2020 Vol.32(3)
Display Mode: |
2020, 32(3): 271-286.
doi: 10.21147/j.issn.1000-9604.2020.03.01
Abstract:
Esophageal cancer (EC) remains one of the most common and aggressive diseases worldwide. This review discusses some debates in the modern management of the disease. Endoscopic procedures for early cancer (T1a−b) are now embedded in routine care and the challenge will be to more accurately select patients for endoscopic resection with or without adjuvant therapy. Perioperative multimodal therapies are associated with improved survival compared to surgery alone for locally advanced esophageal cancer. However, there is no global consensus on the optimal regimen. Furthermore, histological subtype (adenocarcinoma vs. squamous cell cancer) plays a role in the choice for treatment. New studies are underway to resolve some issues. The extent of the lymphadenectomy during esophagectomy remains controversial especially after neoadjuvant chemoradiation. The ideal operation balances between limiting surgical trauma and optimizing survival. Minimally invasive esophagectomy and enhanced recovery pathways are associated with decreased morbidity and faster recovery albeit there is no consensus yet what approach should be used. Finally, immune checkpoint inhibitors present promising preliminary results in the novel treatment of advanced or metastatic EC but their widespread application in clinical practice is still awaited.
Esophageal cancer (EC) remains one of the most common and aggressive diseases worldwide. This review discusses some debates in the modern management of the disease. Endoscopic procedures for early cancer (T1a−b) are now embedded in routine care and the challenge will be to more accurately select patients for endoscopic resection with or without adjuvant therapy. Perioperative multimodal therapies are associated with improved survival compared to surgery alone for locally advanced esophageal cancer. However, there is no global consensus on the optimal regimen. Furthermore, histological subtype (adenocarcinoma vs. squamous cell cancer) plays a role in the choice for treatment. New studies are underway to resolve some issues. The extent of the lymphadenectomy during esophagectomy remains controversial especially after neoadjuvant chemoradiation. The ideal operation balances between limiting surgical trauma and optimizing survival. Minimally invasive esophagectomy and enhanced recovery pathways are associated with decreased morbidity and faster recovery albeit there is no consensus yet what approach should be used. Finally, immune checkpoint inhibitors present promising preliminary results in the novel treatment of advanced or metastatic EC but their widespread application in clinical practice is still awaited.
2020, 32(3): 287-302.
doi: 10.21147/j.issn.1000-9604.2020.03.02
Abstract:
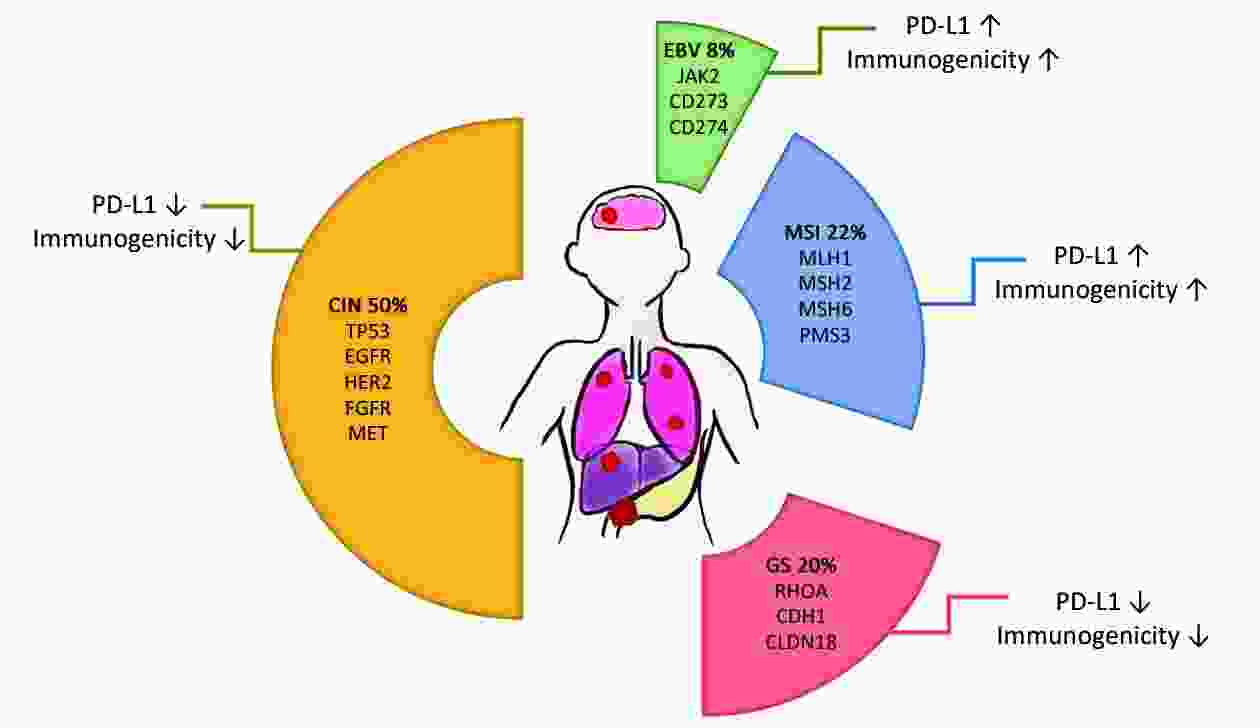
