2020 Vol.32(2)
Display Mode: |
2020, 32(2): 129-139.
doi: 10.21147/j.issn.1000-9604.2020.02.01
Abstract:
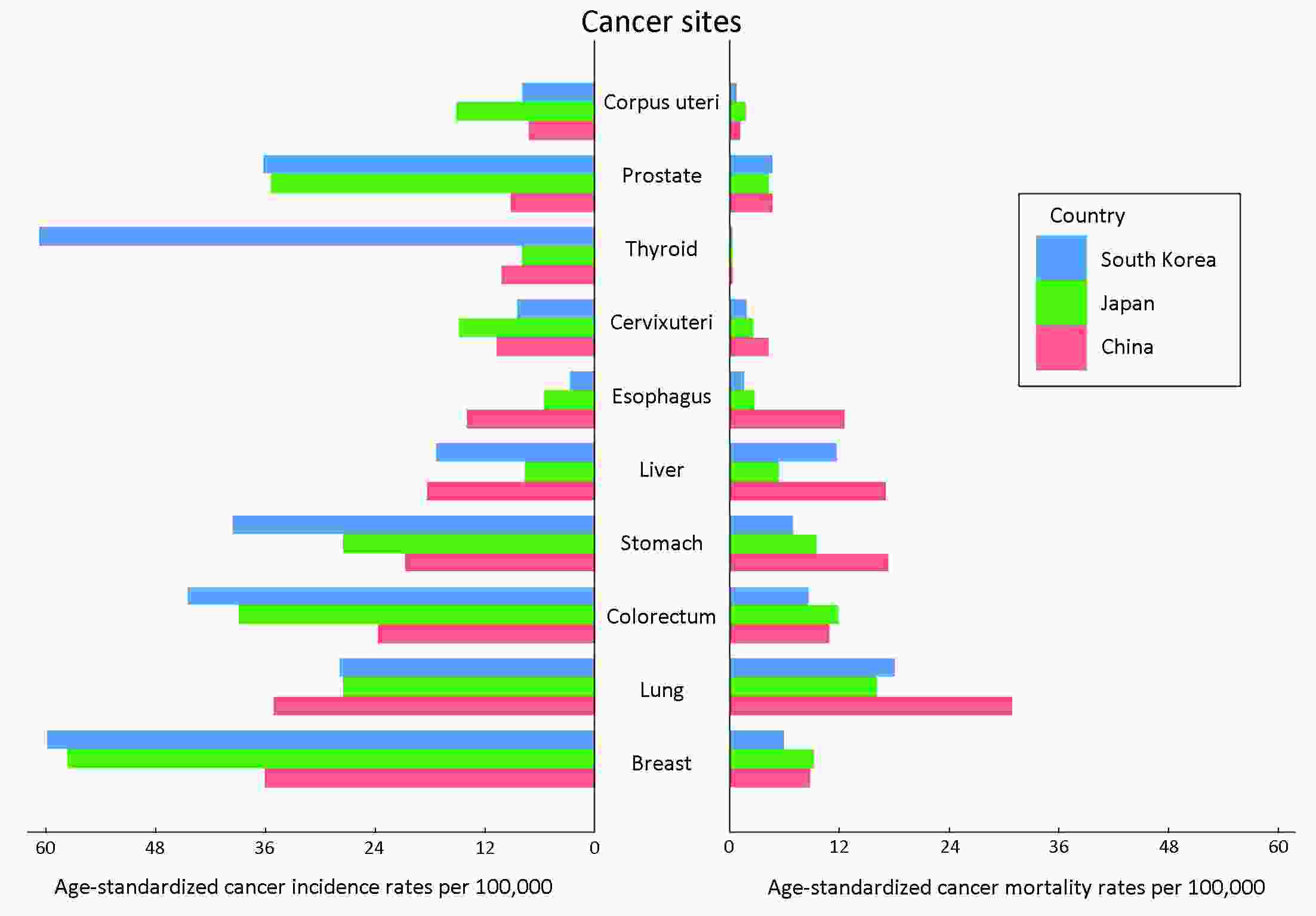
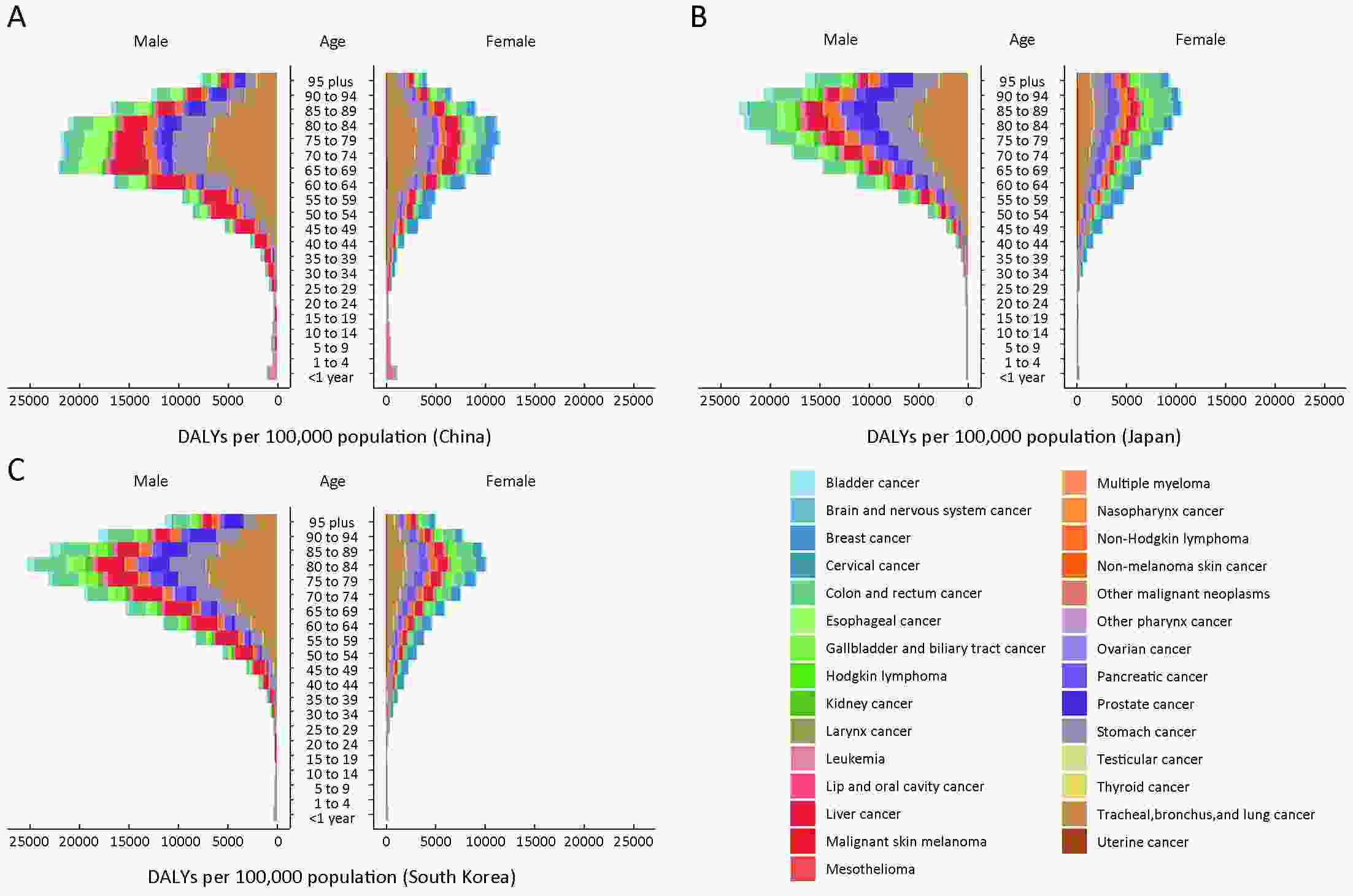
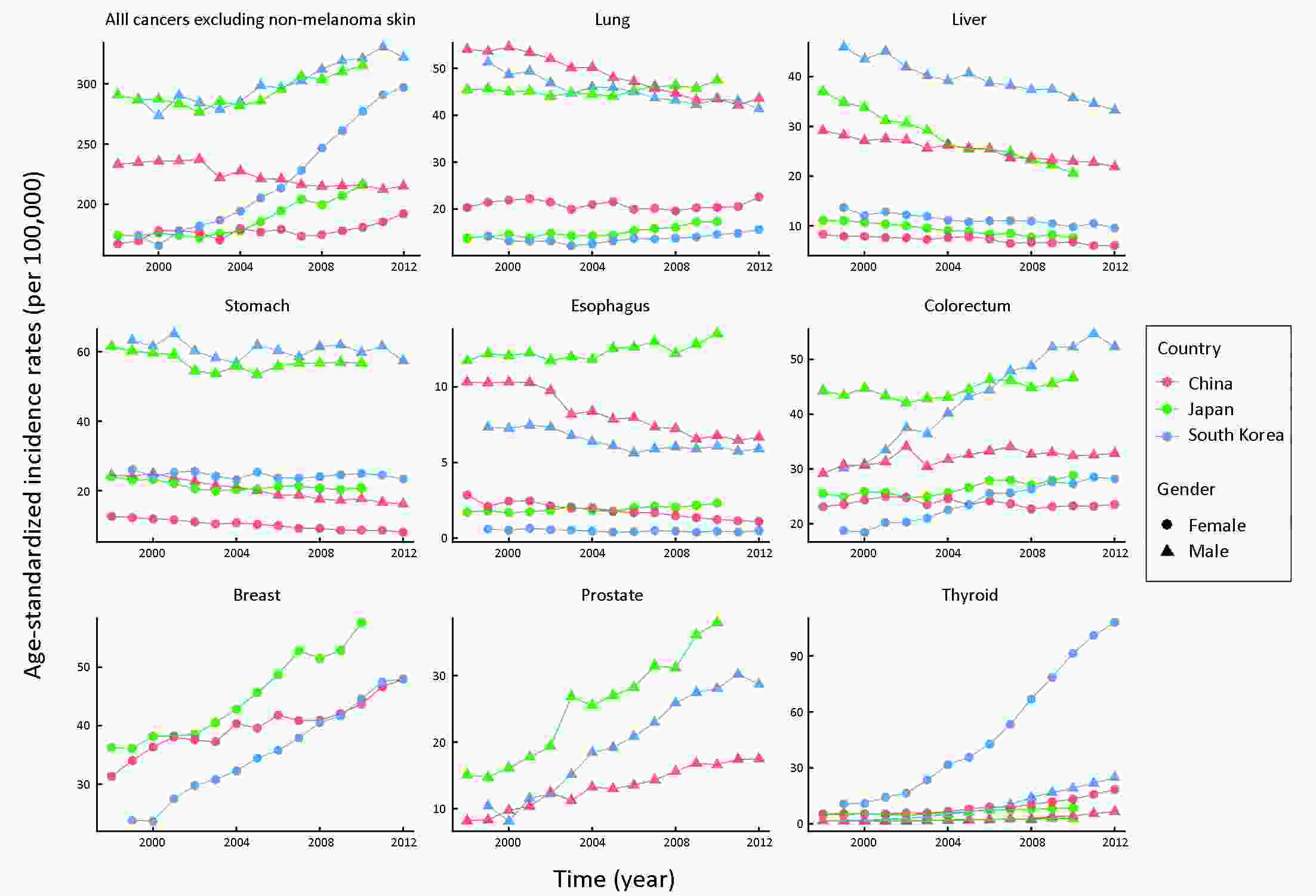
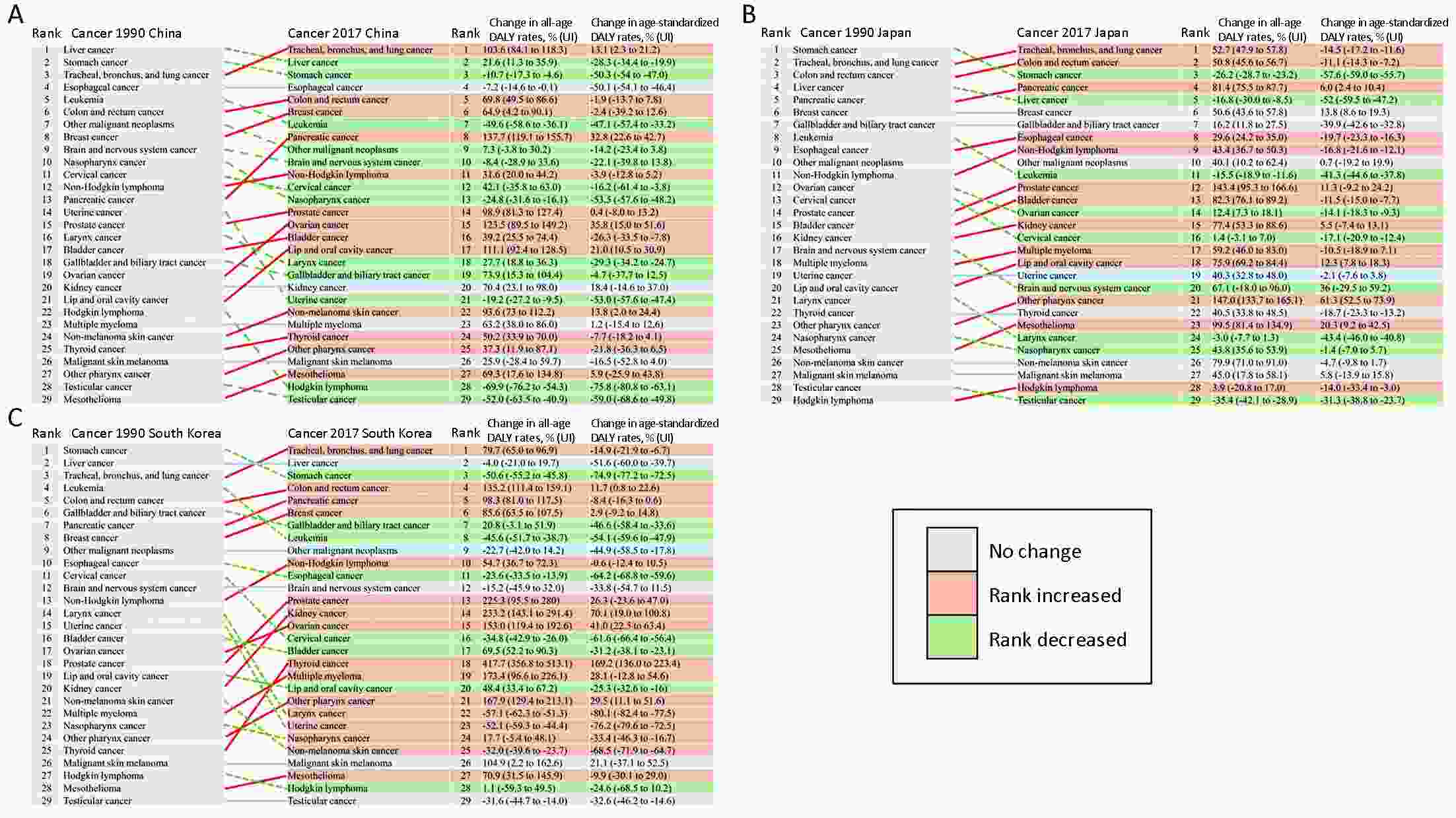
ObjectiveTo summarize the cancer burden and trends in China, compare the differences among China, Japan, and South Korea and discuss possible causes of the disparities. MethodsIncidence and mortality data were extracted from the online cancer database including the GLOBOCAN 2018 and the Global Burden of Disease Study 2017. Trend analysis was conducted using the join-point analysis, and annual percent changes were calculated. ResultsCancers resulted in approximately 62.9 million disability-adjusted life years (DALYs) in China in 2017. Lung cancer had the greatest contribution, followed by liver cancer, stomach cancer, and esophageal cancer. The trajectory of progress in the reduction of liver and stomach cancers was observed in China. However, China still faced a heavy burden of lung cancer and a growing burden of cancers related to westernized lifestyle such as colorectal cancer, while Japan and South Korea have achieved reductions in colorectal cancer and lung cancer, respectively. Besides, China had a lower age-standardized cancer incidence rate but higher cancer mortality and DALY rates than Japan and South Korea. ConclusionsChina is in the cancer transition stage with a rising burden of colorectal, prostate, and breast cancers along with a heavy burden of lung and upper digestive tract cancers. Taking into consideration the effectiveness of screening and tobacco control in Japan and South Korea, improvement in the current tobacco control policy and cancer screening systems may contribute to cancer control in China.
