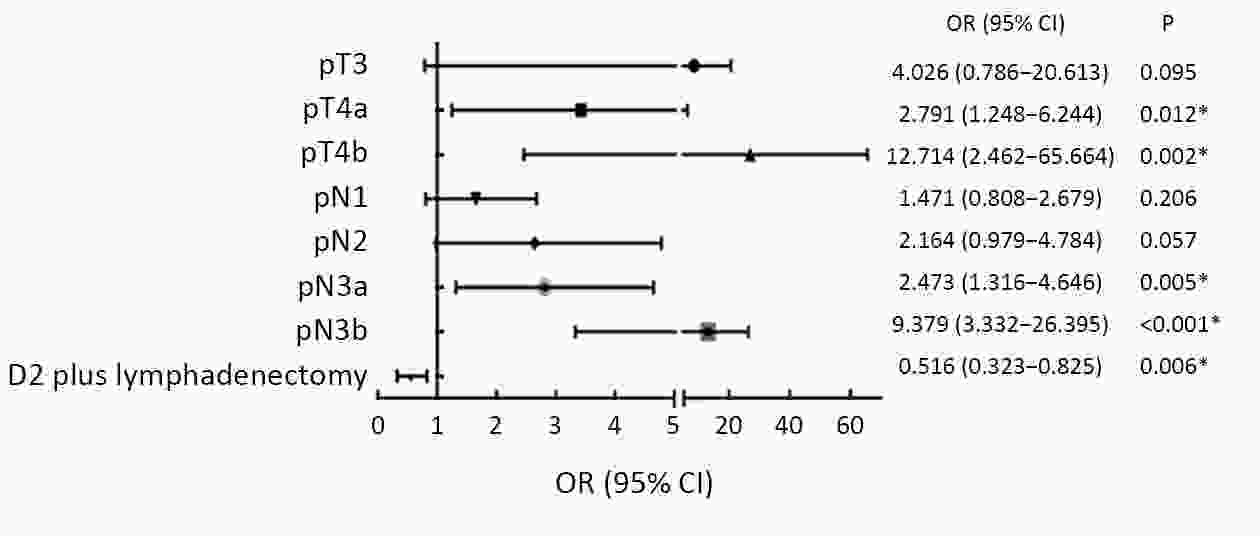
ObjectiveTo investigate the prognostic impact of D2-plus lymphadenectomy including the posterior (No. 8p, No. 12b/p, No. 13, and No. 14v), and para-aortic (No. 16a2, and No. 16b1) lymph nodes (LNs) in subtotal gastrectomy for advanced gastric antral carcinoma. MethodsA total of 203 patients with advanced gastric cancer (GC) located in the antrum, who underwent R0 gastrectomy with D2 or D2-plus lymphadenectomy between January 2003 and December 2011 were enrolled. Propensity score matching was used to reduce the strength of the confounding factors to accurately evaluate prognoses. The therapeutic value index (TVI) was calculate to evaluate the survival benefit of dissecting each LN station. ResultsOf 102 patients with D2-plus lymphadenectomy, 21 (20.59%) were pathologically identified as having LN metastases beyond the extent of D2 lymphadenectomy. After matching, the overall survival (OS) was significantly better in the D2-plus than the D2 group (P=0.030). In the multivariate survival analysis, D2-plus lymphadenectomy (hazard ratio, 0.516; P=0.006) was confirmed to significantly improve the survival rate. In the logistic regression analysis, pN stage [odds ratio (OR), 2.533; 95% confidence interval (95% CI), 1.368−4.691; P=0.003] and extent of LNs metastasis (OR, 5.965; 95% CI, 1.335−26.650; P=0.019) were identified as independent risk factors for LN metastases beyond the extent of D2 lymphadenectomy. The TVI of patient with metastasis to LNs station was 7.1 (No. 8p), 5.7 (No. 12p), 5.1 (No. 13), and 7.1 (both No. 16a2 and No. 16b1), respectively. ConclusionsD2-plus lymphadenectomy may improve the prognoses of some patients with advanced GC located in the antrum, especially for No. 8p, No. 12b, No. 13, and No. 16.
2020, 32(1): 62-71.
doi: 10.21147/j.issn.1000-9604.2020.01.08
Abstract:
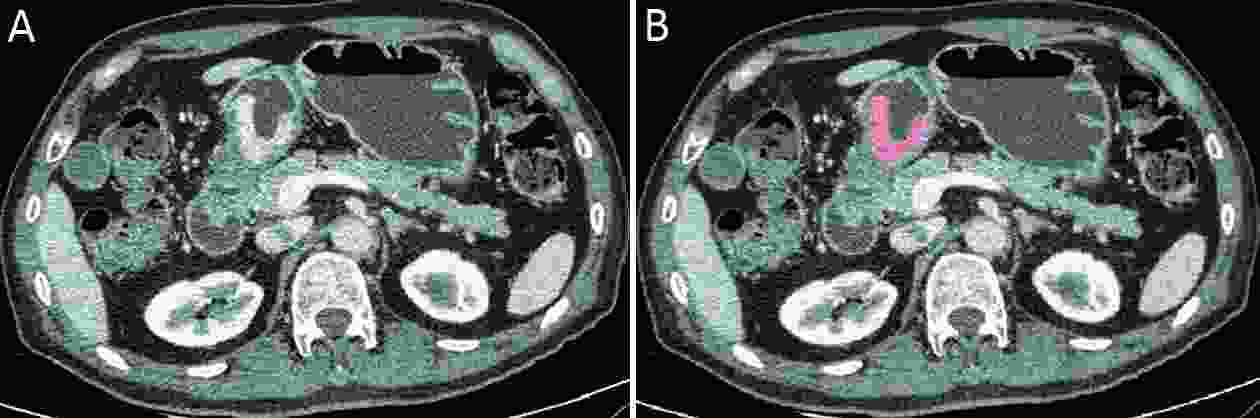
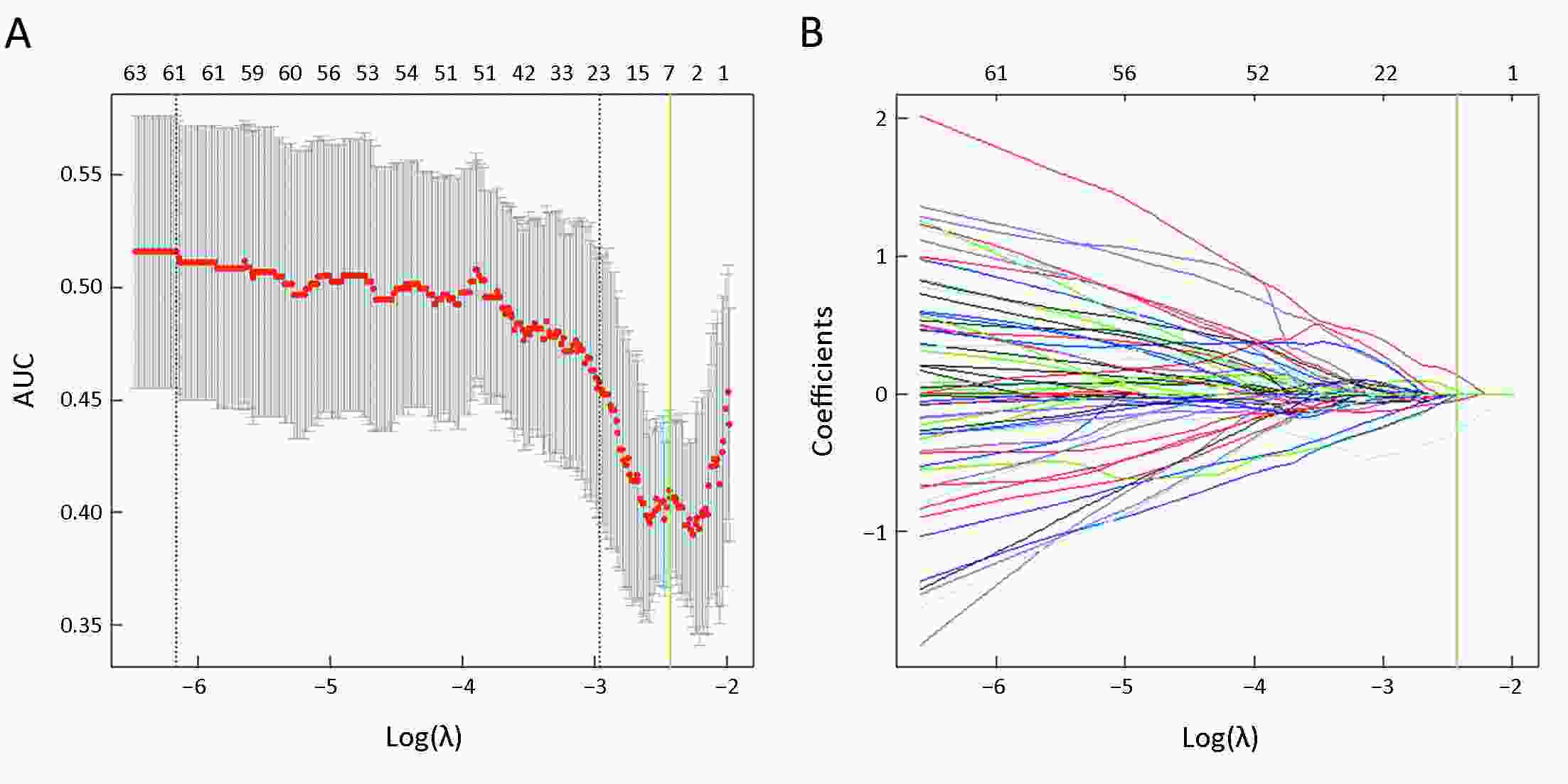
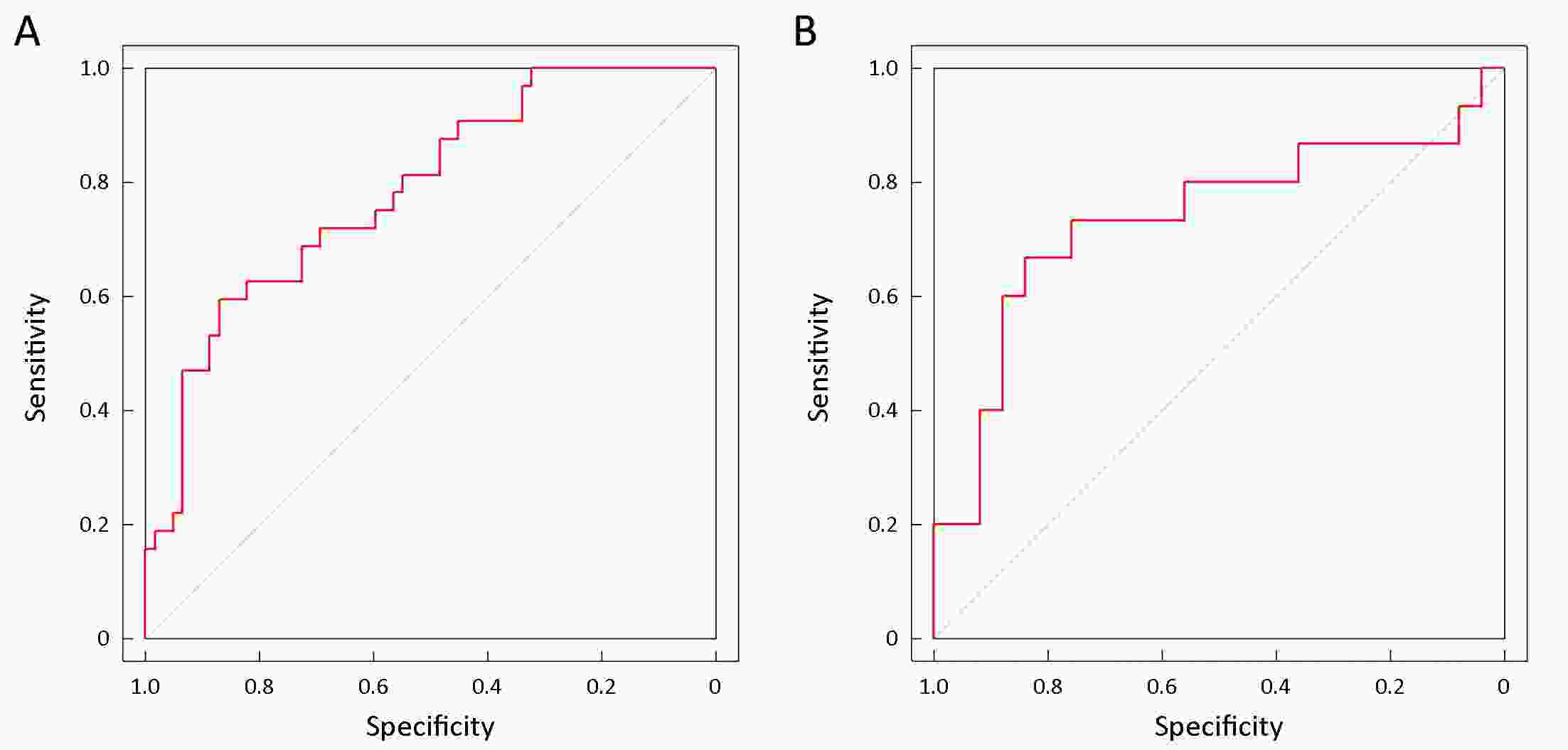