Despite the application of conventional therapies, the prognosis of advanced gastric cancer (GC) or gastroesophageal junction cancer (GEJC) is still poor. In recent years, immune checkpoint inhibitors (ICIs) have reshaped the paradigm of cancer therapy. Emerging evidence support the feasibility of programmed cell death-1 (PD-1) and its ligand (PD-L1) inhibition in chemo-refractory GC/GEJC. Nivolumab and pembrolizumab have initially been approved in Japan and United States, respectively for the third-line treatment of progressive GC or GEJC. In March 2020, nivolumab has also been licensed in China for treating advanced GC/GEJC who received ≥2 lines of systemic therapies. Current studies are moving forward to the first-line application or focusing on combination strategies, though data are insufficient and disputable. In this review, we summarize the recently reported and ongoing clinical trials in ICIs for advanced GC/GEJC. Molecular characteristics and clinical implications of different tumor subtypes are also reviewed. We further discuss the safety profile and biomarkers for predicting the response of ICIs, which has guiding values in clinical practice.
Despite the application of conventional therapies, the prognosis of advanced gastric cancer (GC) or gastroesophageal junction cancer (GEJC) is still poor. In recent years, immune checkpoint inhibitors (ICIs) have reshaped the paradigm of cancer therapy. Emerging evidence support the feasibility of programmed cell death-1 (PD-1) and its ligand (PD-L1) inhibition in chemo-refractory GC/GEJC. Nivolumab and pembrolizumab have initially been approved in Japan and United States, respectively for the third-line treatment of progressive GC or GEJC. In March 2020, nivolumab has also been licensed in China for treating advanced GC/GEJC who received ≥2 lines of systemic therapies. Current studies are moving forward to the first-line application or focusing on combination strategies, though data are insufficient and disputable. In this review, we summarize the recently reported and ongoing clinical trials in ICIs for advanced GC/GEJC. Molecular characteristics and clinical implications of different tumor subtypes are also reviewed. We further discuss the safety profile and biomarkers for predicting the response of ICIs, which has guiding values in clinical practice.
2020, 32(3): 303-318.
doi: 10.21147/j.issn.1000-9604.2020.03.03
Abstract:
Classical Hodgkin lymphoma (cHL) has been identified with universal genetic alterations of chromosome 9p24.1, which contains PD-L1/PD-L2 genes. The amplification of 9p24.1 is associated with the increased expression of PD-L1 and PD-L2 on RS cells, which promotes their immune evasion, and subsequently makes cHL sensitive to PD-1 blockade. Several PD-1 inhibitors have shown significant efficacies with overall response rate (ORR) of 70%−90% in relapse/refractory (r/r) cHL and have acquired the approvals for this indication. Recently, more and more studies are conducted to investigate PD-1 blockade in earlier disease course and in combination with neo-agents or chemotherapy. Unlike cHL, non-Hodgkin lymphoma (NHL) consists of numerous subtypes harboring highly biological heterogeneity. Only a few subtypes have been shown to have genetic alteration of 9p24.1 including primary mediastinal B cell lymphoma (PMBL), gray zone lymphoma (GZL) with features intermediate between diffuse large B cell lymphoma (DLBCL) and cHL, primary central nervous system lymphoma (PCNSL) and primary testicular lymphoma (PTL). Epstein-Barr virus (EBV)-associated lymphomas have a virally mediated overexpression of PD-L1, also making them sensitive to PD-1 blockade. Therefore, PD-1 inhibitors are less effective in most r/r NHL than in r/r cHL. Further understanding of the biological features of NHL and immune checkpoint inhibitors (ICPi) combined therapy is the research focus in the future. In this review, we outlined the recent progress of ICPi in lymphoma originating from clinical studies.
Classical Hodgkin lymphoma (cHL) has been identified with universal genetic alterations of chromosome 9p24.1, which contains PD-L1/PD-L2 genes. The amplification of 9p24.1 is associated with the increased expression of PD-L1 and PD-L2 on RS cells, which promotes their immune evasion, and subsequently makes cHL sensitive to PD-1 blockade. Several PD-1 inhibitors have shown significant efficacies with overall response rate (ORR) of 70%−90% in relapse/refractory (r/r) cHL and have acquired the approvals for this indication. Recently, more and more studies are conducted to investigate PD-1 blockade in earlier disease course and in combination with neo-agents or chemotherapy. Unlike cHL, non-Hodgkin lymphoma (NHL) consists of numerous subtypes harboring highly biological heterogeneity. Only a few subtypes have been shown to have genetic alteration of 9p24.1 including primary mediastinal B cell lymphoma (PMBL), gray zone lymphoma (GZL) with features intermediate between diffuse large B cell lymphoma (DLBCL) and cHL, primary central nervous system lymphoma (PCNSL) and primary testicular lymphoma (PTL). Epstein-Barr virus (EBV)-associated lymphomas have a virally mediated overexpression of PD-L1, also making them sensitive to PD-1 blockade. Therefore, PD-1 inhibitors are less effective in most r/r NHL than in r/r cHL. Further understanding of the biological features of NHL and immune checkpoint inhibitors (ICPi) combined therapy is the research focus in the future. In this review, we outlined the recent progress of ICPi in lymphoma originating from clinical studies.
2020, 32(3): 319-333.
doi: 10.21147/j.issn.1000-9604.2020.03.04
Abstract:
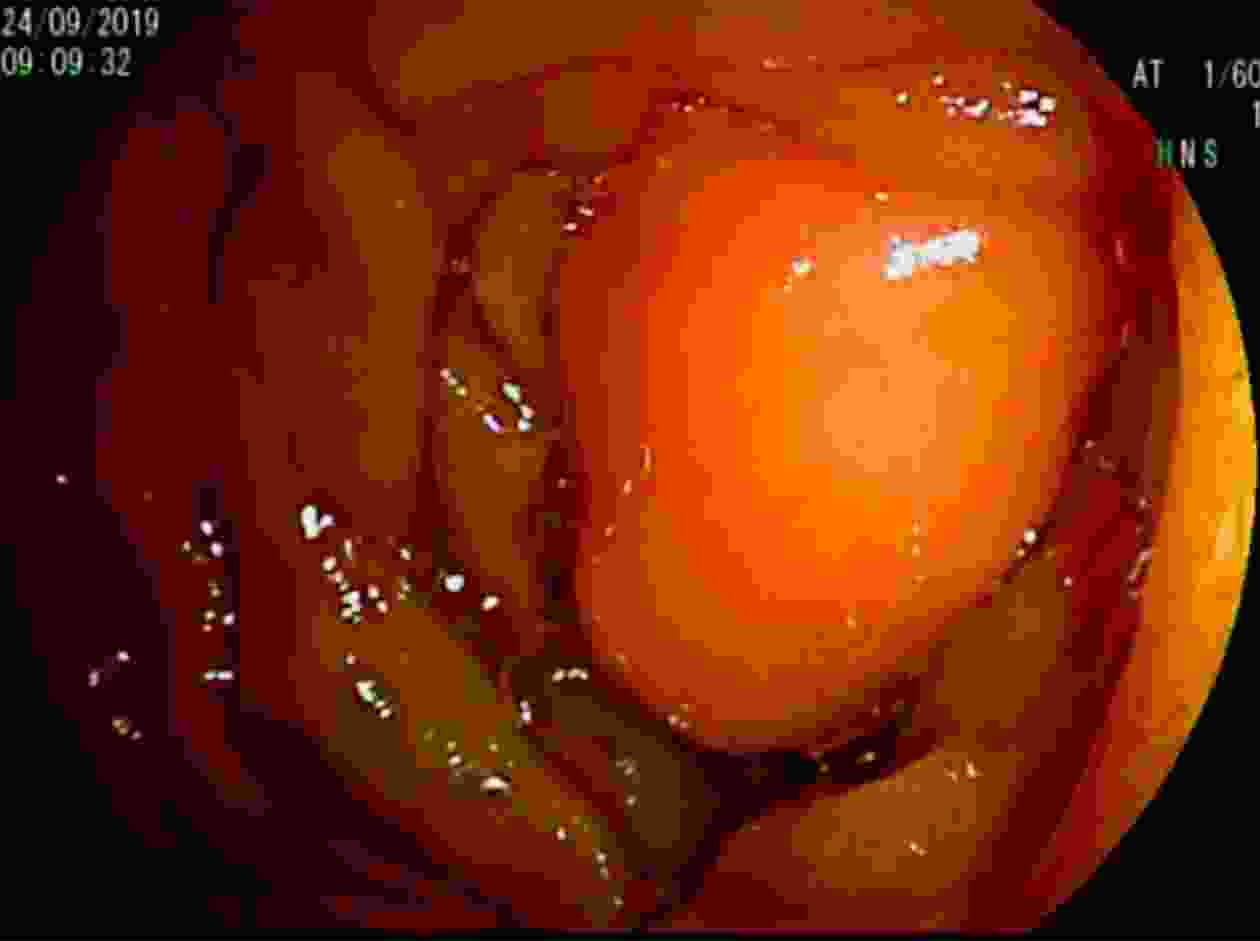