2020, 32(2): 140-148.
doi: 10.21147/j.issn.1000-9604.2020.02.02
Abstract:
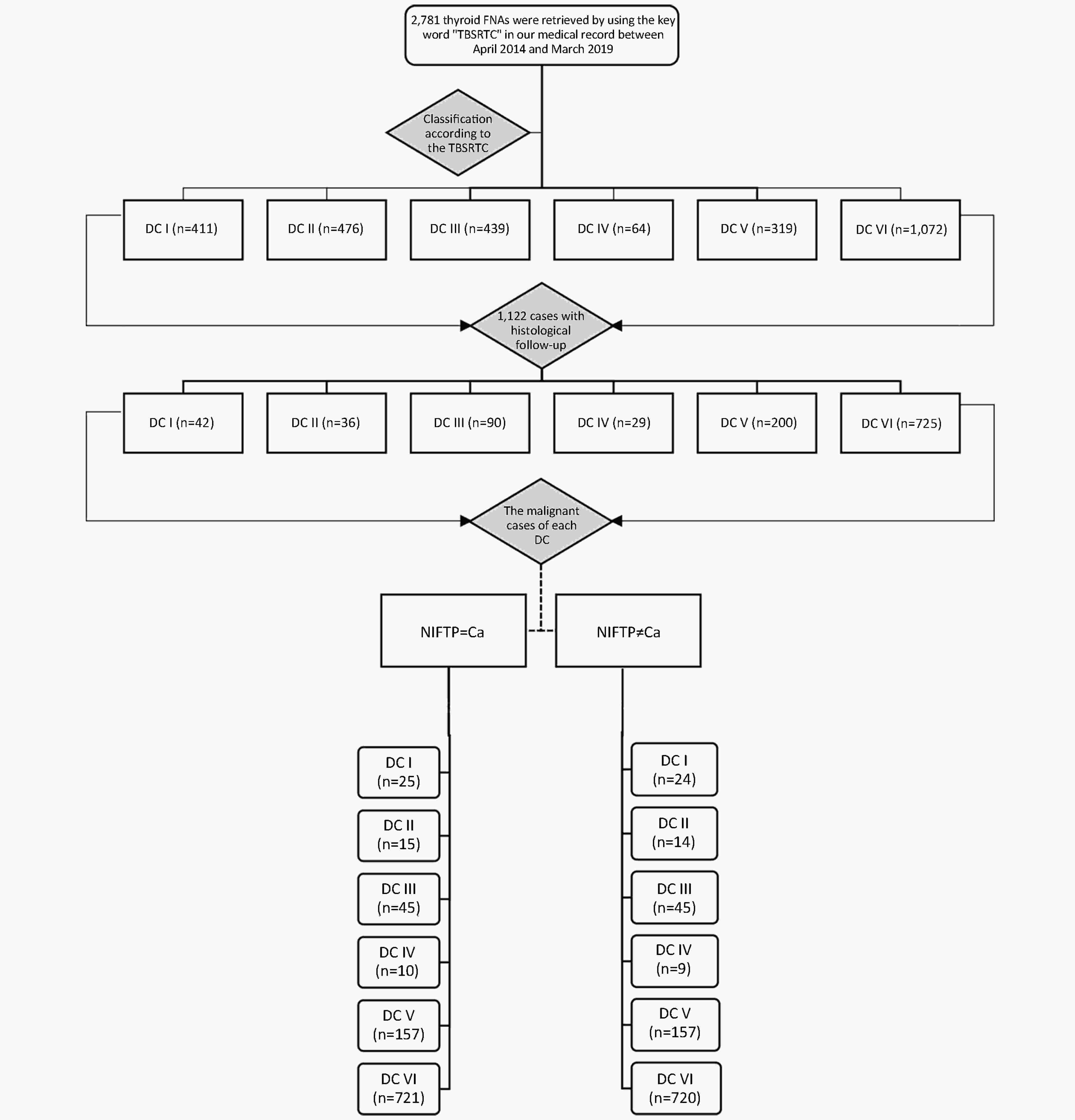
ObjectiveTo evaluate the diagnostic utility of The Bethesda System for Reporting Thyroid Cytology (TBSRTC) at Peking University Cancer Hospital, the incidence of noninvasive follicular thyroid neoplasms with papillary-like nuclear features (NIFTP), and the impact of reclassification on cytopathological outcomes. MethodsWe performed a retrospective study of thyroid fine-needle aspiration (FNA) cases between April 2014 and March 2019. The FNA results were classified according to TBSRTC. Post-surgery histological findings were followed up. ResultsA total of 2,781 thyroid FNAs were performed. The incidences of the 6 diagnostic categories (DCs I−VI) were 14.8%, 17.1%, 15.8%, 2.3%, 11.6% and 38.5%, respectively. A total of 1,122 patients (40.3%) had corresponding histological results. NIFTP accounted for 0.4% of papillary thyroid carcinoma (PTC) cases, and there was no significant difference in the risk of malignancy (ROM) for each TBSRTC DC between “NIFTP=carcinoma (Ca)” and “NIFTP≠Ca”. When “NIFTP=Ca”, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of TBSRTC were 98.0%, 84.0%, 99.4%, 58.3%, and 97.5%, respectively. When “NIFTP≠Ca”, the sensitivity, specificity, PPV, NPV and accuracy of the TBSRTC were 98.1%, 81.5%, 99.3%, 61.1%, and 97.5%, respectively. ConclusionsTBSRTC is effective in the preoperative diagnosis of thyroid nodules in Peking University Cancer Hospital. The impact of the reclassification of NIFTP on cytopathological outcomes is limited because of its low incidence, and the revised ROMs are not suitable for Asian patients.
2020, 32(2): 149-162.
doi: 10.21147/j.issn.1000-9604.2020.02.03
Abstract:
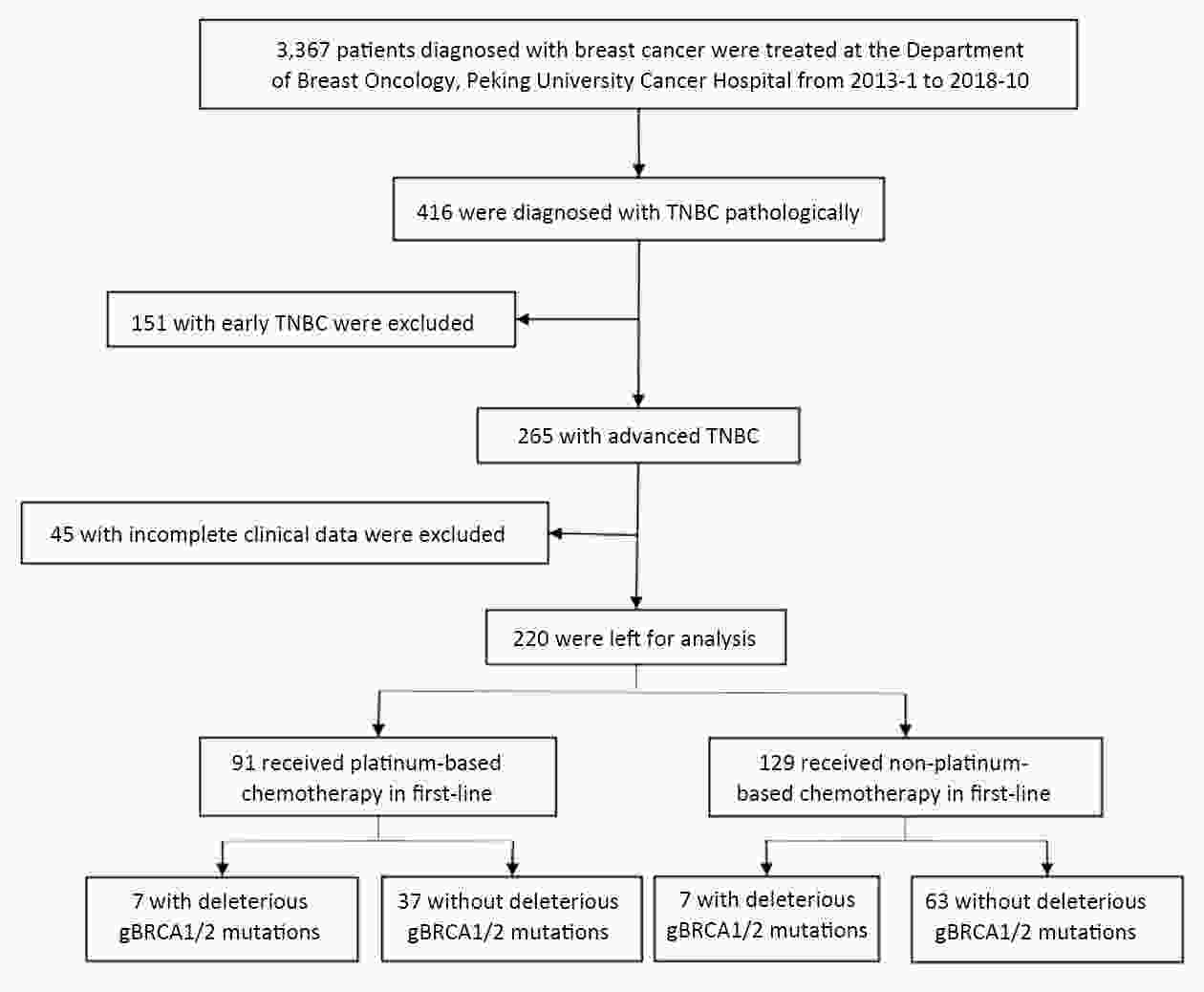
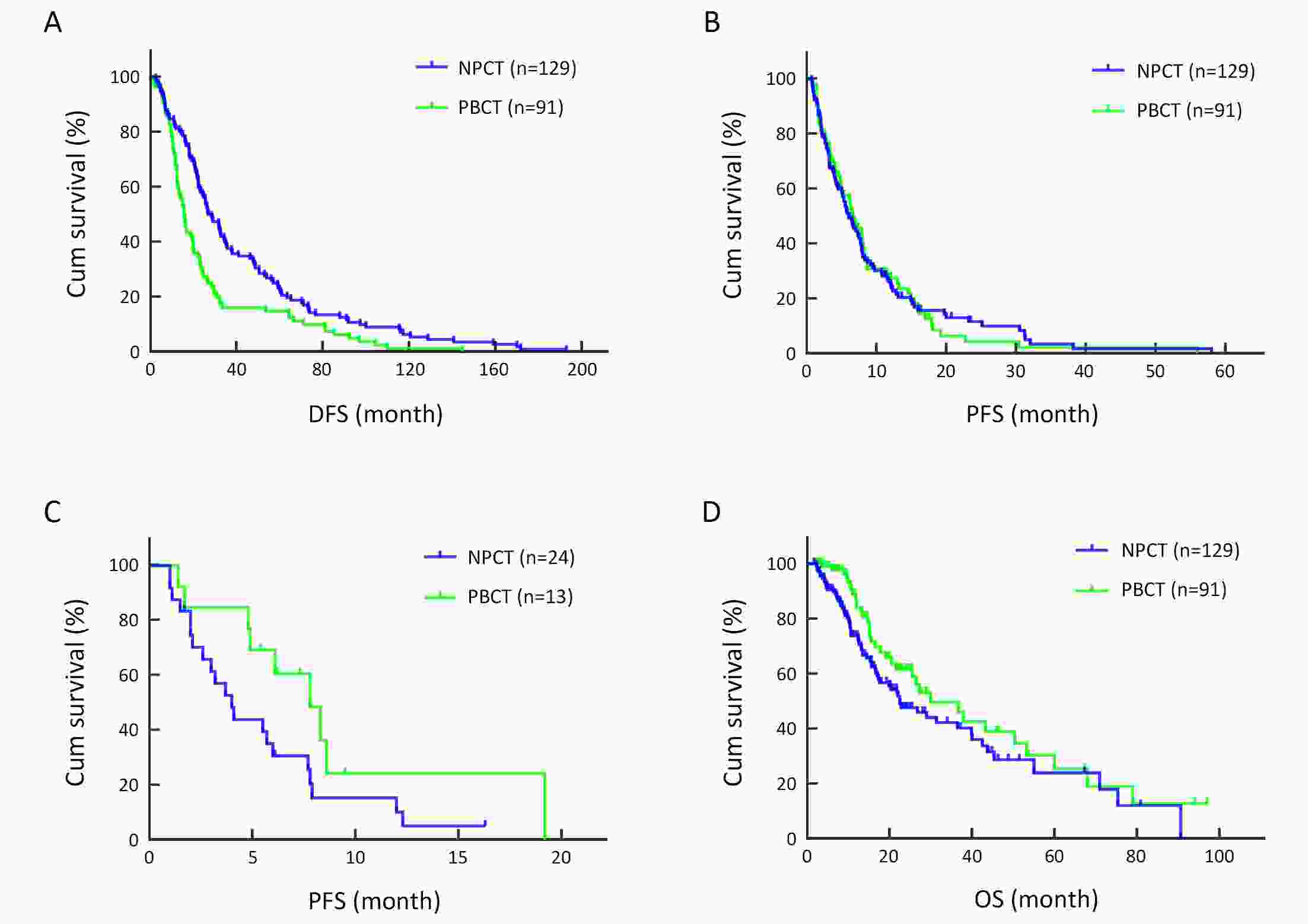
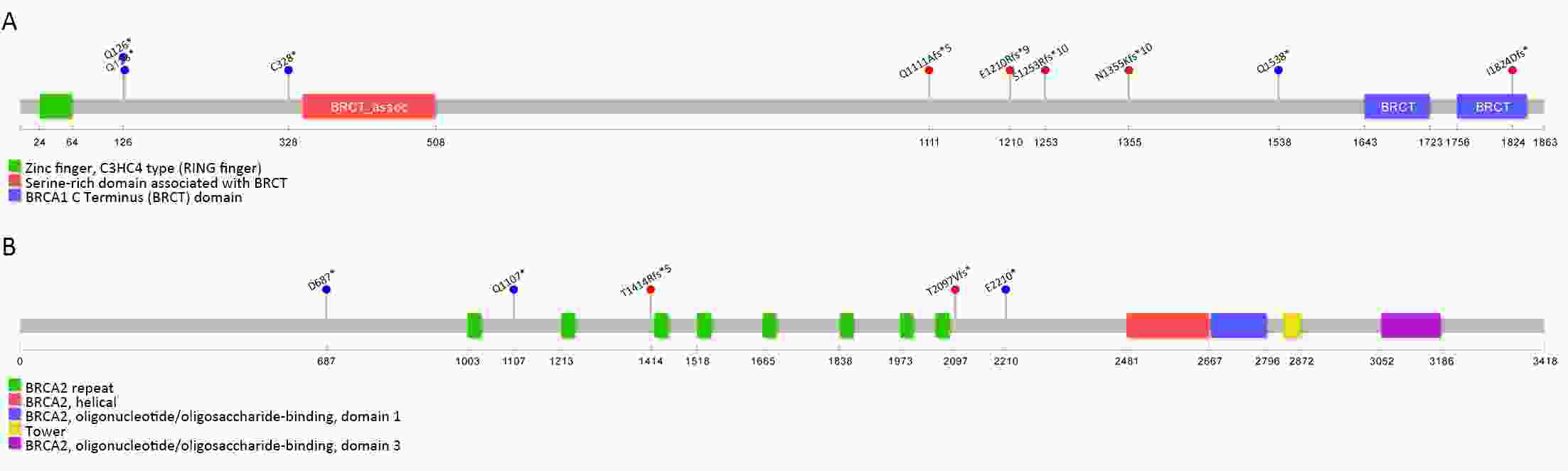
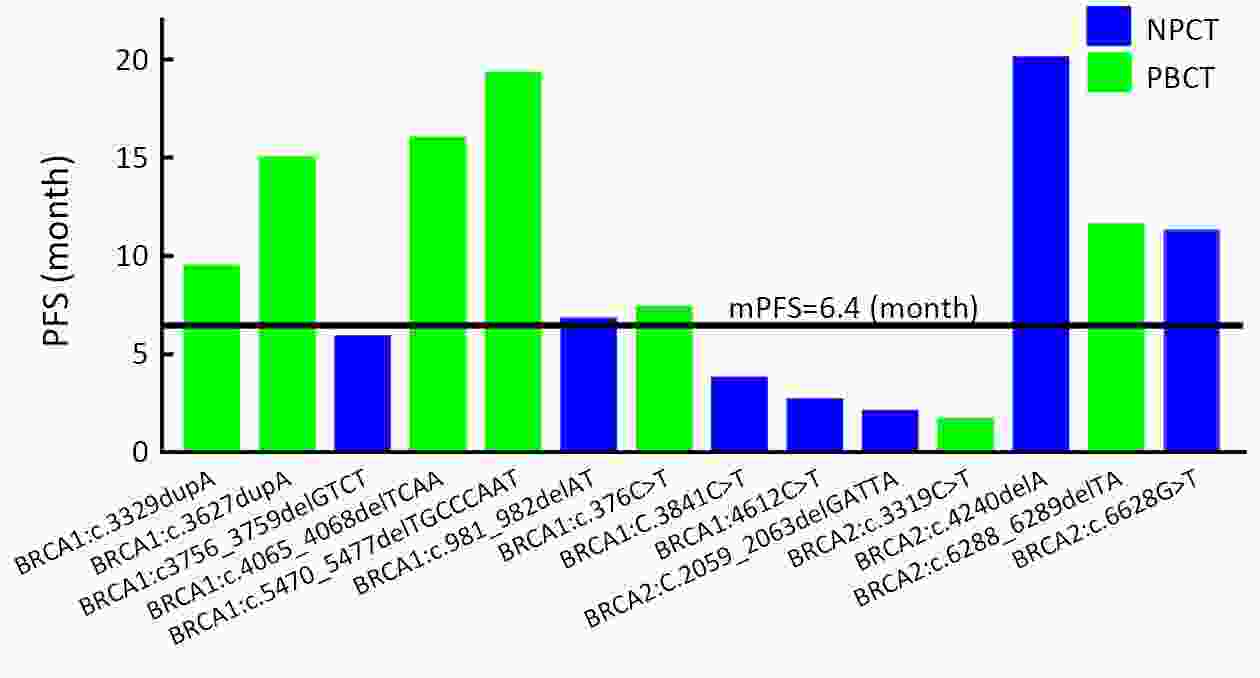
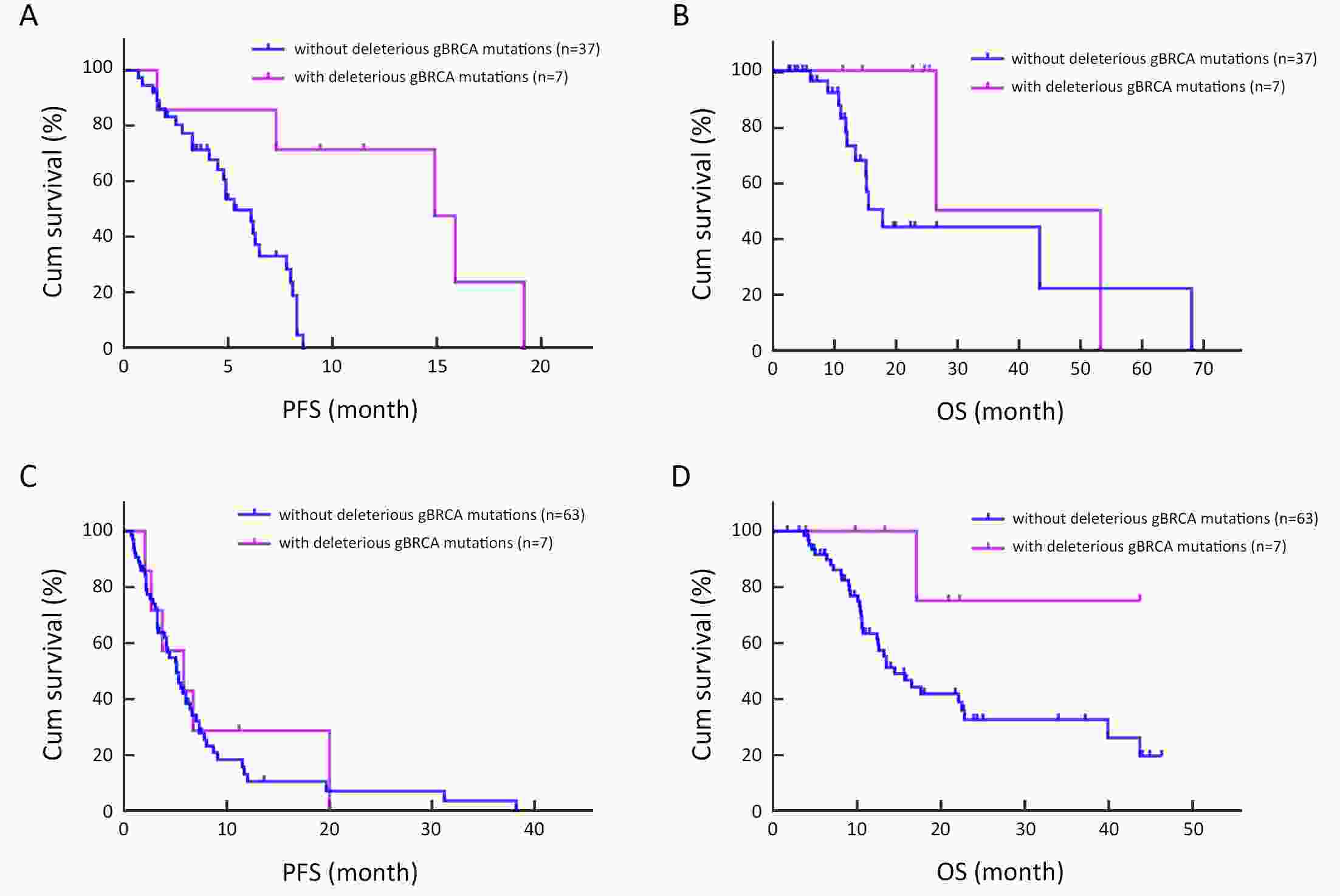
ObjectiveTo compare the efficacy of platinum- and non-platinum-based regimens as first-line treatment for advanced triple-negative breast cancer (TNBC) and analyze the relationship between their efficacy and BRCA gene status. MethodsRetrospectively analyze clinical data of 220 patients diagnosed pathologically with advanced TNBC and treated at the Department of Breast Oncology, Peking University Cancer Hospital from 2013 to 2018 and evaluate the efficacy of chemotherapy. A total of 114 patients had BRCA1/2 gene tested by next generation sequencing (NGS) using peripheral blood, and we analyzed the correlation between their efficacy and BRCA1/2 gene status. ResultsNon-platinum-based chemotherapy (NPCT) was administered to 129 and platinum-based chemotherapy (PBCT) to 91 study patients. The clinical benefit rate (CBR) and median progression-free survival (PFS) were not statistically different between NPCT and PBCT groups. The median overall survival (OS) was 30.0 and 22.5 months for PBCT and NPCT group, respectively [P=0.090, hazard ratios (HR)=0.703]. BRCA status was assessed in 114 patients, 14 of whom had deleterious germline BRCA1/2 (gBRCA) mutations (seven in each group). In PBCT group, the CBR was 85.7% and 35.1% for patients with and without deleterious gBRCA mutations, respectively (P=0.039). The median PFS were 14.9 and 5.3 months and median OS were 26.5 and 15.5 months for patients with and without deleterious gBRCA mutations, respectively (P=0.001, P=0.161, respectively). Patients in PBCT group had significantly greater rates of grade 3−4 anemia (5.5% vs. 0%) and thrombocytopenia (8.8% vs. 0%), whereas palmar-plantar erythrodysesthesia (12.4% vs. 0%) and peripheral neuropathy (8.6% vs. 1.1%) occurred more frequently in NPCT group. ConclusionsPlatinum-based regimens are more effective in patients with deleterious gBRCA mutations, but no difference in patients without BRCA gene mutations, so non-platinum is an option in patients without BRCA gene mutations considering the toxicity and side effect. And we recommend that patients with advanced TNBC should have BRCA gene test.