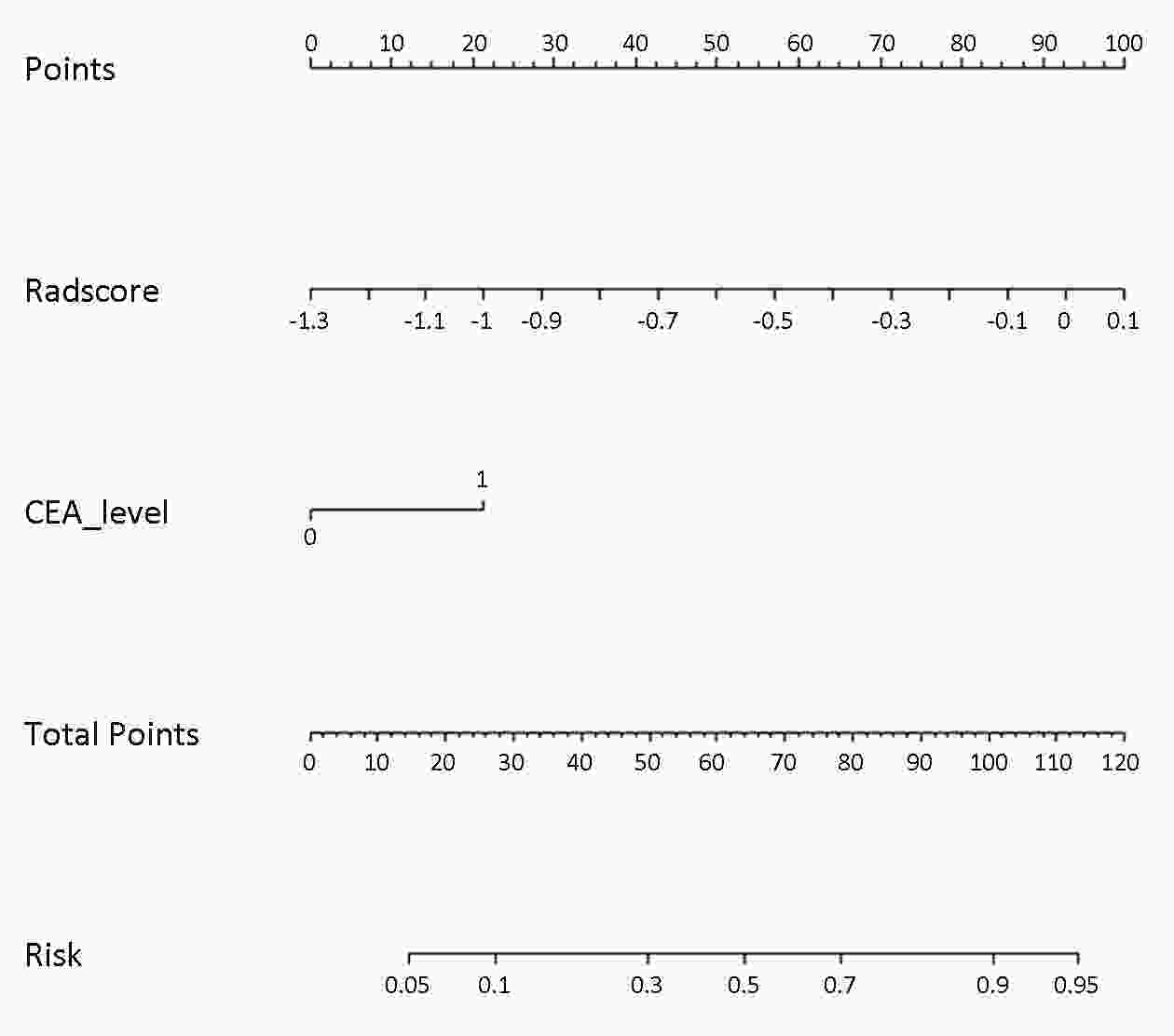
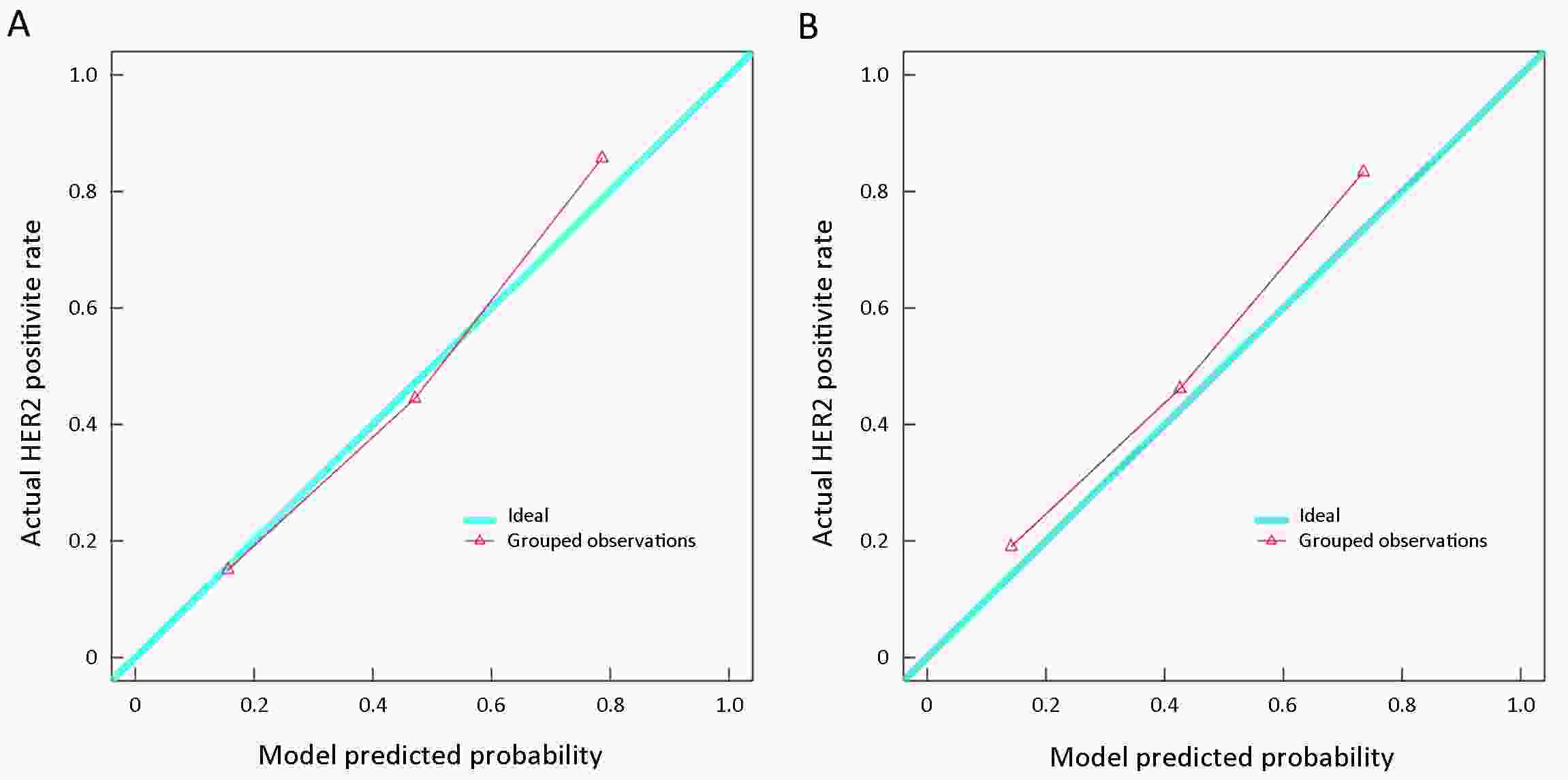
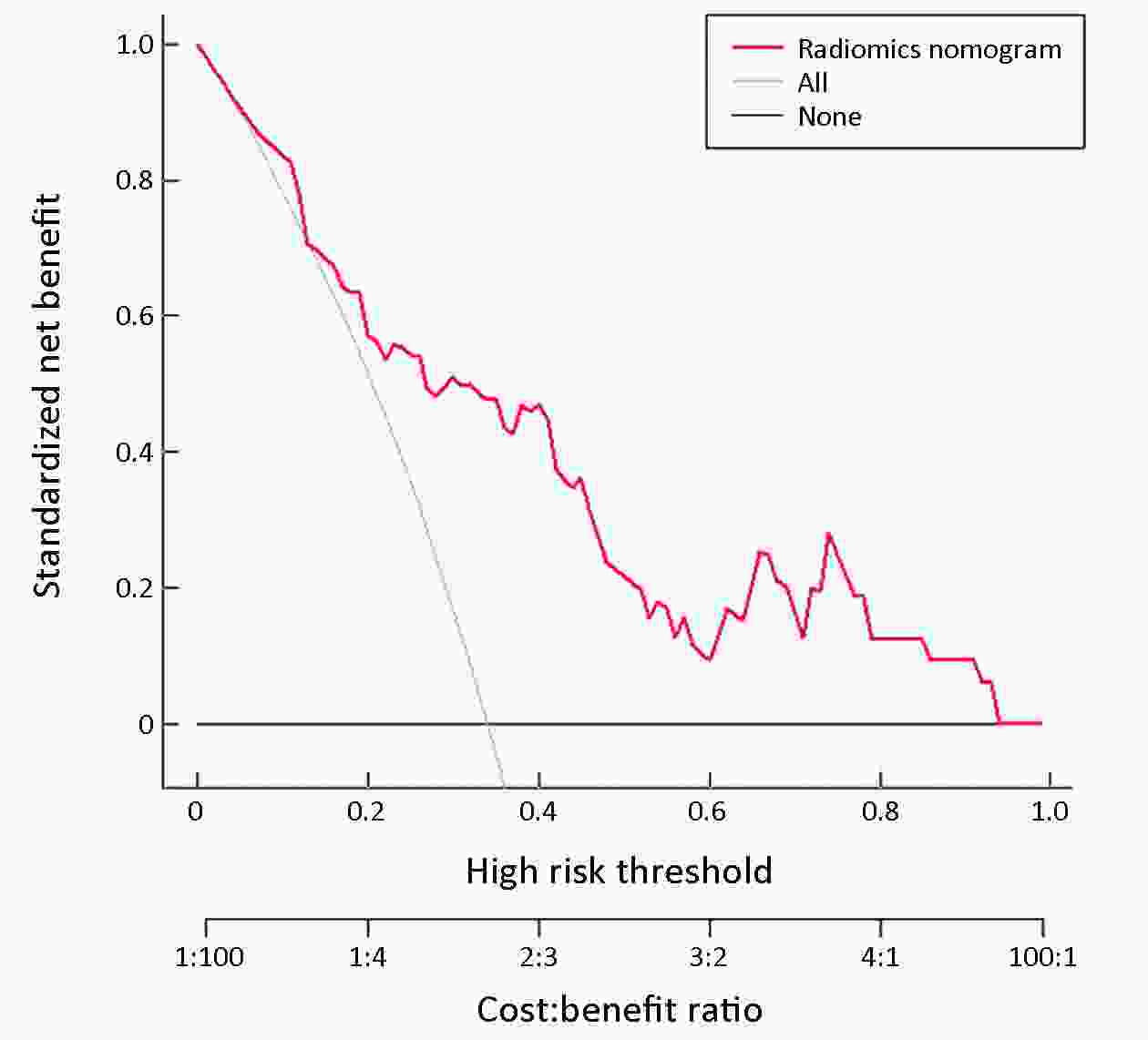
ObjectiveTo develop and validate a computed tomography (CT)-based radiomics nomogram for predicting human epidermal growth factor receptor 2 (HER2) status in patients with gastric cancer. MethodsThis retrospective study included 134 patients with gastric cancer (HER2-negative: n=87; HER2-positive: n=47) from April 2013 to March 2018, who were then randomly divided into training (n=94) and validation (n=40) cohorts. Radiomics features were obtained from the CT images showing gastric cancer. Least absolute shrinkage and selection operator (LASSO) regression analysis was utilized for building the radiomics signature. A multivariable logistic regression method was applied to develop a prediction model incorporating the radiomics signature and independent clinicopathologic risk predictors, which were then visualized as a radiomics nomogram. The predictive performance of the nomogram was assessed in the training and validation cohorts. ResultsThe radiomics signature was significantly associated with HER2 status in both training (P<0.001) and validation (P=0.023) cohorts. The prediction model that incorporated the radiomics signature and carcinoembryonic antigen (CEA) level demonstrated good discriminative performance for HER2 status prediction, with an area under the curve (AUC) of 0.799 [95% confidence interval (95% CI): 0.704−0.894] in the training cohort and 0.771 (95% CI: 0.607−0.934) in the validation cohort. The calibration curve of the radiomics nomogram also showed good calibration. Decision curve analysis showed that the radiomics nomogram was useful. ConclusionsWe built and validated a radiomics nomogram with good performance for HER2 status prediction in gastric cancer. This radiomics nomogram could serve as a non-invasive tool to predict HER2 status and guide clinical treatment.