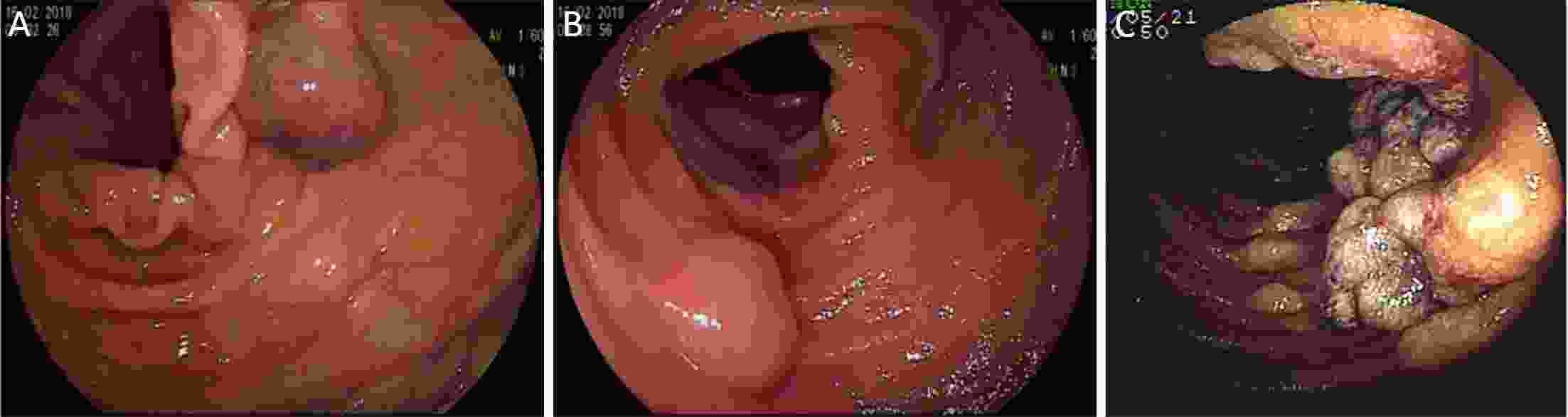
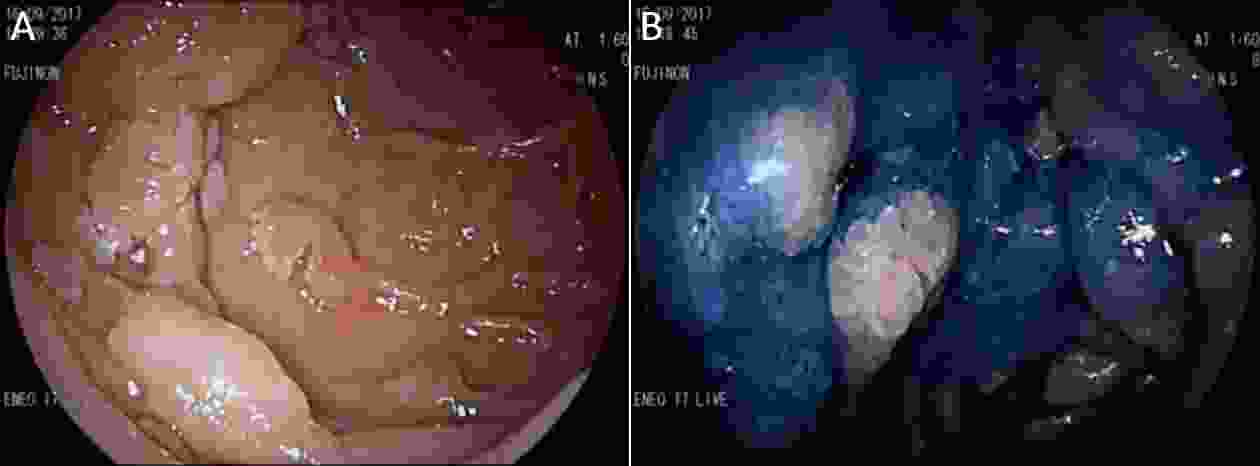
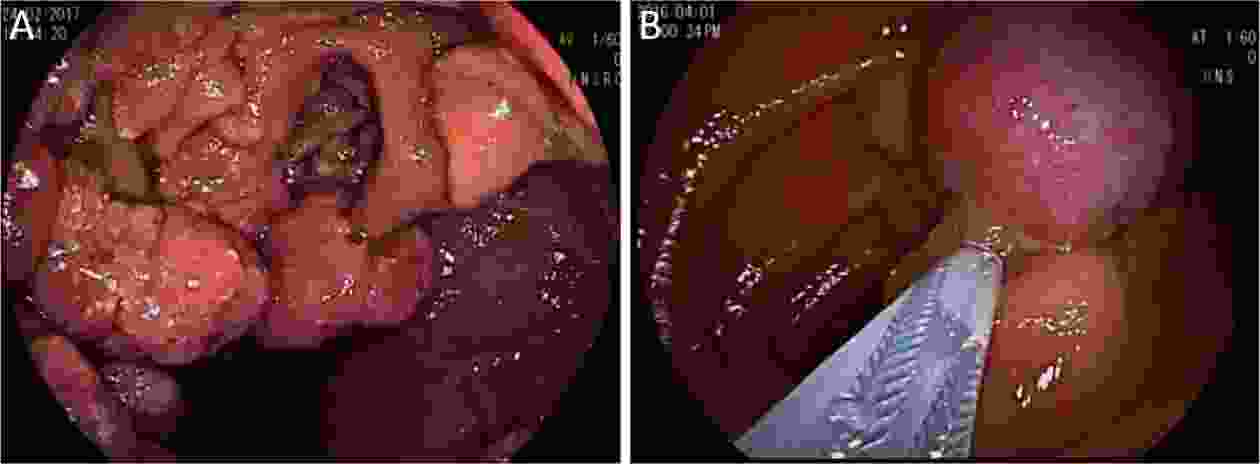
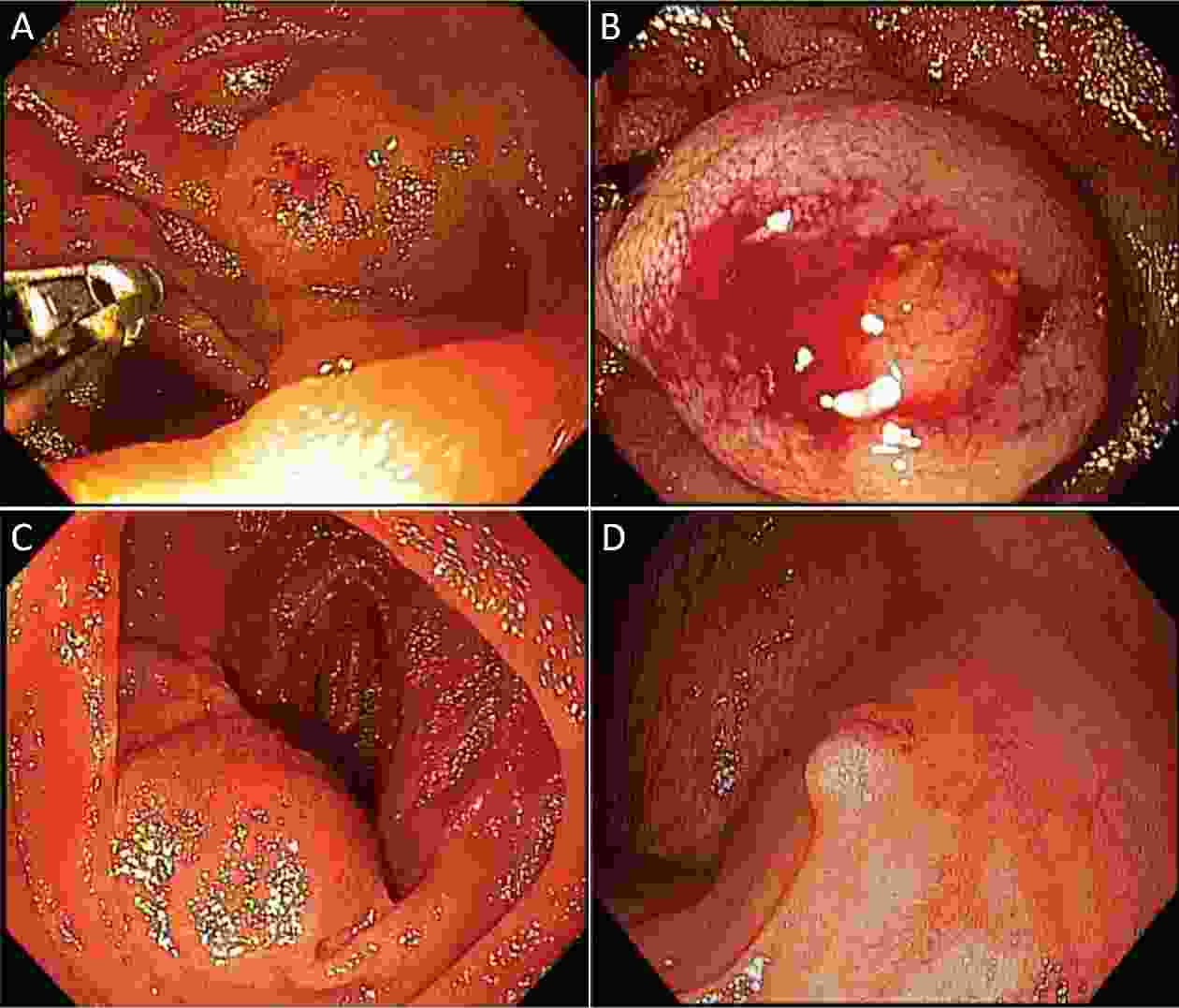
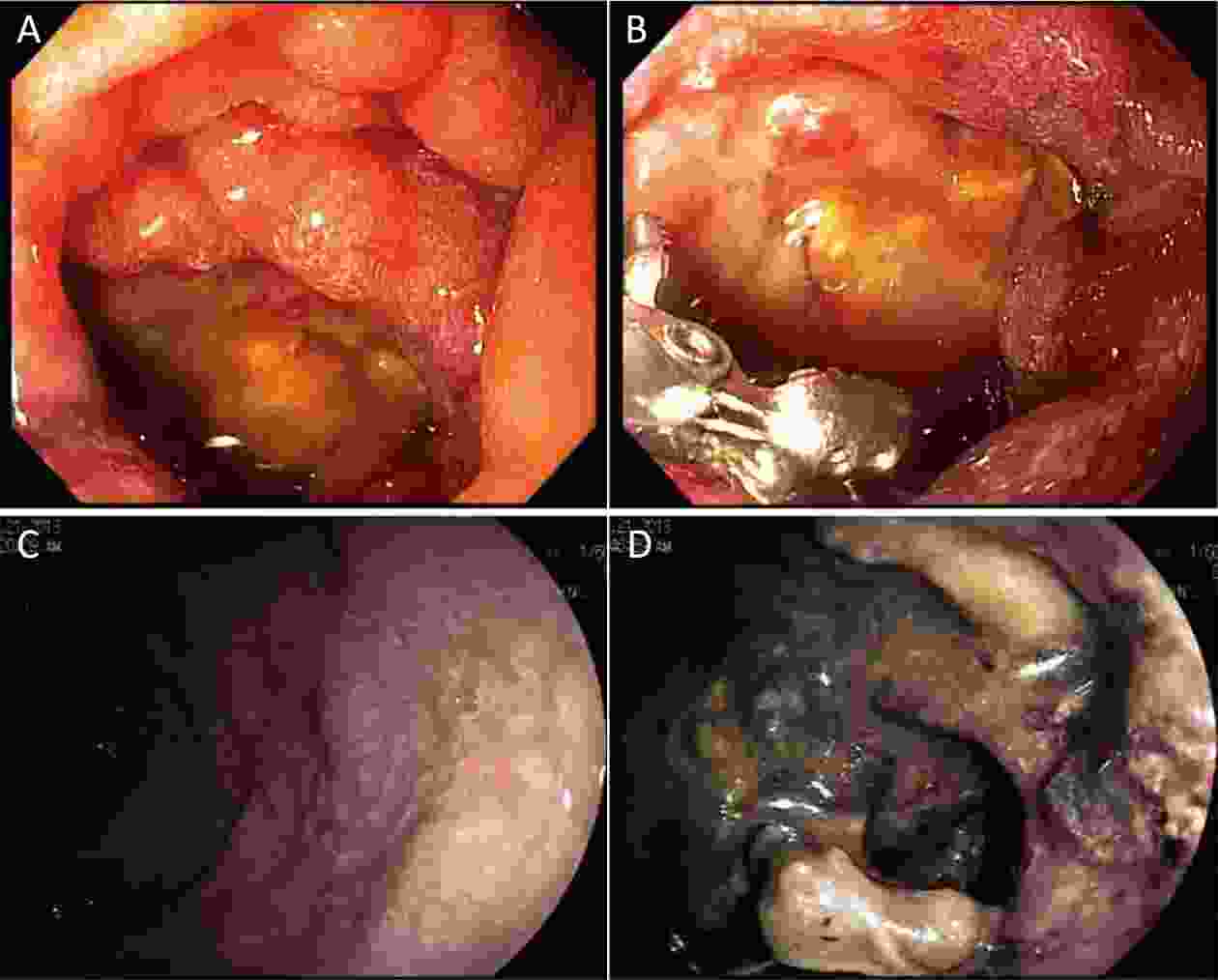
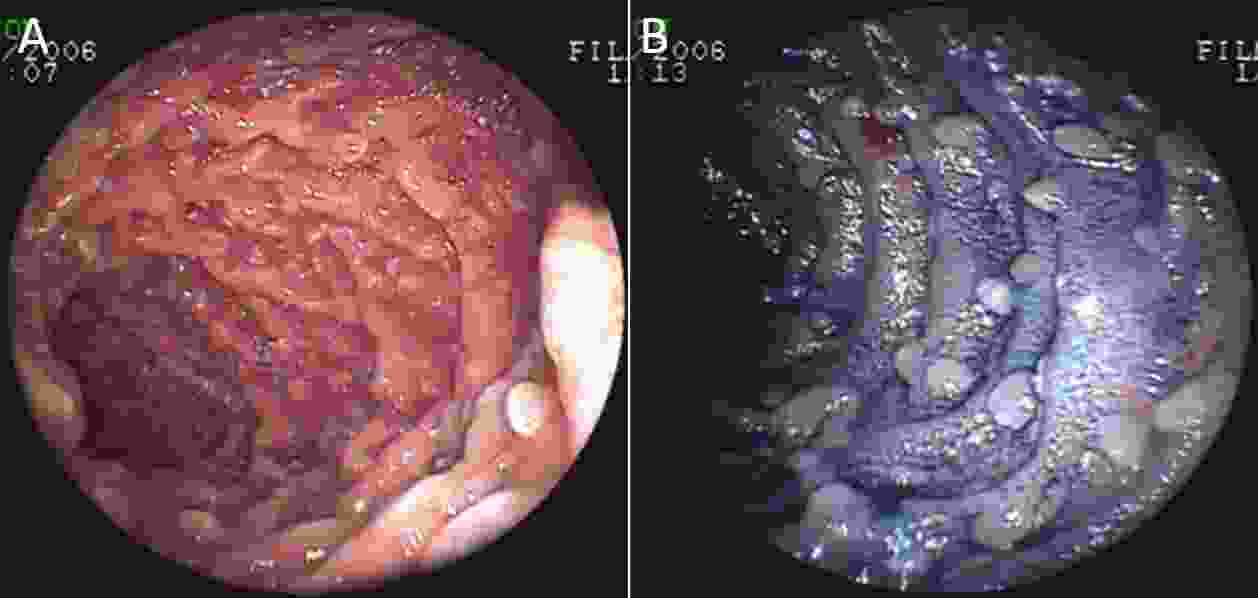
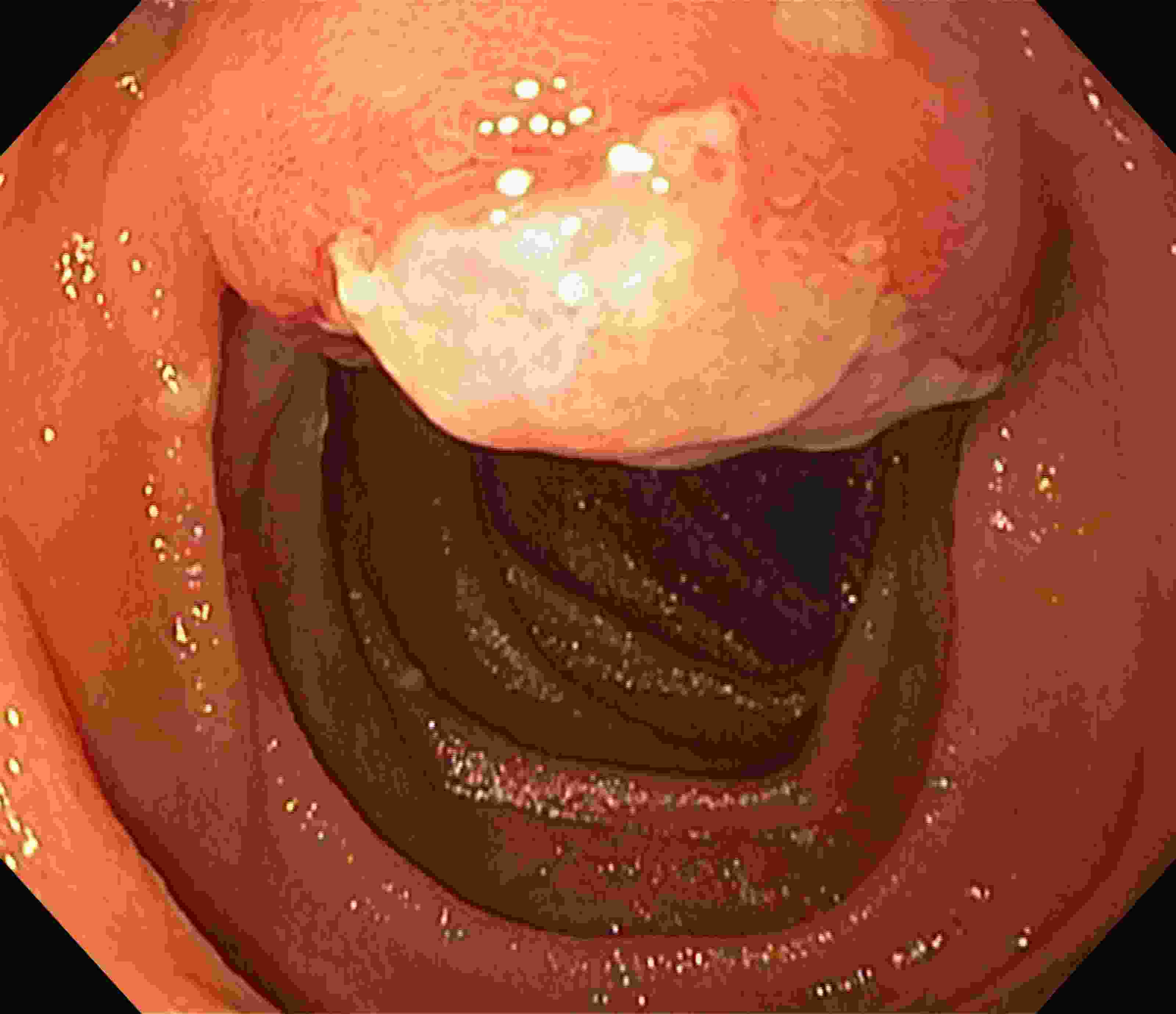
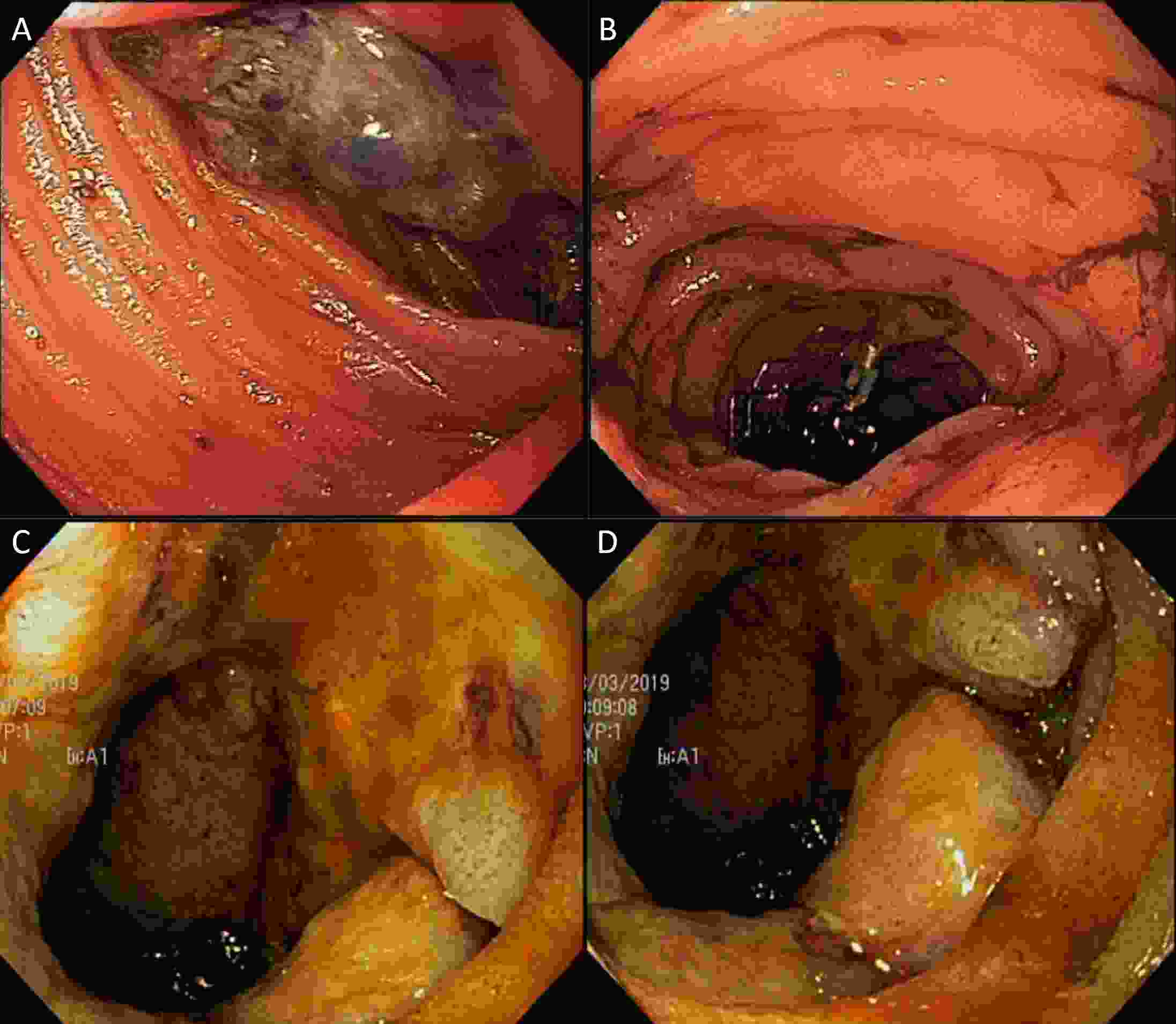
Small bowel tumors (SBTs) have been increasingly diagnosed in recent decades. The pathogenesis of this increment is largely unknown, but advances in radiological and endoscopic methods facilitate the improvement of the diagnosis. Capsule endoscopy (CE) and device-assisted enteroscopy (DAE) allow the clinician to assess the entire small bowel in the search for suspicious lesions, or a cause of symptoms. In this review, we discuss the role of enteroscopy, techniques and strategies in the diagnosis and management of SBTs, and a brief description of the most common tumors.
Small bowel tumors (SBTs) have been increasingly diagnosed in recent decades. The pathogenesis of this increment is largely unknown, but advances in radiological and endoscopic methods facilitate the improvement of the diagnosis. Capsule endoscopy (CE) and device-assisted enteroscopy (DAE) allow the clinician to assess the entire small bowel in the search for suspicious lesions, or a cause of symptoms. In this review, we discuss the role of enteroscopy, techniques and strategies in the diagnosis and management of SBTs, and a brief description of the most common tumors.
2020, 32(3): 334-346.
doi: 10.21147/j.issn.1000-9604.2020.03.05
Abstract:
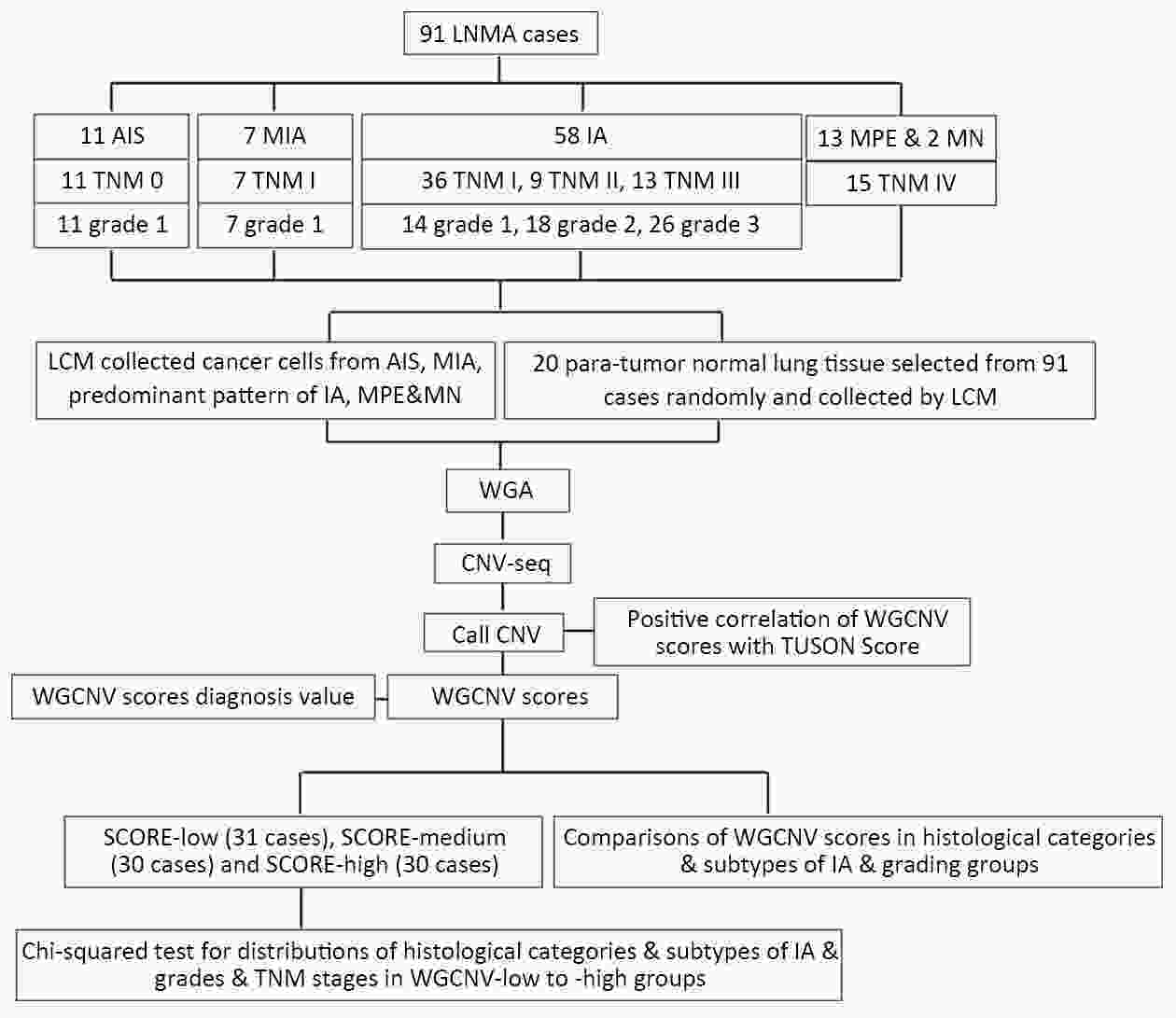
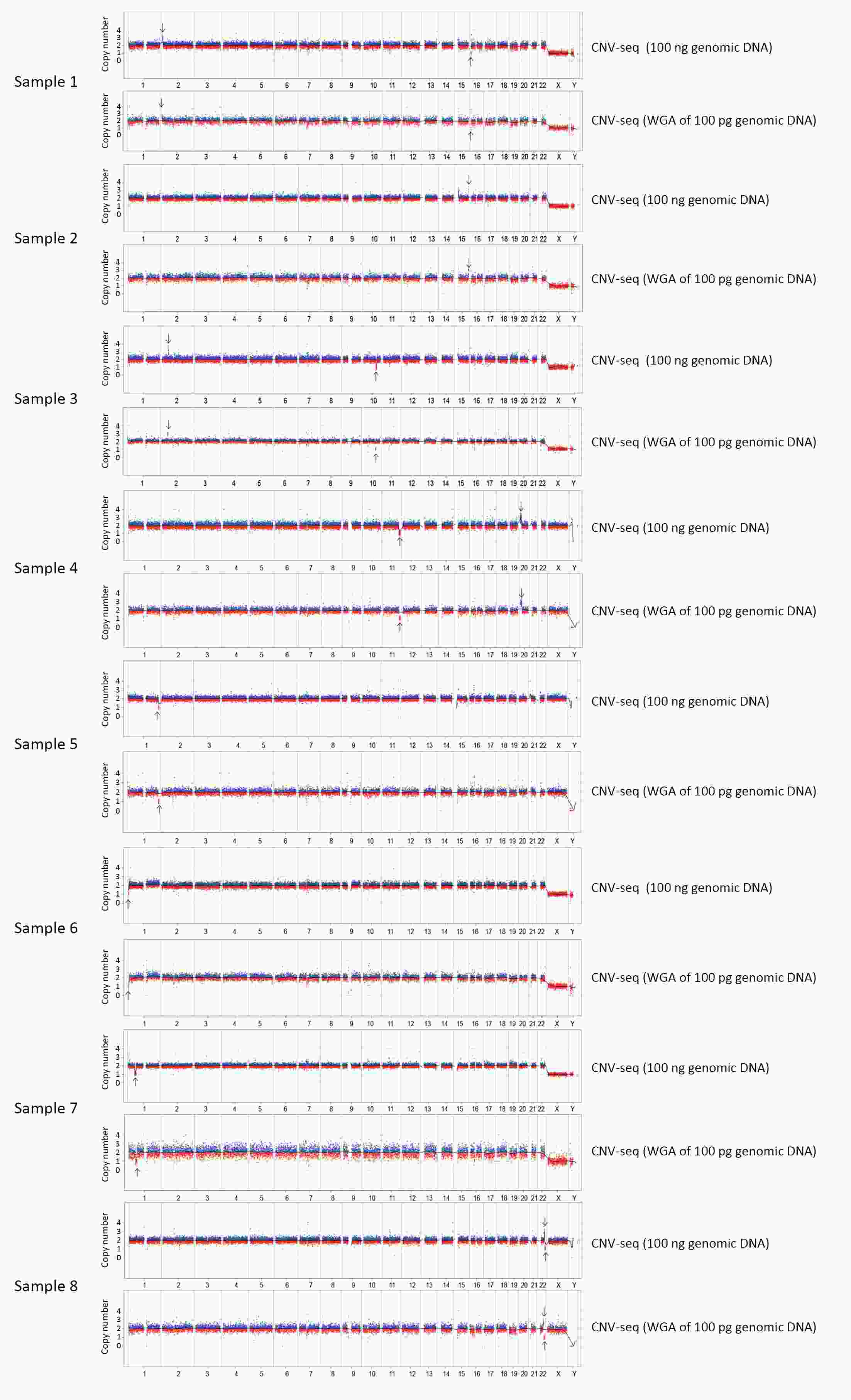
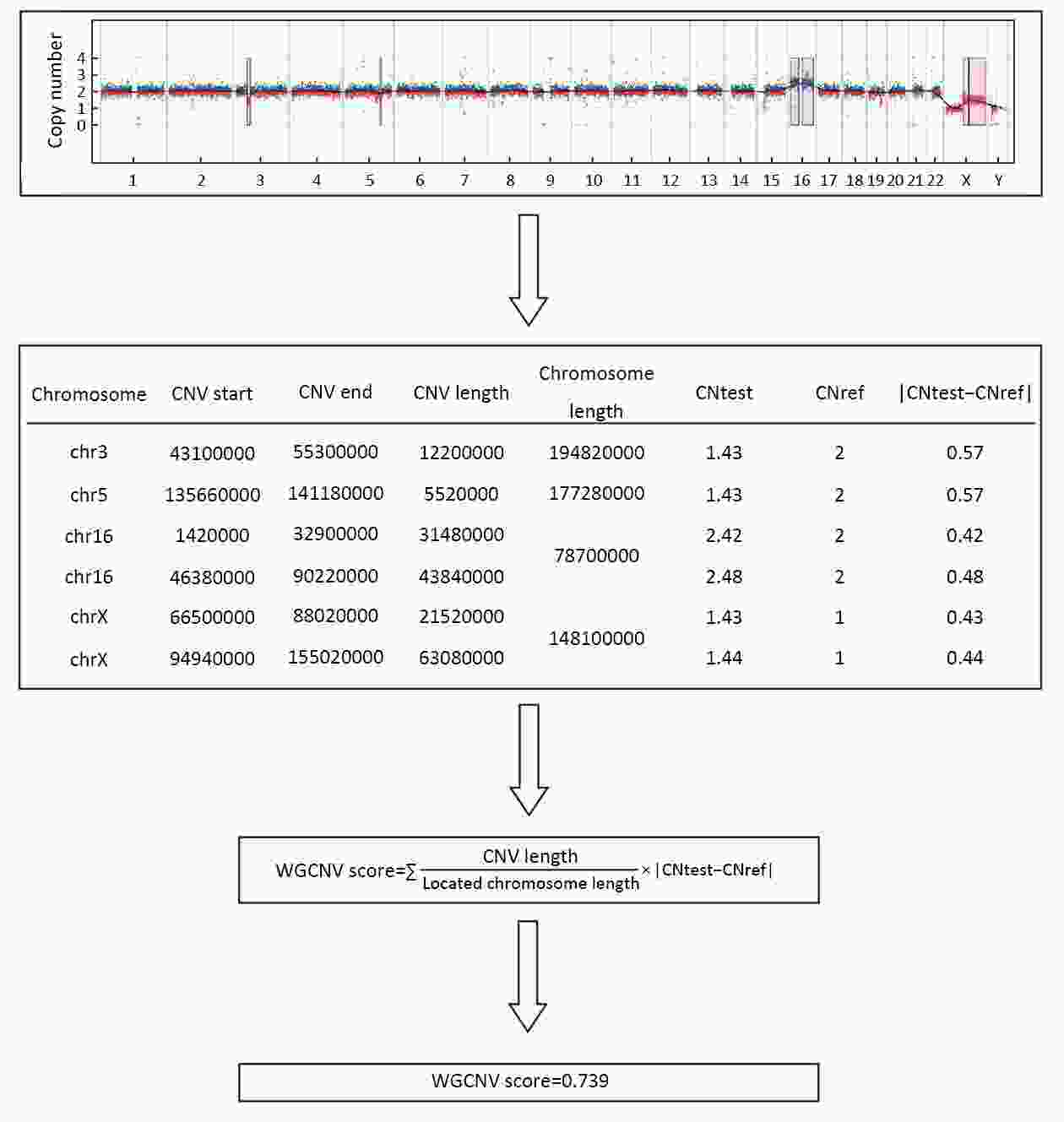
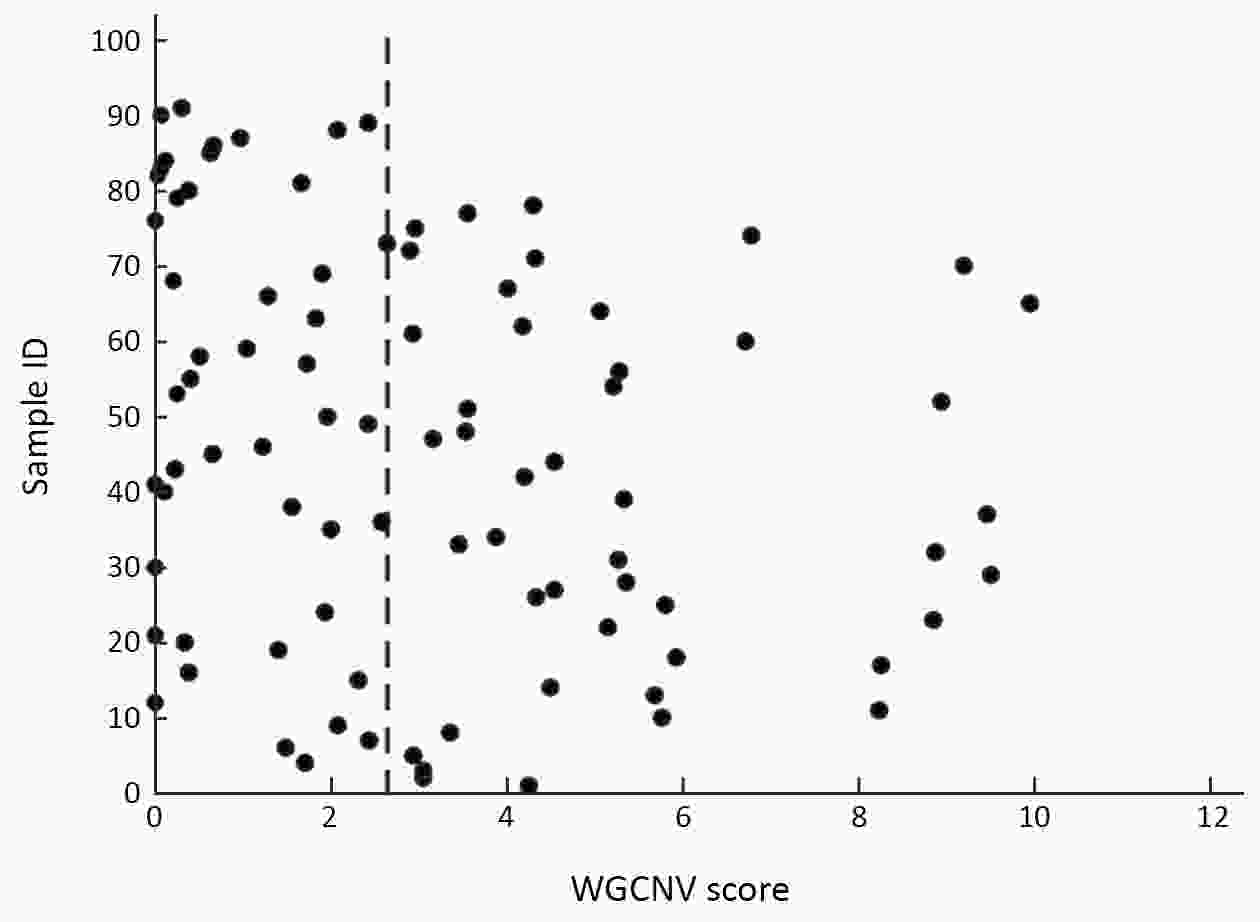
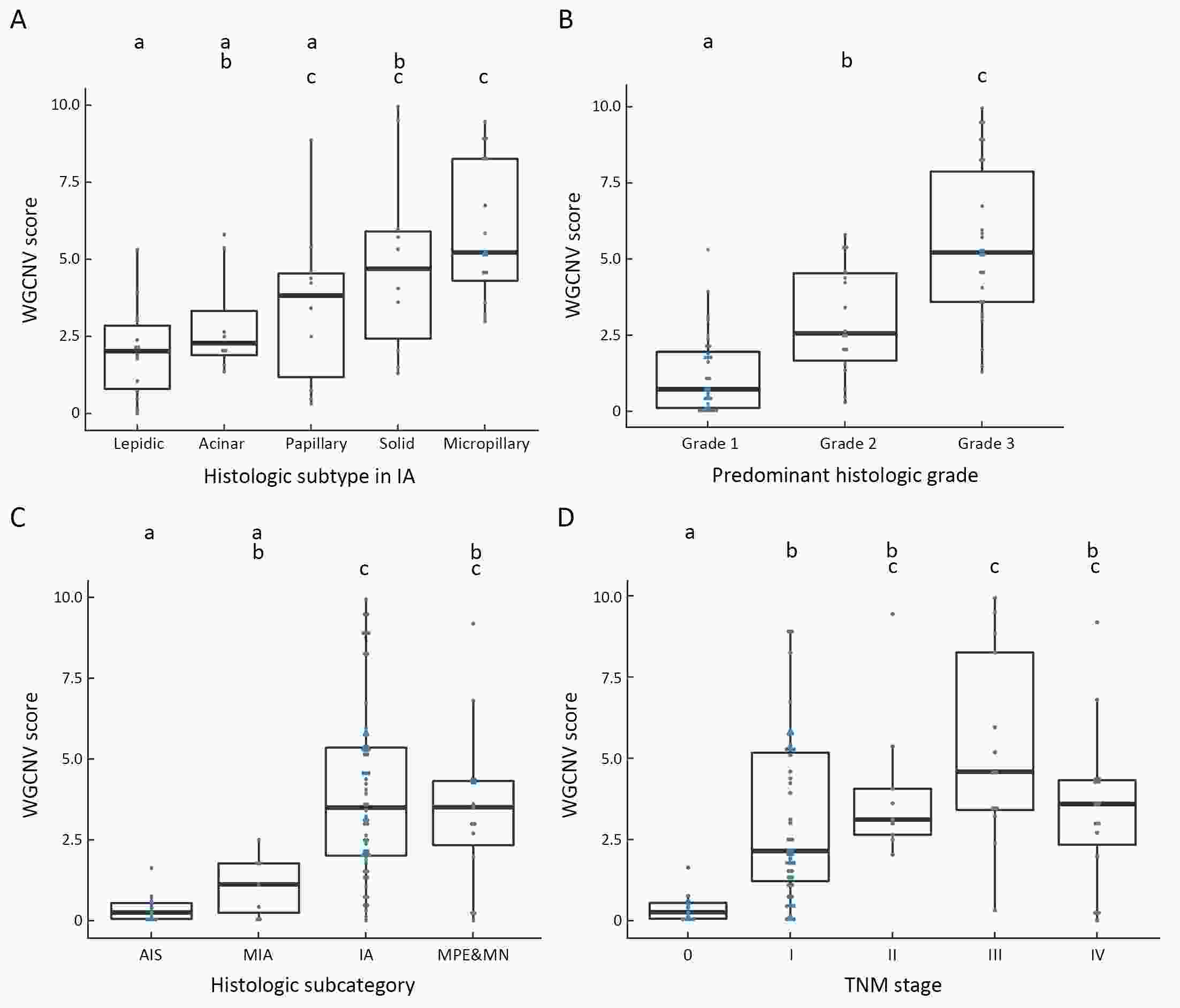
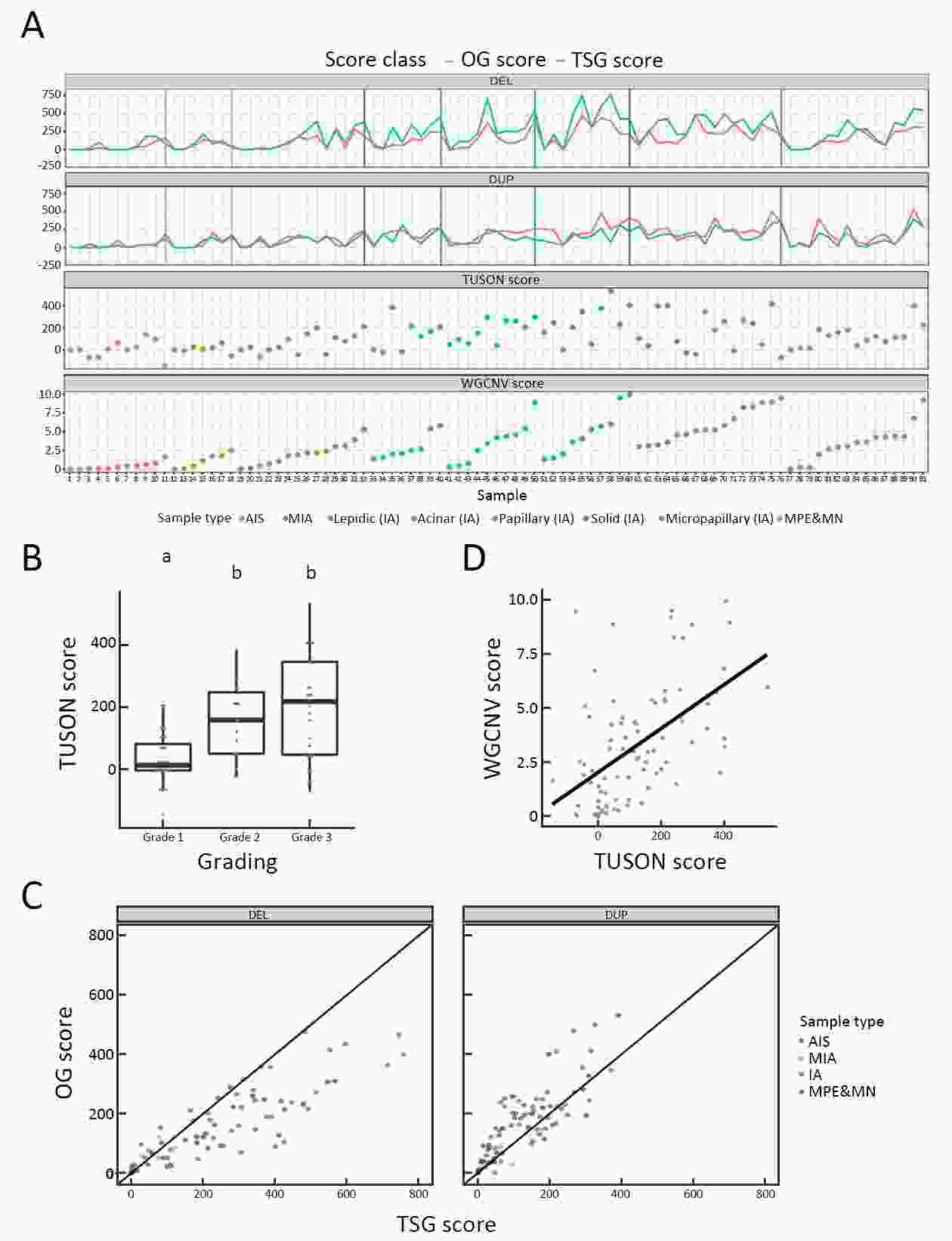
ObjectiveHistology grade, subtypes and TNM stage of lung adenocarcinomas are useful predictors of prognosis and survival. The aim of the study was to investigate the relationship between chromosomal instability, morphological subtypes and the grading system used in lung non-mucinous adenocarcinoma (LNMA). MethodsWe developed a whole genome copy number variation (WGCNV) scoring system and applied next generation sequencing to evaluate CNVs present in 91 LNMA tumor samples. ResultsHigher histological grades, aggressive subtypes and more advanced TNM staging were associated with an increased WGCNV score, particularly in CNV regions enriched for tumor suppressor genes and oncogenes. In addition, we demonstrate that 24-chromosome CNV profiling can be performed reliably from specific cell types (<100 cells) isolated by sample laser capture microdissection. ConclusionsOur findings suggest that the WGCNV scoring system we developed may have potential value as an adjunct test for predicting the prognosis of patients diagnosed with LNMA.
2020, 32(3): 347-360.