2020, 32(2): 163-174.
doi: 10.21147/j.issn.1000-9604.2020.02.04
Abstract:
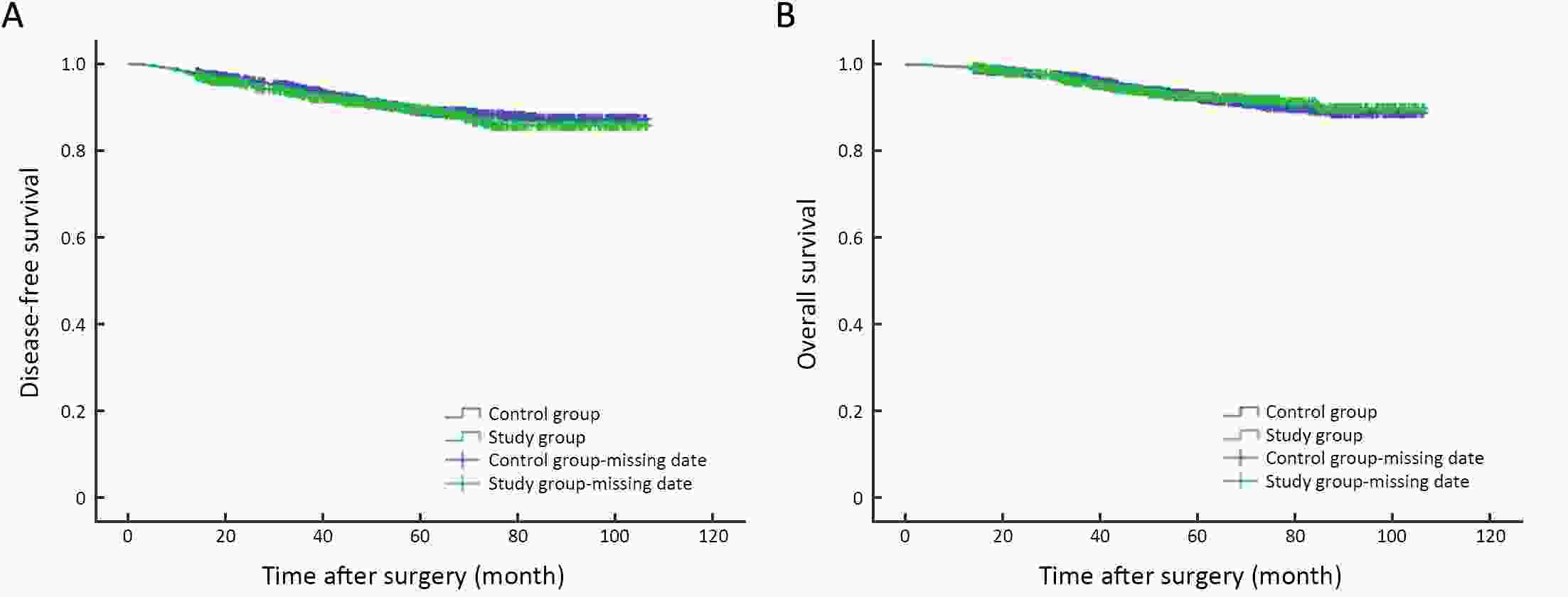
ObjectiveTo investigate the clinicopathological characteristics and prognostic factors of early-stage breast cancer patients with indications for breast cancer susceptibility genes 1/2 (BRCA1/2) genetic testing in China. MethodsBased on the indication criteria for BRCA genetic testing specified in the National Comprehensive Cancer Network (NCCN) clinical practice guidelines in oncology, genetic/familial high-risk assessment: Breast and ovarian (Version 2. 2019), a retrospective analysis was performed on patients with early-stage invasive breast cancer treated at Breast Disease Center, Peking University First Hospital between January 2008 and December 2016. Clinicopathological characteristics of all patients were analyzed, and prognoses were calculated using the Kaplan-Meier method and a Cox proportionate hazards model. ResultsA total of 906 early-stage breast cancer patients who had indications for BRCA genetic testing and had complete clinicopathological data and follow-up information were included in the study group, accounting for 34.7% of all breast cancer patients treated in Breast Disease Center, Peking University First Hospital during the study period. Compared with breast cancer patients without indications for BRCA genetic testing, the overall survival (OS) and disease-free survival (DFS) of patients with indications were not significantly different. In the study group, patients with premenopausal status, high T stage, lymph node positive, estrogen receptor (ER) negative, Ki-67>20% and presence of a vascular tumor thrombus had worse prognosis. There were more family histories of gastrointestinal cancer in patients with related indications than in patients without such indications. ConclusionsSingle-center data showed that more than 30% of patients with early-stage breast cancer had indications for BRCA genetic testing. There was no prognostic difference in patients with or without indications for BRCA genetic testing. Premenopausal status, high T stage, lymph node positive, ER negative, Ki-67>20%, and presence of a vascular tumor thrombus were associated with poor prognosis.
2020, 32(2): 175-185.
doi: 10.21147/j.issn.1000-9604.2020.02.05
Abstract:
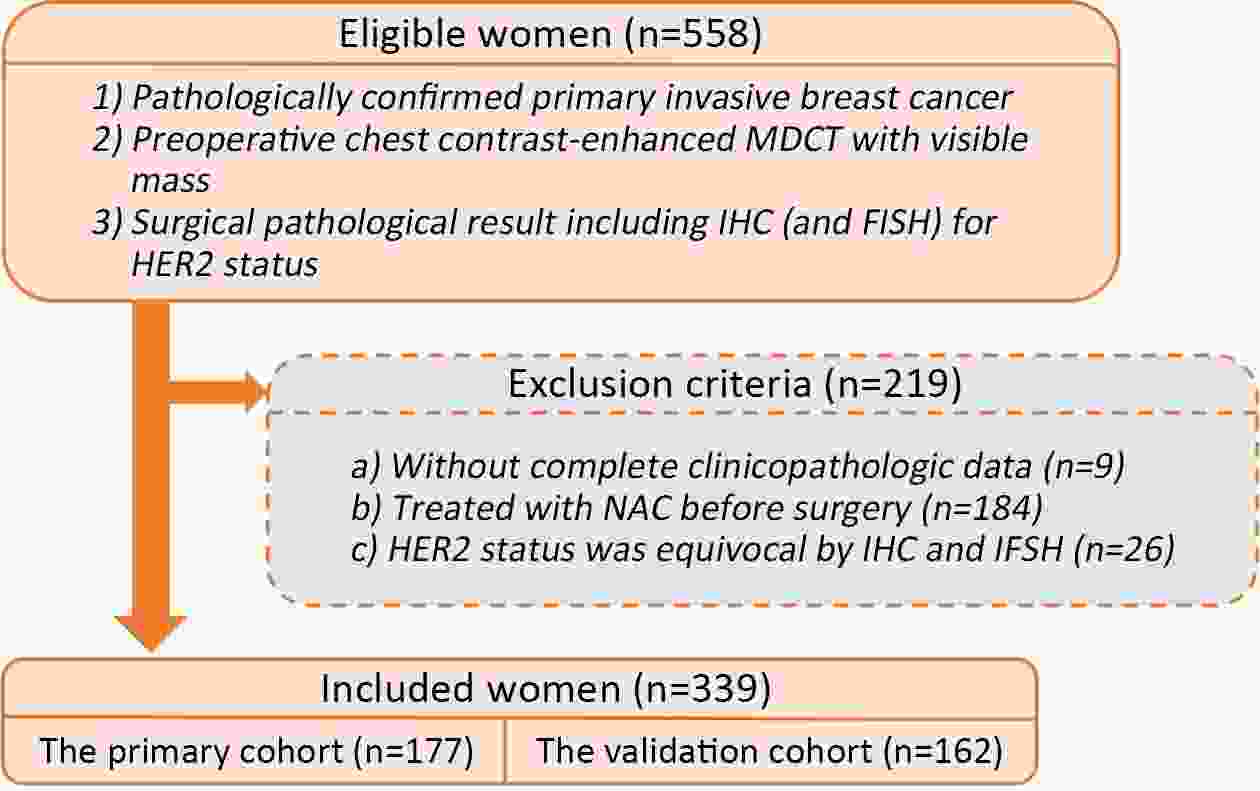
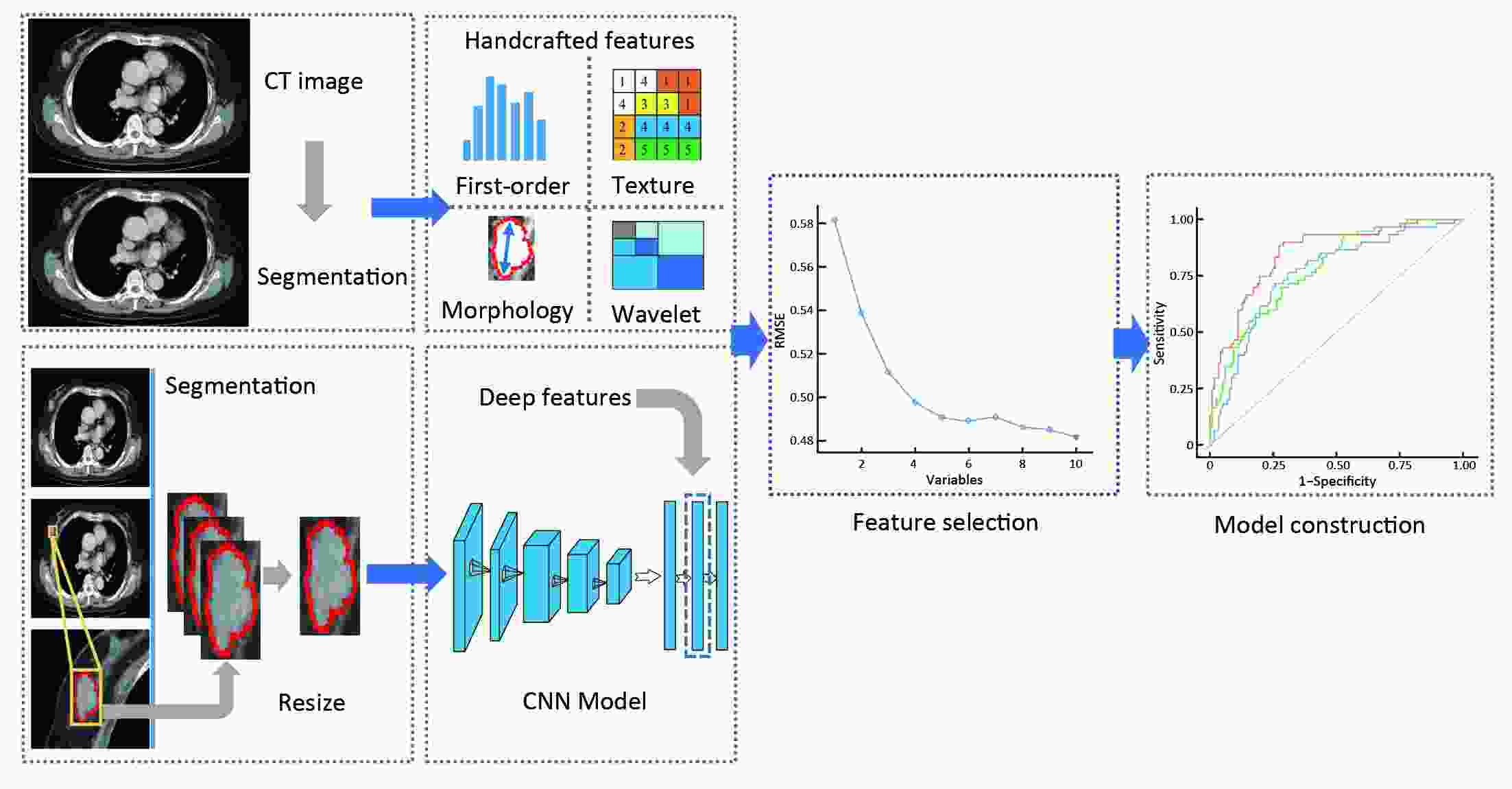
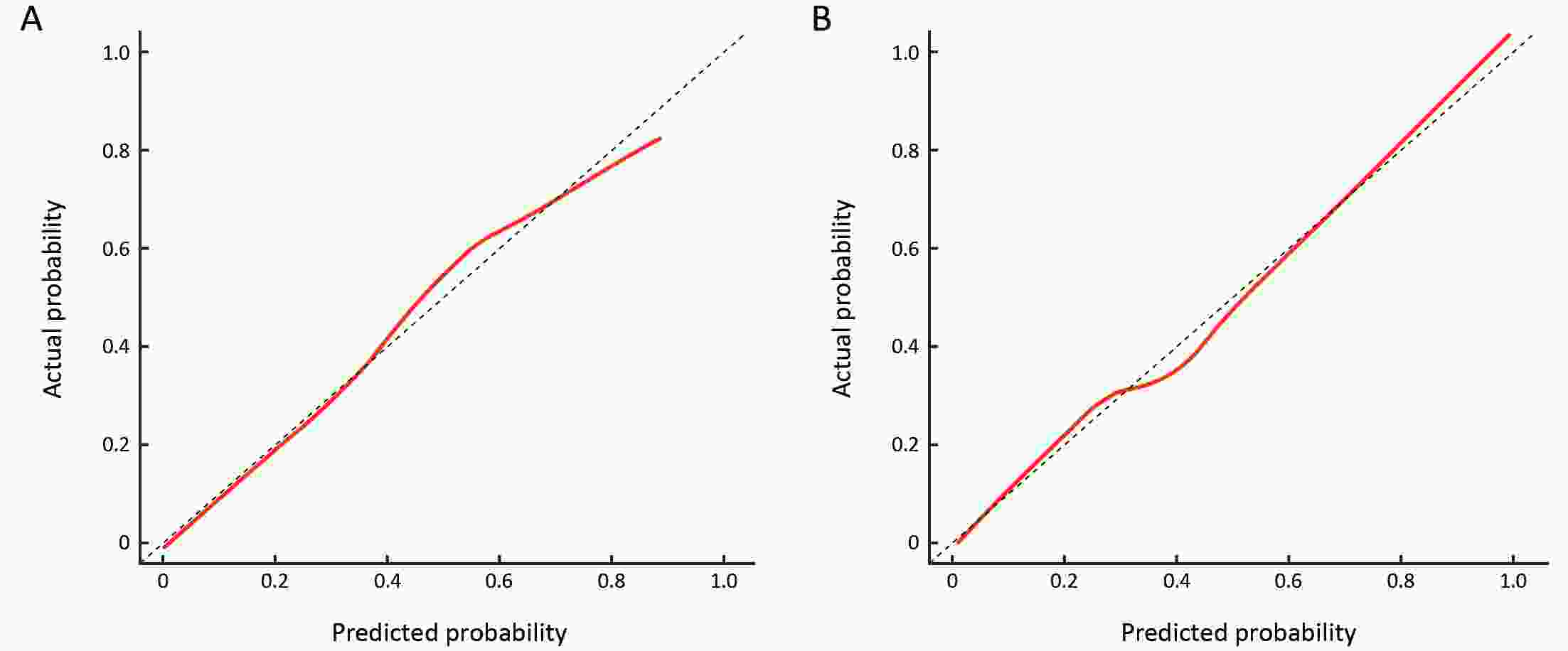
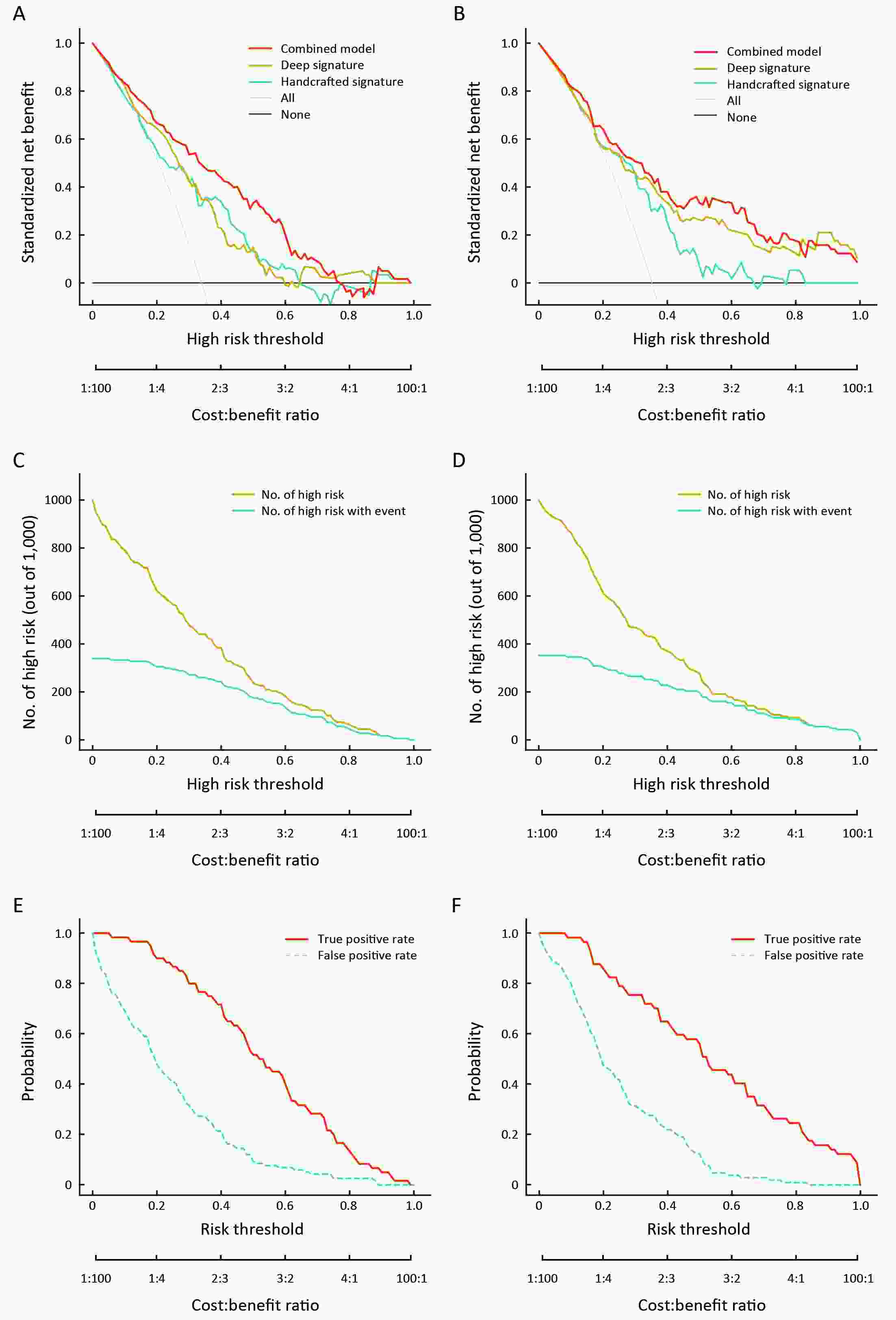
ObjectiveTo evaluate the human epidermal growth factor receptor 2 (HER2) status in patients with breast cancer using multidetector computed tomography (MDCT)-based handcrafted and deep radiomics features. MethodsThis retrospective study enrolled 339 female patients (primary cohort, n=177; validation cohort, n=162) with pathologically confirmed invasive breast cancer. Handcrafted and deep radiomics features were extracted from the MDCT images during the arterial phase. After the feature selection procedures, handcrafted and deep radiomics signatures and the combined model were built using multivariate logistic regression analysis. Performance was assessed by measures of discrimination, calibration, and clinical usefulness in the primary cohort and validated in the validation cohort. ResultsThe handcrafted radiomics signature had a discriminative ability with a C-index of 0.739 [95% confidence interval (95% CI): 0.661−0.818] in the primary cohort and 0.695 (95% CI: 0.609−0.781) in the validation cohort. The deep radiomics signature also had a discriminative ability with a C-index of 0.760 (95% CI: 0.690−0.831) in the primary cohort and 0.777 (95% CI: 0.696−0.857) in the validation cohort. The combined model, which incorporated both the handcrafted and deep radiomics signatures, showed good discriminative ability with a C-index of 0.829 (95% CI: 0.767−0.890) in the primary cohort and 0.809 (95% CI: 0.740−0.879) in the validation cohort. ConclusionsHandcrafted and deep radiomics features from MDCT images were associated with HER2 status in patients with breast cancer. Thus, these features could provide complementary aid for the radiological evaluation of HER2 status in breast cancer.