2020, 32(1): 72-88.
doi: 10.21147/j.issn.1000-9604.2020.01.09
Abstract:
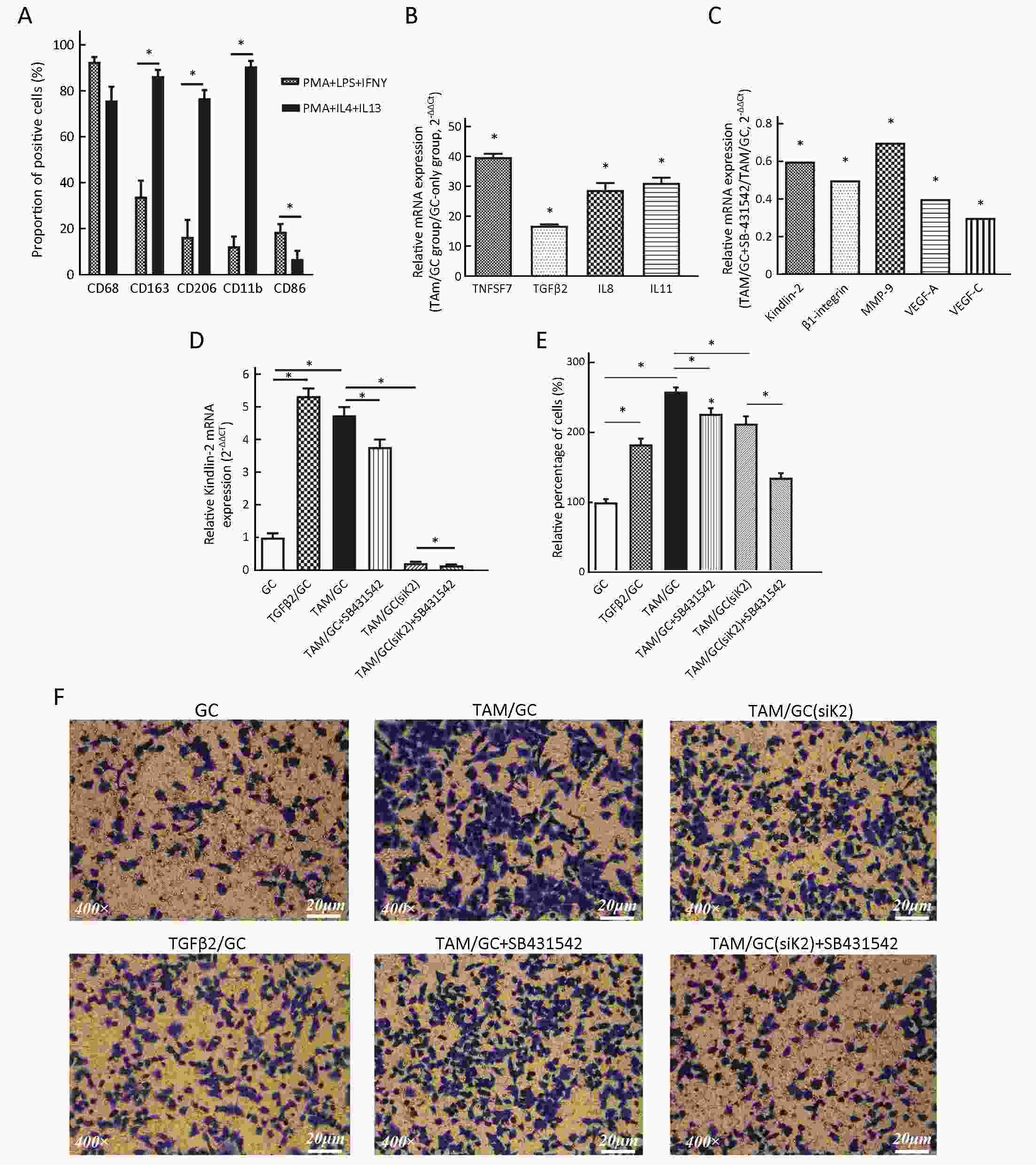
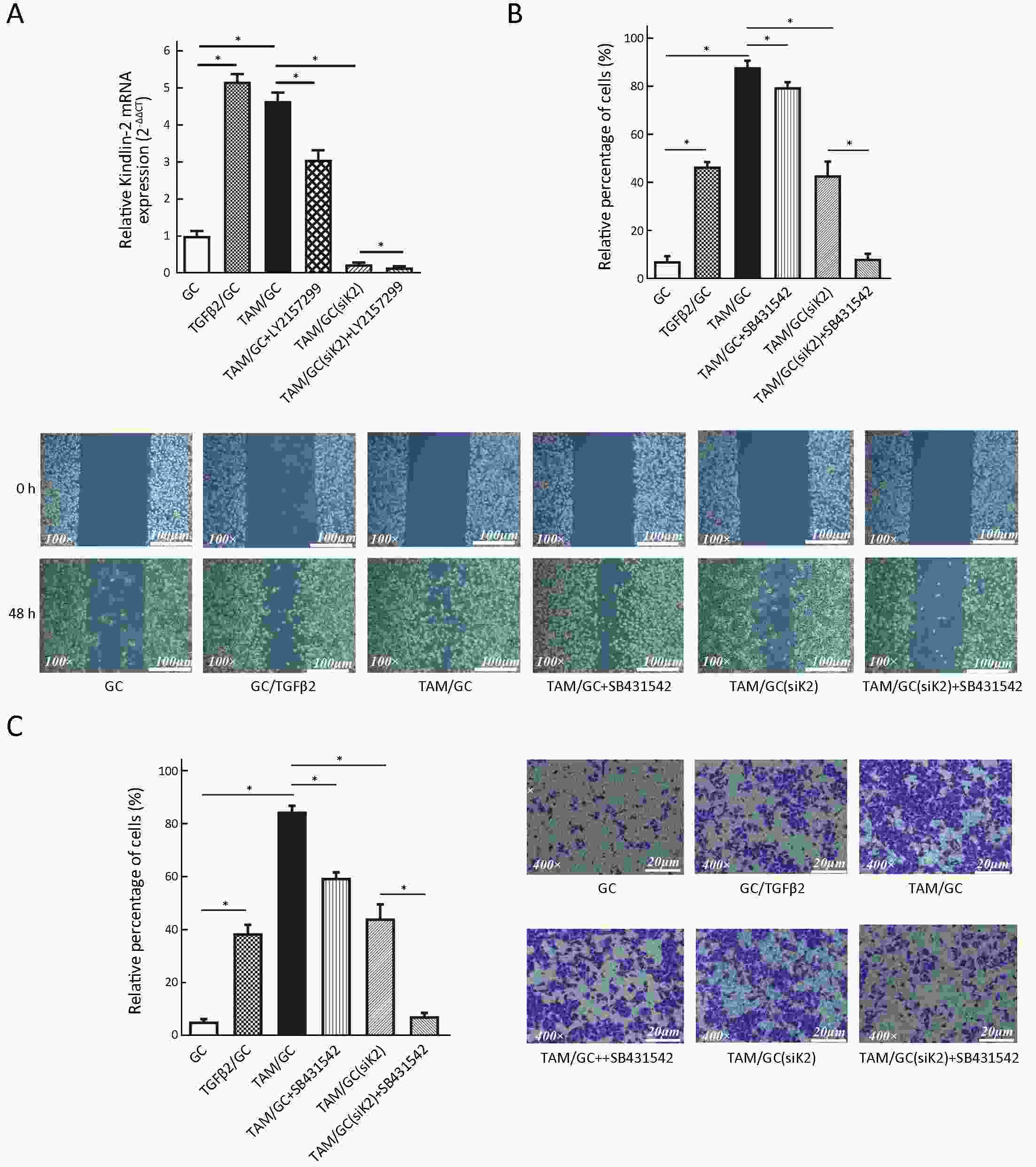
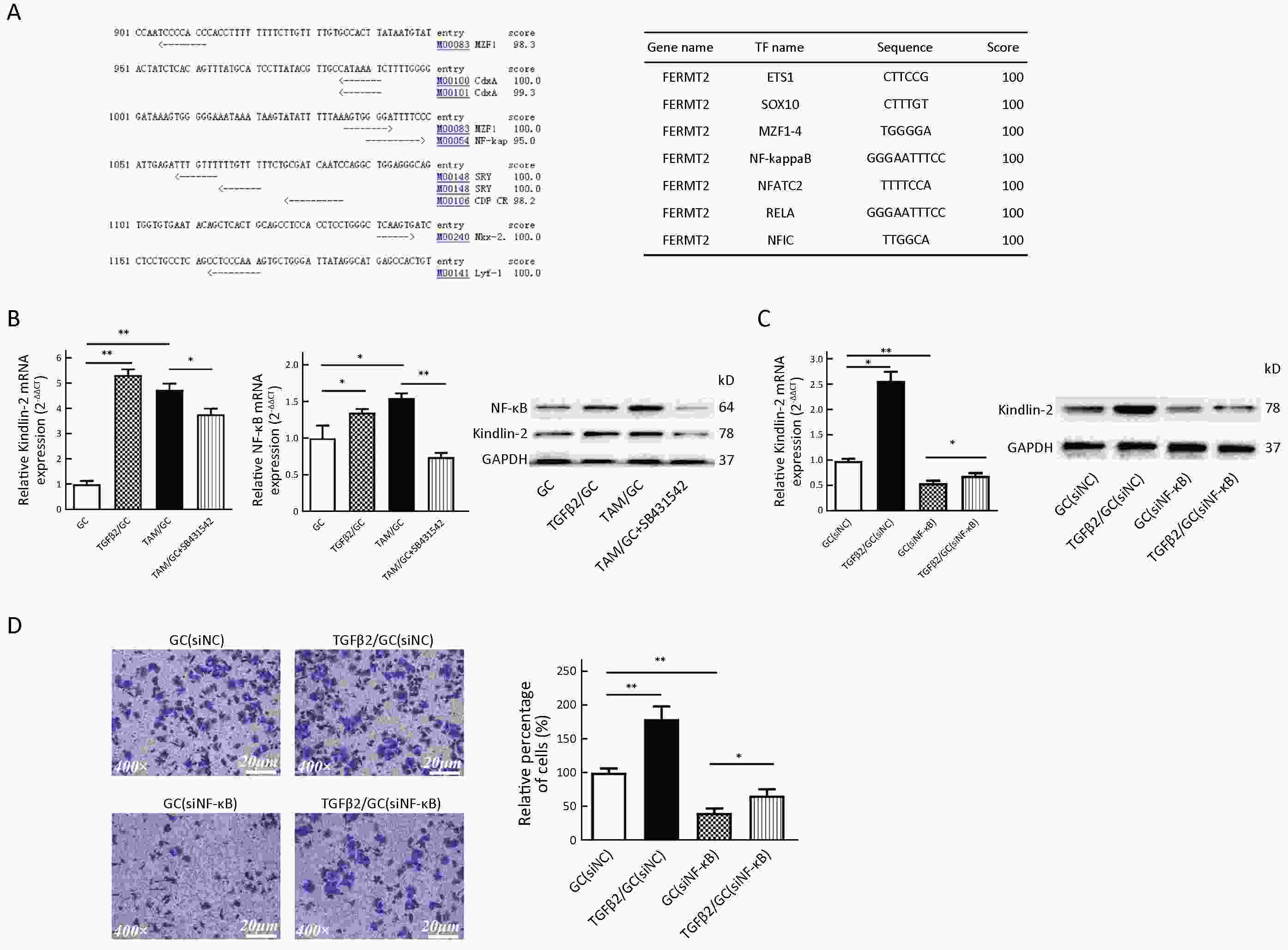
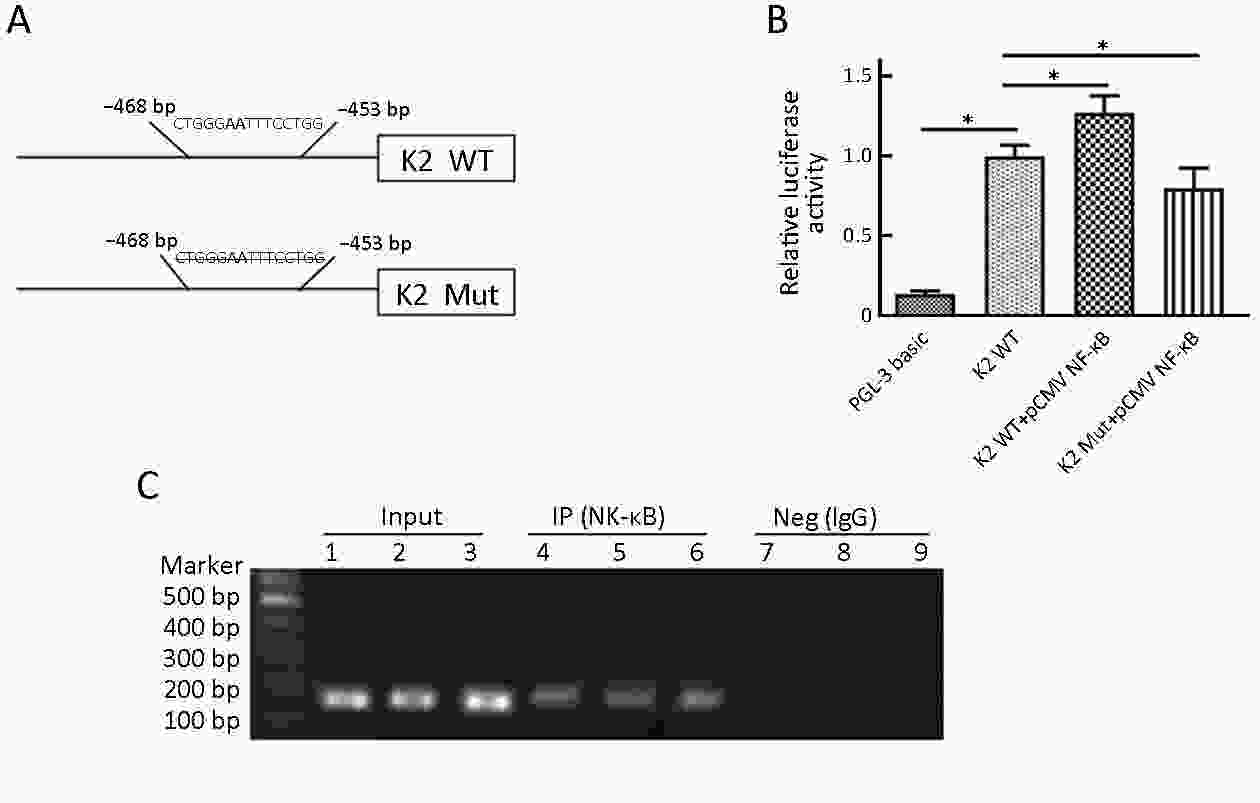
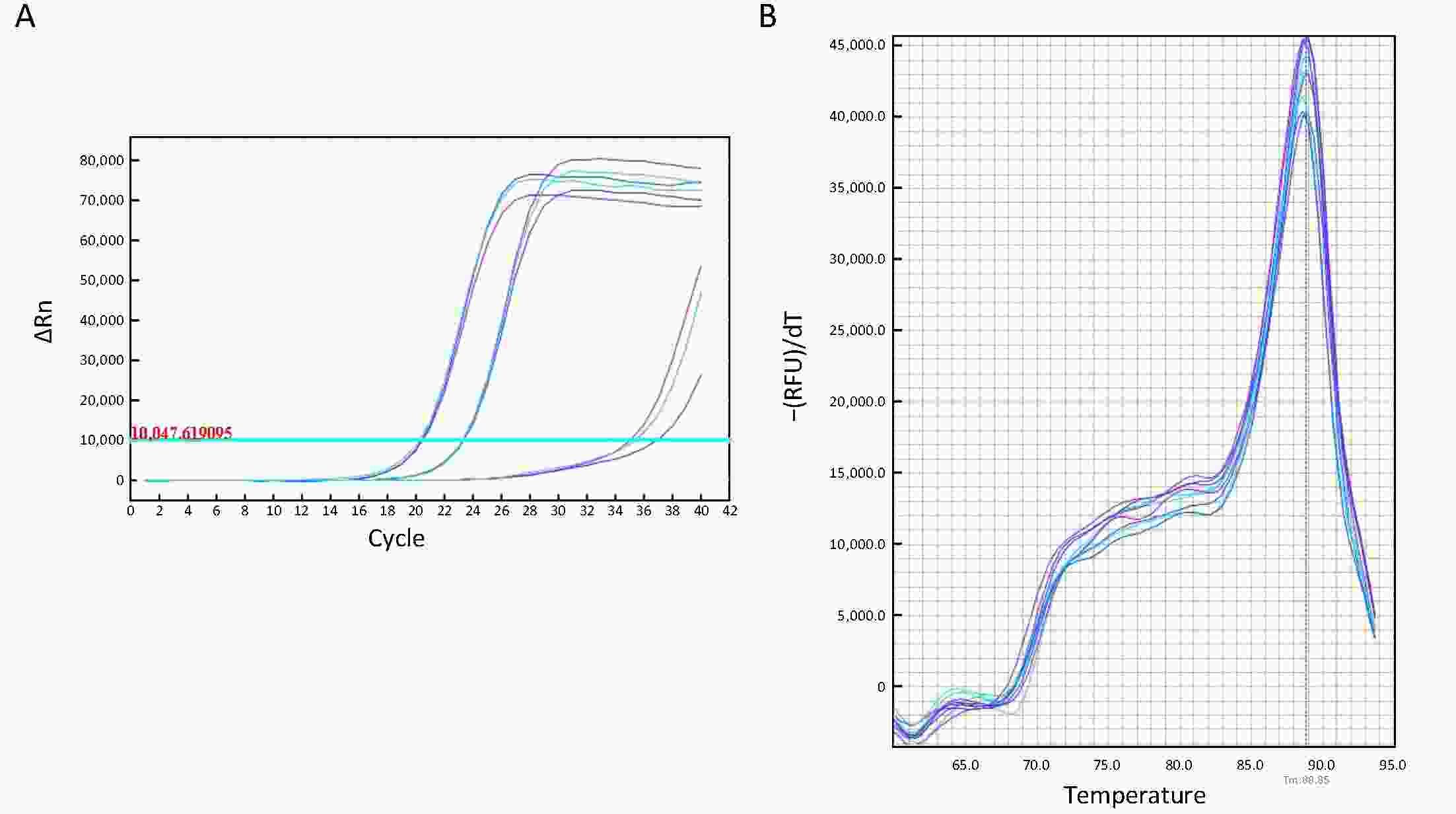
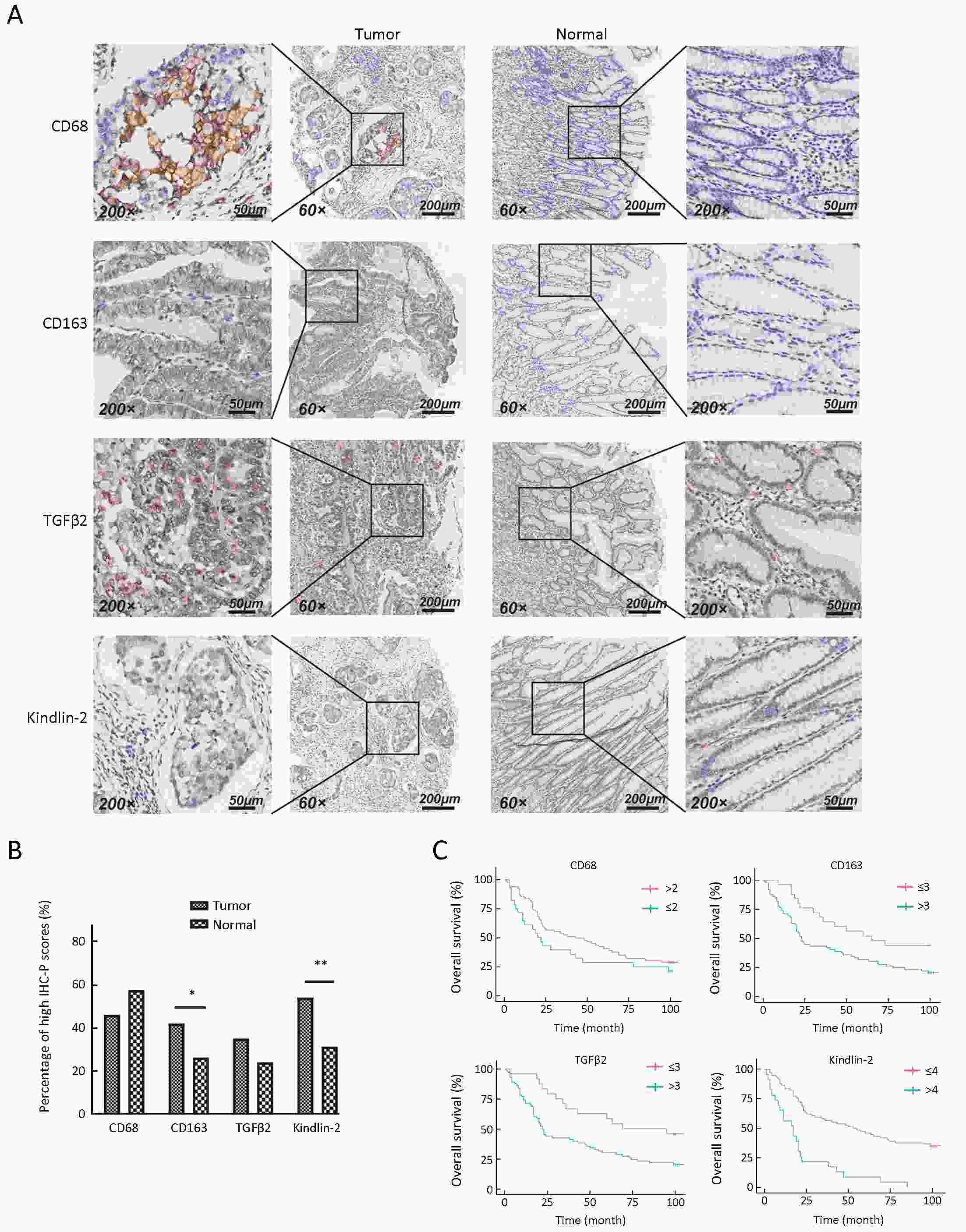
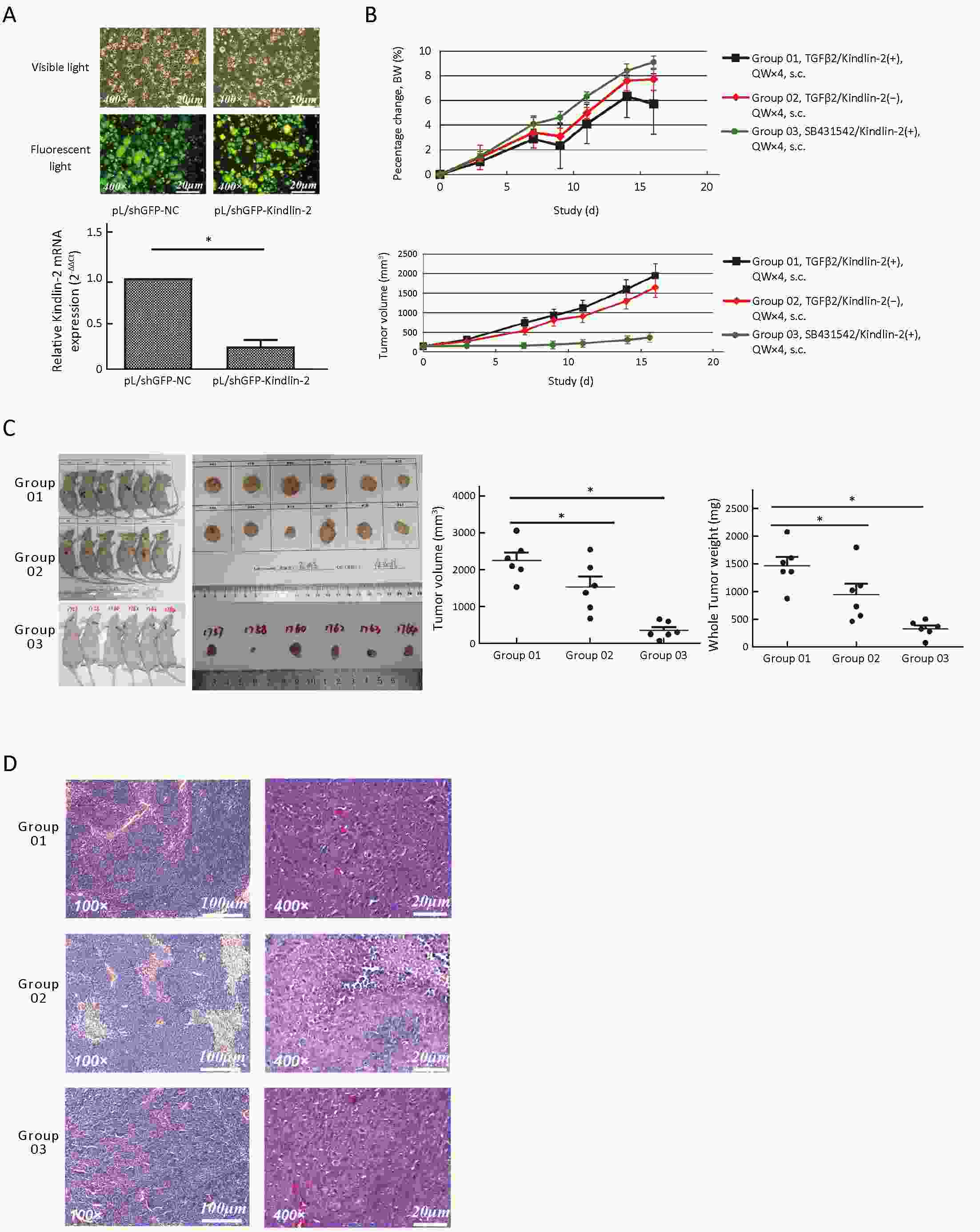
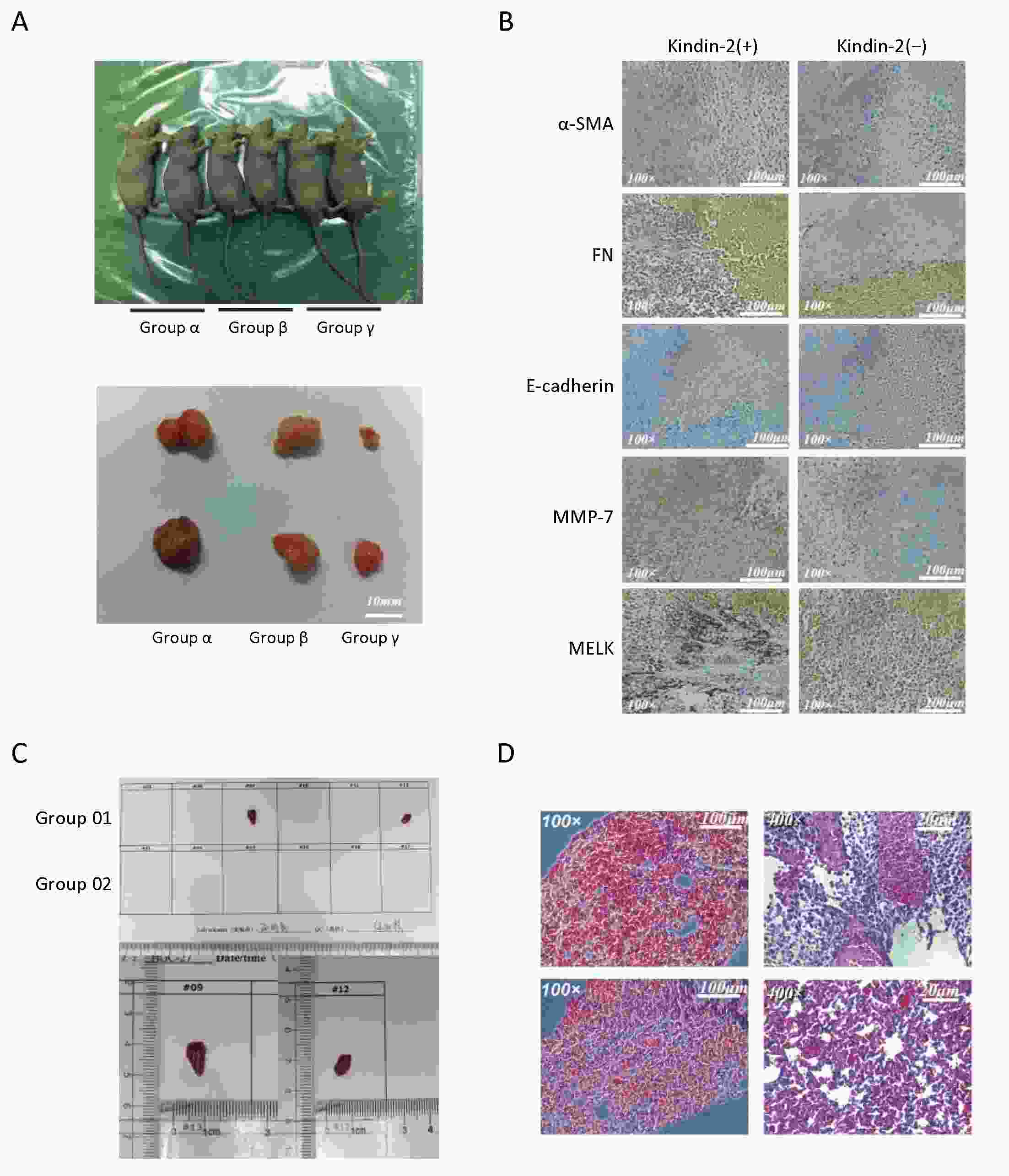
ObjectiveRecent studies have shown that tumor-associated macrophages (TAMs) play an important role in cancer invasion and metastasis. Our previous studies have reported that TAMs promote the invasion and metastasis of gastric cancer (GC) cells through the Kindlin-2 pathway. However, the mechanism needs to be clarified. MethodsTHP-1 monocytes were induced by PMA/interleukin (IL)-4/IL-13 to establish an efficient TAM model in vitro and M2 macrophages were isolated via flow cytometry. A dual luciferase reporter system and chromatin immunoprecipitation (ChIP) assay were used to investigate the mechanism of transforming growth factor β2 (TGFβ2) regulating Kindlin-2 expression. Immunohistochemistry was used to study the relationships among TAM infiltration in human GC tissues, Kindlin-2 protein expression, clinicopathological parameters and prognosis in human GC tissues. A nude mouse oncogenesis model was used to verify the invasion and metastasis mechanisms in vivo. ResultsWe