doi: 10.21147/j.issn.1000-9604.2020.03.06
Abstract:
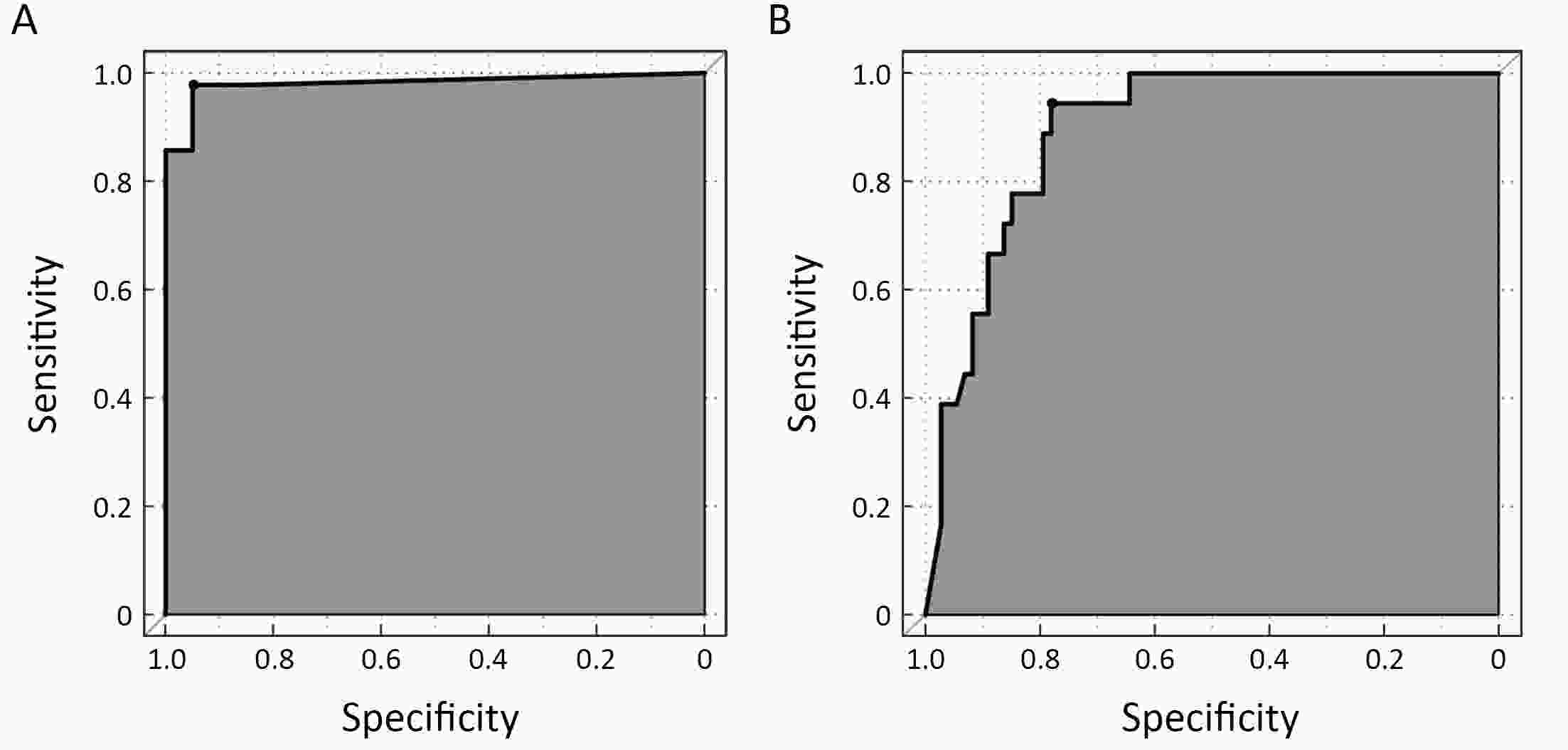
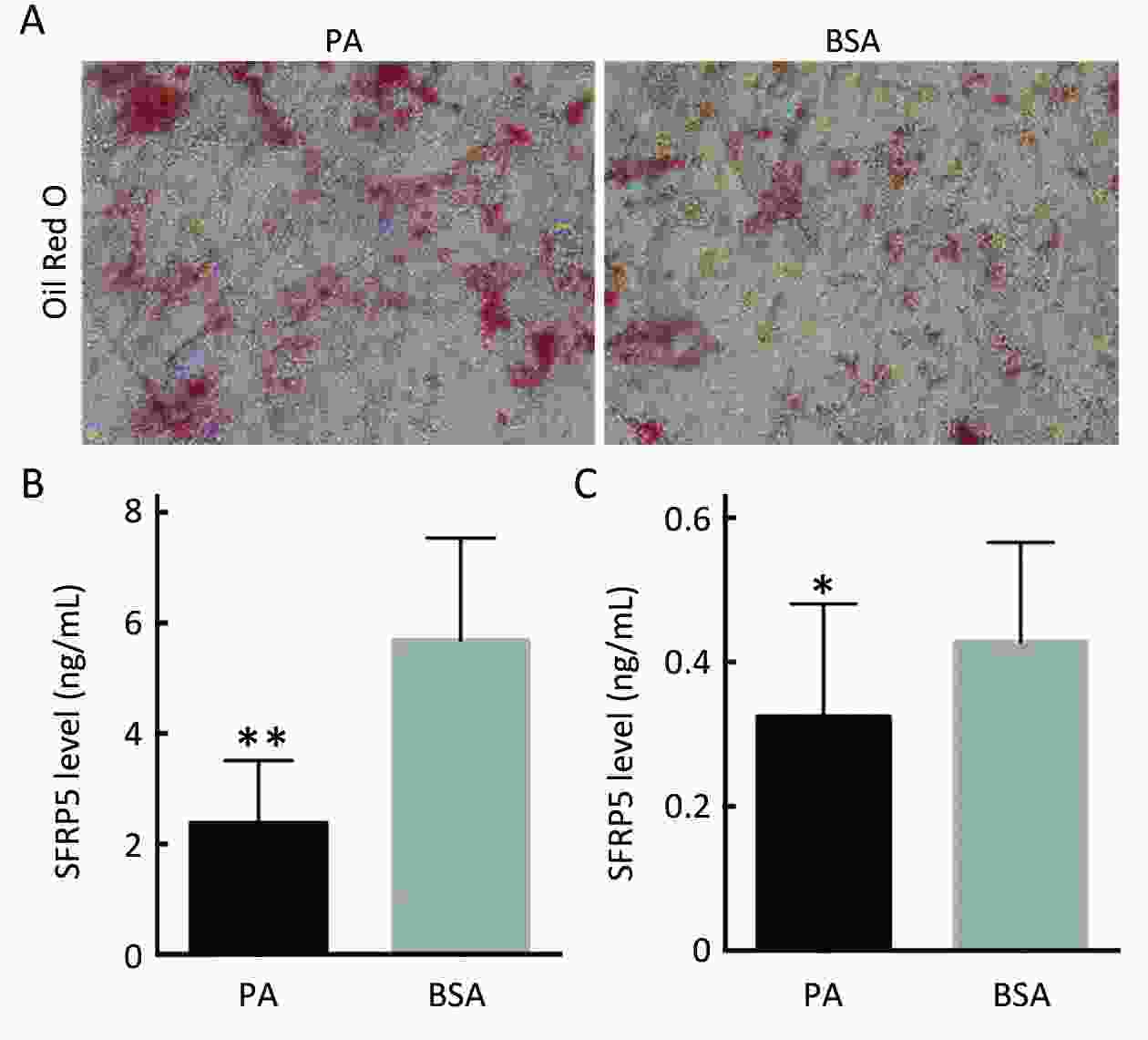
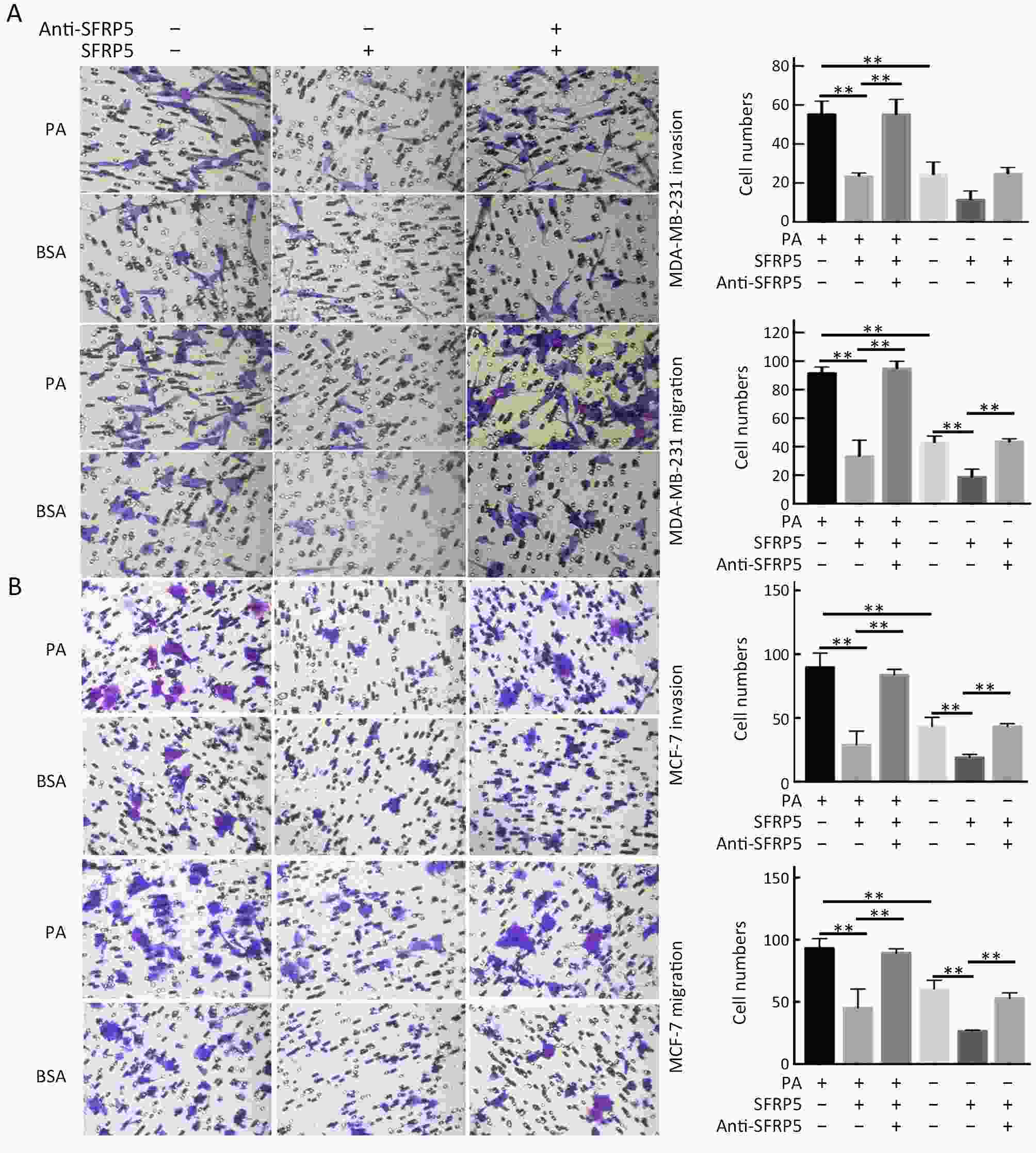
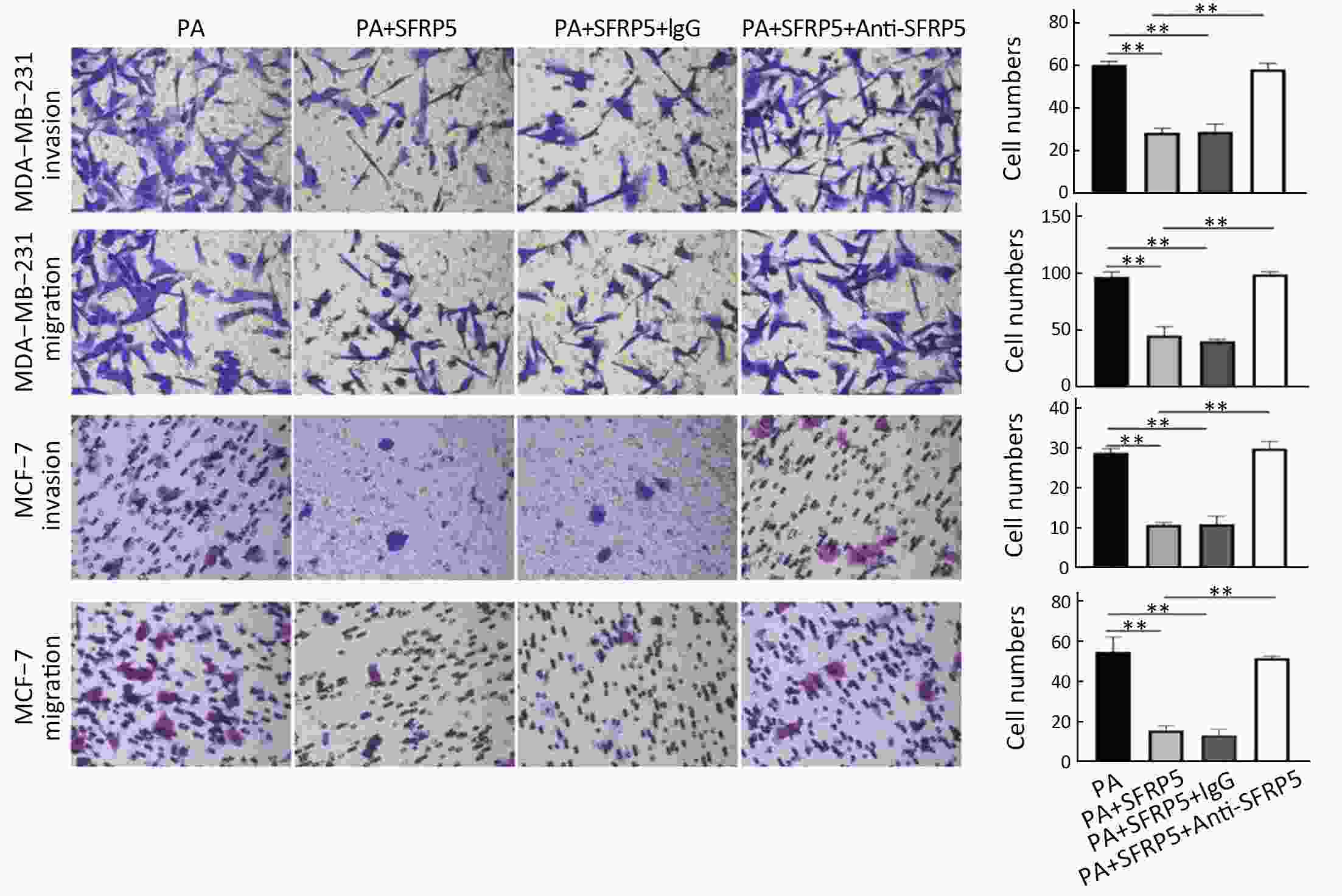
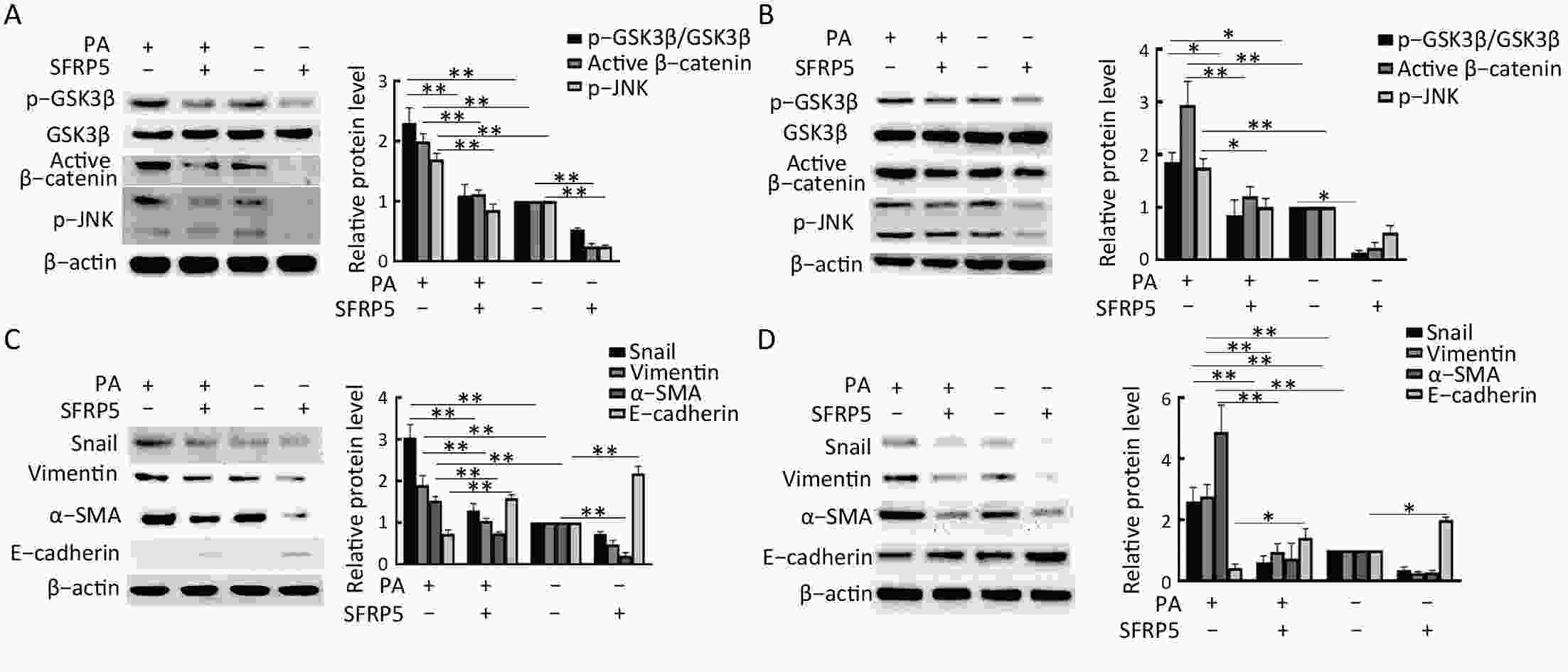
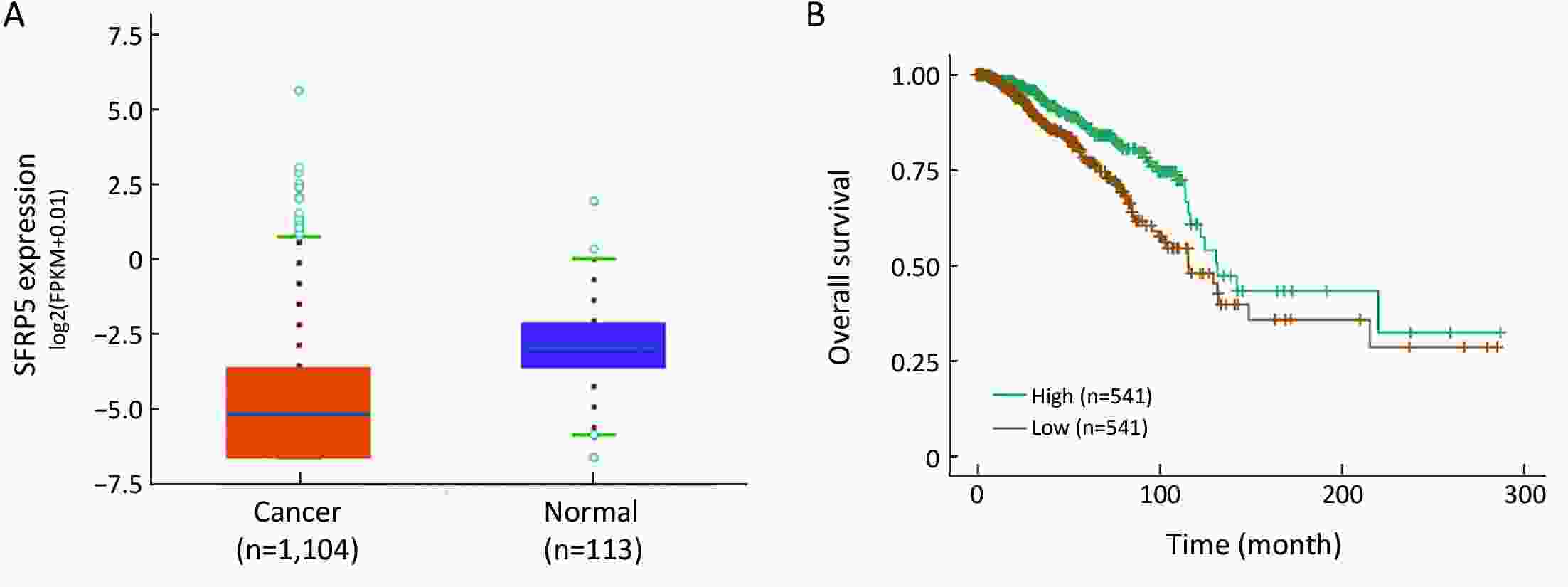
ObjectiveObesity is closely associated with metastasis in breast cancer patients. Secreted frizzled-related protein 5 (SFRP5), one of the novel adipokines with anti-inflammatory properties, is associated with obesity. This study aims to study the role of SFRP5 in the crosstalk between obesity and breast cancer metastasis and identify the underlying mechanism. Methods3T3-L1 pre-adipocytes were differentiated to mature adipocytes and a hypertrophic adipocyte model was induced with palmitic acid (PA). Cell motility was measured in MDA-MB-231 and MCF-7 breast cancer cells co-cultured with adipocytes conditioned medium (CM) with or without SFRP5 protein. Wnt and epithelial-mesenchymal transition (EMT) signal pathways were investigated by western blot. Circulating SFRP5 level in 218 breast cancer patients and the association with clinicopathologic characteristics of breast cancer were further determined. Online databases ENCORI and PREDICT Plus were used to exam the link between SFRP5 and prognosis. ResultsReduced SFRP5 level was detected in the hypertrophic adipocyte model. Recombinant SFRP5 protein inhibited MDA-MB-231 and MCF-7 cells invasion and migration induced by PA-treated adipocyte CM, and SFRP5 inhibition by specific antibody reversed the effect of SFRP5. Furthermore, SFRP5 significantly inhibited Wnt and downstream EMT in breast cancer cells. Low circulating SFRP5 level correlated with body mass index (BMI), lymph node (LN) metastasis, TNM stage and high Ki67 expression in breast cancer patients. Increased SFRP5 level was associated with favorable predicted survival. Kaplan-Meier curves showed high SFRP5 level in tumor tissue was associated with better outcome of breast cancer patients. ConclusionsOur findings demonstrated SFRP5 is a vital adipokine that mediates the crosslink between obesity and the metastatic potential of breast cancer. Promotion of SFRP5 expression in the adipose microenvironment may represent a novel approach for preventing breast cancer metastasis.