2020, 32(2): 186-196.
doi: 10.21147/j.issn.1000-9604.2020.02.06
Abstract:
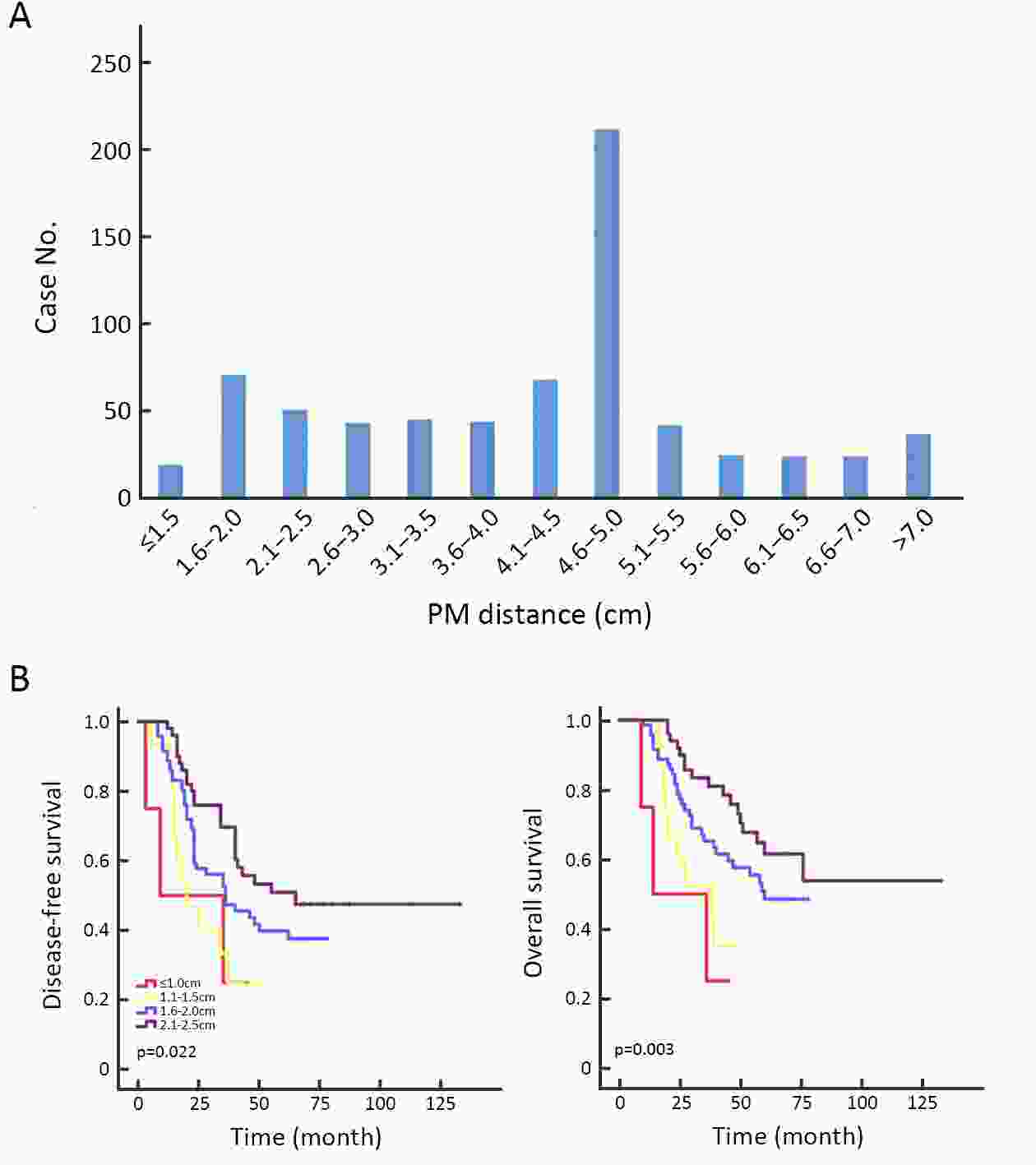
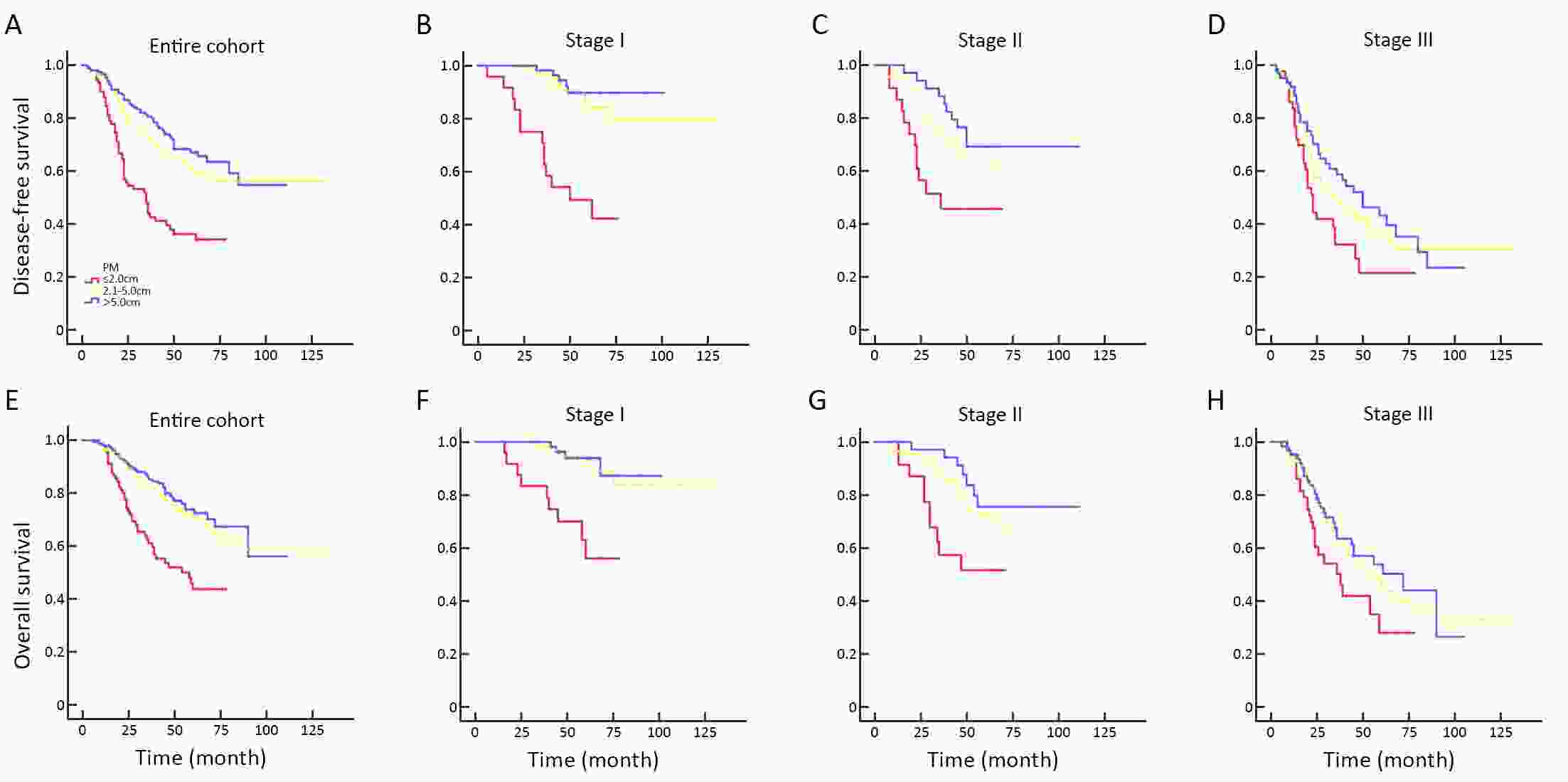
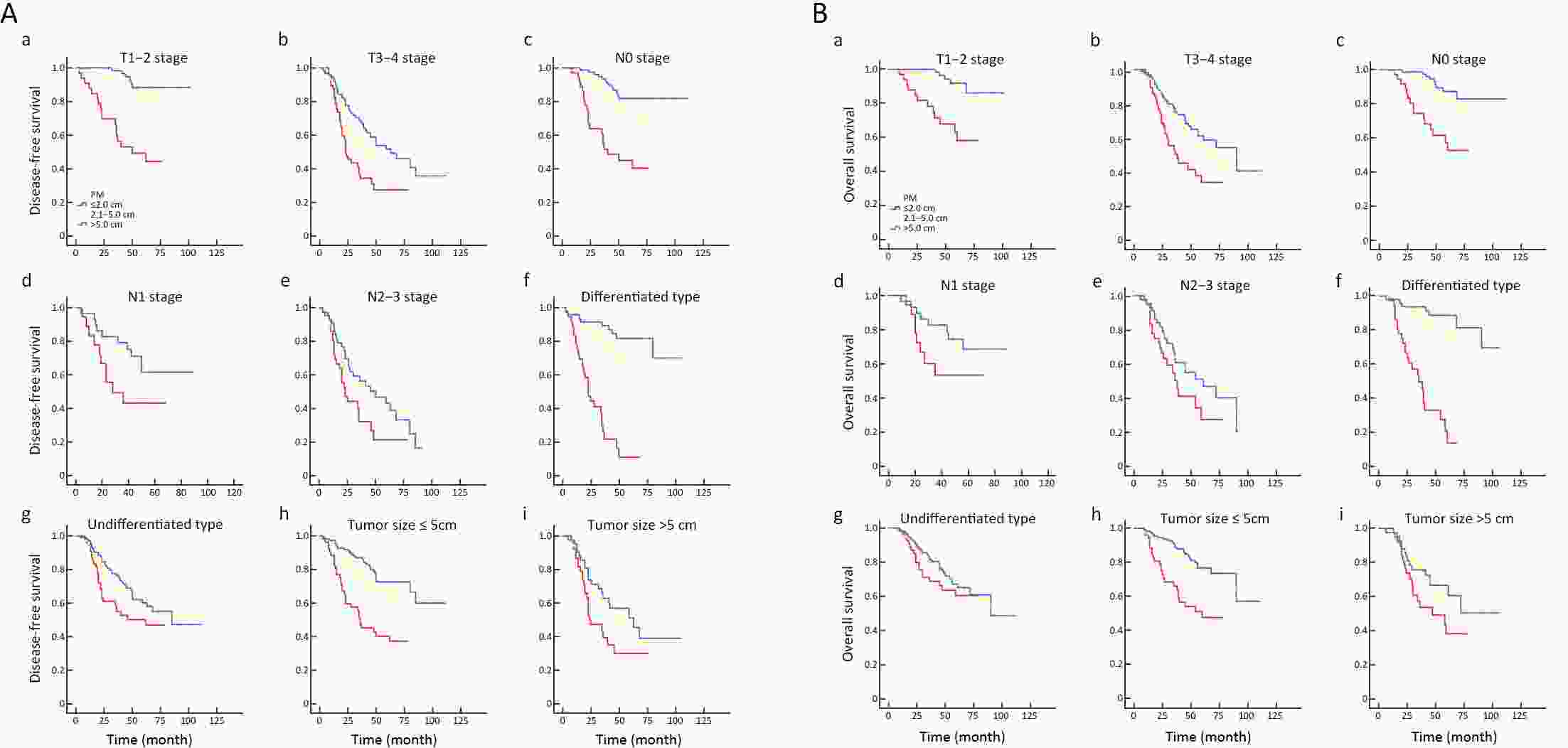
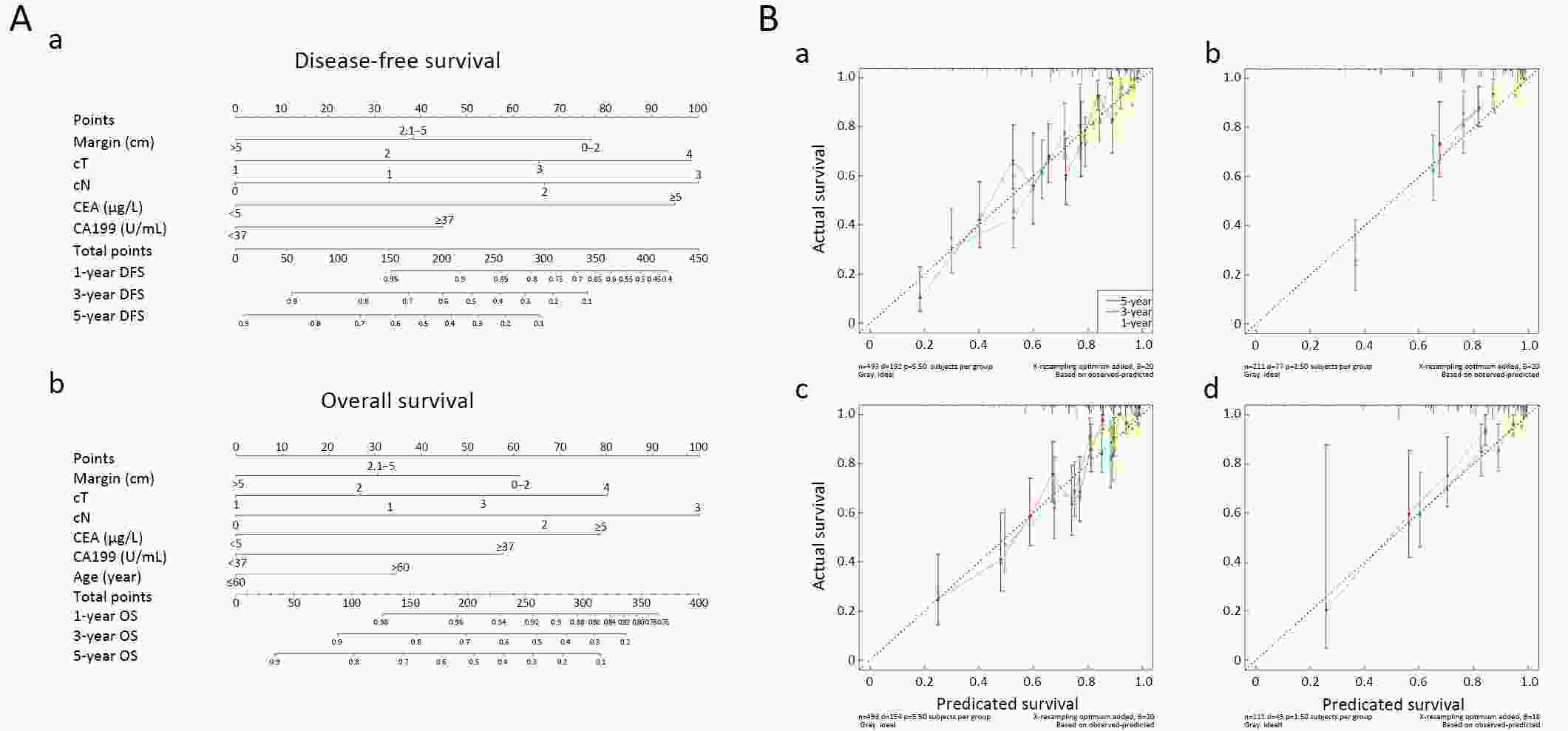
ObjectiveThe proximal margin (PM) distance for distal gastrectomy (DG) of gastric cancer (GC) remains controversial. This study investigated the prognostic value of PM distance for survival outcomes, and aimed to combine clinicopathologic variables associated with survival outcomes after DG with different PM distance for GC into a prediction nomogram. MethodsPatients who underwent radical DG from June 2004 to June 2014 at Department of General Surgery, Nanfang Hospital, Southern Medical University were included. The first endpoints of the prognostic value of PM distance (assessed in 0.5 cm increments) for disease-free survival (DFS) and overall survival (OS) were assessed. Multivariate analysis by Cox proportional hazards regression was performed using the training set, and the nomogram was constructed, patients were chronologically assigned to the training set for dates from June 1, 2004 to January 30, 2012 (n=493) and to the validation set from February 1, 2012 to June 30, 2014 (n=211). ResultsAmong 704 patients with pTNM stage I, pTNM stage II, T1−2, T3−4, N0, differentiated type, tumor size ≤5.0 cm, a PM of (2.1−5.0) cm vs. PM≤2.0 cm showed a statistically significant difference in DFS and OS, while a PM>5.0 cm was not associated with any further improvement in DFS and OS vs. a PM of 2.1−5.0 cm. In patients with pTNM stage III, N1, N2−3, undifferentiated type, tumor size >5.0 cm, the PM distance was not significantly correlated with DFS and OS between patients with a PM of (2.1−5.0) cm and a PM≤2 cm, or between patients with a PM >5.0 cm and a PM of (2.1−5.0) cm, so there were no significant differences across the three PM groups. In the training set, the C-indexes of DFS and OS, were 0.721 and 0.735, respectively, and in the validation set, the C-indexes of DFS and OS, were 0.752 and 0.751, respectively. ConclusionsIt is necessary to obtain not less than 2.0 cm of PM distance in early-stage disease, while PM distance was not associated with long-term survival in later and more aggressive stages of disease because more advanced GC is a systemic disease. Different types of patients should be considered for removal of an individualized PM distance intra-operatively. We developed a universally applicable prediction model for accurately determining the 1-year, 3-year and 5-year DFS and OS of GC patients according to their preoperative clinicopathologic characteristics and PM distance.
