2020 Vol.32(6)
Display Mode: |
2020, 32(6): 673-682.
doi: 10.21147/j.issn.1000-9604.2020.06.01
Abstract:
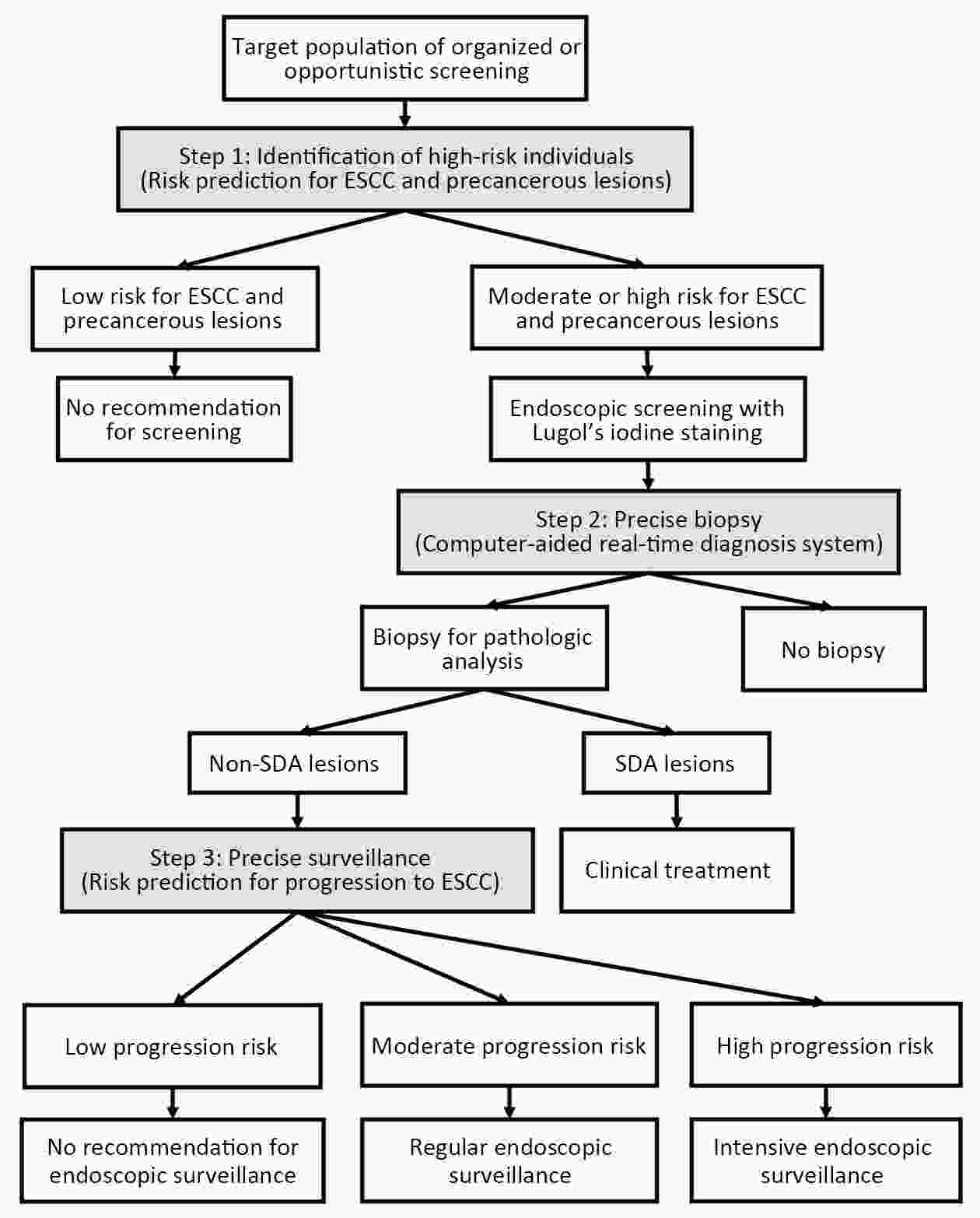
Esophageal squamous cell carcinoma (ESCC) is the predominant subtype of esophageal cancer in China, and this neoplasm is associated with high morbidity and mortality as well as clear geographical heterogeneity. Since primary prevention for ESCC lacks a clear intervention target, secondary prevention, also known as screening and early diagnosis and early treatment, has become the mainstay of ESCC prevention and control in China. ESCC screening in China has been subject to decades of evaluation and practice. However, the ESCC screening strategy currently adopted in China has encountered a developmental bottleneck. In this review, we have summarized studies and significant findings for ESCC screening and proposed advancement of screening strategies as follows: 1) evidence from randomized controlled trials is needed to support the effectiveness and health economic value of endoscopic screening for ESCC; 2) the current traditional screening and surveillance strategies warrant reform, and a risk-prediction-based precision strategy should be established; and 3) a deeper understanding of the value of opportunistic screening in the prevention and control of ESCC in China is called for. Due to the low absolute prevalence of precancerous lesions, substantial investment of resources and nonnegligible risks of invasive screening techniques, precision and individualization should be the main direction of cancer screening programs for the future. We advocate cooperation on the part of Chinese scientists to solve this major China-specific health problem in the next decades.
Esophageal squamous cell carcinoma (ESCC) is the predominant subtype of esophageal cancer in China, and this neoplasm is associated with high morbidity and mortality as well as clear geographical heterogeneity. Since primary prevention for ESCC lacks a clear intervention target, secondary prevention, also known as screening and early diagnosis and early treatment, has become the mainstay of ESCC prevention and control in China. ESCC screening in China has been subject to decades of evaluation and practice. However, the ESCC screening strategy currently adopted in China has encountered a developmental bottleneck. In this review, we have summarized studies and significant findings for ESCC screening and proposed advancement of screening strategies as follows: 1) evidence from randomized controlled trials is needed to support the effectiveness and health economic value of endoscopic screening for ESCC; 2) the current traditional screening and surveillance strategies warrant reform, and a risk-prediction-based precision strategy should be established; and 3) a deeper understanding of the value of opportunistic screening in the prevention and control of ESCC in China is called for. Due to the low absolute prevalence of precancerous lesions, substantial investment of resources and nonnegligible risks of invasive screening techniques, precision and individualization should be the main direction of cancer screening programs for the future. We advocate cooperation on the part of Chinese scientists to solve this major China-specific health problem in the next decades.
2020, 32(6): 683-694.
doi: 10.21147/j.issn.1000-9604.2020.06.02
Abstract:
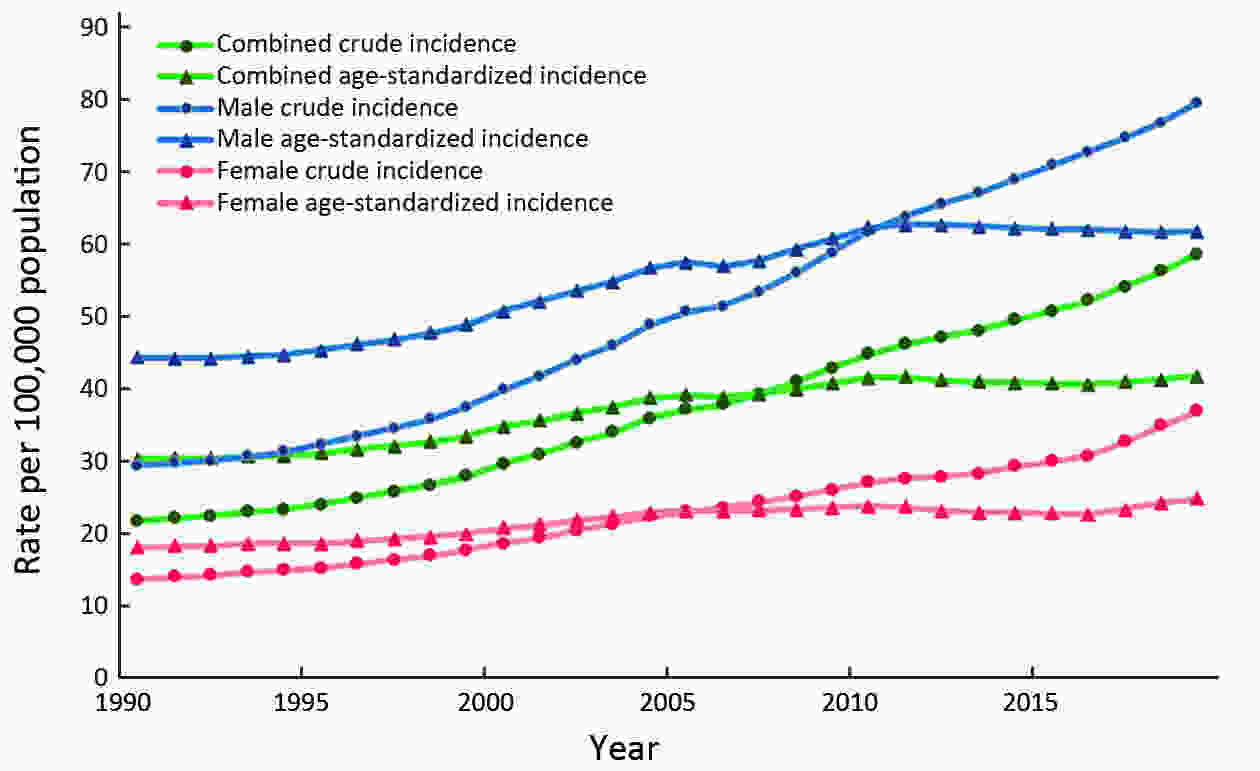
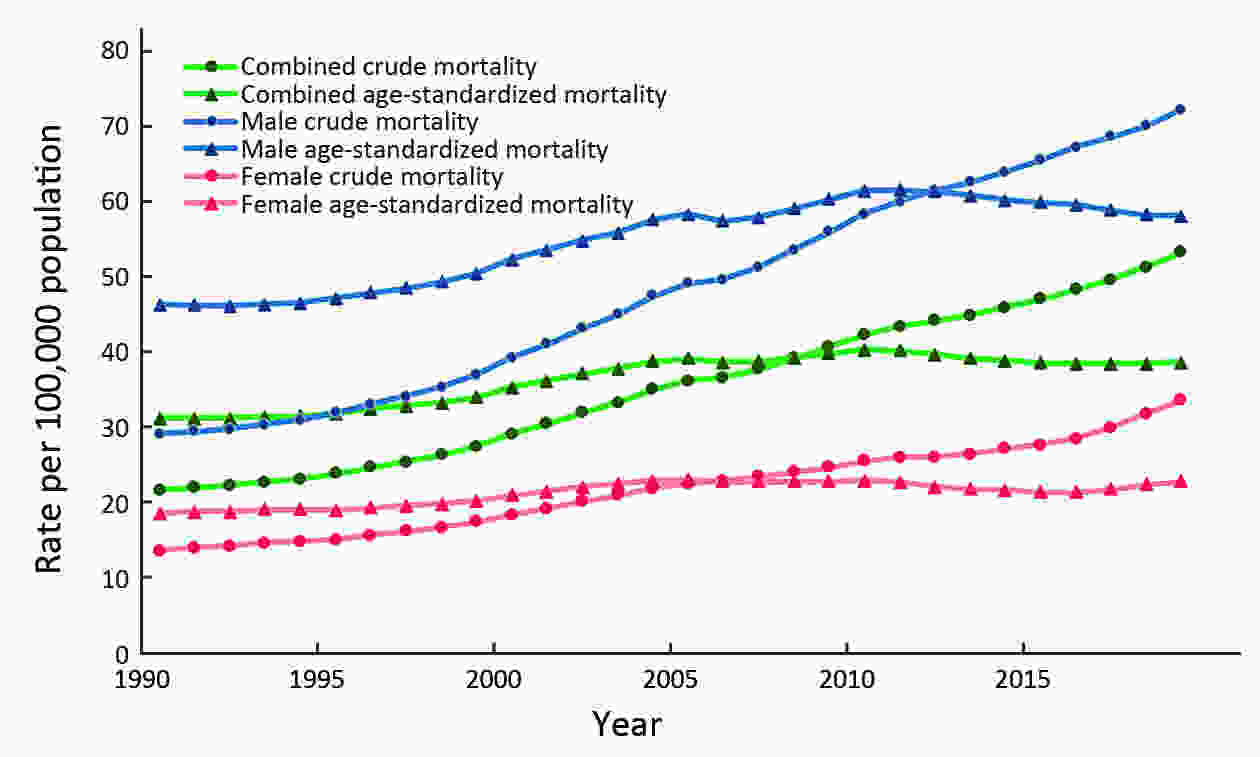
China is faced with heavy burdens caused by lung cancer, which has climbed to the top of both cancer incidence and mortality spectrums. The age-standardized rates of incidence and mortality have shown a trend of gradual up-trends in the last decades, while the crude rates rise much quickly due to the aging of population. Although the improvement in health care has contributed to better survival of lung cancer, its prognosis is still challenging. Apart from the common risk factors such as tobacco use, air pollution, and occupational hazards, some specific factors like Chinese-style cooking also have posed great threats to human health. In light of such national conditions, specific interventions should be conducted to curb the burden of lung cancer including smoking cessation, improvement of air quality, early detection and effective treatment of lung cancer.