found that Kindlin-2 expression was upregulated at both mRNA and protein levels in GC cells cocultured with TAMs, associated with higher invasion rate. Kindlin-2 knockdown reduced the invasion rate of GC cells under coculture condition. TGFβ2 secreted by TAMs regulated the expression of Kindlin-2 through the transcription factor NF-кB. TAMs thus participated in the progression of GC through the TGFβ2/NF-κB/Kindlin-2 axis. Kindlin-2 expression and TAM infiltration were significantly positively correlated with TNM stage, and patients with high Kindlin-2 expression had significantly poorer overall survival than patients with low Kindlin-2 expression. Furthermore, Kindlin-2 promoted the invasion of GC cells in vivo. ConclusionsThis study elucidates the mechanism of TAMs participating in GC cell invasion and metastasis through the TGFβ2/NF-κB/Kindlin-2 axis, providing a possibility for new treatment options and approaches.
2020, 32(1): 89-95.
doi: 10.21147/j.issn.1000-9604.2020.01.10
Abstract:
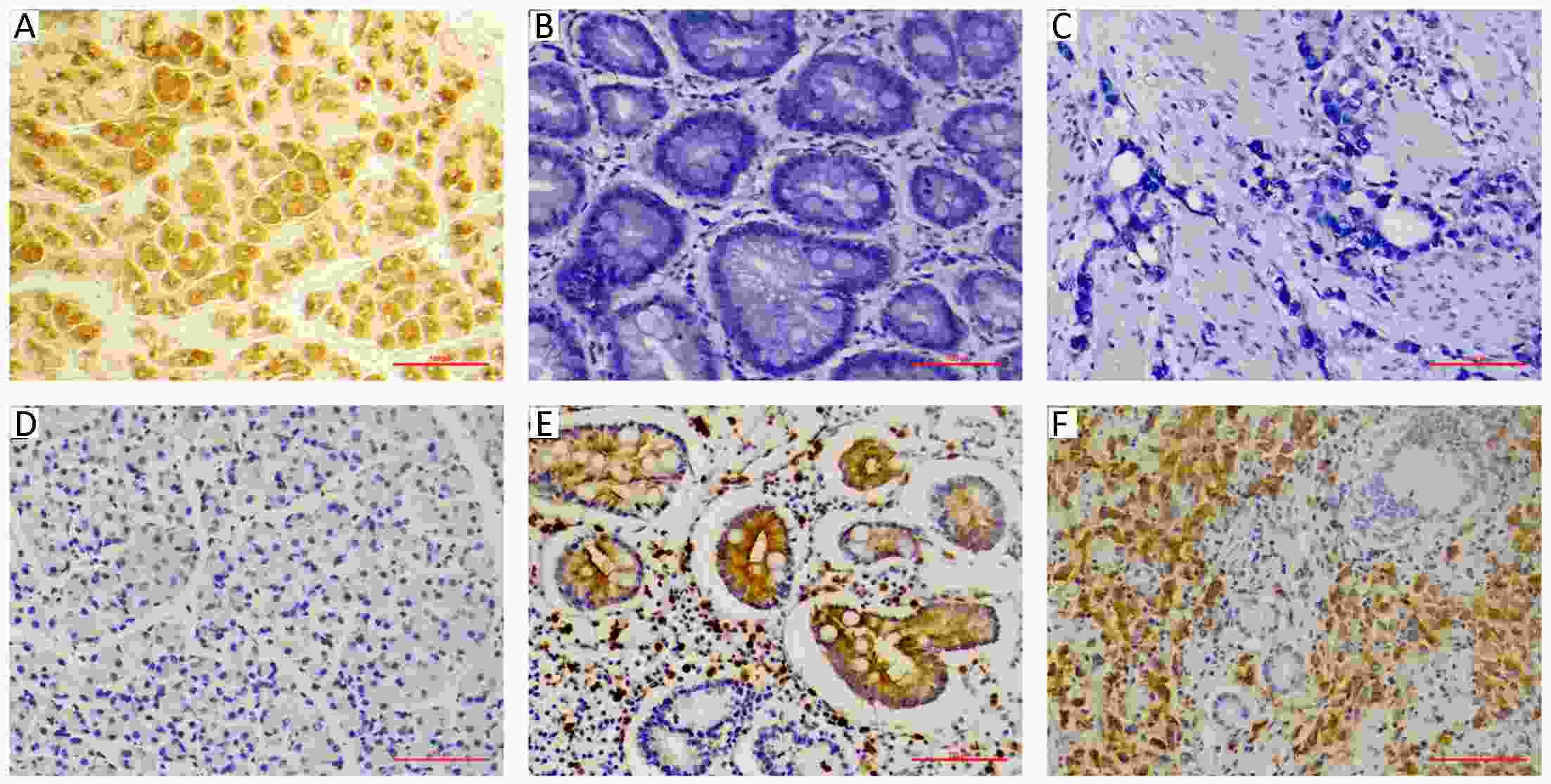
ObjectiveThe aim of this study was to investigate the value of the combined expression of the gastric mucosal differentiation protein pepsinogen C (PGC) and gastric cancer (GC)-associated antigen MG7 for the diagnosis of GC and prediction of the development from precancerous conditions to GC. MethodsThe gastric mucosal biopsies of 285 