2020, 32(3): 361-369.
doi: 10.21147/j.issn.1000-9604.2020.03.07
Abstract:
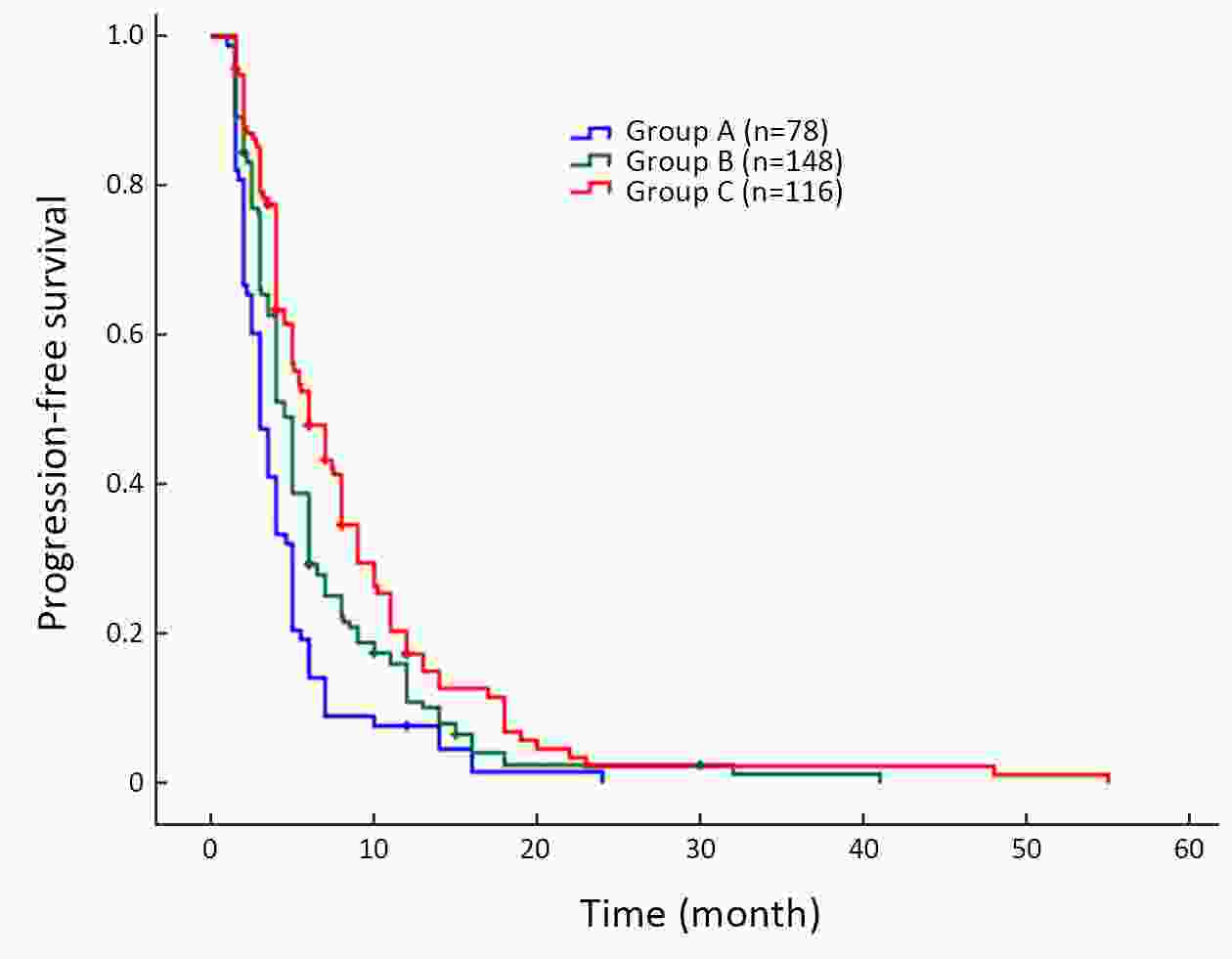
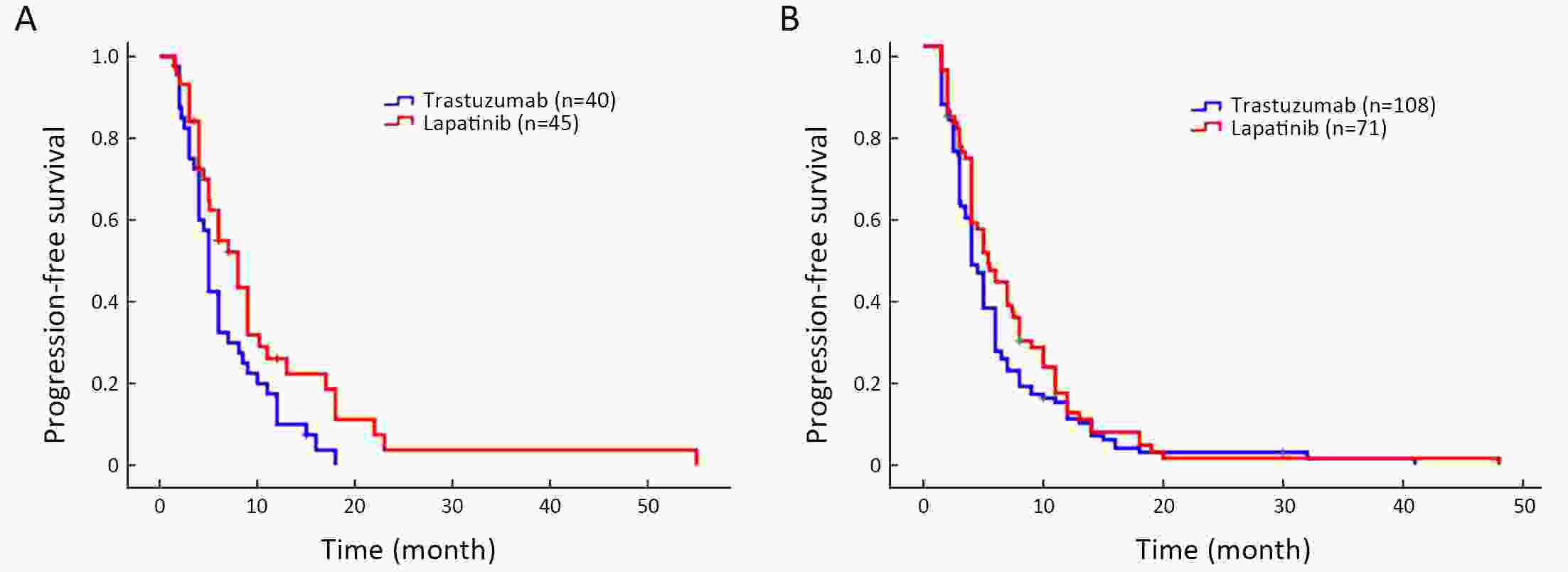
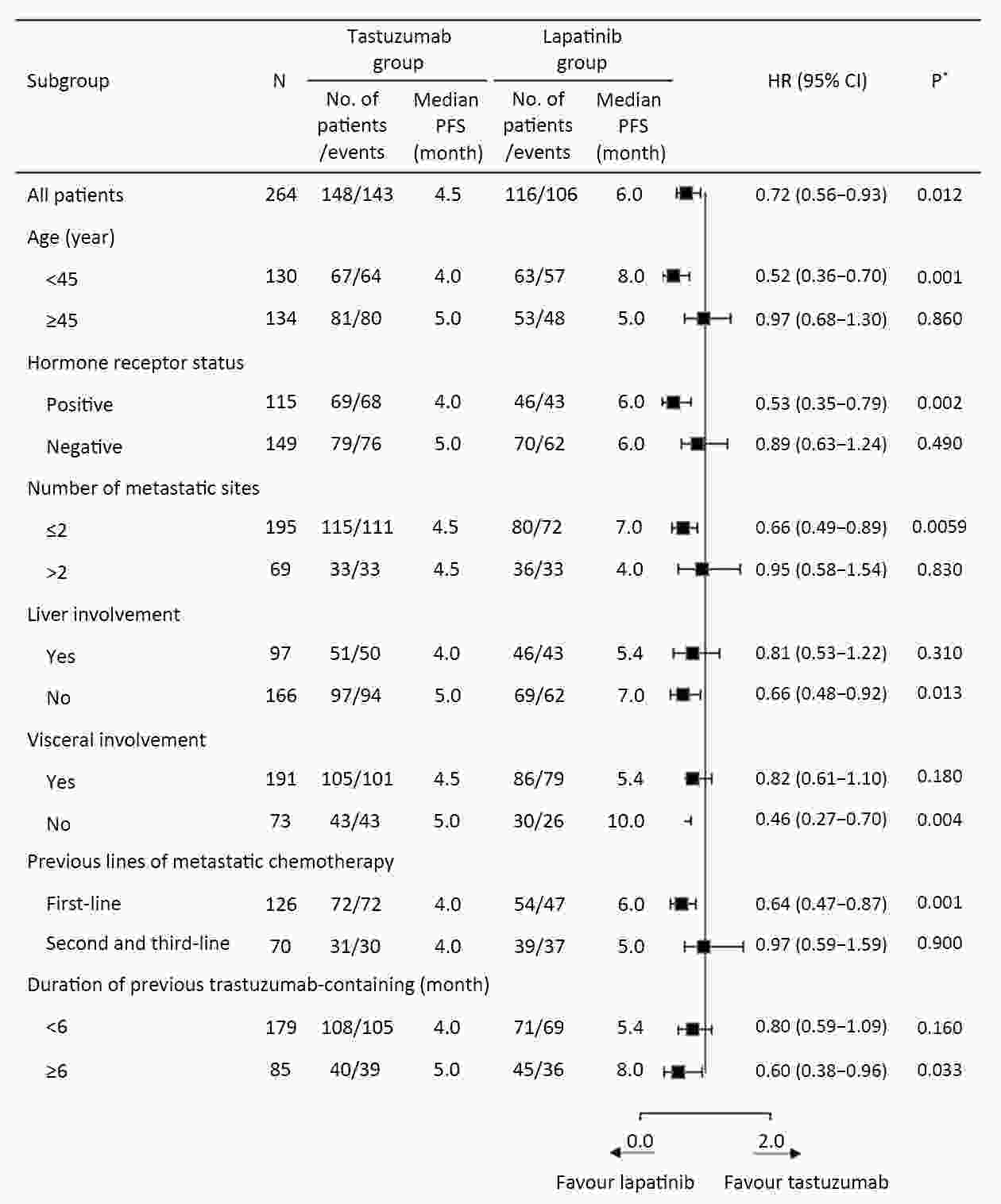
ObjectiveSeveral studies have demonstrated different benefits for patients whose disease progressed despite previous trastuzumab treatment. Due to limited real-world data, we evaluate the effectiveness of anti-human epidermal growth factor receptor 2 (HER2) therapy (lapatinib or trastuzumab) plus chemotherapy or chemotherapy alone in patients who were previously treated with trastuzumab-containing regimens and investigate factors associated with effectiveness. And we further show the effectiveness of the two anti-HER2 therapy groups. MethodsA total of 342 HER2-positive metastatic breast cancer (MBC) patients whose disease progressed during prior anti-HER2 (trastuzumab) and standard chemotherapy therapy from Department of Breast Oncology, the Fifth Medical Center of Chinese PLA General Hospital, from August 2010 to December 2016 were included. Seventy-eight patients received standard chemotherapy only, 148 patients continued to receive trastuzumab and switched to other chemotherapy drugs, and 116 patients received tyrosine-kinase inhibitors (TKIs; lapatinib) and chemotherapy. The main outcome measures were progression-free survival (PFS), overall response rate (ORR), and clinical benefit rate (CBR). Subgroup analyses were conducted to identify patient characteristics associated with the greatest clinical benefit. ResultsAfter a median follow-up of 26.2 (range, 2.0−56.0) months, PFS significantly improved with anti-HER2 therapy compared with chemotherapy alone: median 6.0 months with lapatinib [95% confidence interval (95% CI), 4.53−7.47], 4.5 months with trastuzumab (95% CI, 3.99−5.01) vs. 3.0 months with chemotherapy alone (95% CI, 2.42−3.58); stratified hazard ratio (HR)=0.70, 95% CI, 0.60−0.81; P<0.0001. The ORR values were 33.6%, 25.0% and 12.8 %, respectively, the CBR values were 60.3%, 48.6% and 26.9%, respectively. The effectiveness of lapatinib group and trastuzumab group were further analyzed. In multivariate analysis, lapatinib group was associated with a longer PFS, after controlling other potential confounders (HR=0.68, 95% CI, 0.52−0.90; P=0.006). ConclusionsThe combination of TKIs and chemotherapy was effective in this cohort previously treated with trastuzumab treatment. Therefore, TKIs combined with chemotherapy is an option for Chinese HER2-positive MBC patients previously treated with trastuzumab treatment.