Analysis and external validation of a nomogram to predict peritoneal dissemination in gastric cancer
2020, 32(2): 197-207.
doi: 10.21147/j.issn.1000-9604.2020.02.07
Abstract:
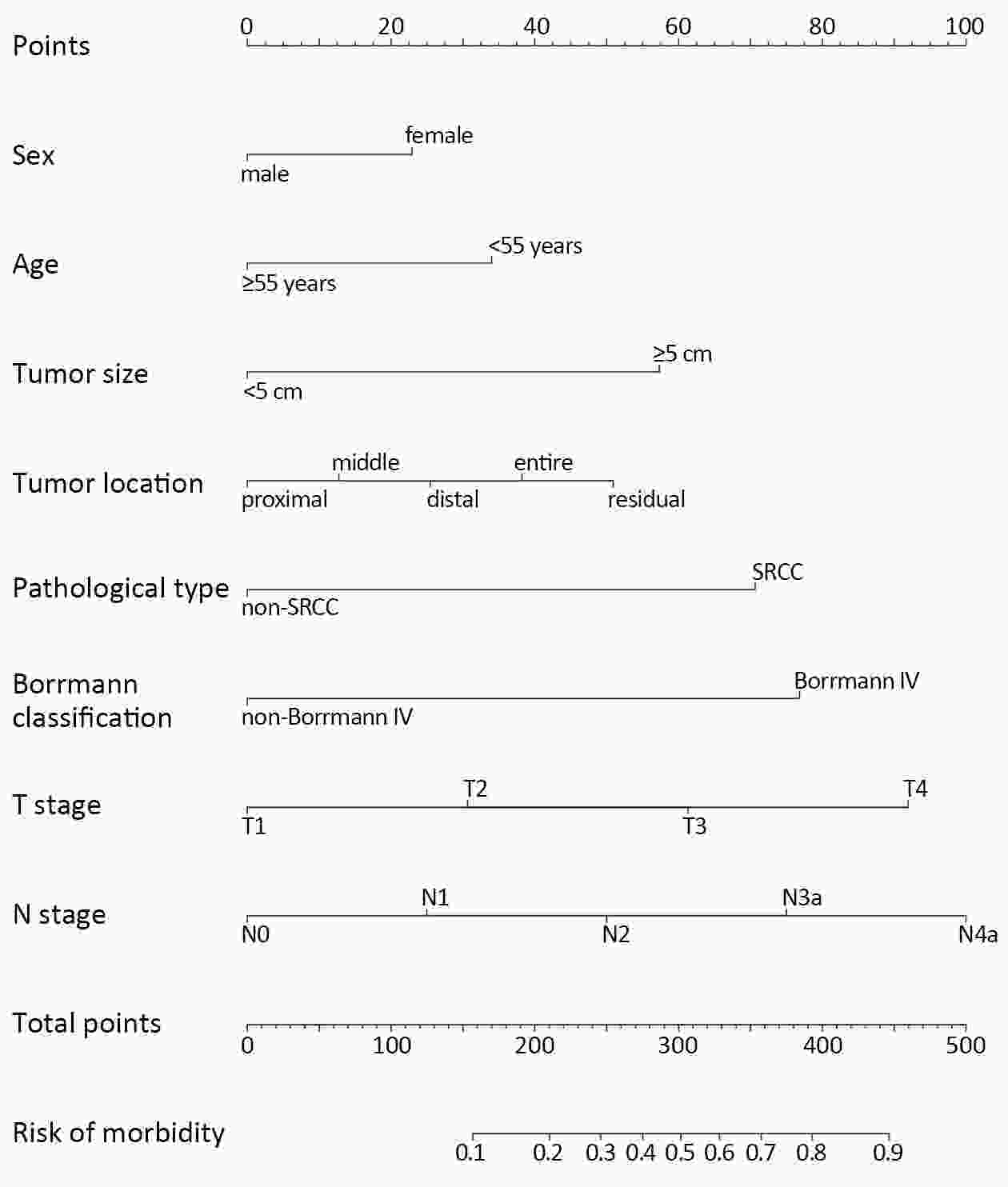
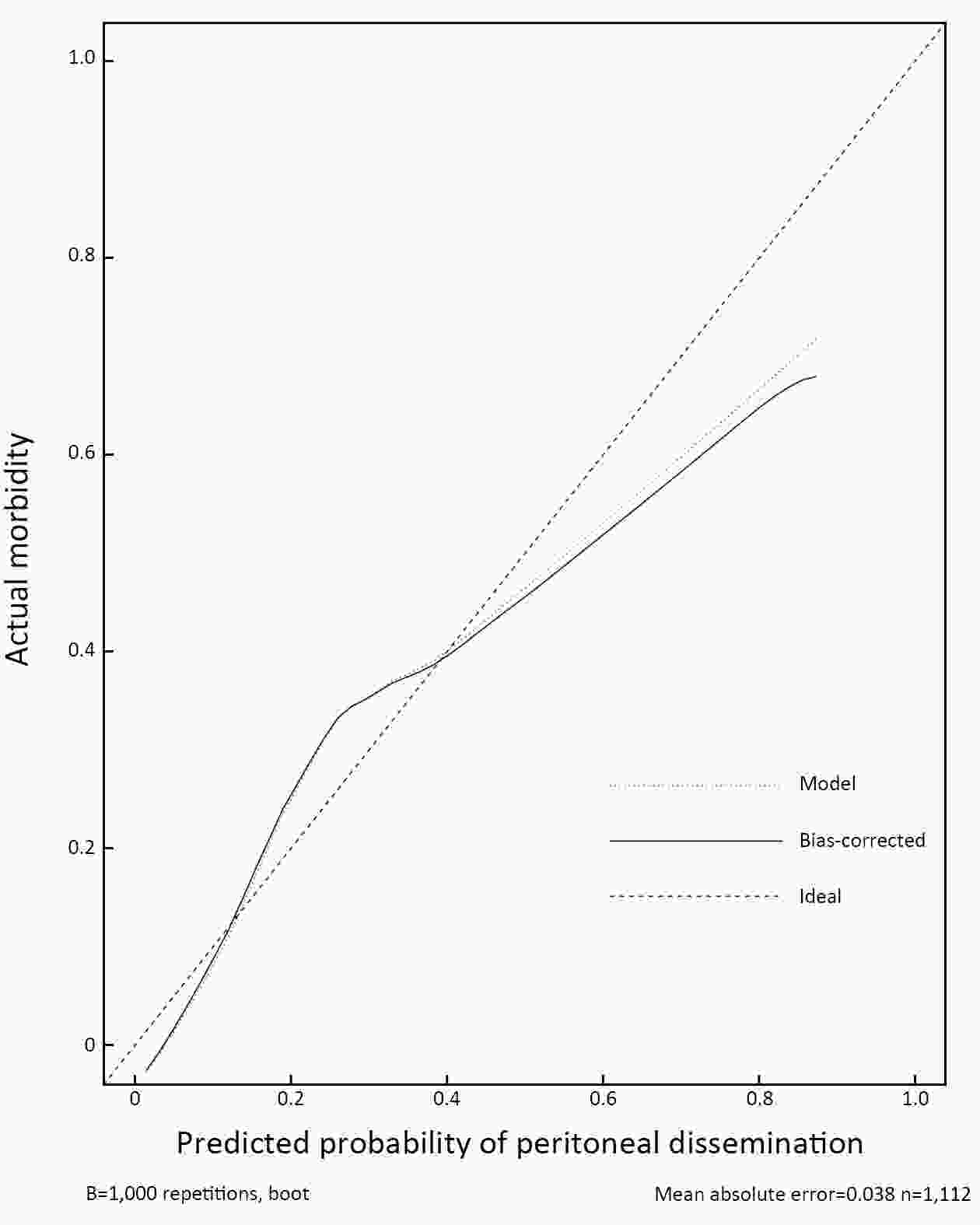
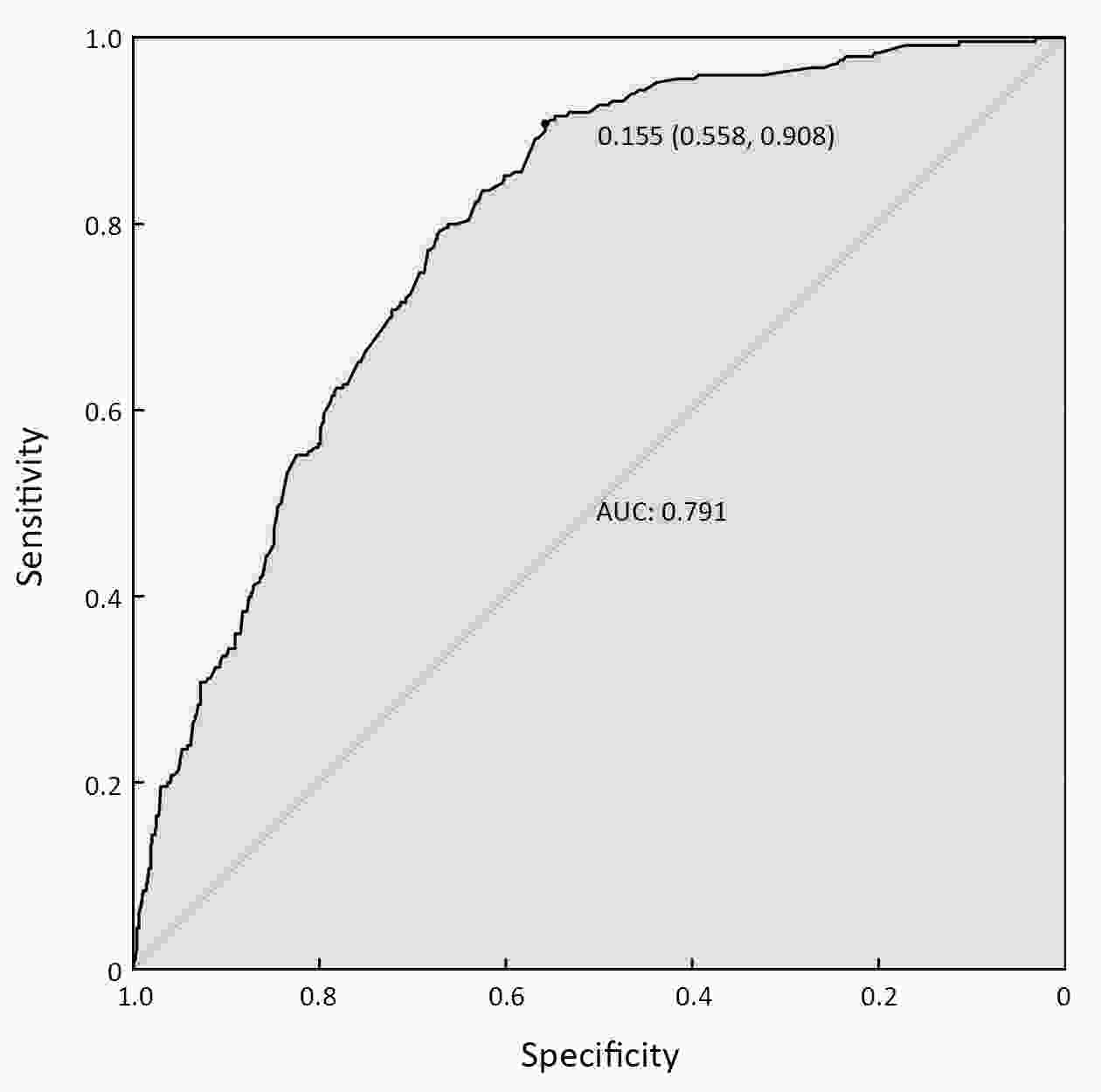
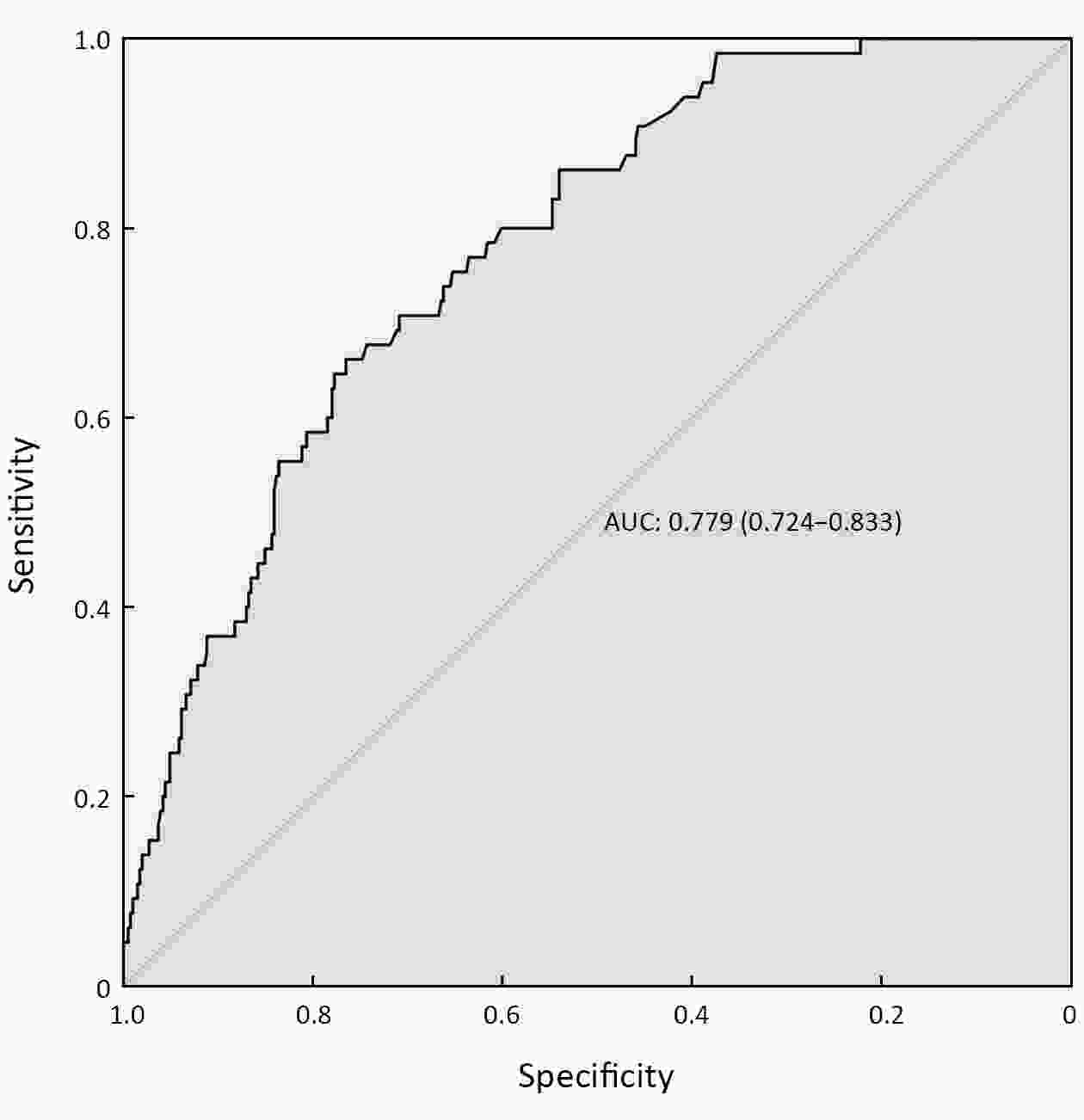
ObjectivePeritoneal dissemination is difficult to diagnose by conventional imaging technologies. We aimed to construct a nomogram to predict peritoneal dissemination in gastric cancer (GC) patients. MethodsWe retrospectively analyzed 1,112 GC patients in Sun Yat-sen University Cancer Center between 2001 and 2010 as the development set and 474 patients from The Sixth Affiliated Hospital, Sun Yat-sen University between 2010 and 2016 as the validation set. The clinicopathological variables associated with gastric cancer with peritoneal dissemination (GCPD) were analyzed. We used logistic regression analysis to identify independent risk factors for peritoneal dissemination. Then, we constructed a nomogram for the prediction of GCPD and defined its predictive value with a receiver operating characteristic (ROC) curve. External validation was performed to validate the applicability of the nomogram. ResultsIn total, 250 patients were histologically identified as having peritoneal dissemination. Logistic regression analysis demonstrated that age, sex, tumor location, tumor size, signet-ring cell carcinoma (SRCC), T stage, N stage and Borrmann classification IV (Borrmann IV) were independent risk factors for peritoneal dissemination. We constructed a nomogram consisting of these eight factors to predict GCPD and found an optimistic predictive capability, with a C-index of 0.791, an area under the curve (AUC) of 0.791, and a 95% confidence interval (95% CI) of 0.762−0.820. The results found in the external validation set were also promising. ConclusionsWe constructed a highly sensitive nomogram that can assist clinicians in the early diagnosis of GCPD and serve as a reference for optimizing clinical management strategies.