subjects enrolled from a region with a high incidence of GC were obtained and histopathologically examined. Subjects testing negative for GC (n=208) were followed up from 1998 to 2015. The levels of PGC and MG7 in the biopsies were determined by immunohistochemistry. ResultsPGC was positive in 91.4% of the non-atrophic gastritis, 26.5% of the atrophic gastritis, and 0% of the GC. MG7 was positive in 15.0% of the non-atrophic gastritis, 82.4% of the atrophic gastritis, and 94.8% of the GC. The non-atrophic gastritis group was predominantly “PGC+MG7−”. The atrophic gastritis and GC groups were predominantly “PGC−MG7+”. The rate of GC in subjects with “PGC−MG7+” staining was 113.4-fold higher [95% confidence interval (95% CI): 15.3−869.4, P<0.001] than that in subjects with other staining patterns. The sensitivity and specificity of the “PGC−MG7+” pattern were 92.2% and 78.8% for the detection of GC and 77.2% and 97.9% for GC and precancerous disease, respectively. In the follow-up cohort of non-GC subjects, the risk of developing GC was higher in those with the “PGC−MG7+” staining pattern. ConclusionsOur data suggest that the “PGC−MG7+” pattern can be employed as a useful follow-up panel for detecting individuals with a high risk of GC, and the dynamic assessment of the follow-up panel needs multi-centre large-scale validation in the future.
2020, 32(1): 96-104.