2020, 32(3): 370-382.
doi: 10.21147/j.issn.1000-9604.2020.03.08
Abstract:
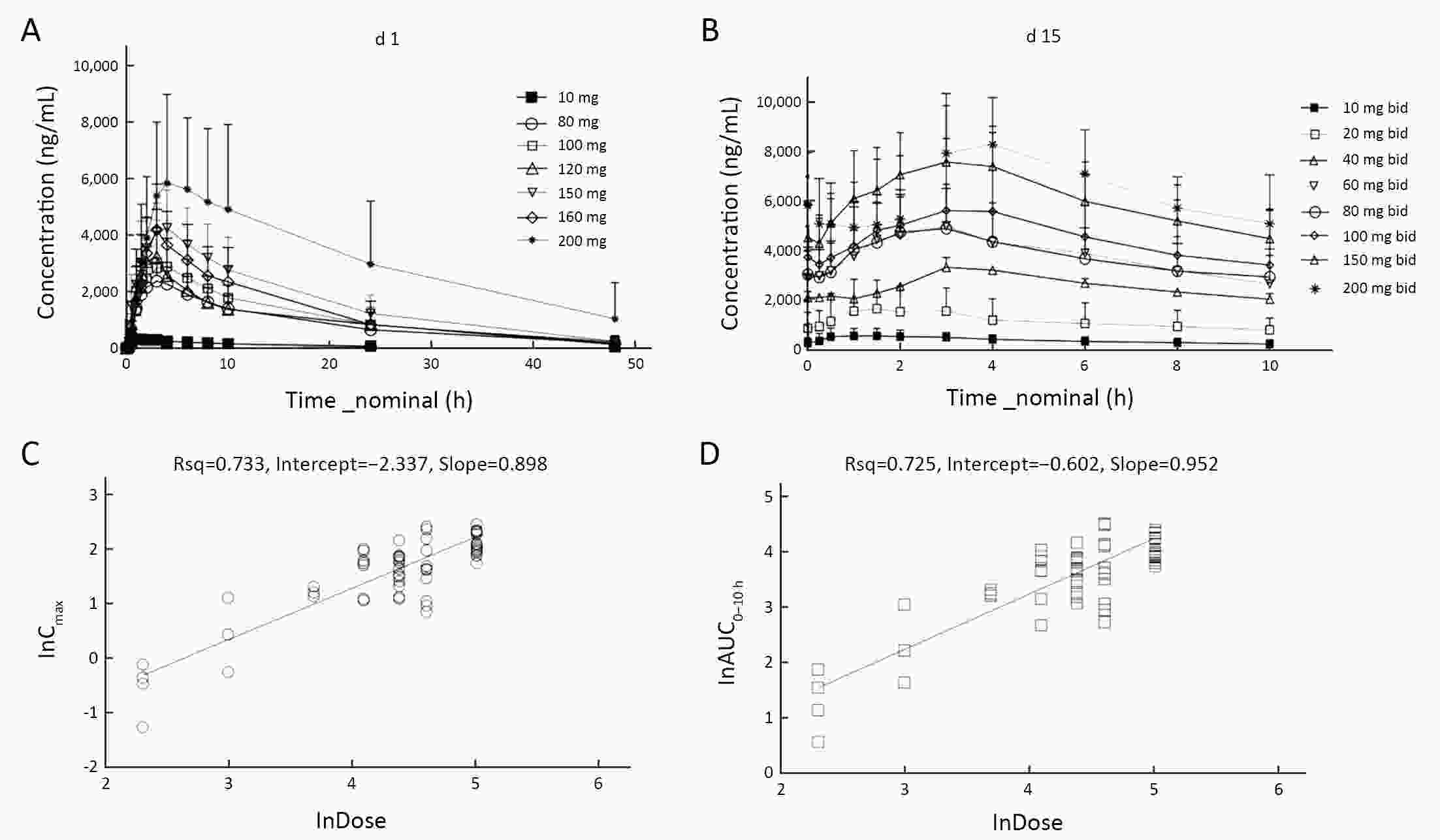
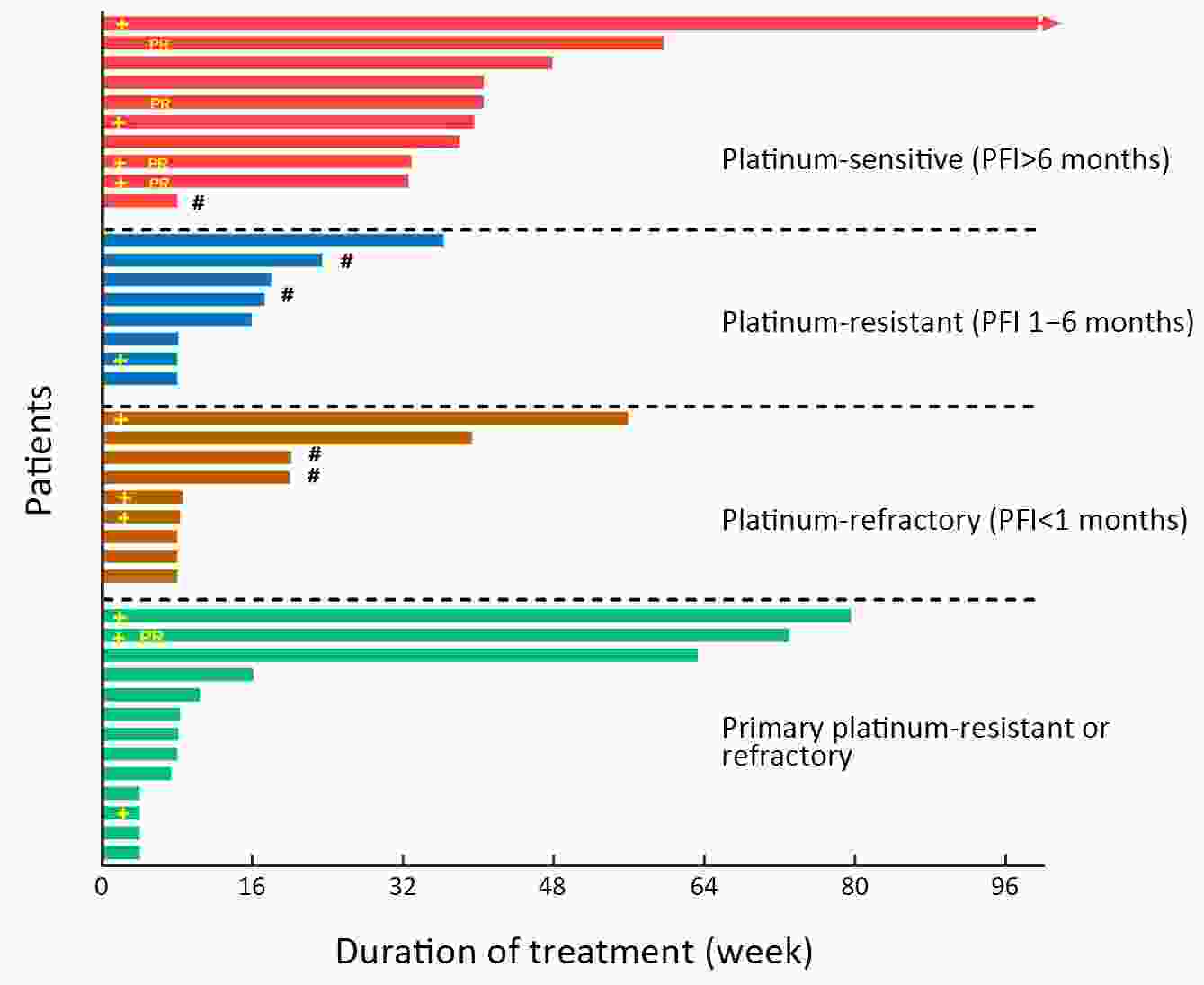
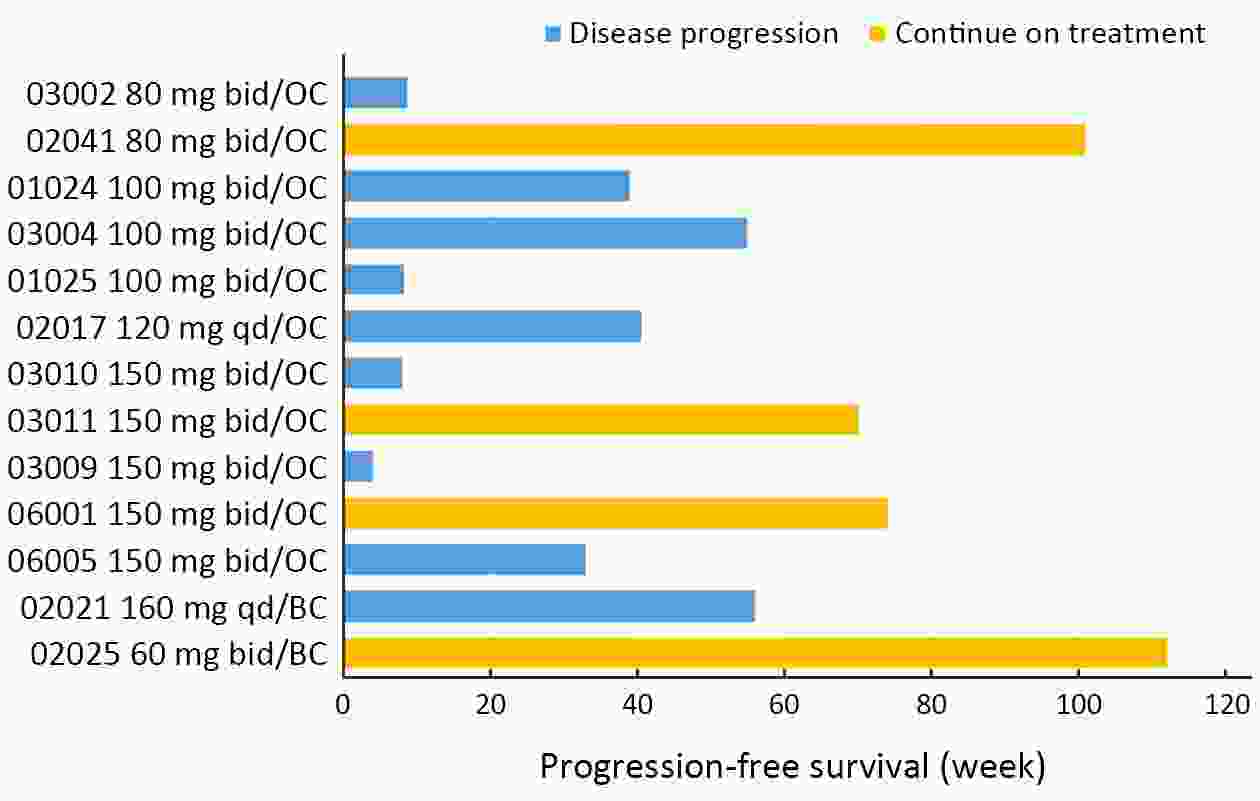
ObjectiveFluzoparib (SHR3162) is a novel, potent poly(ADP-ribose) polymerases (PARP)1, 2 inhibitor that showed anti-tumor activity in xenograft models. We conducted a phase I, first-in-human, dose-escalation and expansion (D-Esc and D-Ex) trial in patients with advanced solid cancer. MethodsThis was a 3+3 phase I D-Esc trial with a 3-level D-Ex at 5 hospitals in China. Eligible patients for D-Esc had advanced solid tumors refractory to standard therapies, and D-Ex enrolled patients with ovarian cancer (OC). Fluzoparib was administered orally once or twice daily (bid) at 11 dose levels from 10 to 400 mg/d. Endpoints included dose-finding, safety, pharmacokinetics, and antitumor activity. ResultsSeventy-nine patients were enrolled from March, 2015 to January, 2018 [OC (47, 59.5%); breast cancer (BC) (16, 20.3%); colorectal cancer (8, 10.1%), other tumors (8, 10.1%)]; 48 patients were treated in the D-Esc arm and 31 in the D-Ex arm. The maximum tolerated dose (MTD) was 150 mg bid, with a half-life of 9.14 h. Grade 3/4 adverse events included anemia (7.6%) and neutropenia (5.1%). The objective response rate (ORR) was 30% (3/10) in patients with platinum-sensitive OC and 7.7% (1/13) in patients with BC. Among patients treated with fluzoparib ≥120 mg/d, median progression-free survival (mPFS) was 7.2 [95% confidence interval (95% CI), 1.8−9.3] months in OC, 9.3 (95% CI, 7.2−9.3) months in platinum-sensitive OC, and 3.5 (range, 2.0−28.0) months in BC. In patients with germline BC susceptibility gene mutation (gBRCAMut) (11/43 OC; 2/16 BC), mPFS was 8.9 months for OC (range, 1.0−23.2; 95% CI, 1.0−16.8) and 14 and 28 months for BC (those two patients both also had somatic BRCAMut). ConclusionsThe MTD of fluzoparib was 150 mg bid in advanced solid malignancies. Fluzoparib demonstrated single-agent antitumor activity in BC and OC, particularly in BRCAMut and platinum-sensitive OC.
2020, 32(3): 383-394.