China is faced with heavy burdens caused by lung cancer, which has climbed to the top of both cancer incidence and mortality spectrums. The age-standardized rates of incidence and mortality have shown a trend of gradual up-trends in the last decades, while the crude rates rise much quickly due to the aging of population. Although the improvement in health care has contributed to better survival of lung cancer, its prognosis is still challenging. Apart from the common risk factors such as tobacco use, air pollution, and occupational hazards, some specific factors like Chinese-style cooking also have posed great threats to human health. In light of such national conditions, specific interventions should be conducted to curb the burden of lung cancer including smoking cessation, improvement of air quality, early detection and effective treatment of lung cancer.
2020, 32(6): 695-704.
doi: 10.21147/j.issn.1000-9604.2020.06.03
Abstract:
Gastric cancer (GC) is a global health problem, with more than 1 million people newly diagnosed with GC worldwide each year. GC is more prevalent in less developed countries than in more developed countries. About half of all GC cases worldwide occur in East Asia, notably China. Globally, overall incidence rates of GC are declining, which is potentially attributed to a decrease in Helicobacter pylori (H. pylori) infection and the use of refrigeration to preserve foods rather than salt. GC is a multifactorial disease, and its occurrence and development were impacted by environmental and genetic factors. H. pylori infection is the primary risk factor for GC, especially for non-cardia. The prognosis of GC is poor due to stages at the first diagnosis. The 5-year survival rate is less than 10% when patients are diagnosed at an advanced stage, but the rate is as high as 85% if patients are detected at an earlier stage. Endoscopic screening can potentially prevent GC by early diagnosis and early treatment and has been widely adopted in screening programs in East Asian countries, such as Japan and Korea. This review summarizes updated epidemiological aspects, risk factors, and prevention strategies of GC in recent years to help researchers determine the most effective intervention strategies for reducing risk of GC.
Gastric cancer (GC) is a global health problem, with more than 1 million people newly diagnosed with GC worldwide each year. GC is more prevalent in less developed countries than in more developed countries. About half of all GC cases worldwide occur in East Asia, notably China. Globally, overall incidence rates of GC are declining, which is potentially attributed to a decrease in Helicobacter pylori (H. pylori) infection and the use of refrigeration to preserve foods rather than salt. GC is a multifactorial disease, and its occurrence and development were impacted by environmental and genetic factors. H. pylori infection is the primary risk factor for GC, especially for non-cardia. The prognosis of GC is poor due to stages at the first diagnosis. The 5-year survival rate is less than 10% when patients are diagnosed at an advanced stage, but the rate is as high as 85% if patients are detected at an earlier stage. Endoscopic screening can potentially prevent GC by early diagnosis and early treatment and has been widely adopted in screening programs in East Asian countries, such as Japan and Korea. This review summarizes updated epidemiological aspects, risk factors, and prevention strategies of GC in recent years to help researchers determine the most effective intervention strategies for reducing risk of GC.
2020, 32(6): 705-719.
doi: 10.21147/j.issn.1000-9604.2020.06.04
Abstract:
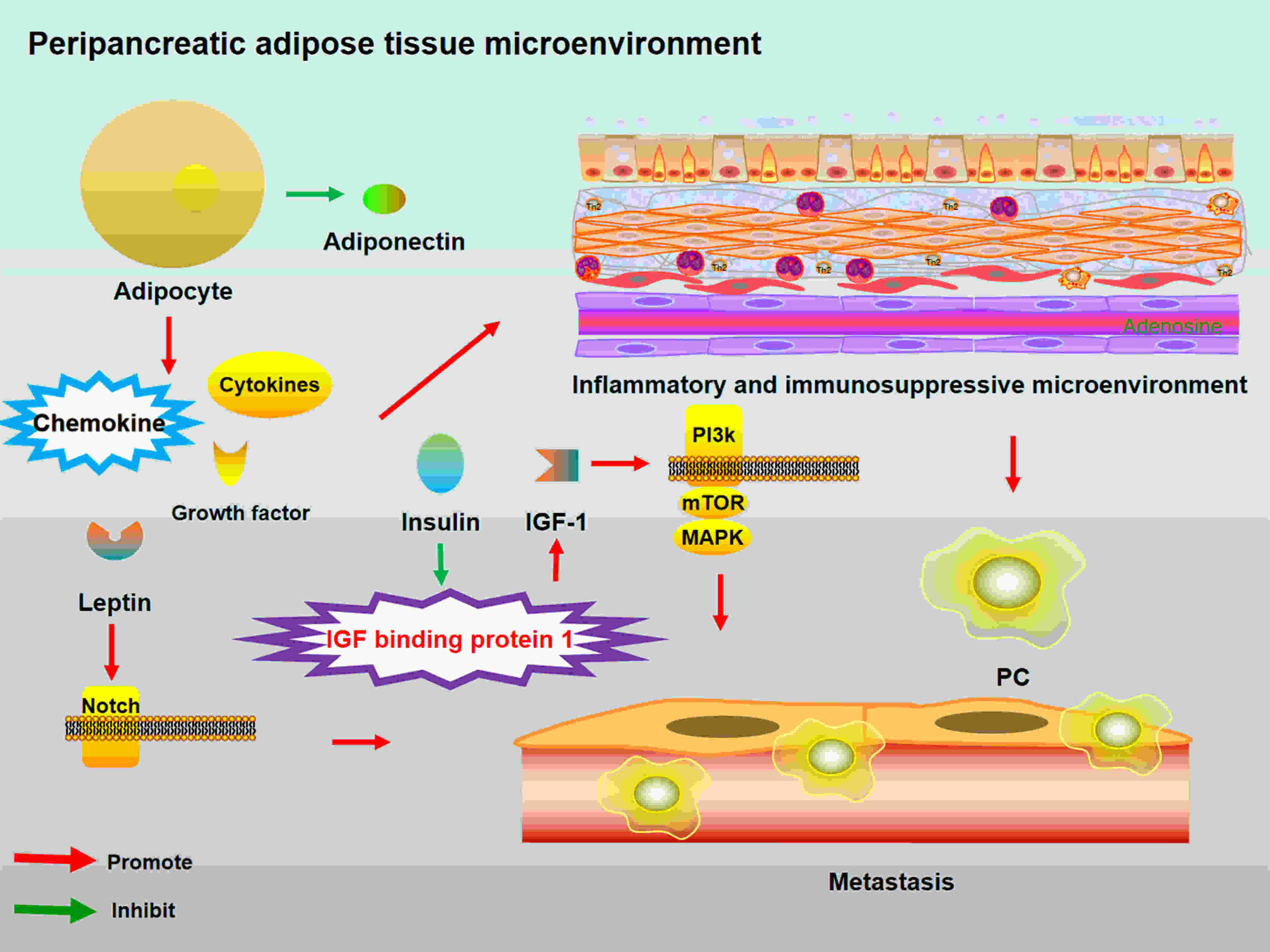
Pancreatic cancer (PC) is an increasingly common disease worldwide. Having a better understanding of worldwide and regional epidemiologic features and risk factors of PC is essential to identify new approaches for prevention, early diagnosis, surveillance, and treatment. In this article, we review the epidemiologic features and risk factors for PC and discuss opportunities and challenges of PC future treatment.
Pancreatic cancer (PC) is an increasingly common disease worldwide. Having a better understanding of worldwide and regional epidemiologic features and risk factors of PC is essential to identify new approaches for prevention, early diagnosis, surveillance, and treatment. In this article, we review the epidemiologic features and risk factors for PC and discuss opportunities and challenges of PC future treatment.
2020, 32(6): 720-728.
doi: 10.21147/j.issn.1000-9604.2020.06.05
Abstract:
Cervical cancer is one of the leading causes of cancer death among females worldwide and its behavior epidemiologically likes a venereal disease of low infectiousness. Early age at first intercourse and multiple sexual partners have been shown to exert strong effects on risk. The wide differences in the incidence among different countries also influenced by the introduction of screening. Although the general picture remains one of decreasing incidence and mortality, there are signs of an increasing cervical cancer risk probably due to changes in sexual behavior. Smoking and human papillomavirus (HPV) 16/18 are currently important issues in a concept of multifactorial, stepwise carcinogenesis at the cervix uteri. Therefore, society-based preventive and control measures, screening activities and HPV vaccination are recommended. Cervical cancer screening methods have evolved from cell morphology observation to molecular testing. High-risk HPV genotyping and liquid-based cytology are common methods which have been widely recommended and used worldwide. In future, accurate, cheap, fast and easy-to-use methods would be more popular. Artificial intelligence also shows to be promising in cervical cancer screening by integrating image recognition with big data technology. Meanwhile, China has achieved numerous breakthroughs in cervical cancer prevention and control which could be a great demonstration for other developing and resource-limited areas. In conclusion, although cervical cancer threatens female health, it could be the first cancer that would be eliminated by human beings with comprehensive preventive and control strategy.
Cervical cancer is one of the leading causes of cancer death among females worldwide and its behavior epidemiologically likes a venereal disease of low infectiousness. Early age at first intercourse and multiple sexual partners have been shown to exert strong effects on risk. The wide differences in the incidence among different countries also influenced by the introduction of screening. Although the general picture remains one of decreasing incidence and mortality, there are signs of an increasing cervical cancer risk probably due to changes in sexual behavior. Smoking and human papillomavirus (HPV) 16/18 are currently important issues in a concept of multifactorial, stepwise carcinogenesis at the cervix uteri. Therefore, society-based preventive and control measures, screening activities and HPV vaccination are recommended. Cervical cancer screening methods have evolved from cell morphology observation to molecular testing. High-risk HPV genotyping and liquid-based cytology are common methods which have been widely recommended and used worldwide. In future, accurate, cheap, fast and easy-to-use methods would be more popular. Artificial intelligence also shows to be promising in cervical cancer screening by integrating image recognition with big data technology. Meanwhile, China has achieved numerous breakthroughs in cervical cancer prevention and control which could be a great demonstration for other developing and resource-limited areas. In conclusion, although cervical cancer threatens female health, it could be the first cancer that would be eliminated by human beings with comprehensive preventive and control strategy.
2020, 32(6): 729-741.
doi: 10.21147/j.issn.1000-9604.2020.06.06
Abstract:
In China, colorectal cancer (CRC) ranked fourth and fifth in the highest incidence and mortality rates of all malignancies in 2018, respectively. Although these rates are below the world average, China placed first worldwide in the number of new CRC cases and CRC-related deaths because of its comparatively large population. This disease represents a threat to the health of population and incurs a heavy economic burden on the society and individuals. CRC has various risk factors, including age, sex, lifestyle, genetic factors, obesity, diabetes, gut microbiota status, and precancerous lesions. Furthermore, incidence and mortality rates of CRC are closely related to socioeconomic development levels, varying according to regional and population characteristics. Prevention is the main strategy to reduce incidence and mortality rates of CRC. This can be achieved through strategies stimulating lifestyle changes, healthy diet habits, and early screening for high-risk individuals. To reduce the burden of CRC, public health officials should promote prevention and management of modifiable risk factors through national policies. The rising incidence and mortality rates of CRC in China may be timely curbed by clarifying specific epidemiological characteristics, optimizing early screening strategies, and strictly implementing diagnosis and treatment guidelines. Thus, this study aimed to collect and report the current research status on epidemiology and risk factors of CRC in China.