doi: 10.21147/j.issn.1000-9604.2020.01.11
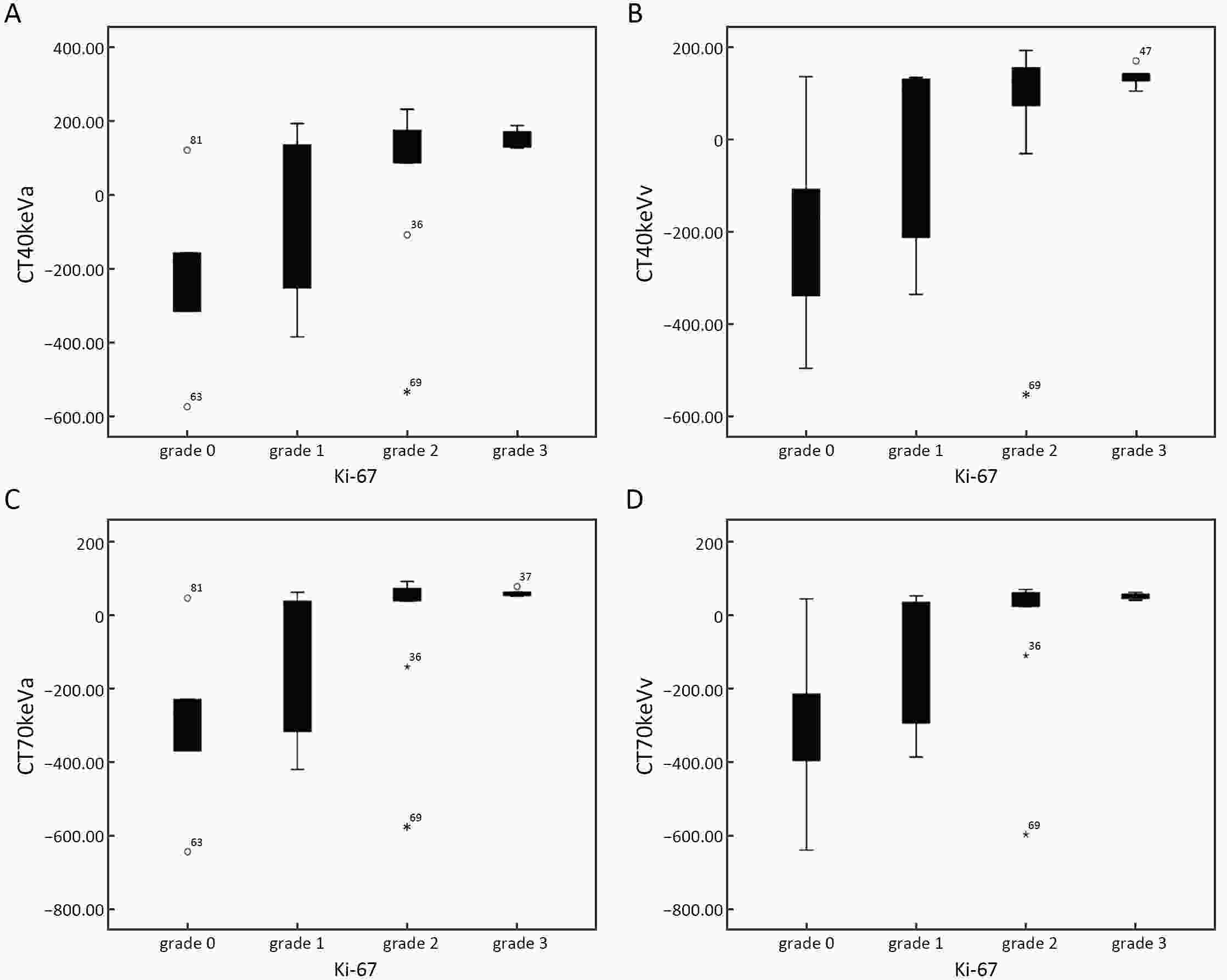
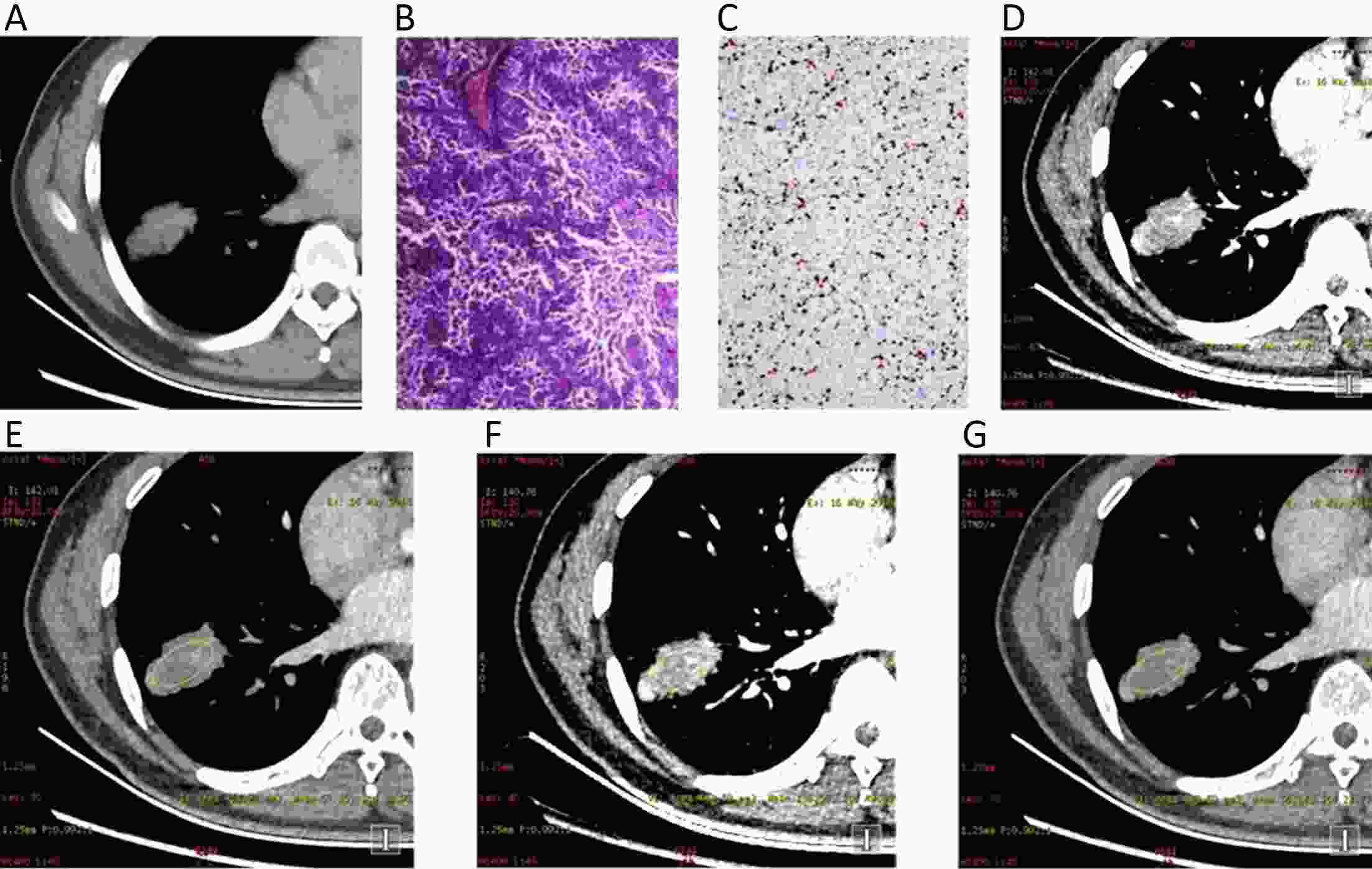
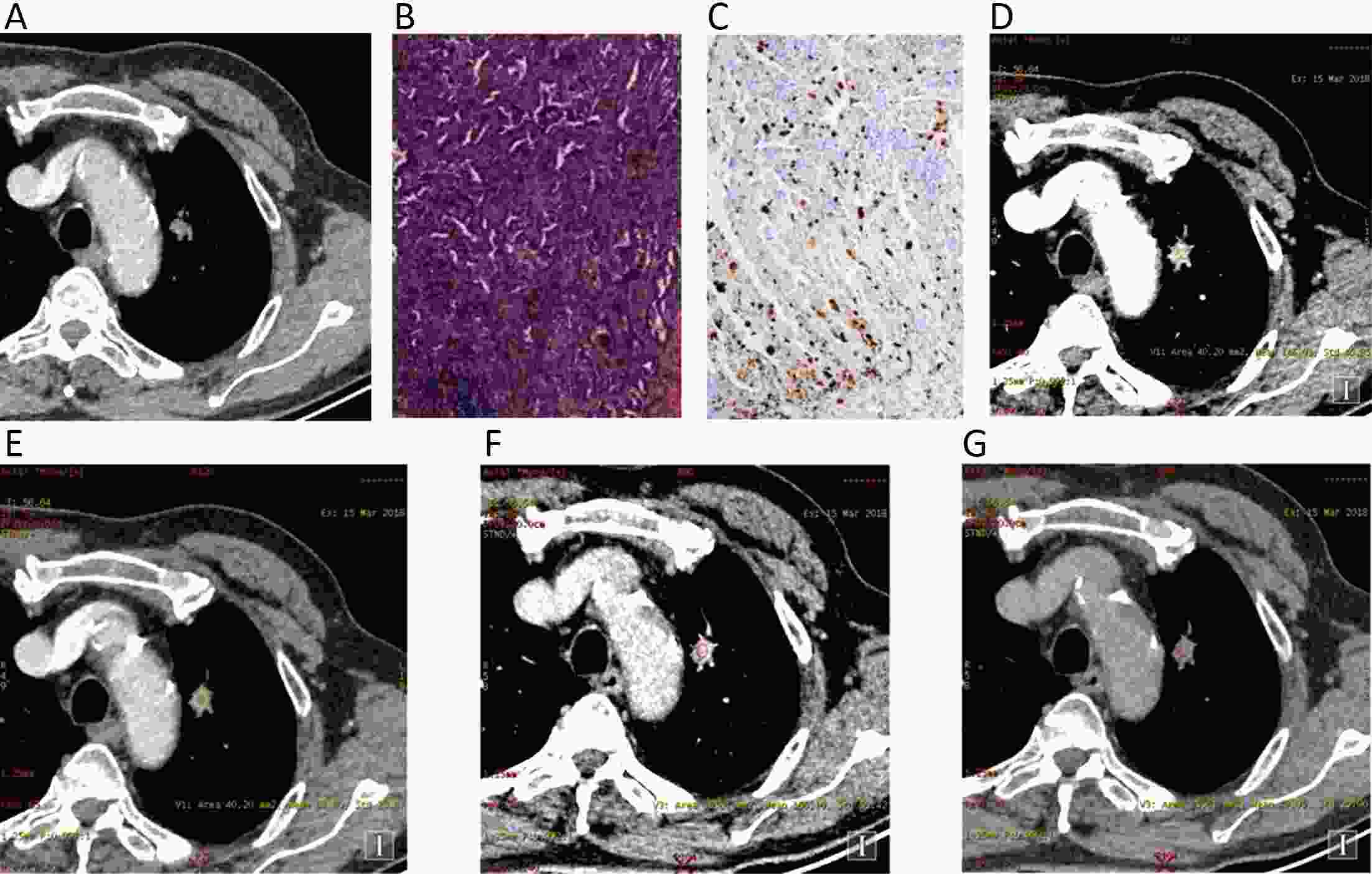
Abstract:
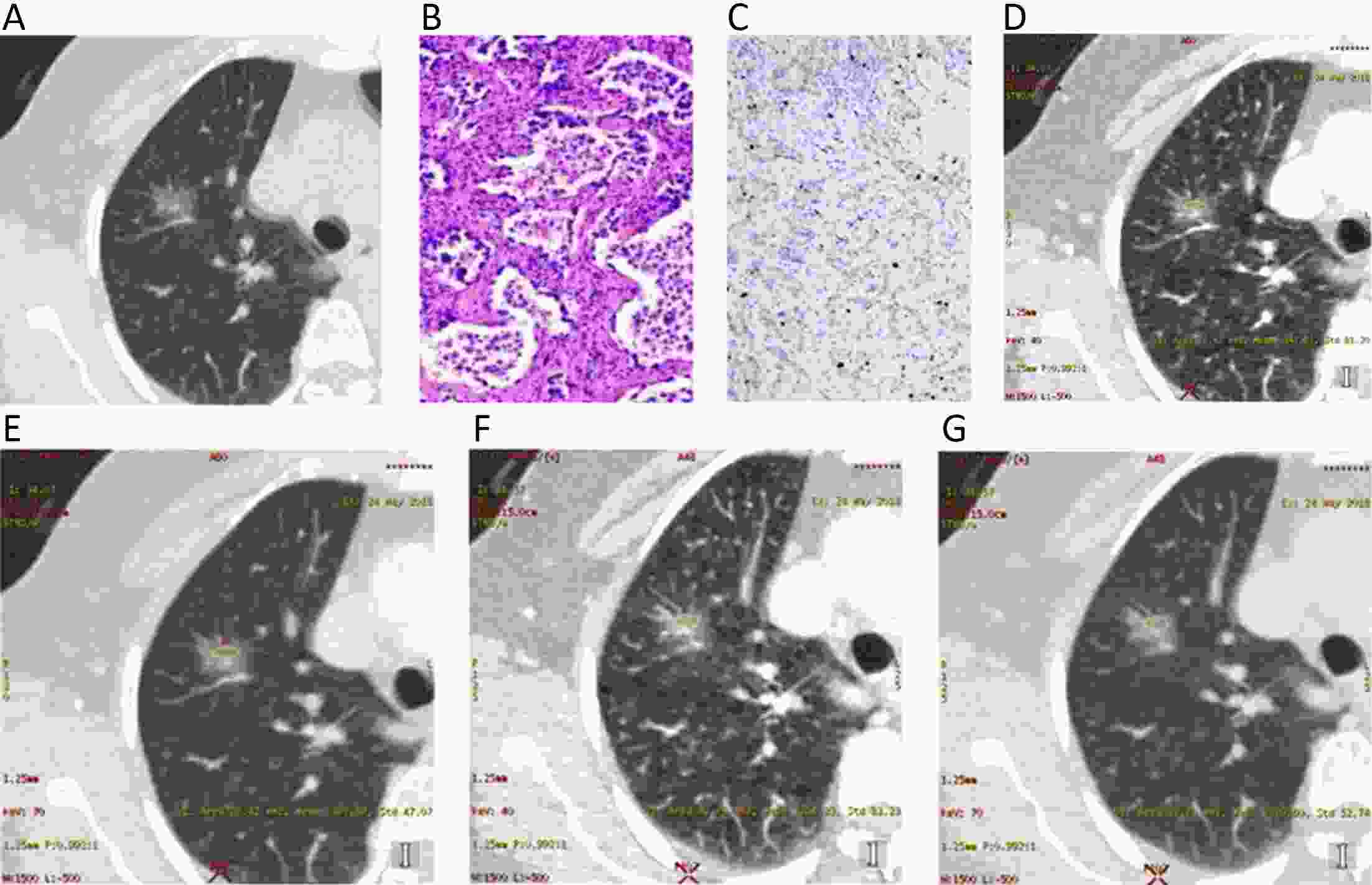
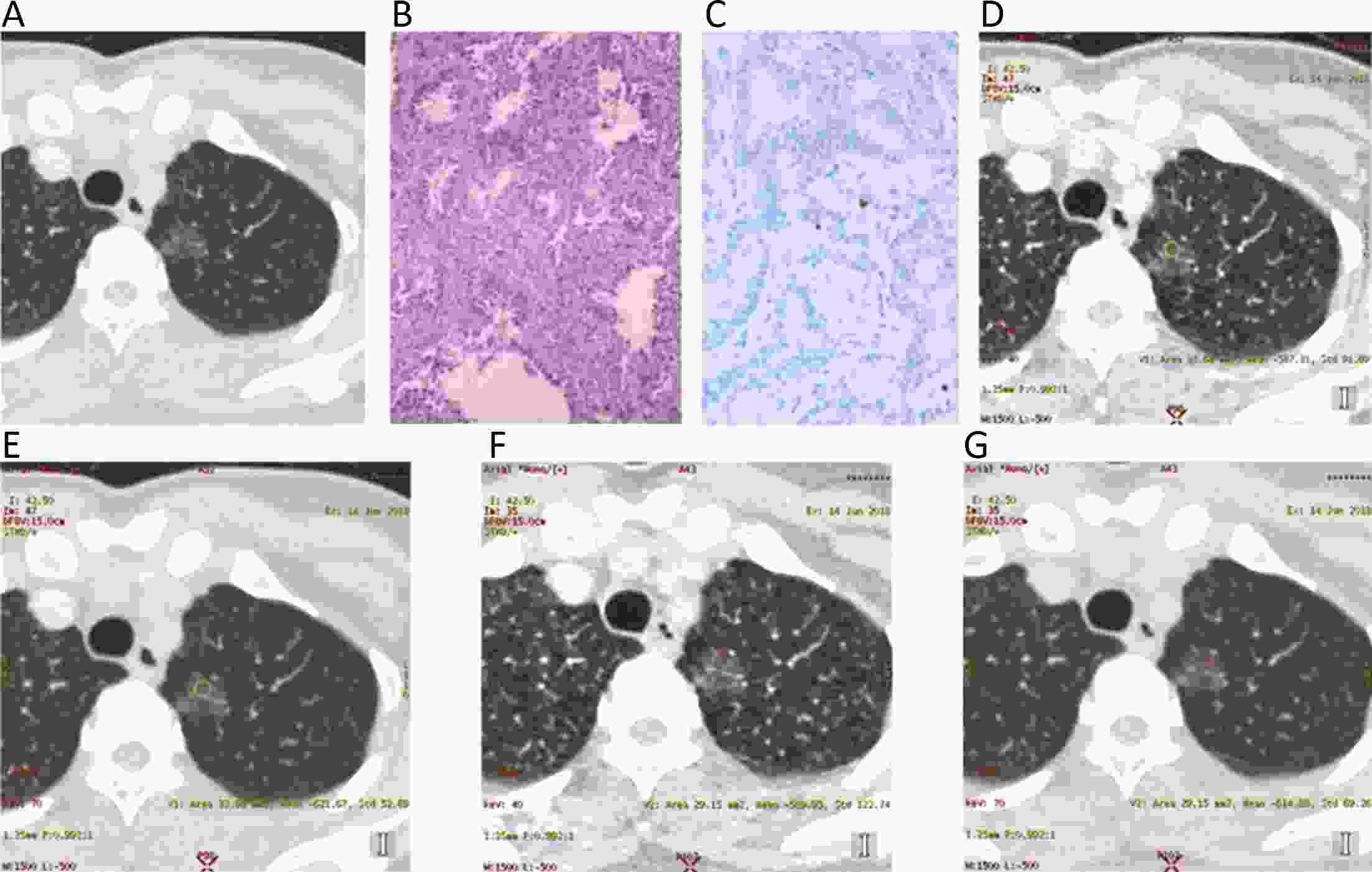
ObjectiveTo explore the correlation between the spectral computed tomography (CT) imaging parameters and the Ki-67 labeling index in lung adenocarcinoma. MethodsSpectral CT imaging parameters [iodine concentrations of lesions (ICLs) in the arterial phase (ICLa) and venous phase (ICLv), normalized IC in the aorta (NICa/NICv), slope of the spectral HU curve (λHUa/λHUv) and monochromatic CT number enhancement on 40 keV and 70 keV images (CT40keVa/v, CT70keVa/v)] in 34 lung adenocarcinomas were analyzed, and common molecular markers, including the Ki-67 labeling index, were detected with immunohistochemistry. Different Ki-67 labeling indexes were measured and grouped into four grades according to the number of positive-stained cells (grade 0, ≤1%; 1%<grade 1≤10%; 10%<grade 2≤30%; and grade 3, >30%). One-way analysis of variance (ANOVA) was used to compare the four different grades, and the Bonferroni method was used to correct the P value for multiple comparisons. A Spearman correlation analysis was performed to further research a quantitative correlation between the Ki-67 labeling index and spectral CT imaging parameters. ResultsCT40keVa, CT40keVv, CT70keVa and CT70keVv increased as the grade increased, and CT70keVa and CT70keVv were statistically significant (P<0.05). These four parameters and the Ki-67 labeling index showed a moderate positive correlation with lung adenocarcinoma nodules. ICL, NIC and λHU in the arterial and venous phases were not significantly different among the four grades. ConclusionsThe spectral CT imaging parameters CT40keVa, CT40keVv, CT70keVa and CT70keVv gradually increased with Ki-67 expression and showed a moderate positive correlation with lung adenocarcinomas. Therefore, spectral CT imaging parameter-enhanced monochromatic CT numbers at 70 keV may indicate the extent of proliferation of lung adenocarcinomas.
2020, 32(1): 105-114.
doi: 10.21147/j.issn.1000-9604.2020.01.12
Abstract:
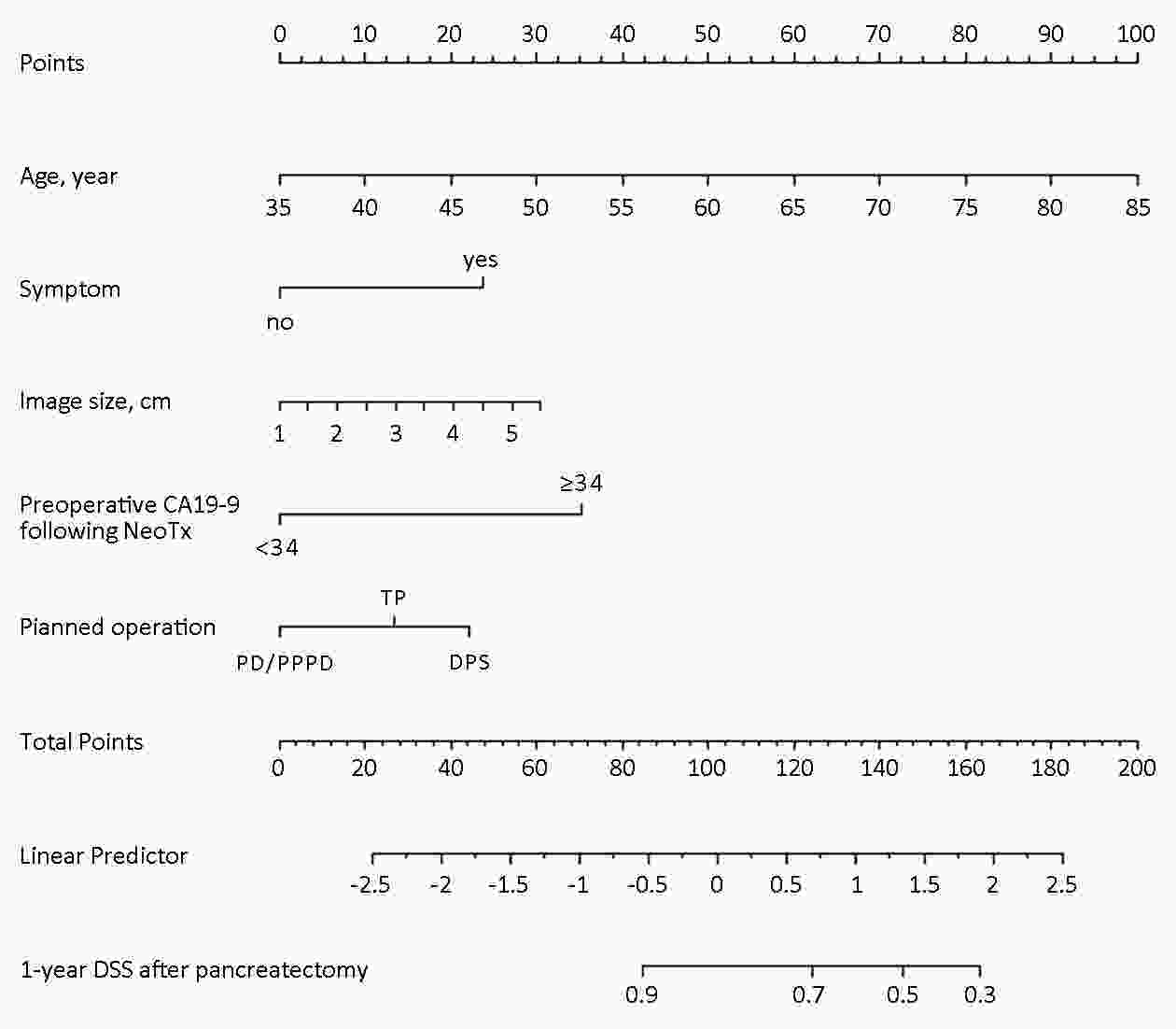