2020, 32(2): 208-217.
doi: 10.21147/j.issn.1000-9604.2020.02.08
Abstract:
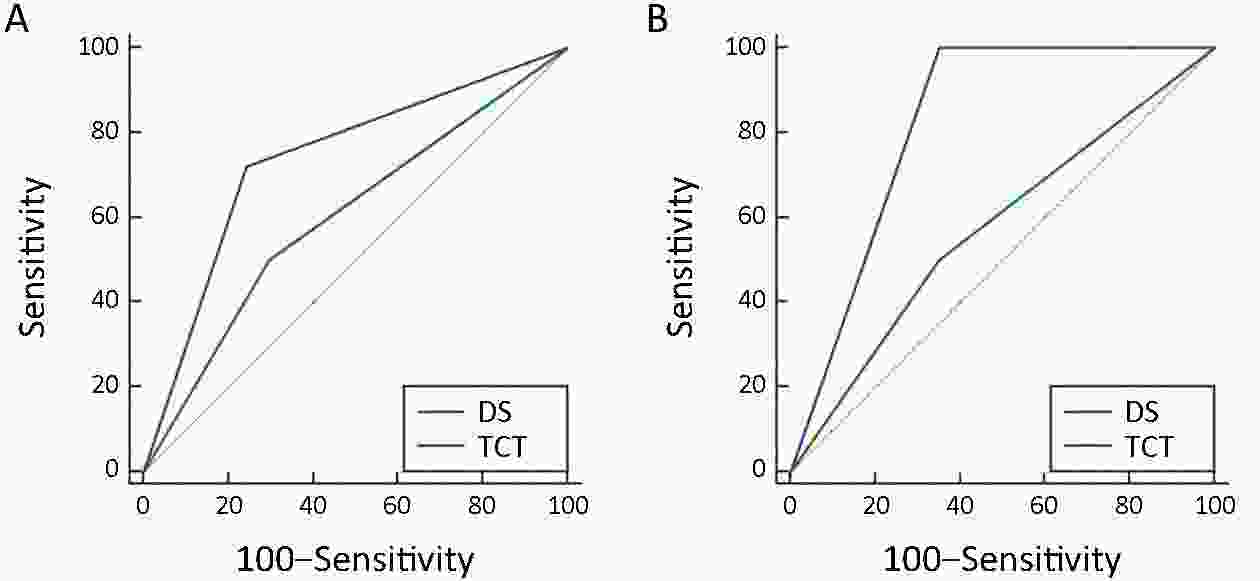
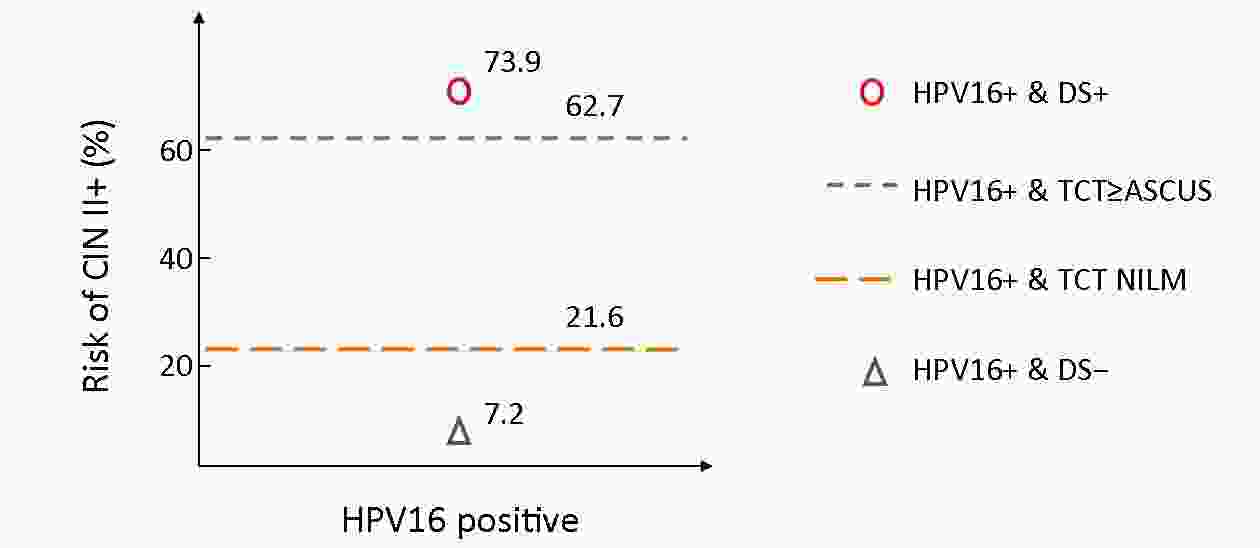
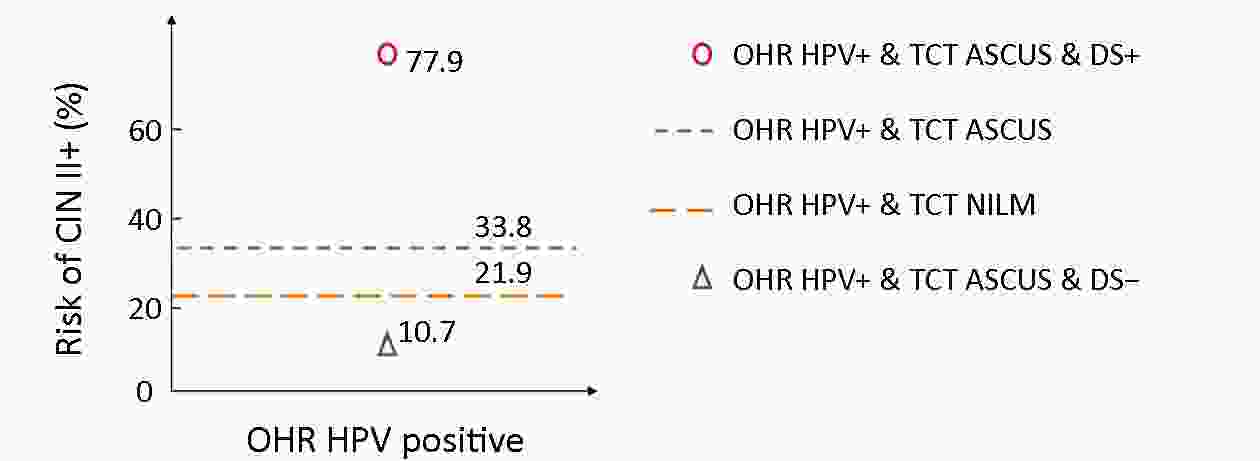
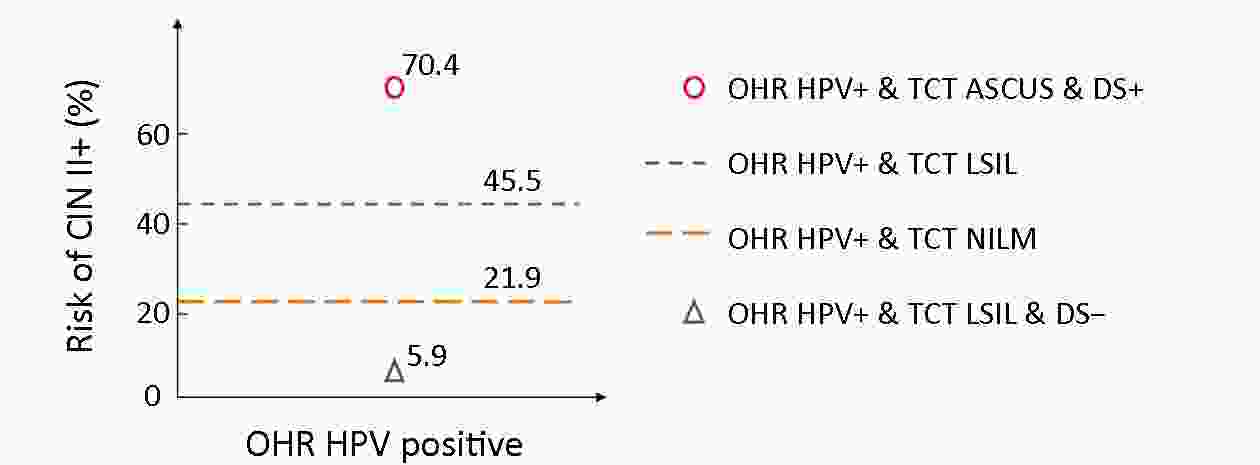
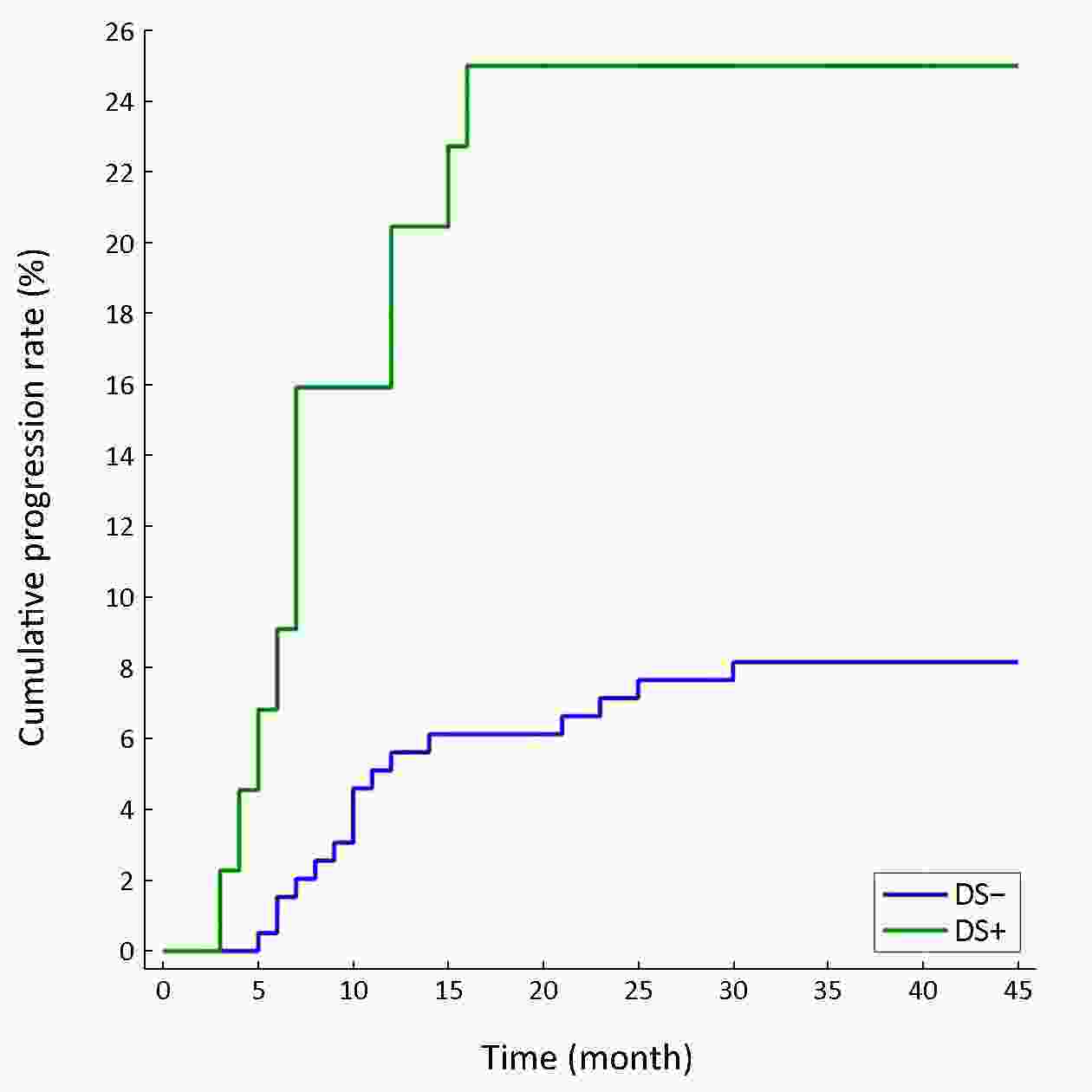
ObjectiveTo evaluate the efficiency of p16/Ki-67 dual stain used as a triage in cervical cancer screening. MethodsIn this study, we did 468 p16/Ki-67 dual stain in human papillomavirus (HPV) 16/18-positive or 12 other high-risk HPV (OHR-HPV) positive Thinprep cytologic test (TCT) atypical squamous cells of undetermined significance (ASCUS)/ lower-grade squamous intraepithelial lesion (LSIL) women. We evaluated the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the triage test. ResultsThe sensitivity, specificity, PPV and NPV of p16/Ki-67 dual stain in HPV 16/18-positive women were 91.5%/68.4%, 77.0%/75.0%, 73.9%/59.1% and 92.8%/81.8%. In 12 OHR-HPV positive TCT ASCUS/LSIL women, the results were 79.1%/95.0%, 88.5%/66.7%, 88.5%/70.4% and 89.2%/94.1%. The risk of precancerous lesions in p16/Ki-67 dual stain positive cases was much higher than before, and the negative cases had lower risk. Besides, there was no cervical intraepithelial neoplasia (CIN) III case missed after triaged by p16/Ki-67 dual-stained cytology. In p16/Ki-67 dual-stained cytology positive women with benign pathology or CIN I, the 1-year progression rate is 20.5% and in p16/Ki-67 dual-stained cytology negative women, the 1-year progression rate is 5.6%. Conclusionshr-HPV genotyping test plays an important role in cervical cancer screening. p16/Ki-67 dual stain may be a promising triage test. As for chronic cervicitis or CIN I patients, a positive p16/Ki-67 dual-stained cytology suggests a high risk in progression and need to be followed up closely.
2020, 32(2): 218-227.