In China, colorectal cancer (CRC) ranked fourth and fifth in the highest incidence and mortality rates of all malignancies in 2018, respectively. Although these rates are below the world average, China placed first worldwide in the number of new CRC cases and CRC-related deaths because of its comparatively large population. This disease represents a threat to the health of population and incurs a heavy economic burden on the society and individuals. CRC has various risk factors, including age, sex, lifestyle, genetic factors, obesity, diabetes, gut microbiota status, and precancerous lesions. Furthermore, incidence and mortality rates of CRC are closely related to socioeconomic development levels, varying according to regional and population characteristics. Prevention is the main strategy to reduce incidence and mortality rates of CRC. This can be achieved through strategies stimulating lifestyle changes, healthy diet habits, and early screening for high-risk individuals. To reduce the burden of CRC, public health officials should promote prevention and management of modifiable risk factors through national policies. The rising incidence and mortality rates of CRC in China may be timely curbed by clarifying specific epidemiological characteristics, optimizing early screening strategies, and strictly implementing diagnosis and treatment guidelines. Thus, this study aimed to collect and report the current research status on epidemiology and risk factors of CRC in China.
2020, 32(6): 742-754.
doi: 10.21147/j.issn.1000-9604.2020.06.07
Abstract:
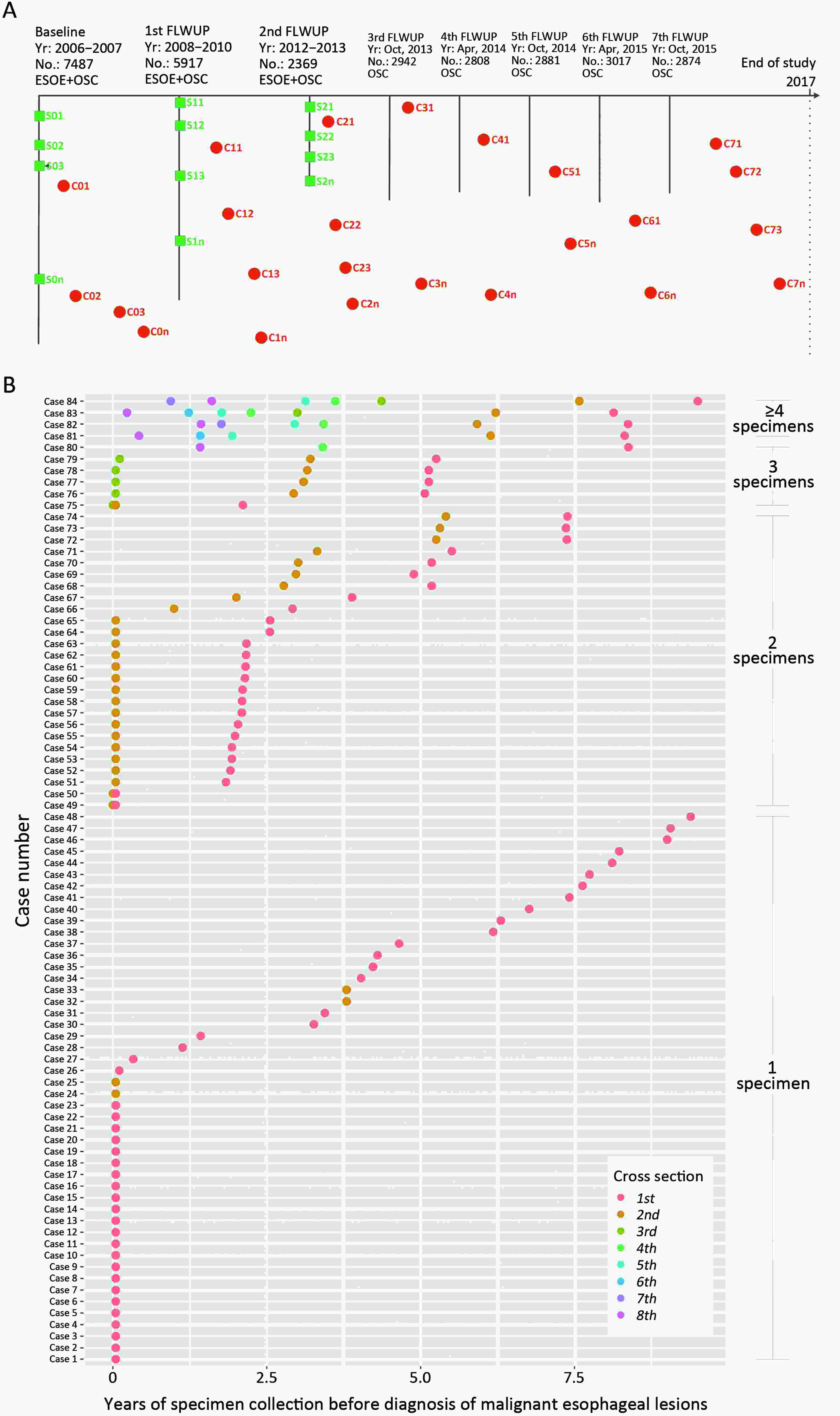
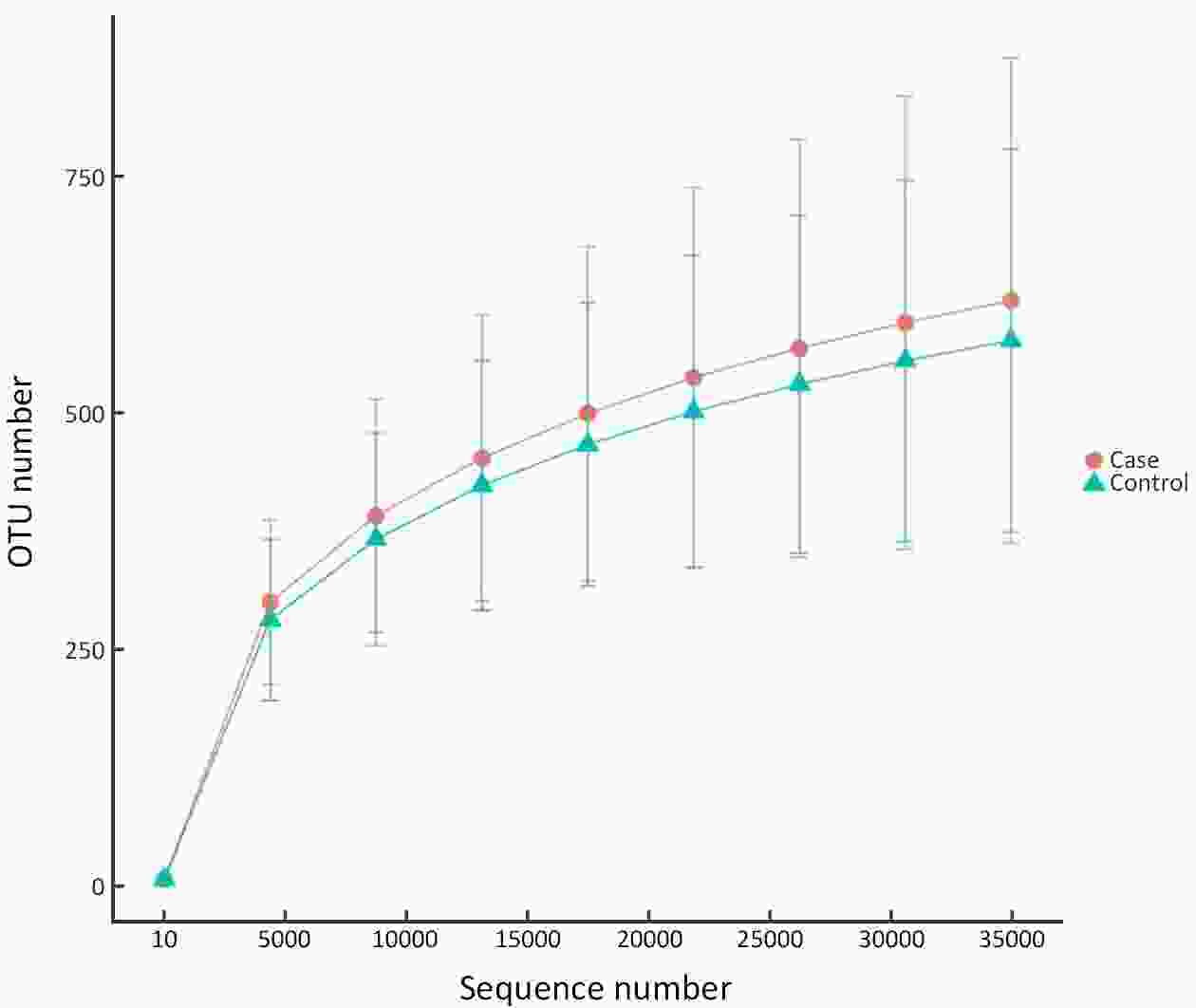
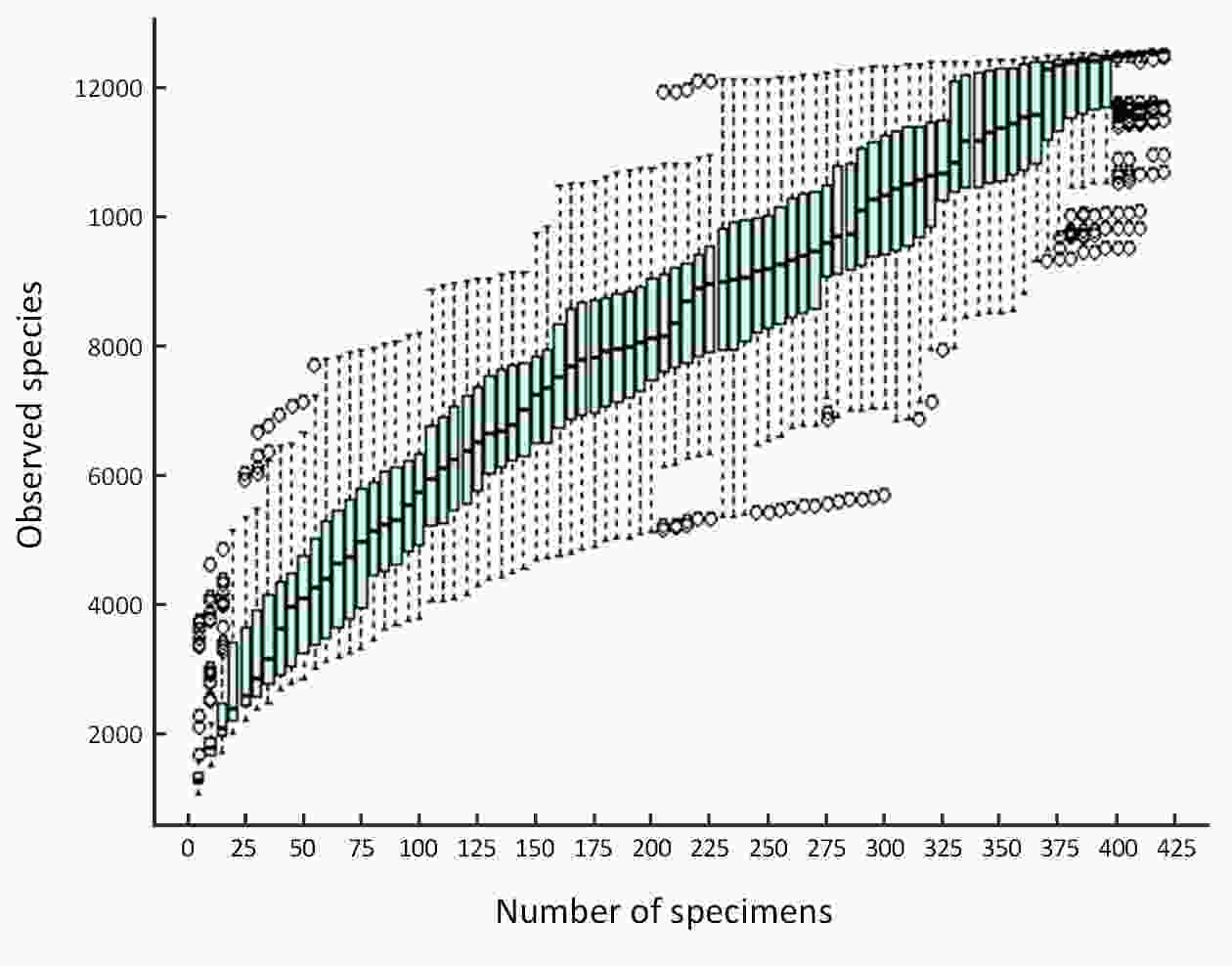
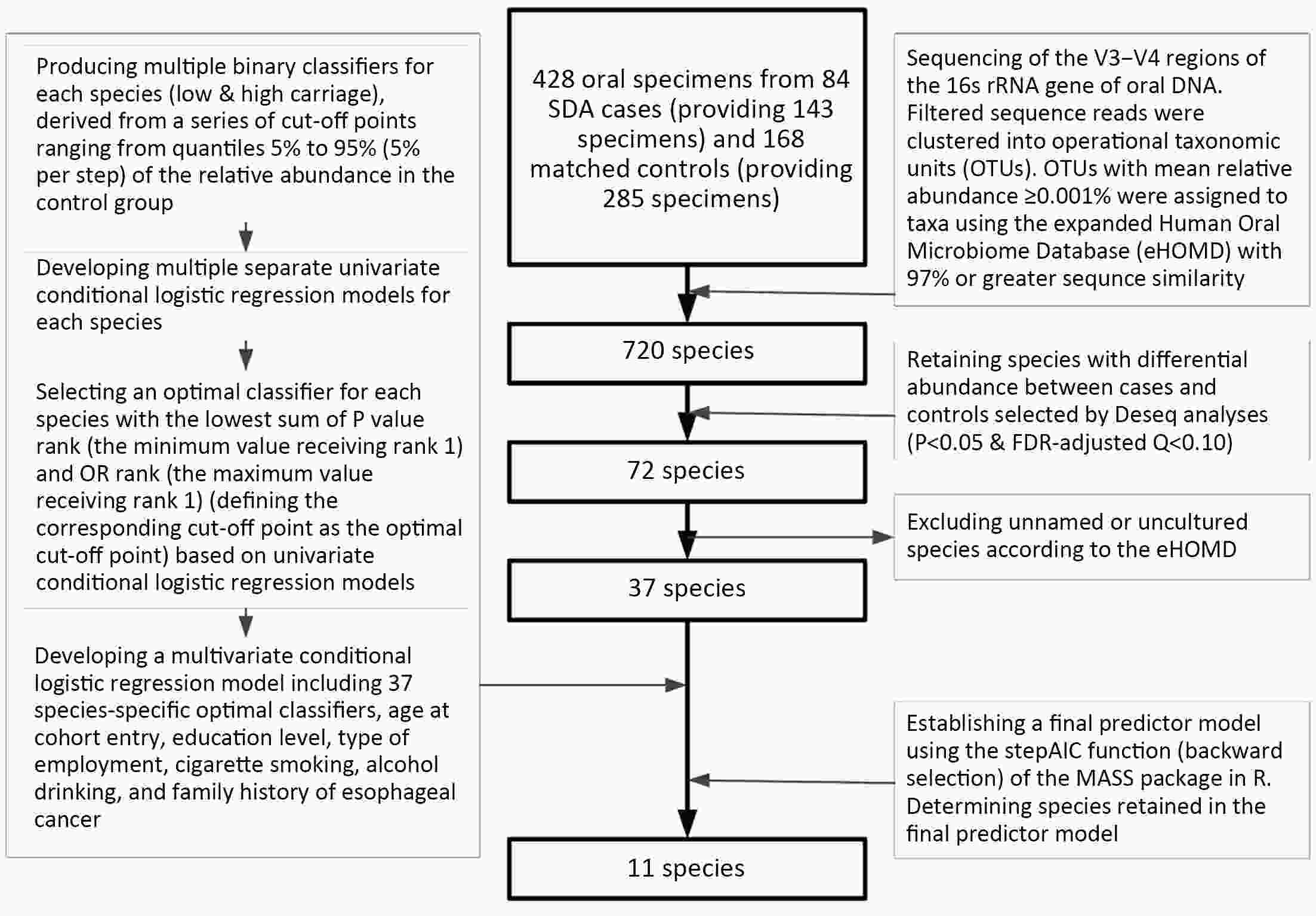
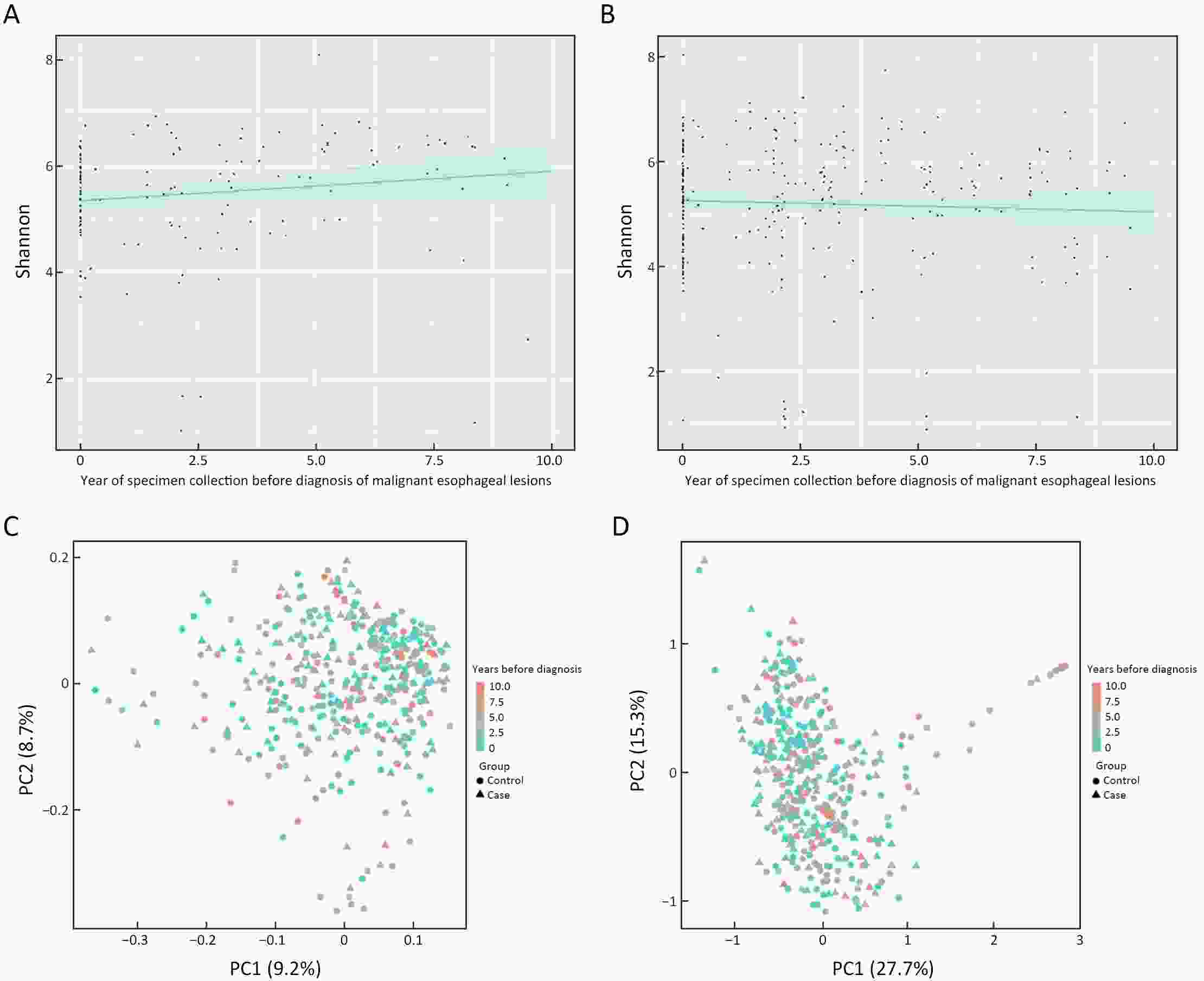
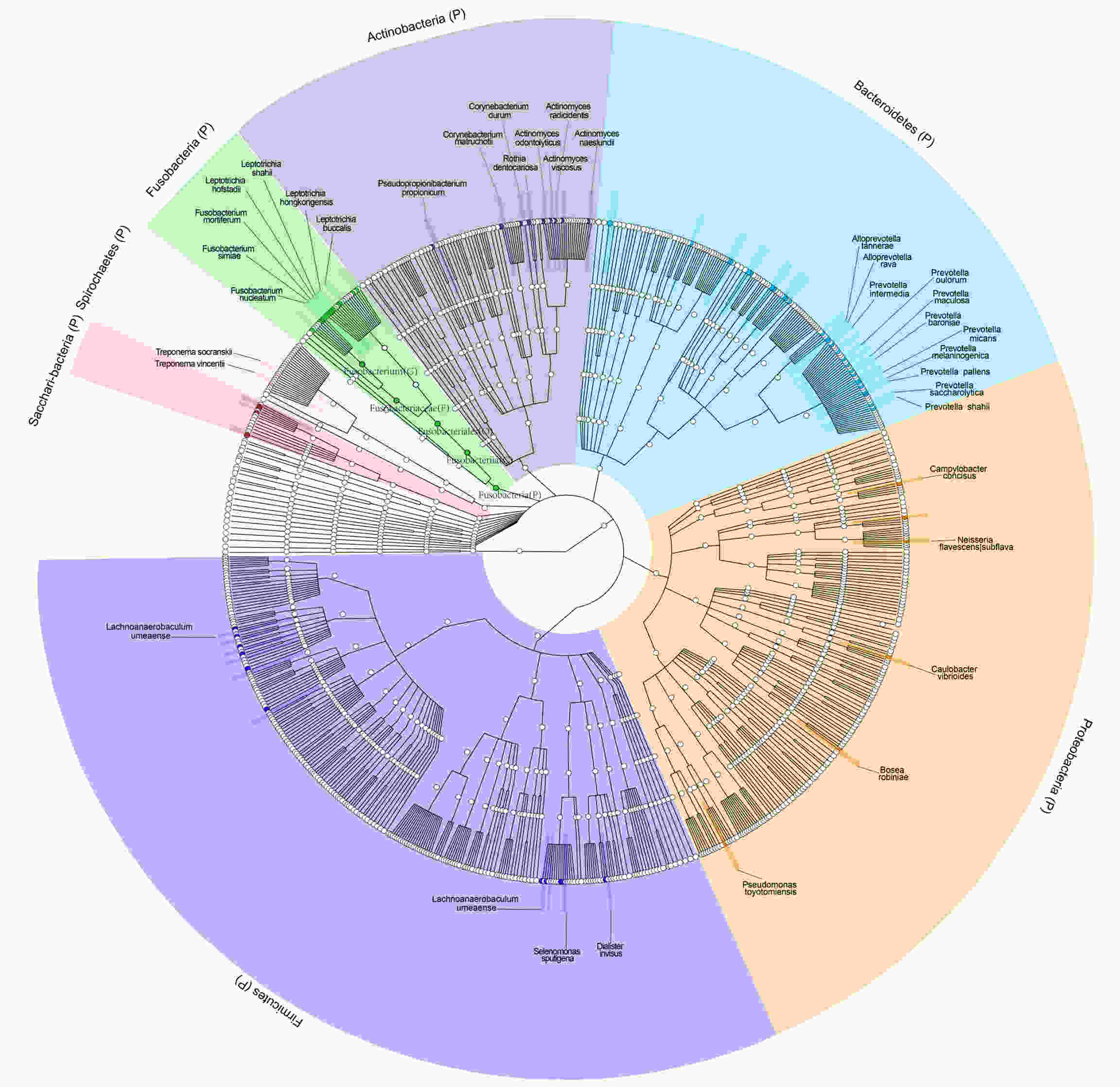
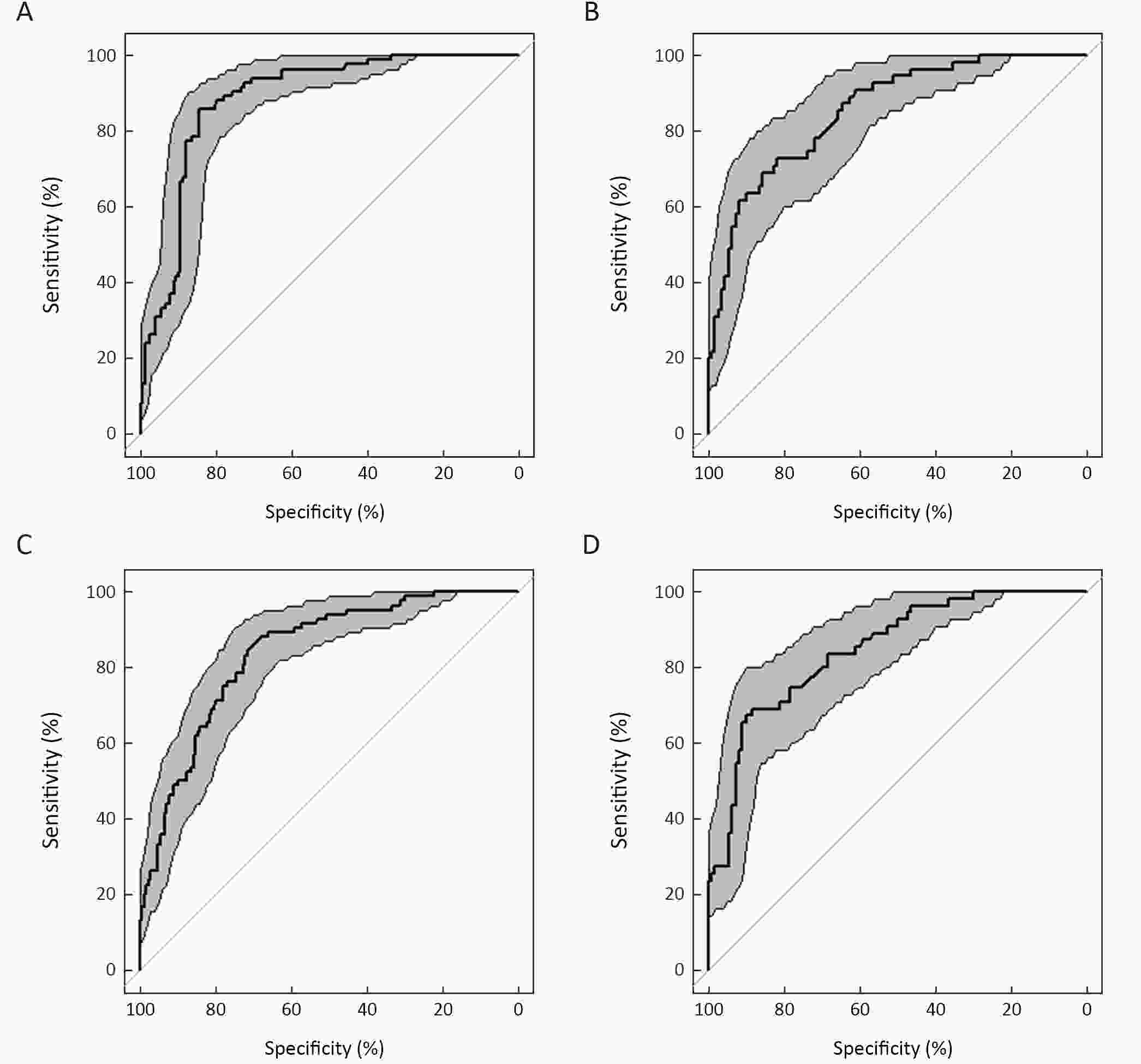
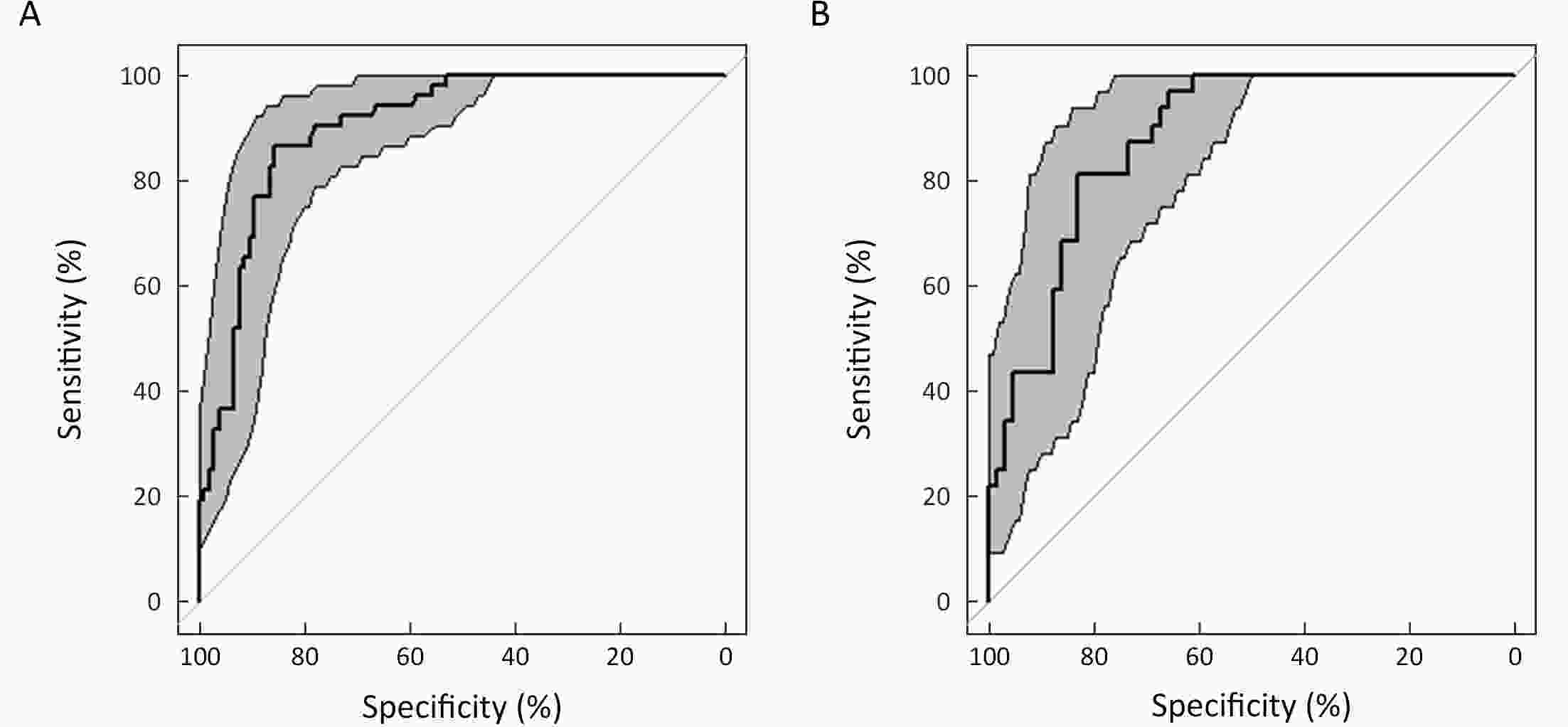
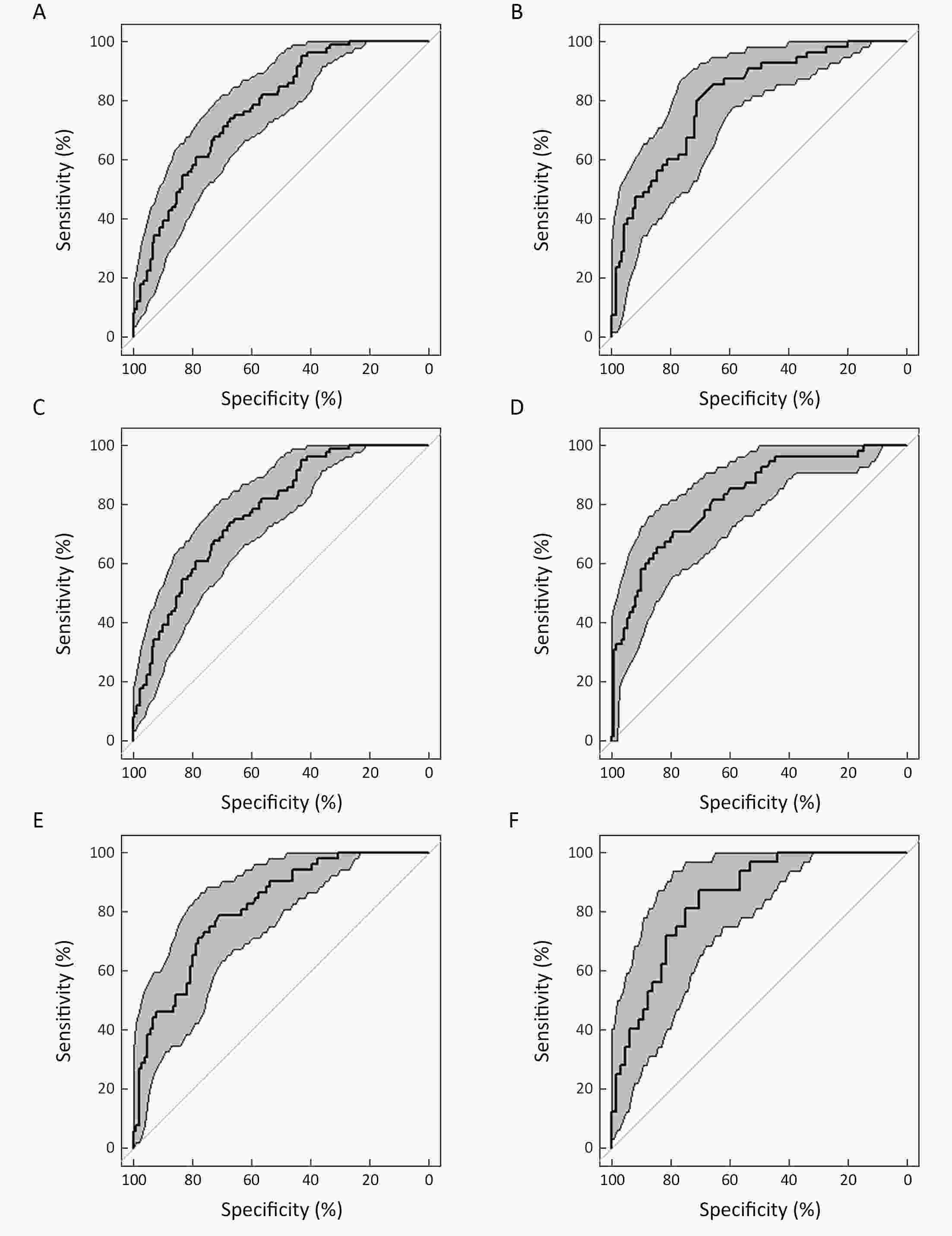
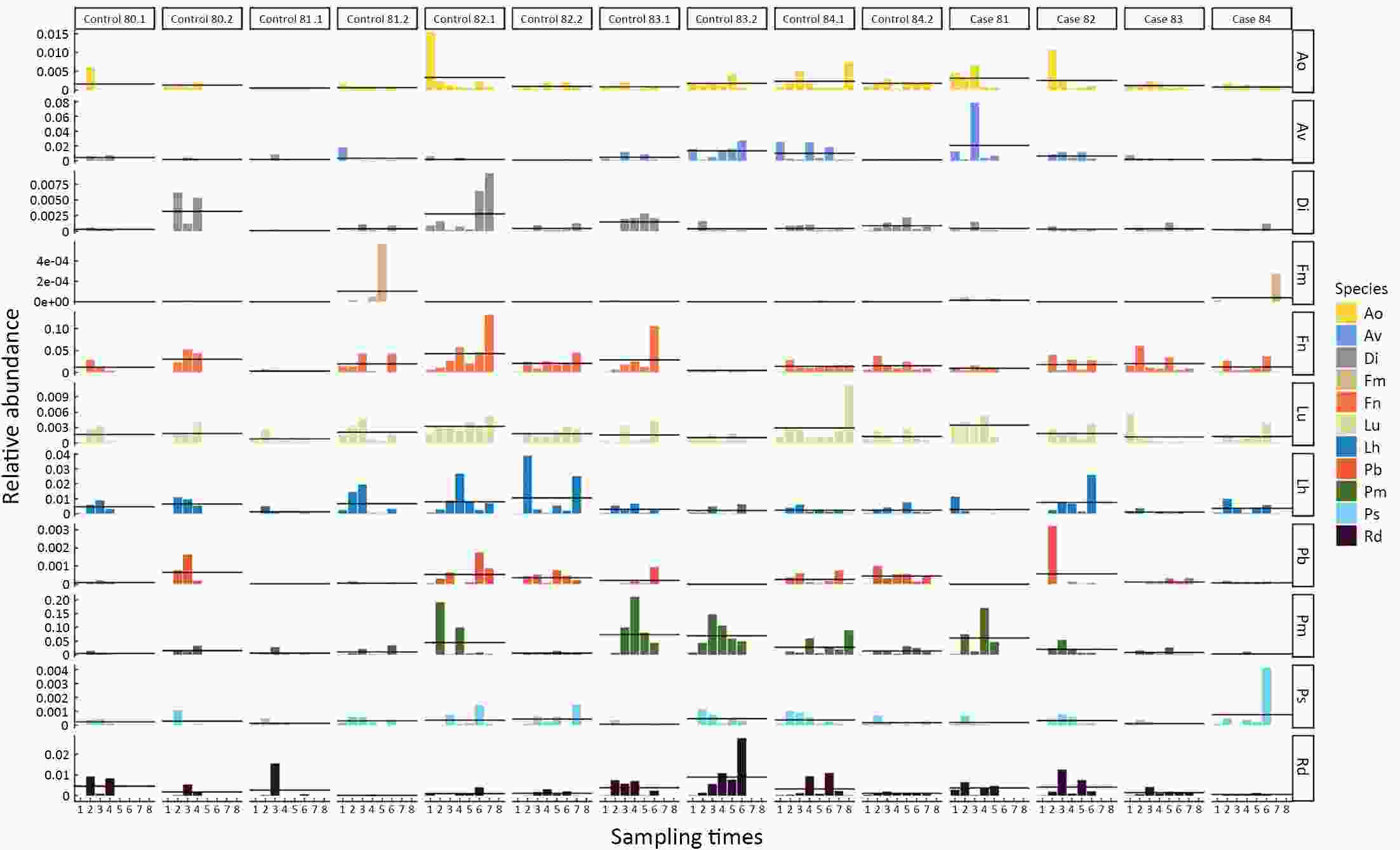
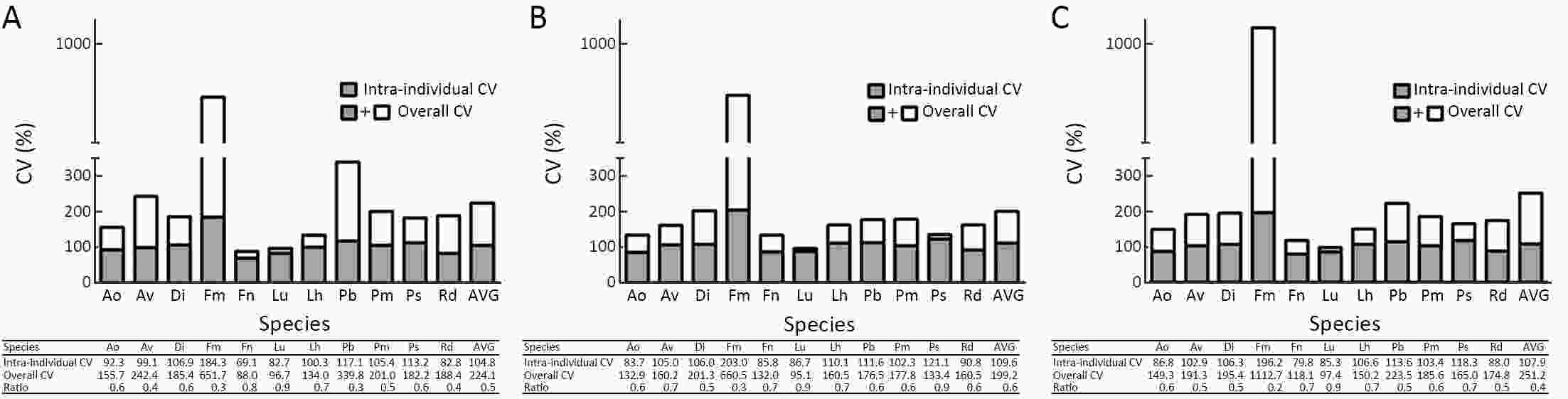
ObjectiveWe aimed to prospectively evaluate the association of oral microbiome with malignant esophageal lesions and its predictive potential as a biomarker of risk. MethodsWe conducted a case-control study nested within a population-based cohort with up to 8 visits of oral swab collection for each subject over an 11-year period in a high-risk area for esophageal cancer in China. The oral microbiome was evaluated with 16S ribosomal RNA (rRNA) gene sequencing in 428 pre-diagnostic oral specimens from 84 cases