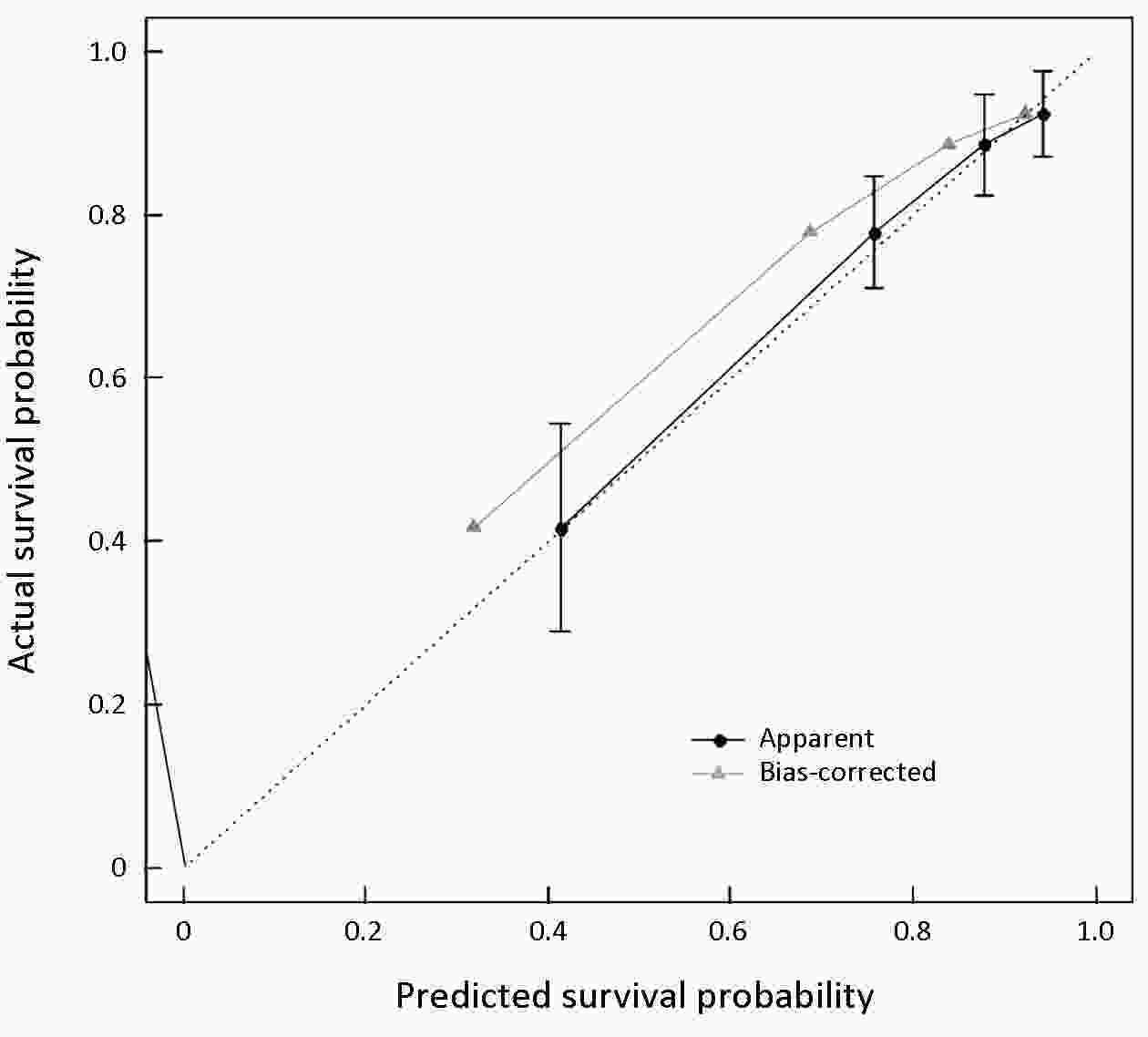
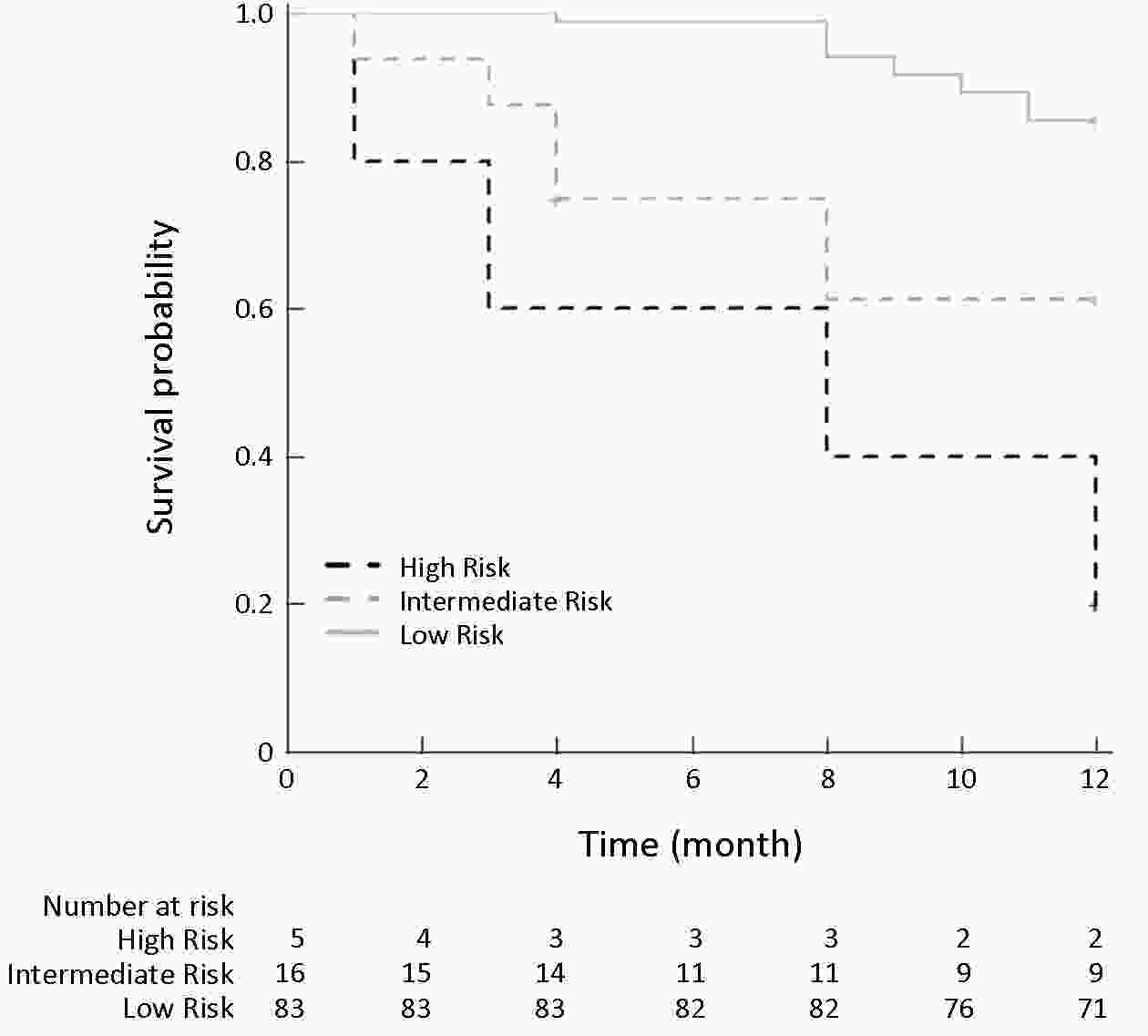
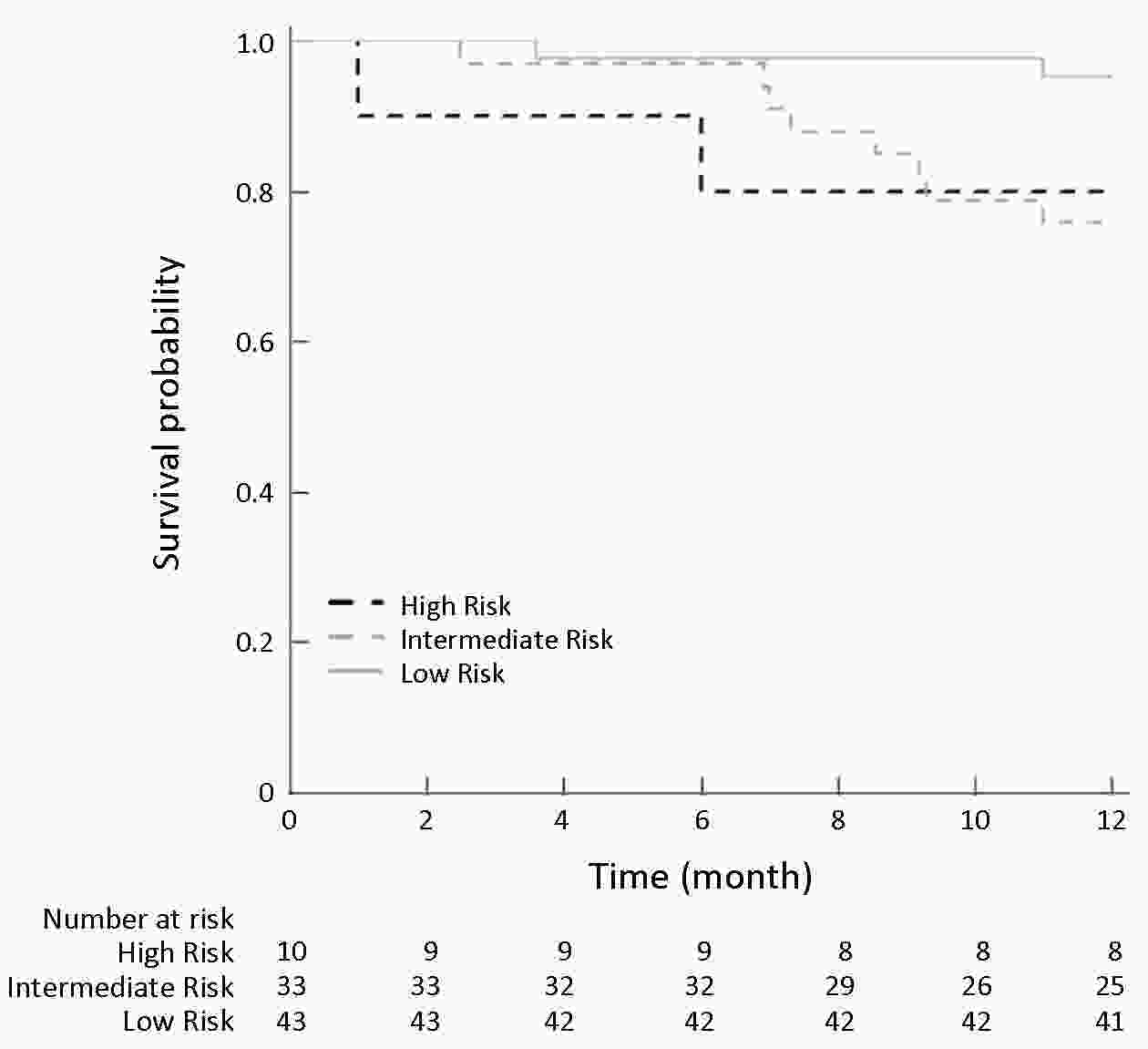
ObjectiveThis study aimed to develop a nomogram to predict the 1-year survival of patients with pancreatic cancer who underwent pancreatectomy following neoadjuvant treatment with preoperatively detectable clinical parameters. Extended pancreatectomy is necessary to achieve complete tumor removal in borderline resectable and locally advanced pancreatic cancer. However, it increases postoperative morbidity and mortality rates, and should be balanced with potential benefit of long-term survival. MethodsThe medical records of patients who underwent pancreatectomy following neoadjuvant treatment from January 2005 to December 2016 at Severance Hospital were retrospectively reviewed. Medical records were collected from five international institutions from Japan and Singapore for external validation. ResultsA total of 113 patients were enrolled. The nomogram for predicting 1-year disease-specific survival was created based on 5 clinically detectable preoperative parameters as follows: age (year), symptom (no/yes), tumor size at initial diagnostic stage (cm), preoperative serum carbohydrate antigen (CA) 19-9 level after neoadjuvant treatment (<34/≥34 U/mL), and planned surgery [pancreaticoduodenectomy (PD) (pylorus-preserving PD)/distal pancreatectomy (DP)/total pancreatectomy]. Model performance was assessed for discrimination and calibration. The calibration plot showed good agreement between actual and predicted survival probabilities; the the Greenwood-Nam-D’Agostino (GND) goodness-of-fit test showed that the model was well calibrated (χ2=8.24, P=0.5099). A total of 84 patients were used for external validation. When correlating actual disease-specific survival and calculated 1-year disease-specific survival, there were significance differences according to the calculated probability of 1-year survival among the three groups (P=0.044). ConclusionsThe developed nomogram had quite acceptable accuracy and clinical feasibility in the decision-making process for the management of pancreatic cancer.
2020, 32(1): 115-128.
doi: 10.21147/j.issn.1000-9604.2020.01.13