doi: 10.21147/j.issn.1000-9604.2020.02.09
Abstract:
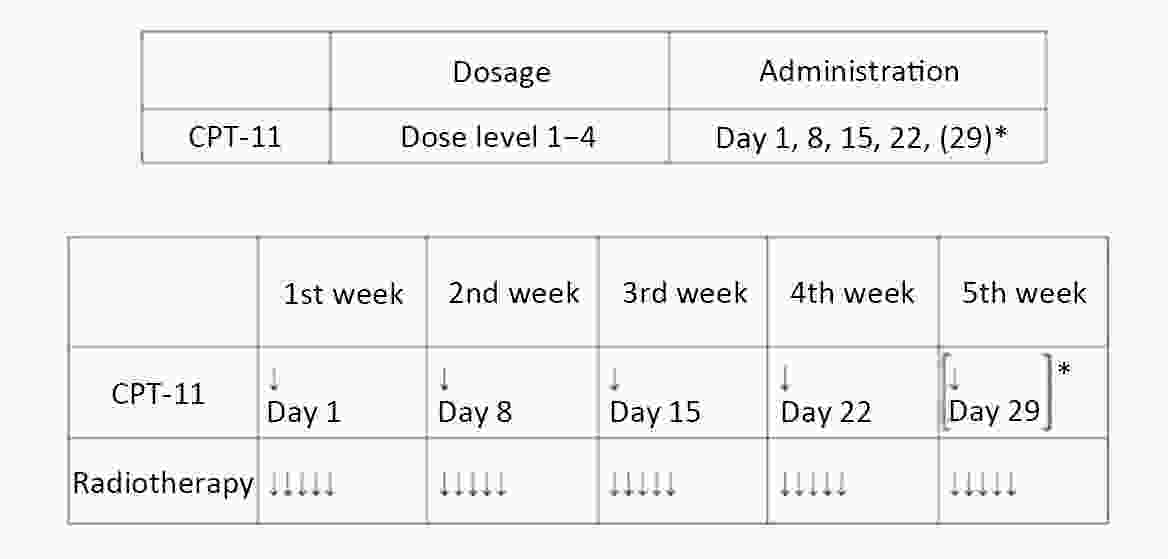
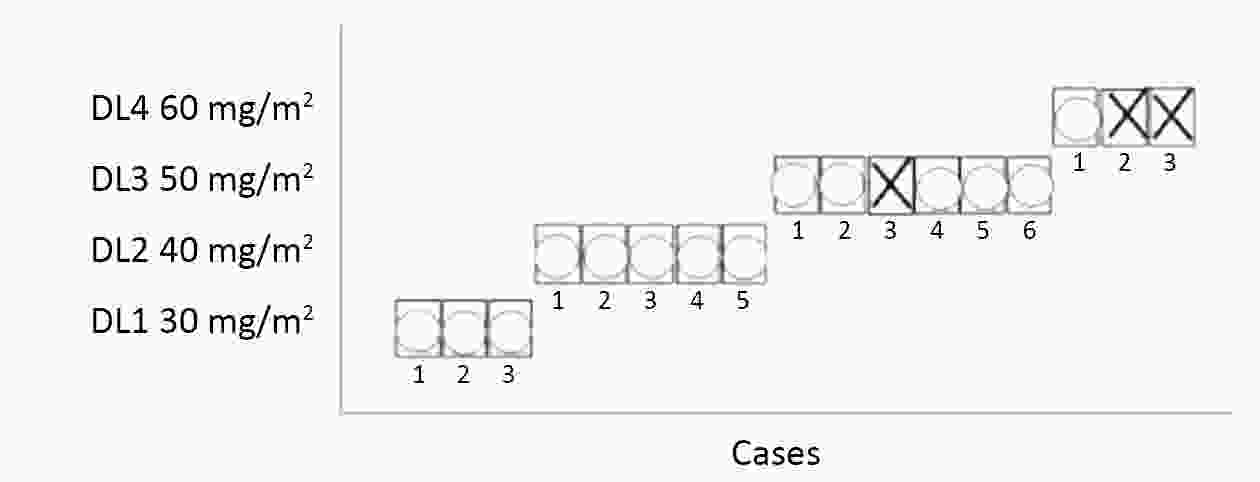
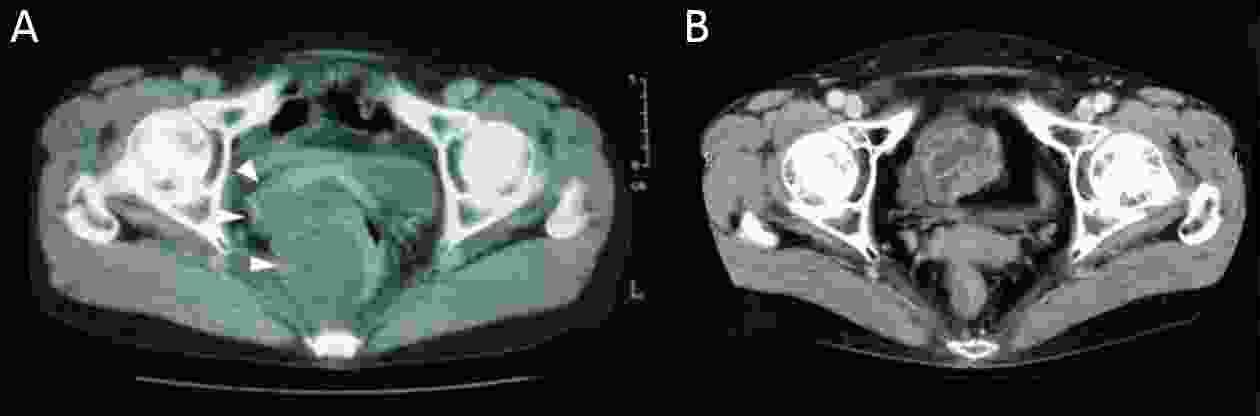
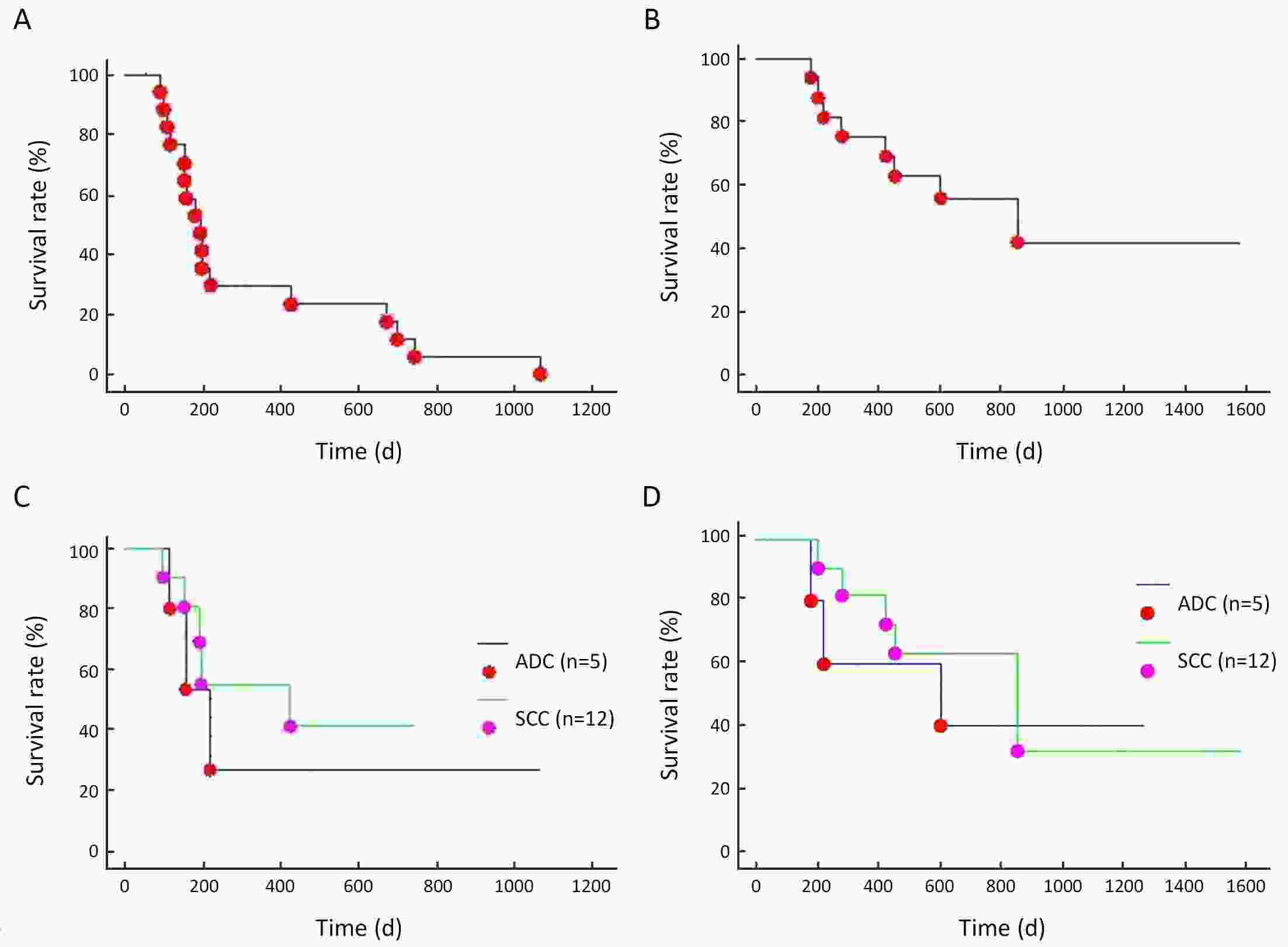
ObjectiveConcurrent chemoradiotherapy using cisplatin was thought to be standard treatment for squamous cell carcinoma of cervix, but it had not been effective for adenocarcinoma. Concurrent chemoradiotherapy using irinotecan hydrochloride (CPT-11) had been effective for colorectal cancer, thus, we chose CPT-11 as a candidate for gynecologic adenocarcinoma. To evaluate the maximum tolerated dose (MTD) of weekly CPT-11 with external pelvic radiotherapy, a phase 1/2 study was conducted according to modified Fibonacci method. MethodsEligible patients were advanced uterine cancer with measurable diseases [performance score (PS): 0−2]. Study period was from August 1st, 2002 to December 31st, 2008. The starting dose level (DL) of CPT-11 was 30 mg/m2 (DL1) given weekly for 4 weeks. Subsequently, dose escalation was scheduled in 10 mg/m2 increments to 60 mg/m2 (DL4). The fixed radiotherapy consisted of whole pelvic 1.8 Gy/d, once a day in weekday for five weeks and it amounted to 45 Gy (25 fractions) in total. ResultsSeventeen patients were enrolled. As for toxicities, one (1/17: 5.9%) grade (G) 4 neutropenia lasting 7 days had been seen in DL4. G2 diarrhea was identified in 35.3% (6/17) of the patients, and 11.8% (2/17) G3 diarrhea was observed in DL3 and DL4. Thus, the MTD of CPT-11 was defined as dose of 60 mg/m2. The recommended dose was decided as 50 mg/m2. The response rate was 88.2% [9 complete response (CR), 3 partial response (PR), 3 stable disease (SD), 2 not evaluable (NE)]. Disease control rate at 1 month after treatment completion was 100% but distant metastases were found in 24% (4/17) in longer outcome. ConclusionsMTD was 60 mg/m2 and recommended dose was set as 50 mg/m2. This concurrent chemoradiation using weekly CPT-11 was feasible at 50 mg/m2, and it might be effective even in adenocarcinoma of the uterus.
2020, 32(2): 228-241.
doi: 10.21147/j.issn.1000-9604.2020.02.10
Abstract:
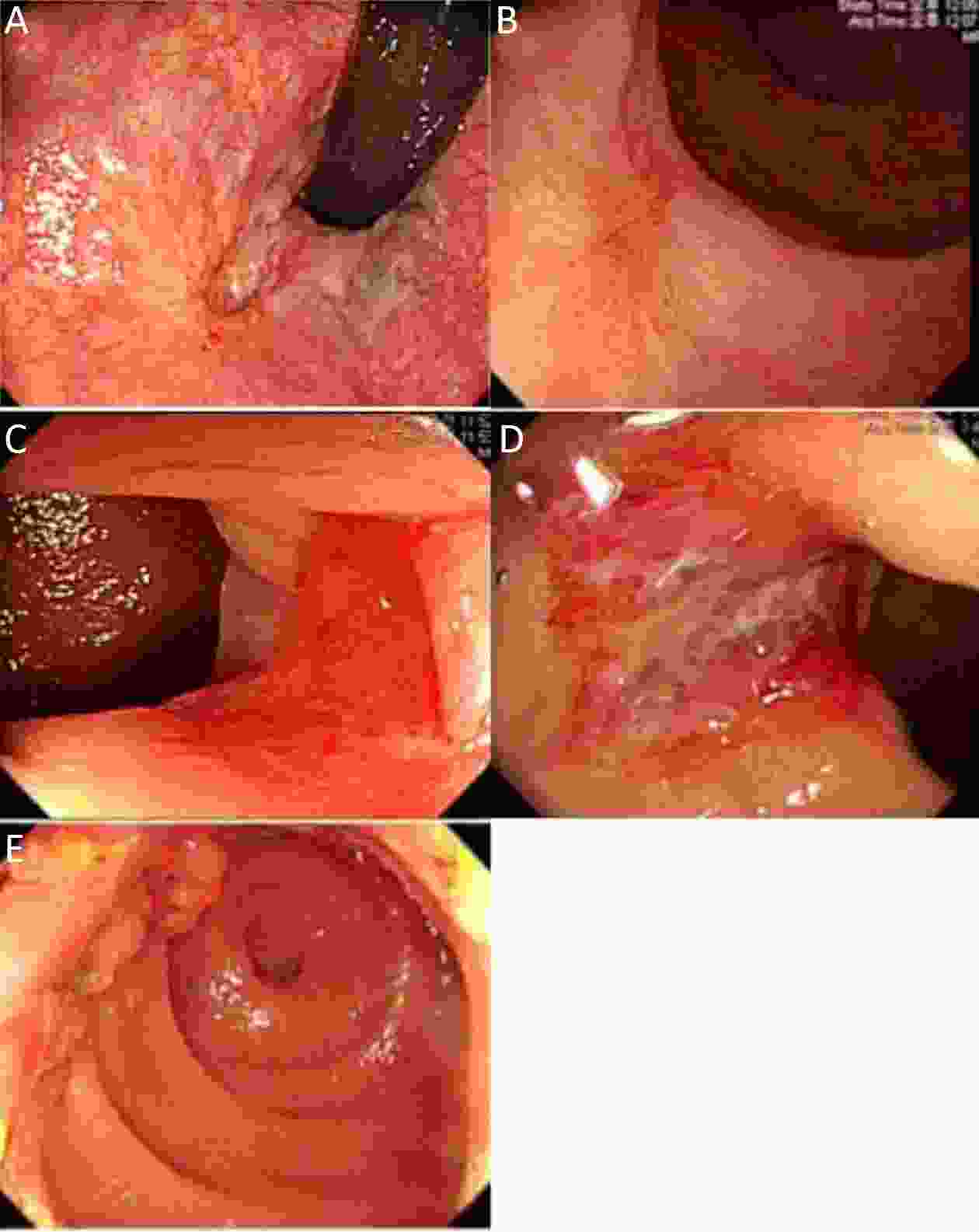
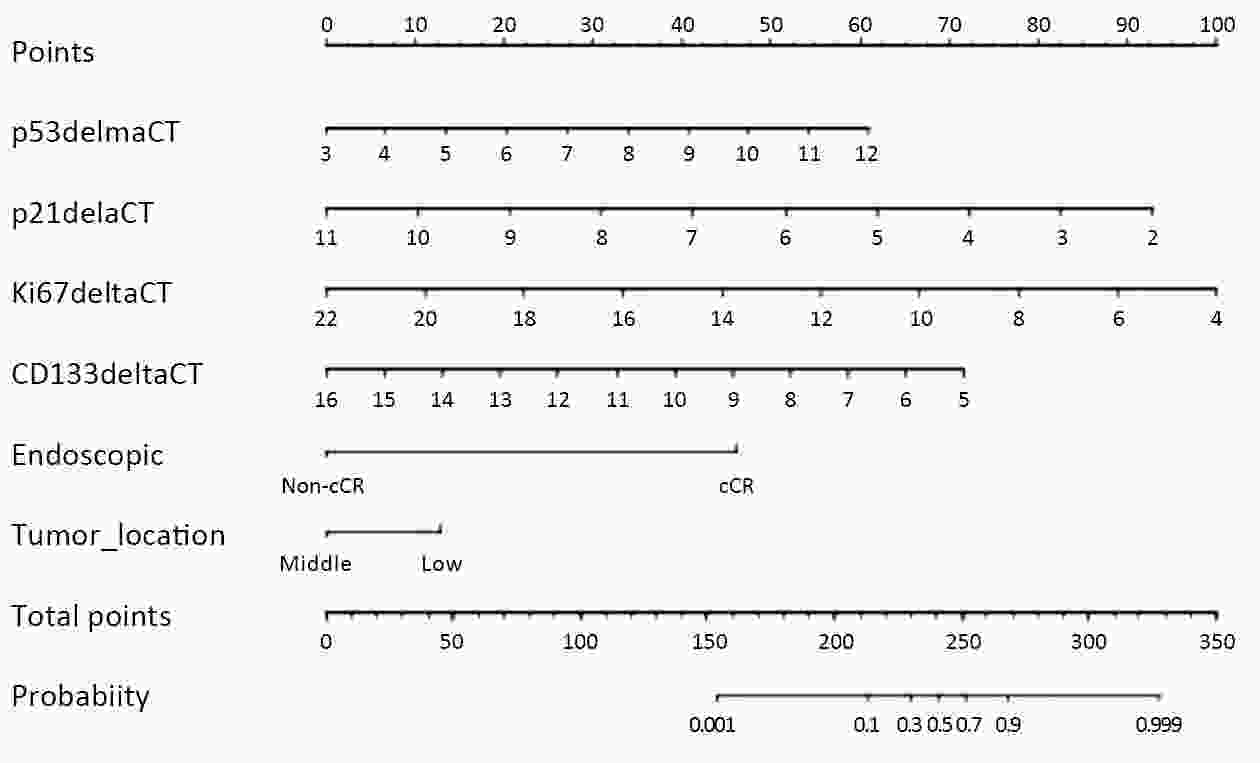
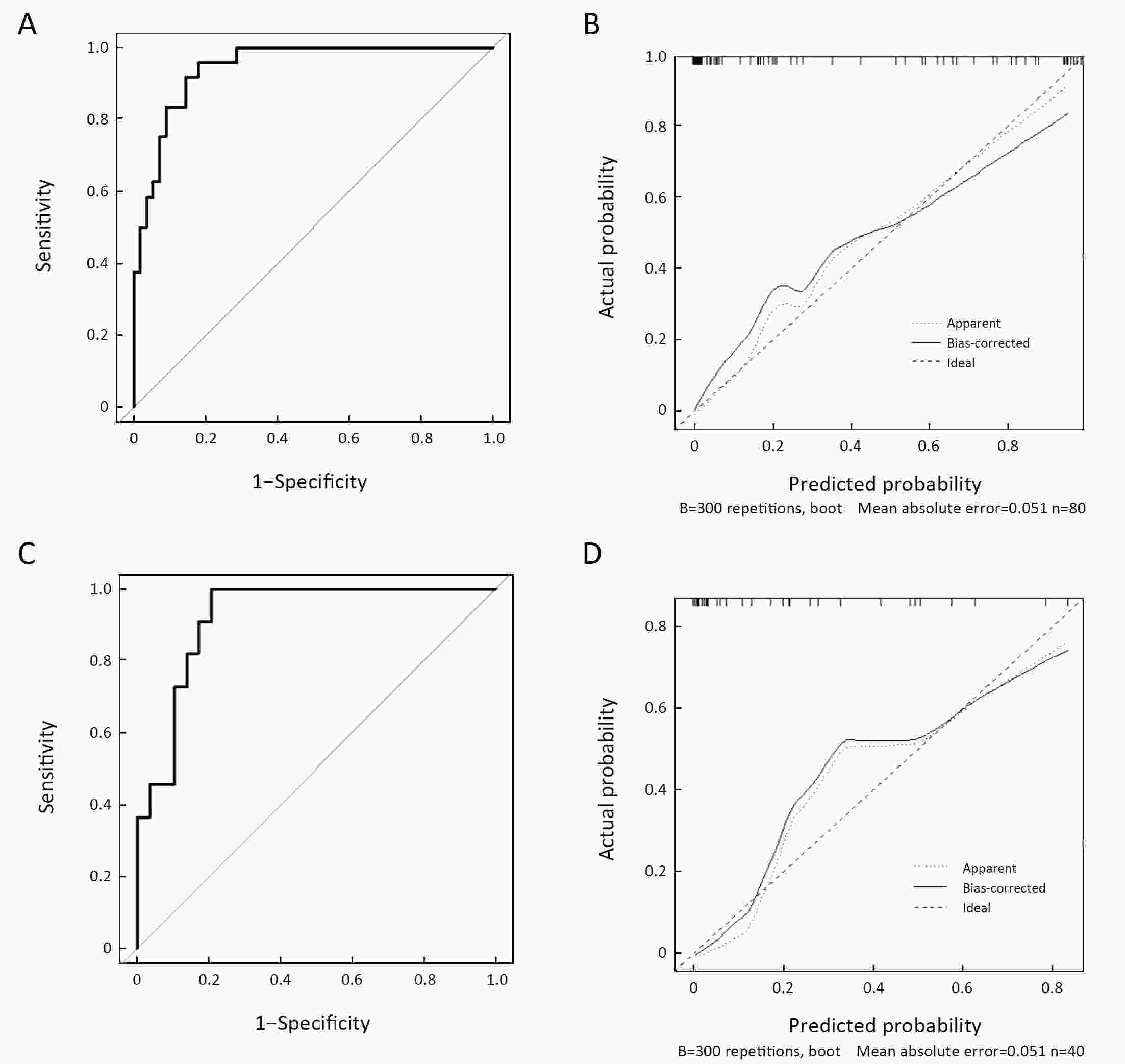
ObjectiveThe aim of this study is to develop a nomogram for prediction of pathologic complete remission (pCR) after preoperative chemoradiotherapy (CRT) for rectal cancer. MethodsmRNA expression levels of seven molecular markers [p53, p21, Ki-67, vascular endothelial growth factor (VEGF), CD133, CD24, CD44] were measured by reverse transcriptase polymerase chain reaction (RT-PCR) in 120 rectal cancers. Endoscopic findings of clinical complete remission (cCR) and biologic variables were used to construct nomogram in the training group (n=80), which was validated in the validation group (n=40). ResultsmRNA expression levels of four markers (p53, p21, Ki67, CD133) correlated with pCR (24/80, 30.0%) in the training group. Low expression of p53 and/or high expression of p21, Ki67 and CD133 showed greater pCR rate. pCR was shown in 18 (69.2%) of 26 cases showing endoscopic cCR in the training group. Higher pCR rate was demonstrated in lower tumor location than middle tumor (19/49, 38.8% vs. 5/31, 16.1%). A nomogram for prediction of pCR was developed from the multivariate prediction model using these six variables, which showed good discrimination ability in the training group [area under the curve (AUC)=0.945] and validation group (AUC=0.922). The calibration plot showed good agreement between actual and predicted pCR in both patient groups. ConclusionsNomogram for assessment of pCR can be useful for making treatment decisions after CRT according to predicted responses.