with esophageal lesions of severe squamous dysplasia and above (SDA) and 168 matched healthy controls. DESeq analysis was performed to identify taxa of differential abundance. Differential oral species together with subject characteristics were evaluated for their potential in predicting SDA risk by constructing conditional logistic regression models. ResultsA total of 125 taxa including 37 named species showed significantly different abundance between SDA cases and controls (all P<0.05 & false discovery rate-adjusted Q<0.10). A multivariate logistic model including 11 SDA lesion-related species and family history of esophageal cancer provided an area under the receiver operating characteristic curve (AUC) of 0.89 (95% CI, 0.84−0.93). Cross-validation and sensitivity analysis, excluding cases diagnosed within 1 year of collection of the baseline specimen and their matched controls, or restriction to screen-endoscopic-detected or clinically diagnosed case-control triads, or using only bacterial data measured at the baseline, yielded AUCs>0.84. ConclusionsThe oral microbiome may play an etiological and predictive role in esophageal cancer, and it holds promise as a non-invasive early warning biomarker for risk stratification for esophageal cancer screening programs.
2020, 32(6): 755-767.
doi: 10.21147/j.issn.1000-9604.2020.06.09
Abstract:
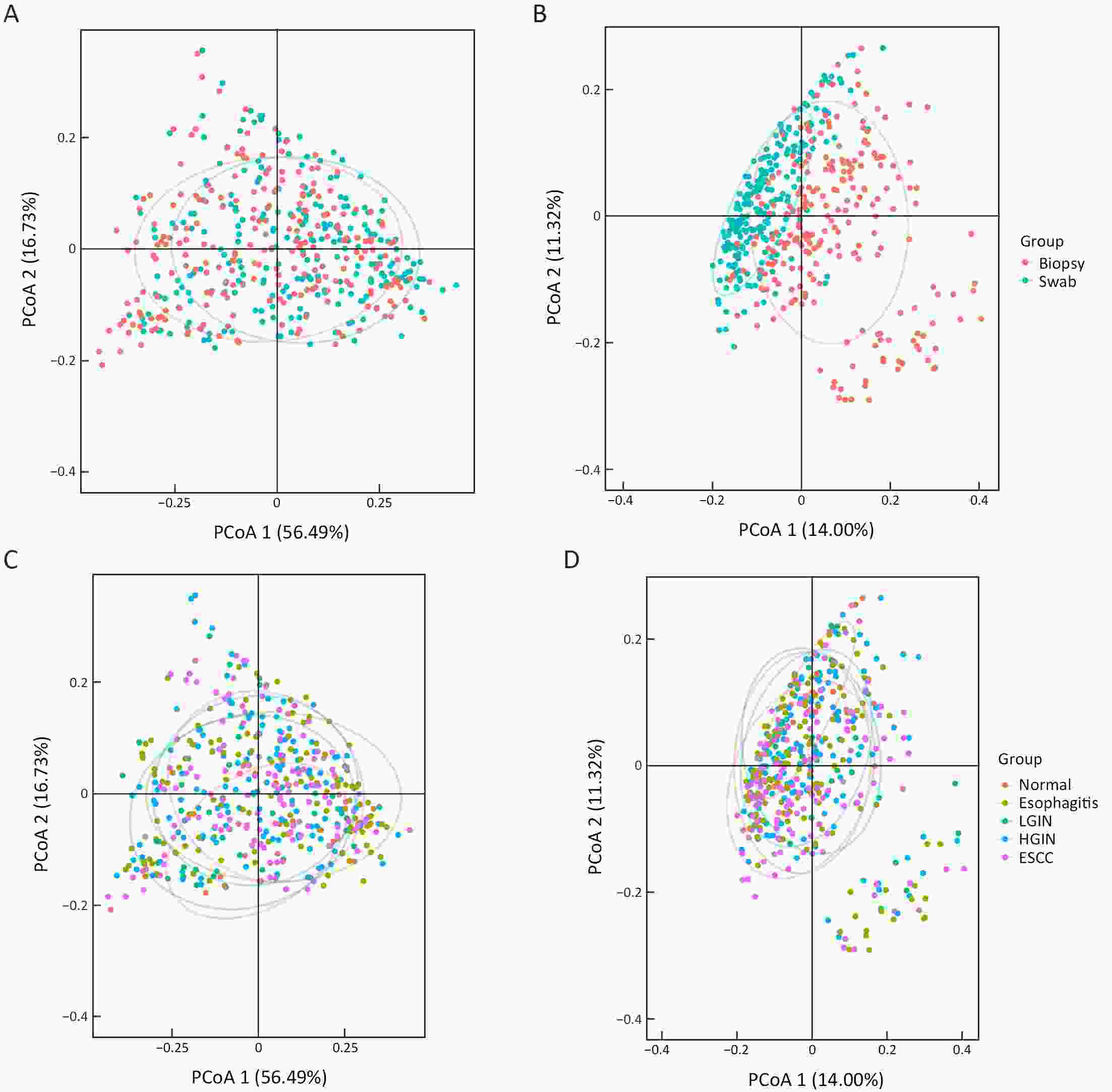
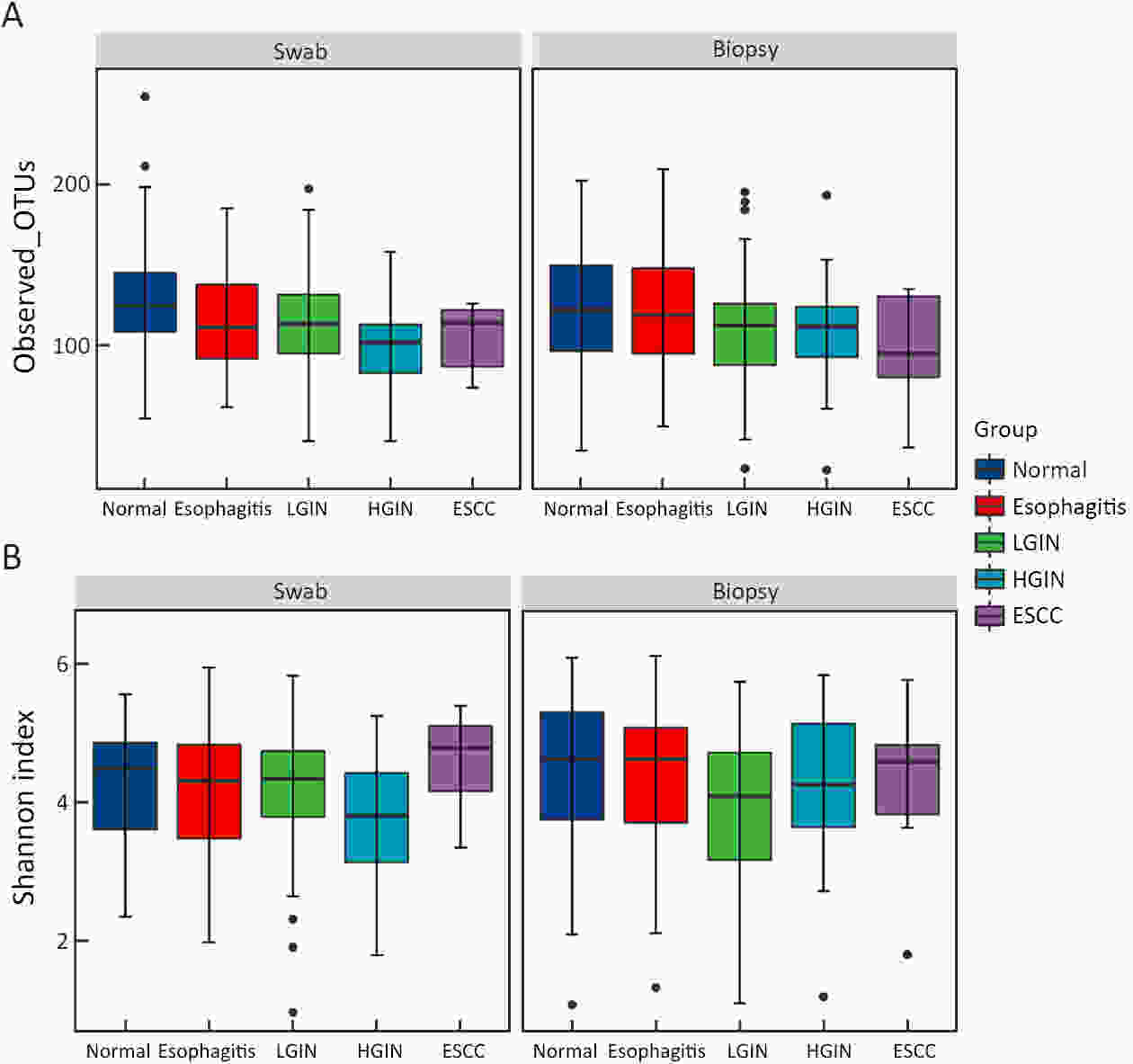
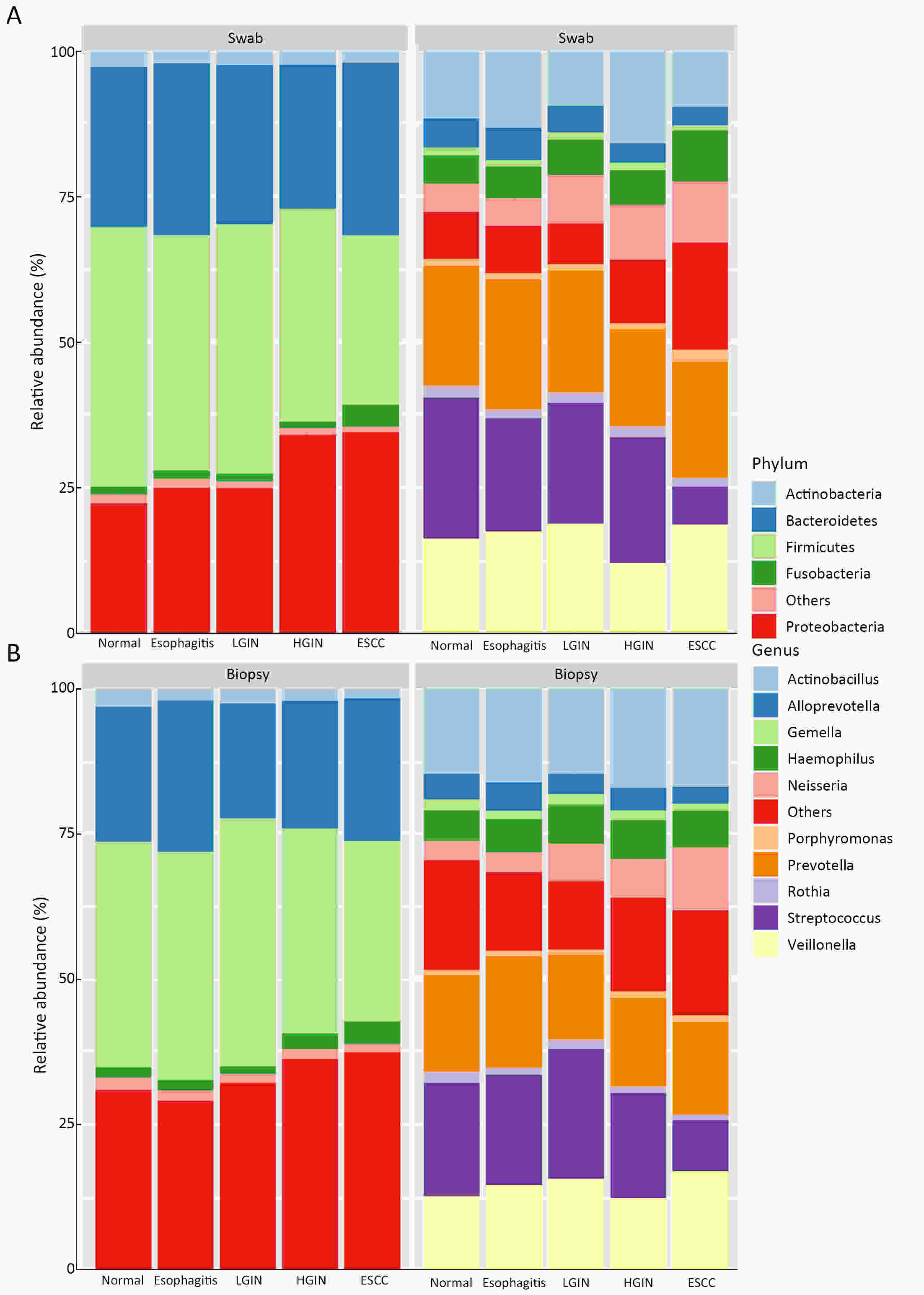
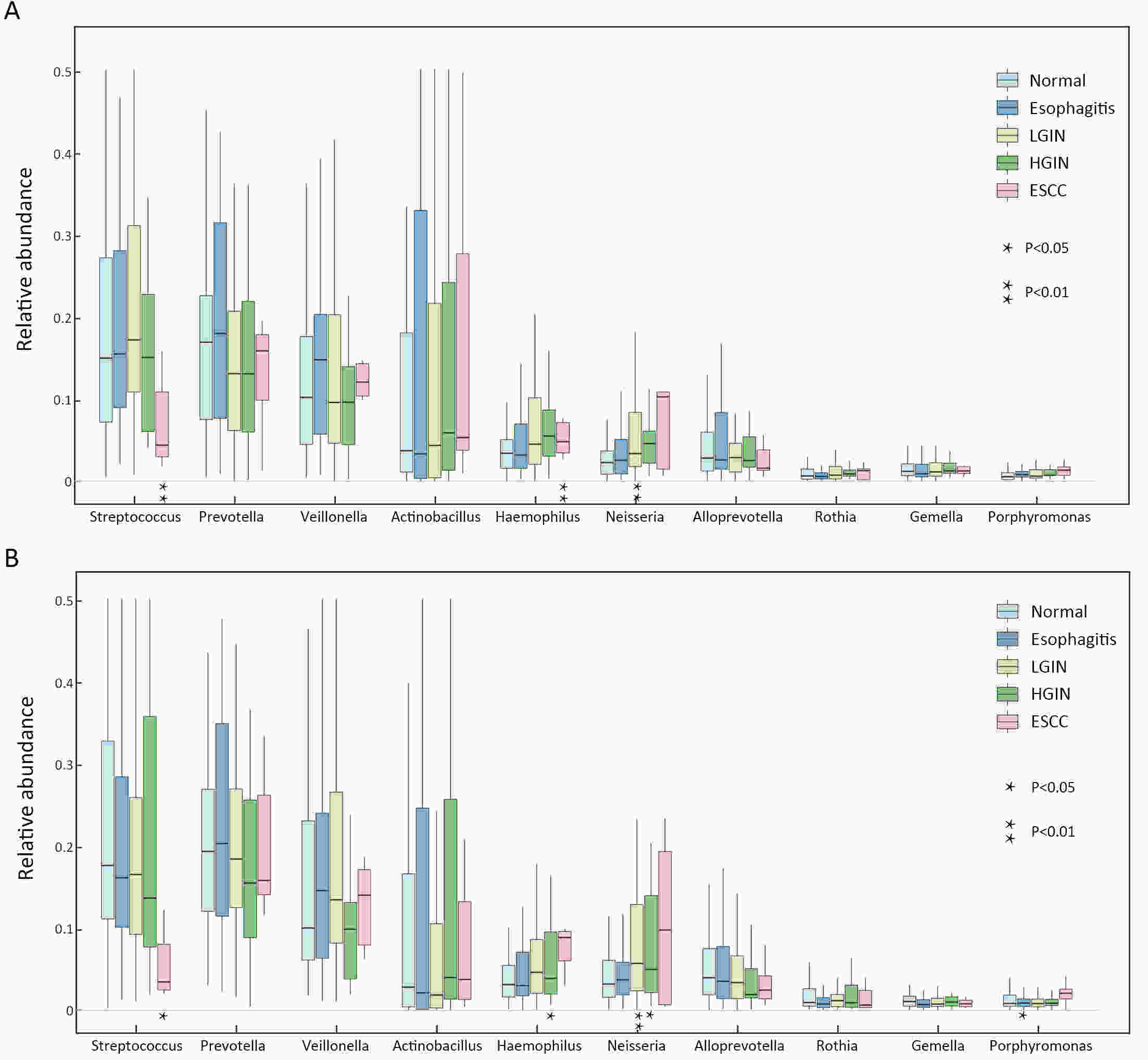
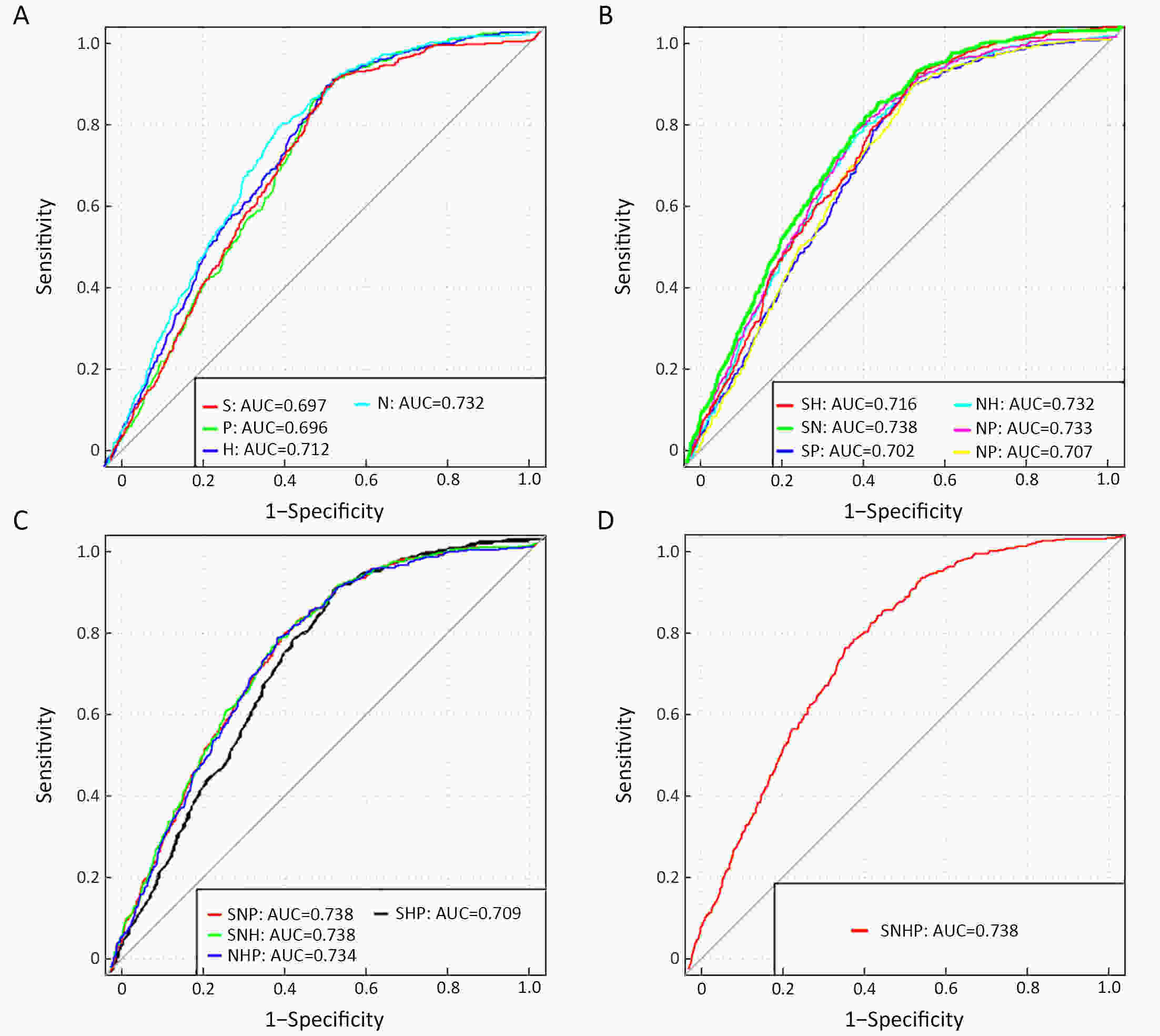
ObjectiveEsophageal squamous cell carcinoma (ESCC) is one of the dominant malignances worldwide, but currently there is less focus on the microbiota with ESCC and its precancerous lesions. MethodsPaired esophageal biopsy and swab specimens were obtained from 236 participants in Linzhou, China. Data from 16S ribosomal RNA gene sequencing were processed using quantitative insights into microbial ecology (QIIME2) and R Studio to evaluate differences. The Wilcoxon rank sum test and Kruskal-Wallis rank sum test were used to compare diversity and characteristic genera by specimens and participant groups. Ordinal logistic regression model was used to build microbiol prediction model. ResultsMicrobial diversity was similar between biopsy and swab specimens, including operational taxonomic unit (OTU) numbers and Shannon index. There were variations and similarities of esophageal microbiota among different pathological characteristics of ESCC. Top 10 relative abundance