Abstract:
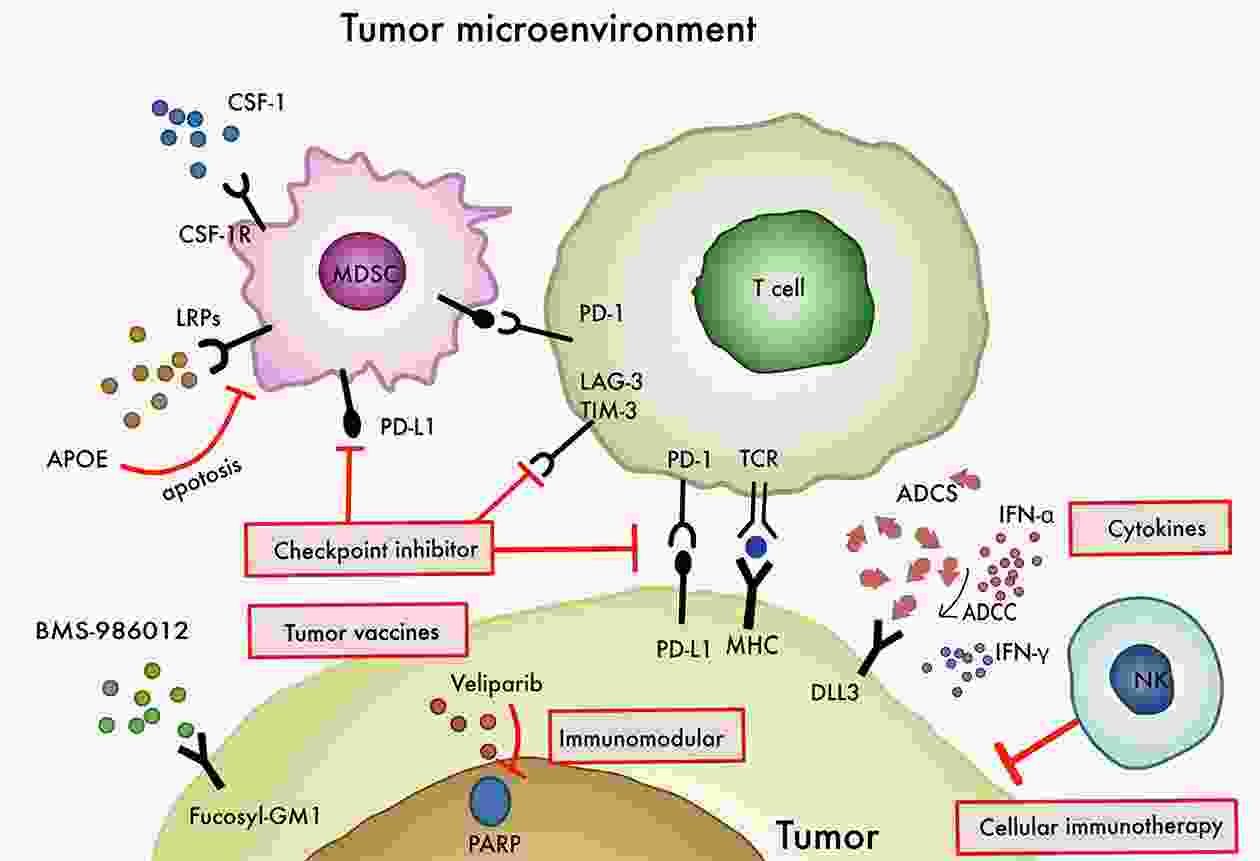
Small cell lung cancer (SCLC) is a highly lethal disease, characterized by early metastasis and rapid growth, and no effective treatment after relapse. Etoposide-platinum (EP) combination has been the backbone therapy of SCLC over the past 30 years. It is extremely urgent and important to seek new therapies for SCLC. In the past 5 years, immunotherapy, such as immune checkpoint inhibitors programmed cell death protein-1 (PD-1), cytotoxic T lymphocyte associatedprotein-4 (CTLA-4), has made remarkable achievements in the treatment of patients with SCLC, and it has become the first-line option for the treatment of some patients. Some traditional chemotherapeutic drugs or targeted drugs, such as alkylating agent temozolomide and transcription inhibitor lurbinectedin, have been found to have immunomodulatory effects and are expected to become new immunotherapeutic agents. In this study, we aimed to review the efficacy of new treatments for SCLC and discuss the current challenges and application prospect in the treatment of SCLC patients.
Small cell lung cancer (SCLC) is a highly lethal disease, characterized by early metastasis and rapid growth, and no effective treatment after relapse. Etoposide-platinum (EP) combination has been the backbone therapy of SCLC over the past 30 years. It is extremely urgent and important to seek new therapies for SCLC. In the past 5 years, immunotherapy, such as immune checkpoint inhibitors programmed cell death protein-1 (PD-1), cytotoxic T lymphocyte associatedprotein-4 (CTLA-4), has made remarkable achievements in the treatment of patients with SCLC, and it has become the first-line option for the treatment of some patients. Some traditional chemotherapeutic drugs or targeted drugs, such as alkylating agent temozolomide and transcription inhibitor lurbinectedin, have been found to have immunomodulatory effects and are expected to become new immunotherapeutic agents. In this study, we aimed to review the efficacy of new treatments for SCLC and discuss the current challenges and application prospect in the treatment of SCLC patients.

 Abstract
Abstract FullText HTML
FullText HTML PDF 579KB
PDF 579KB