2020, 32(2): 242-251.
doi: 10.21147/j.issn.1000-9604.2020.02.11
Abstract:
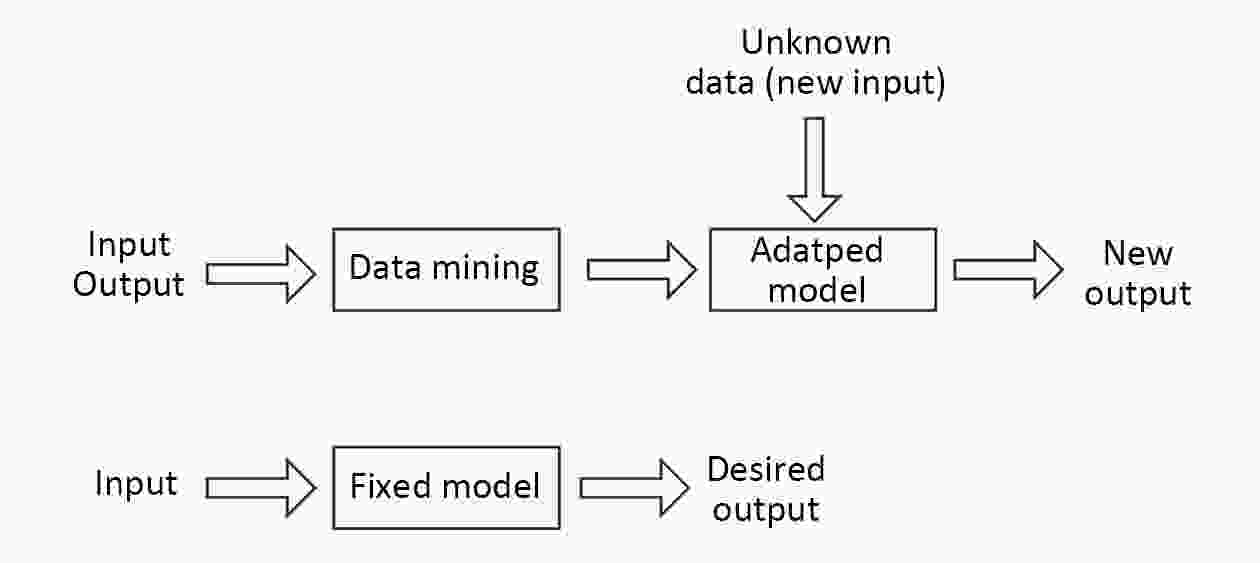
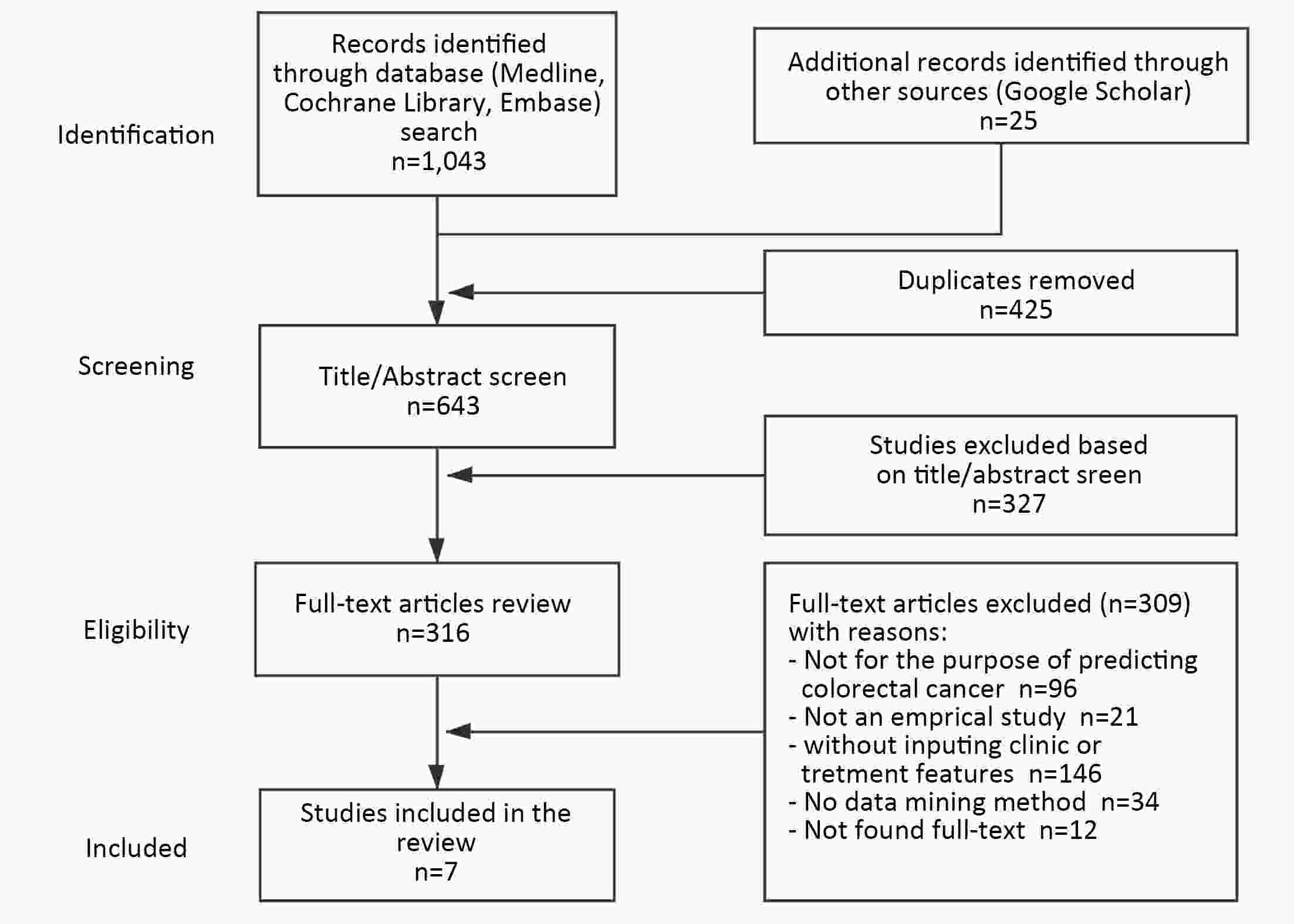
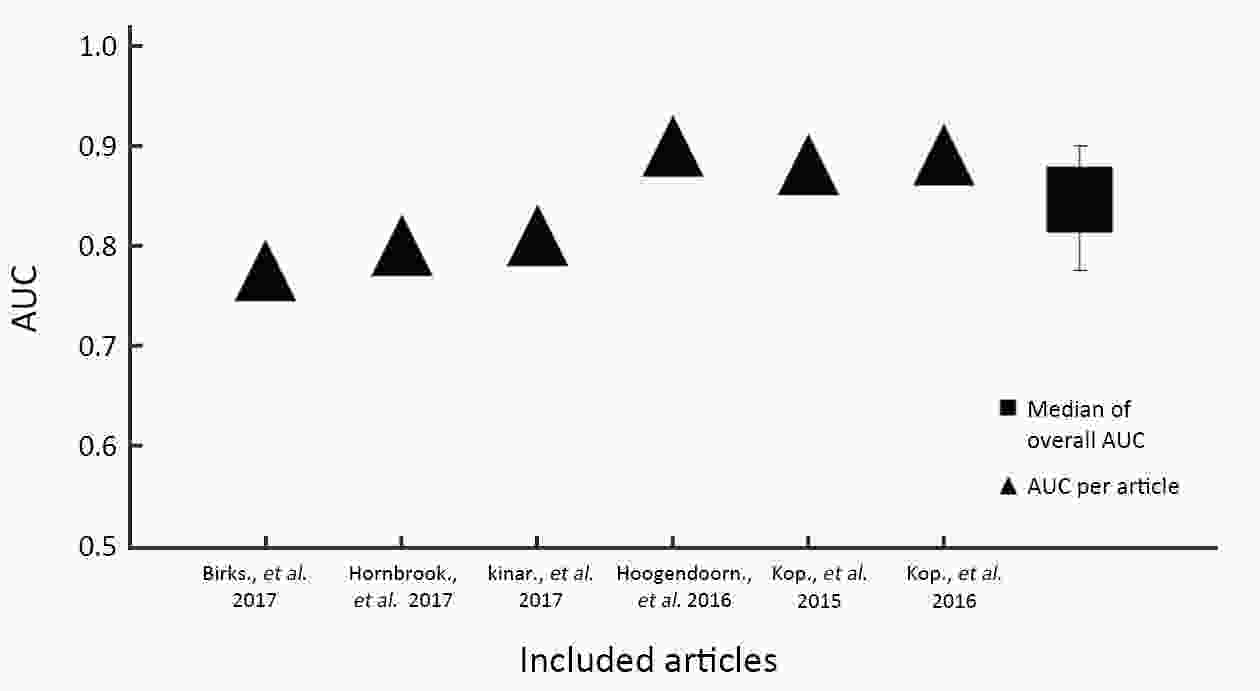
ObjectivePrevention and early detection of colorectal cancer (CRC) can increase the chances of successful treatment and reduce burden. Various data mining technologies have been utilized to strengthen the early detection of CRC in primary care. Evidence synthesis on the model’s effectiveness is scant. This systematic review synthesizes studies that examine the effect of data mining on improving risk prediction of CRC. MethodsThe PRISMA framework guided the conduct of this study. We obtained papers via PubMed, Cochrane Library, EMBASE and Google Scholar. Quality appraisal was performed using Downs and Black’s quality checklist. To evaluate the performance of included models, the values of specificity and sensitivity were comparted, the values of area under the curve (AUC) were plotted, and the median of overall AUC of included studies was computed. ResultsA total of 316 studies were reviewed for full text. Seven articles were included. Included studies implement techniques including artificial neural networks, Bayesian networks and decision trees. Six articles reported the overall model accuracy. Overall, the median AUC is 0.8243 [interquartile range (IQR): 0.8050−0.8886]. In the two articles that reported comparison results with traditional models, the data mining method performed better than the traditional models, with the best AUC improvement of 10.7%. ConclusionsThe adoption of data mining technologies for CRC detection is at an early stage. Limited numbers of included articles and heterogeneity of those studies implied that more rigorous research is expected to further investigate the techniques’ effects.
2020, 32(2): 252-262.
doi: 10.21147/j.issn.1000-9604.2020.02.12
Abstract:
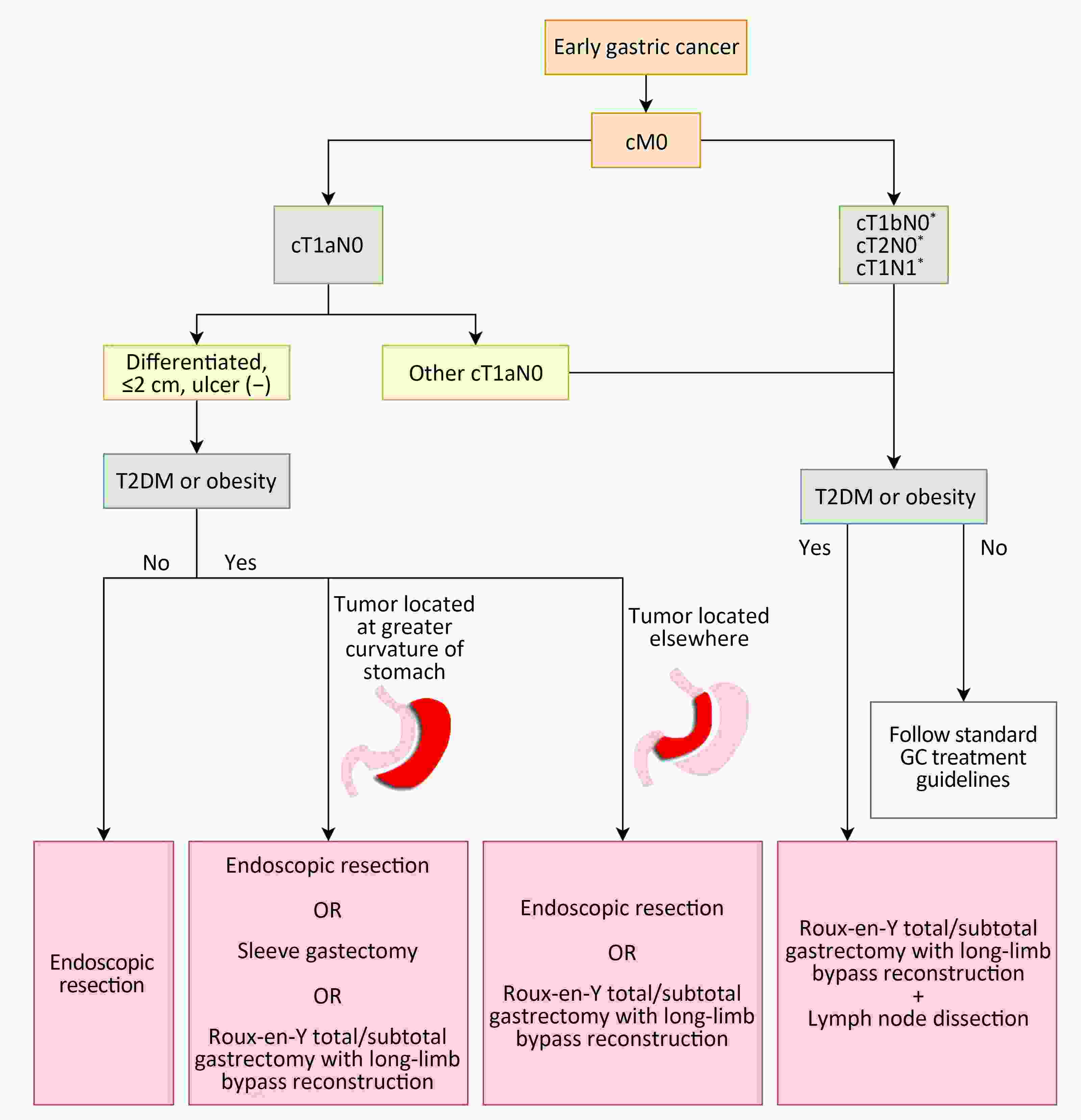
Studies on morbid obesity have shown remarkable improvement of diabetes in patients who have undergone bariatric operations. It was subsequently shown that these operations induce diabetes remission independent of the resultant weight loss; as a result, surgeons began to investigate whether operations for gastric cancer (GC) could have the same beneficial effect on diabetes as bariatric operations. It was then shown in multiple reports that followed that certain operations for GC were able to improve or even cure type 2 diabetes mellitus (T2DM) in GC patients. This finding gave rise to the concept of “oncometabolic surgery”, in which a patient diagnosed with both GC and T2DM undergo a single operation with the purpose of treating both diseases. With the increasing incidence of T2DM, oncometabolic surgery has the potential to improve the quality of life and even extend survival of many GC patients. However, because the GC patient population and the bariatric patient population are wildly different and because different GC operations have different properties, the effect of oncometabolic surgery must be carefully assessed and engineered in order to maximize benefit and avoid harm. This manuscript aims to summarize the findings made so far in the field of oncometabolic surgery and to provide an outlook regarding the possibility of oncometabolic surgery being incorporated into standard clinical practice.
Studies on morbid obesity have shown remarkable improvement of diabetes in patients who have undergone bariatric operations. It was subsequently shown that these operations induce diabetes remission independent of the resultant weight loss; as a result, surgeons began to investigate whether operations for gastric cancer (GC) could have the same beneficial effect on diabetes as bariatric operations. It was then shown in multiple reports that followed that certain operations for GC were able to improve or even cure type 2 diabetes mellitus (T2DM) in GC patients. This finding gave rise to the concept of “oncometabolic surgery”, in which a patient diagnosed with both GC and T2DM undergo a single operation with the purpose of treating both diseases. With the increasing incidence of T2DM, oncometabolic surgery has the potential to improve the quality of life and even extend survival of many GC patients. However, because the GC patient population and the bariatric patient population are wildly different and because different GC operations have different properties, the effect of oncometabolic surgery must be carefully assessed and engineered in order to maximize benefit and avoid harm. This manuscript aims to summarize the findings made so far in the field of oncometabolic surgery and to provide an outlook regarding the possibility of oncometabolic surgery being incorporated into standard clinical practice.
2020, 32(2): 263-270.
doi: 10.21147/j.issn.1000-9604.2020.02.13
Abstract:
Claudin 18.2 (CLDN18.2) is a tight-junction protein. CLDN18.2-targeting strategy has cut a striking figure in CLDN18.2 positive patients with advanced gastric cancer. Zolbetuximab, the CLDN18.2 antibody, obtained a better clinical benefit in patients compared with the controlled. In phase II trials, combination treatment of epirubicin, oxaliplatin and capecitabine (EOX) + zolbetuximab achieved the optimal effects of overall survival which extended to 13.2 months with tolerable safety events, indicating its greater potential playing the second promising target in gastric cancer. This review will reveal the definitive clinical benefit CLDN18.2-targeting therapies have achieved and update the highlighting development (like chimeric antigen receptor T-cell immunotherapy) to CLDN18.2 positive patients. We then focus on 10 questions arisen from recent progress and anticipate to provide a future perspective for novel cancer treatment.
Claudin 18.2 (CLDN18.2) is a tight-junction protein. CLDN18.2-targeting strategy has cut a striking figure in CLDN18.2 positive patients with advanced gastric cancer. Zolbetuximab, the CLDN18.2 antibody, obtained a better clinical benefit in patients compared with the controlled. In phase II trials, combination treatment of epirubicin, oxaliplatin and capecitabine (EOX) + zolbetuximab achieved the optimal effects of overall survival which extended to 13.2 months with tolerable safety events, indicating its greater potential playing the second promising target in gastric cancer. This review will reveal the definitive clinical benefit CLDN18.2-targeting therapies have achieved and update the highlighting development (like chimeric antigen receptor T-cell immunotherapy) to CLDN18.2 positive patients. We then focus on 10 questions arisen from recent progress and anticipate to provide a future perspective for novel cancer treatment.

 Abstract
Abstract FullText HTML
FullText HTML PDF 1728KB
PDF 1728KB