doi: 10.21147/j.issn.1000-9604.2020.03.09
Abstract:
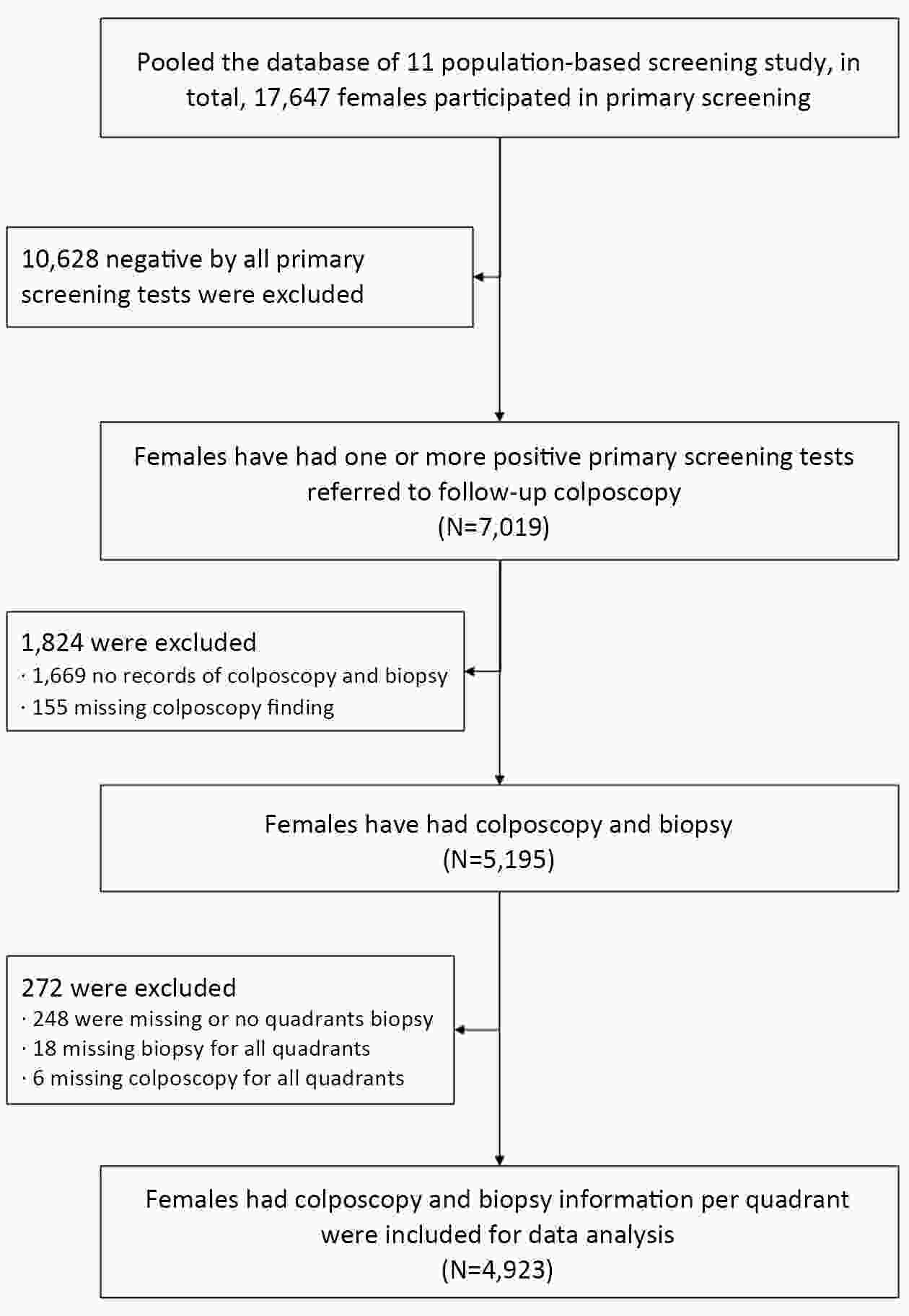
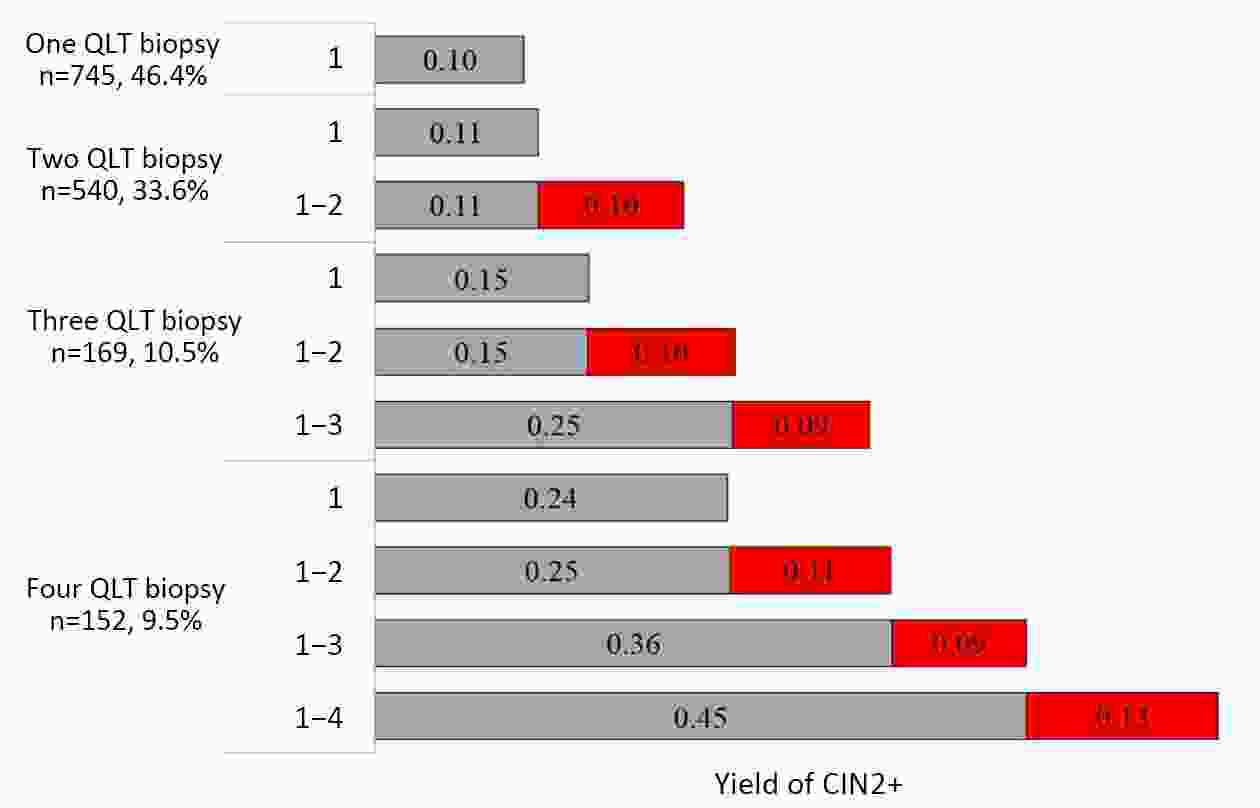
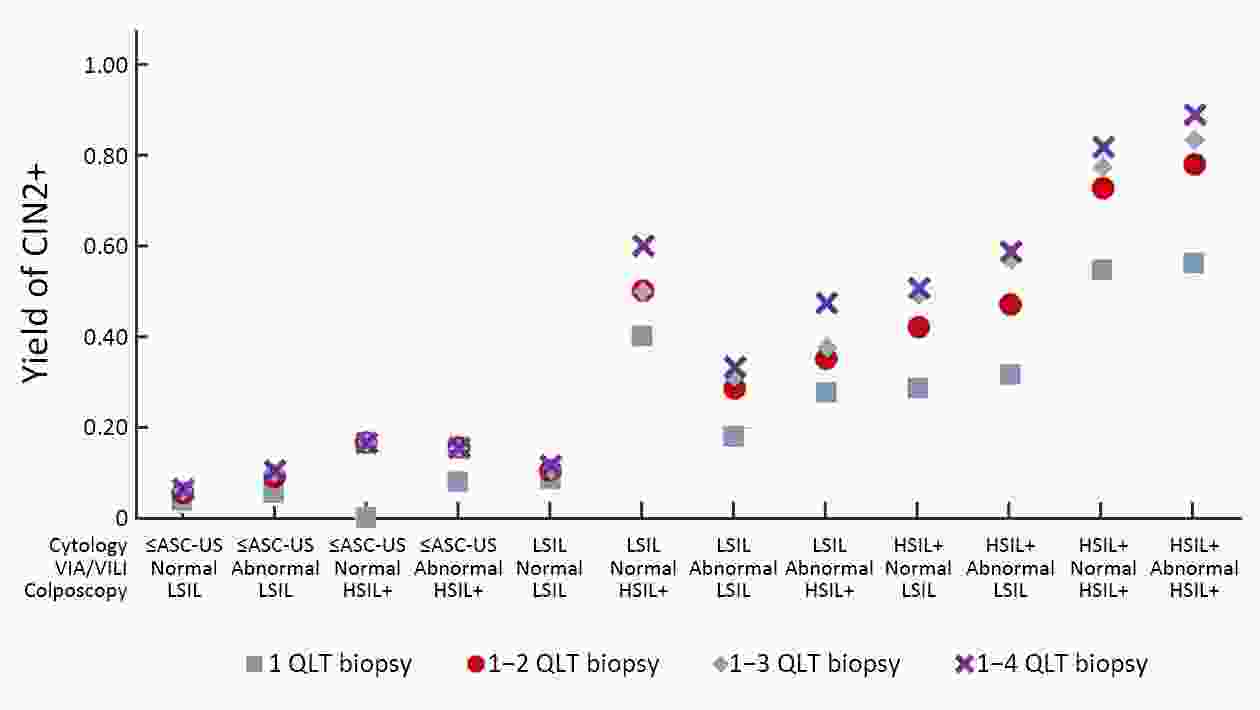
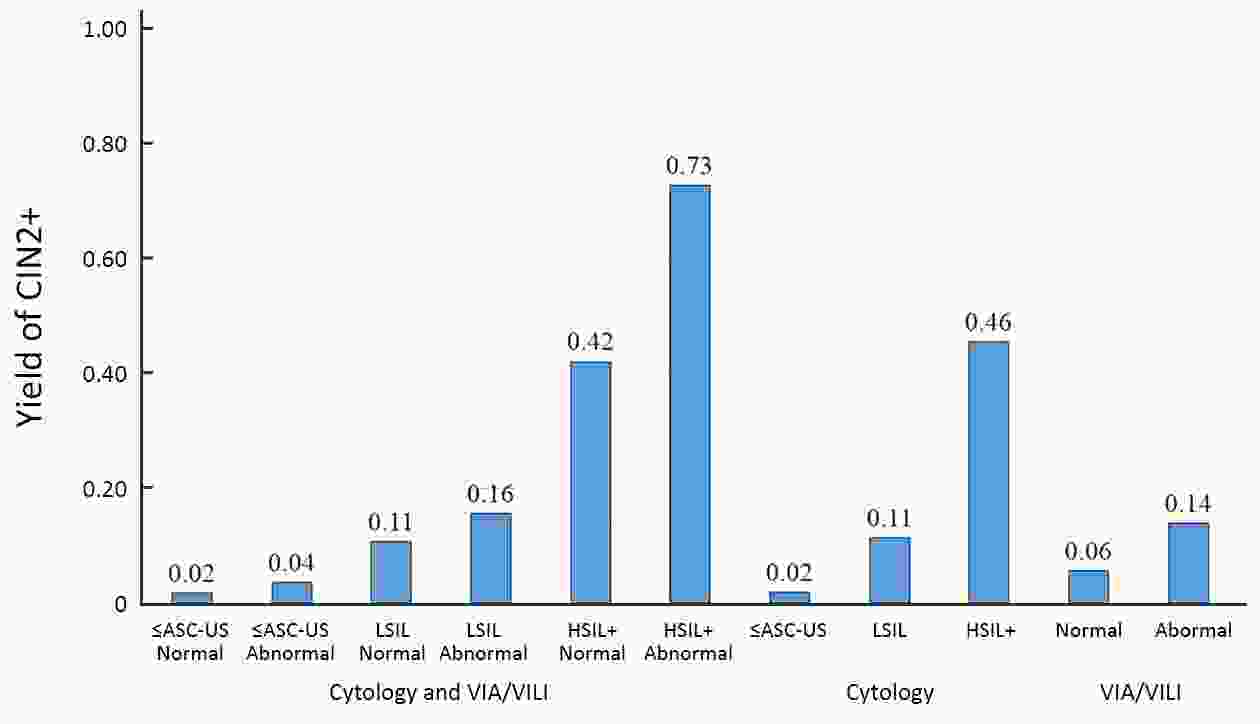
ObjectiveThe accuracy of colposcopy-guided biopsy is key to the success of colposcopic triage in cervical cancer screening programs. However, there is no widely adopted biopsy guideline up to date. Our study aimed to determine whether multi-quadrants biopsy improves the yield of cervical lesions. MethodsEleven population-based cervical cancer screening studies were conducted in China. Cytology, high-risk human papillomavirus (hrHPV) testing and visual inspection were performed for primary screening. Females positive on one or more tests were referred for colposcopy and biopsy. The proportion of detected cervical intraepithelial neoplasia (CIN)2+ and yields by quadrant lesion-targeted biopsy or 4-quadrant random biopsy were compared. ResultsAmong 4,923 females included, 1,606 had quadrant lesion-targeted biopsy, and 3,317 had 4-quadrant random biopsy. The cumulative CIN2+ yield increased from 0.10 for only one quadrant-targeted biopsy to 0.21, 0.34, and 0.58 for at most two, three and four quadrants targeted biopsies. Among hrHPV positive females with high-grade squamous intraepithelial lesion (HSIL)+ cytology, the cumulative CIN2+ yield of a second targeted biopsy in another quadrant was significantly increased (P<0.05). Among hrHPV-negative females, the yield of 4-quadrant random biopsies was 0.005, and the yield by lesion-targeted biopsies was 0.017. For hrHPV positive females who had 4-quadrant random biopsy, the additional CIN2+ yield for HSIL+, low-grade squamous intraepithelial lesion (LSIL) cytology, or abnormal visual inspection via acetic acid and Lugol’s iodine (VIA/VILI) were 0.46, 0.11, 0.14. ConclusionsA 4-quadrant random biopsy is recommended only for hrHPV positive females with HSIL cytology, and is acceptable if hrHPV positive with LSIL cytology or with abnormal VIA/VILI. Our findings add evidences for an objective and practical biopsy standard to guide colposcopy in cervical cancer screening programs in low- and middle-income countries.
2020, 32(3): 395-402.
doi: 10.21147/j.issn.1000-9604.2020.03.10
Abstract:
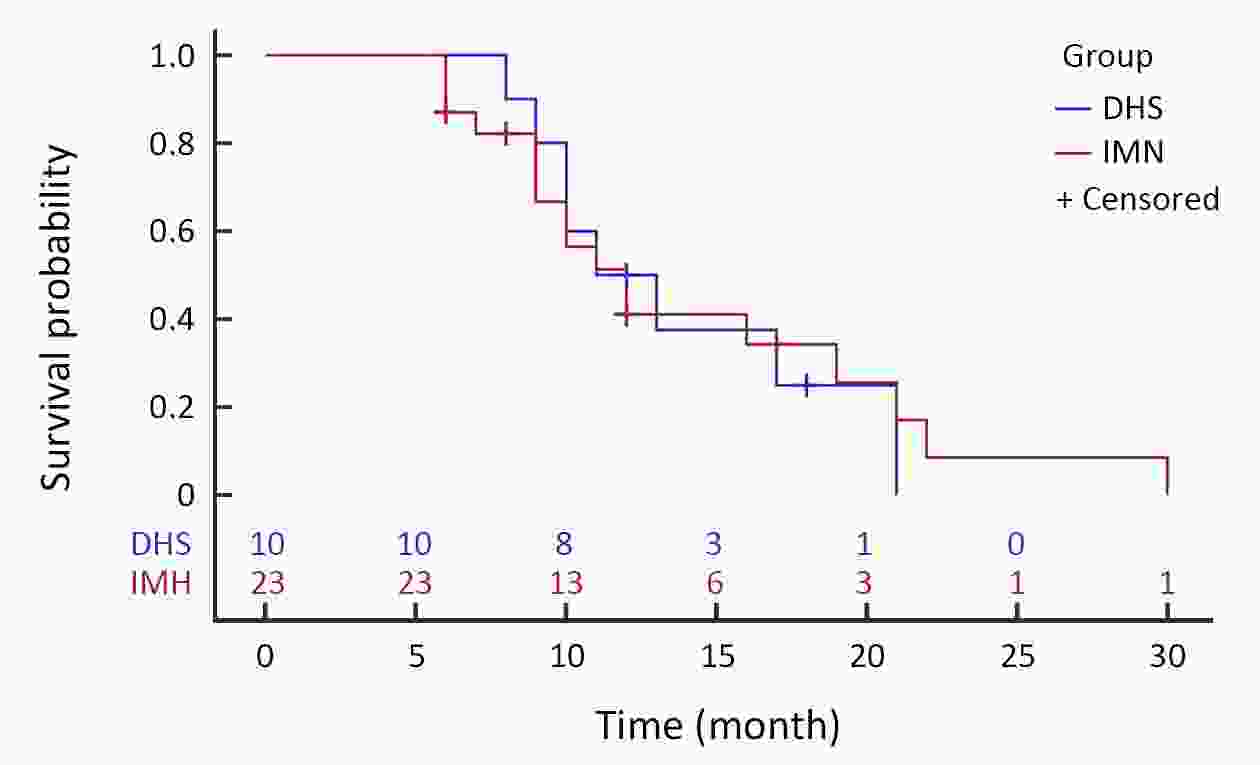
ObjectiveTo compare the outcomes of dynamic hip screws (DHS) and intramedullary nailing (IMN) in the treatment of extra-capsular metastatic carcinoma of the proximal femur. MethodsA retrospective case analysis method was used to examine data of patients with proximal metastatic cancer of the femur who were treated with internal fixation in Department of Orthopaedics, Beijing Friendship Hospital, from January 2007 to December 2018. Blood loss, postoperative pain, functional score, length of stay, and survival rates were compared, and postoperative complications were assessed. ResultsComplete follow-up data were available for 33 patients. The mean follow-up period was 12.2±3.6 (range: 9−32) months and the average age was 72.3±4.7 (range: 59−83) years old. There were 20 females and 13 males. Twenty-three patients had undergone IMN and 10 DHS, according to bone defects and the patient’s overall condition. The median survival time was 10 months in the IMN group and 11 months in the DHS group. Duration of surgery (t=−7.366, P<0.001) and length of hospital stay (t=−3.509, P<0.001) differed significantly between the two groups. There was one case of breakage of internal fixation in the IMN group. ConclusionsThere was no significant difference between DHS and IMN in terms of surgical efficacy. IMN and DHS were different in terms of surgical time and hospital stay. However, due to the limited number of cases in this study, multi-factor analysis has not been performed and needs to be further verified in future analysis. When developing a surgical plan, it is recommended to consider the patient’s condition and the surgeon’s experience.
2020, 32(3): 403-407.
doi: 10.21147/j.issn.1000-9604.2020.03.11
Abstract:
2020, 32(3): 414.
doi: 10.21147/j.issn.1000-9604.2020.03.13
Abstract:

 Abstract
Abstract FullText HTML
FullText HTML PDF 248KB
PDF 248KB