genera in all groups include Streptococcus, Prevotella, Veillonella, Actinobacillus, Haemophilus, Neisseria, Alloprevotella, Rothia, Gemella and Porphyromonas. Genus Streptococcus, Haemophilus, Neisseria and Porphyromonas showed significantly difference in disease groups when compared to normal control, whereas Streptococcus showed an increasing tendency with the progression of ESCC and others showed a decreasing tendency. About models based on all combinations of characteristic genera, only taken Streptococcus and Neisseria into model, the prediction performance was the ideal one, of which the area under the curve (AUC) was 0.738. ConclusionsEsophageal biopsy and swab specimens could yield similar microbial characterization. The combination of Streptococcus and Neisseria has the potential to predict the progression of ESCC, which is needed to confirm by large-scale, prospective cohort studies.
2020, 32(6): 768-777.
doi: 10.21147/j.issn.1000-9604.2020.06.10
Abstract:
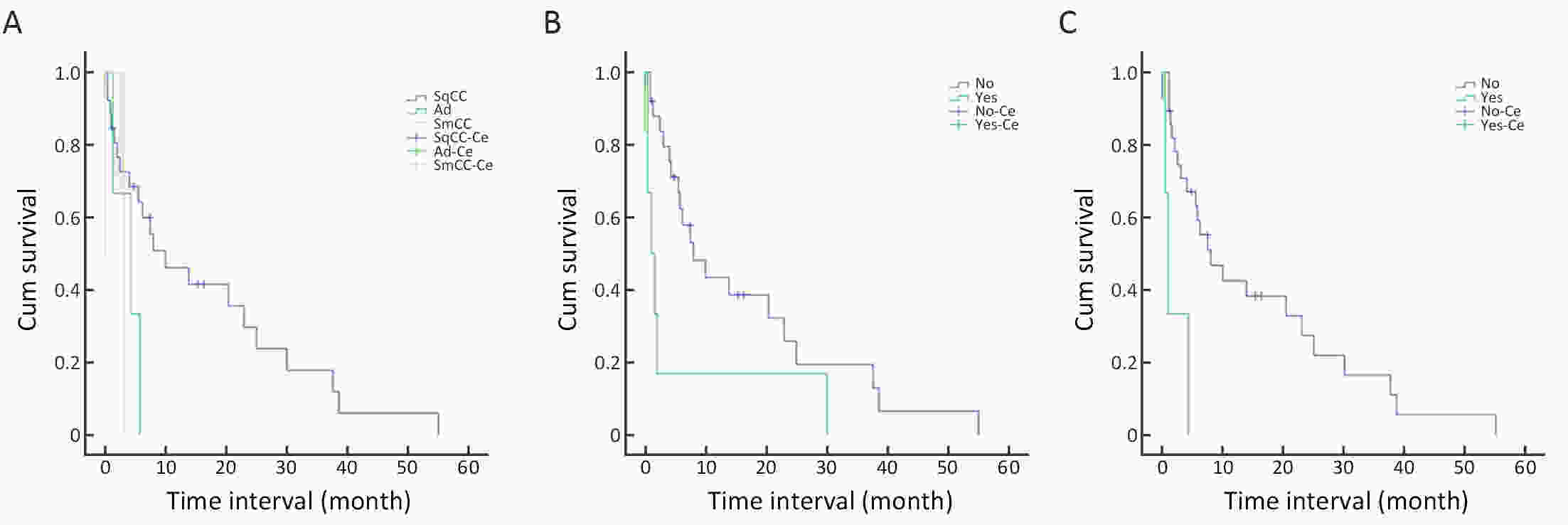
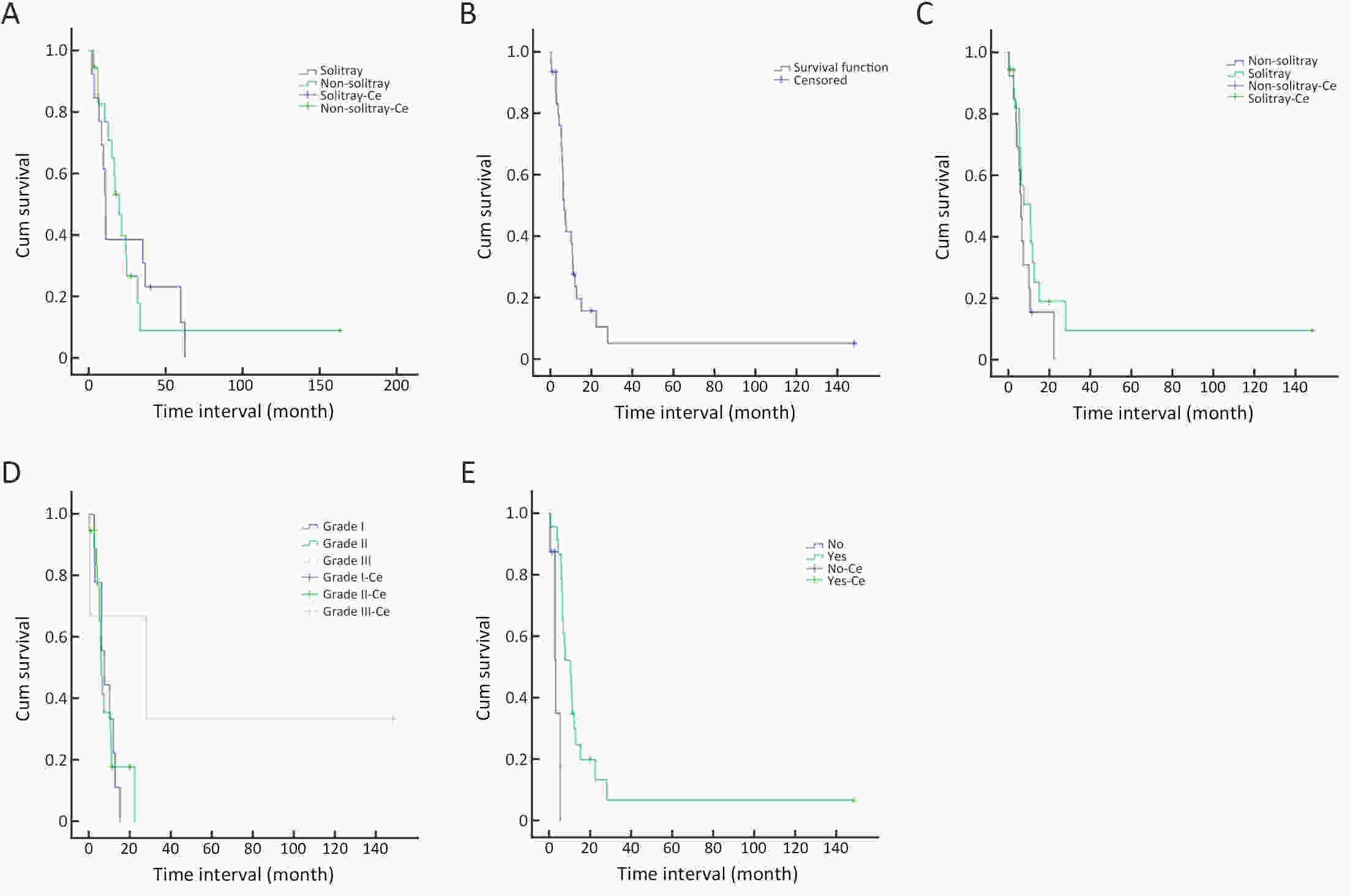
ObjectiveThe incidence of brain metastasis from esophageal cancer (BMEC) has increased in recent years. Thus, it is necessary to identify factors that affect long-term outcomes for such patients. MethodsFrom January 1997 to July 2018, consecutive patients (10,043 patients, 31 with brain metastasis) with esophageal cancer (EC) treated at Zhejiang Cancer Hospital were recruited for retrospective analysis. Demographic, clinical, and pathological variables and the survival data were retrieved. ResultsThe median time from diagnosis of EC to diagnosis of brain metastases was 7.67 (range, 0.43−55.20) months. The median survival time of BMEC patients from diagnosis of primary esophageal tumor was 16.7 (range, 2.33−163.30) months and the median survival time from the point of diagnosis of brain metastasis was 6.47 (range, 0.43−148.13) months. Univariate and multivariate analyses showed that the pathology type, EC without chemotherapy, and bone metastasis history were significantly associated with a shorter time interval between the first treatment of EC and brain metastasis. Chemotherapy history after brain metastasis, whole brain radiation therapy (WBRT) history, and surgery were significant predictors for better long-term survival outcomes. ConclusionsOur findings indicate that the use of surgery, WBRT, and chemotherapy can achieve the best therapeutic effects for BMEC patients.
2020, 32(6): 778-793.
doi: 10.21147/j.issn.1000-9604.2020.06.11
Abstract:
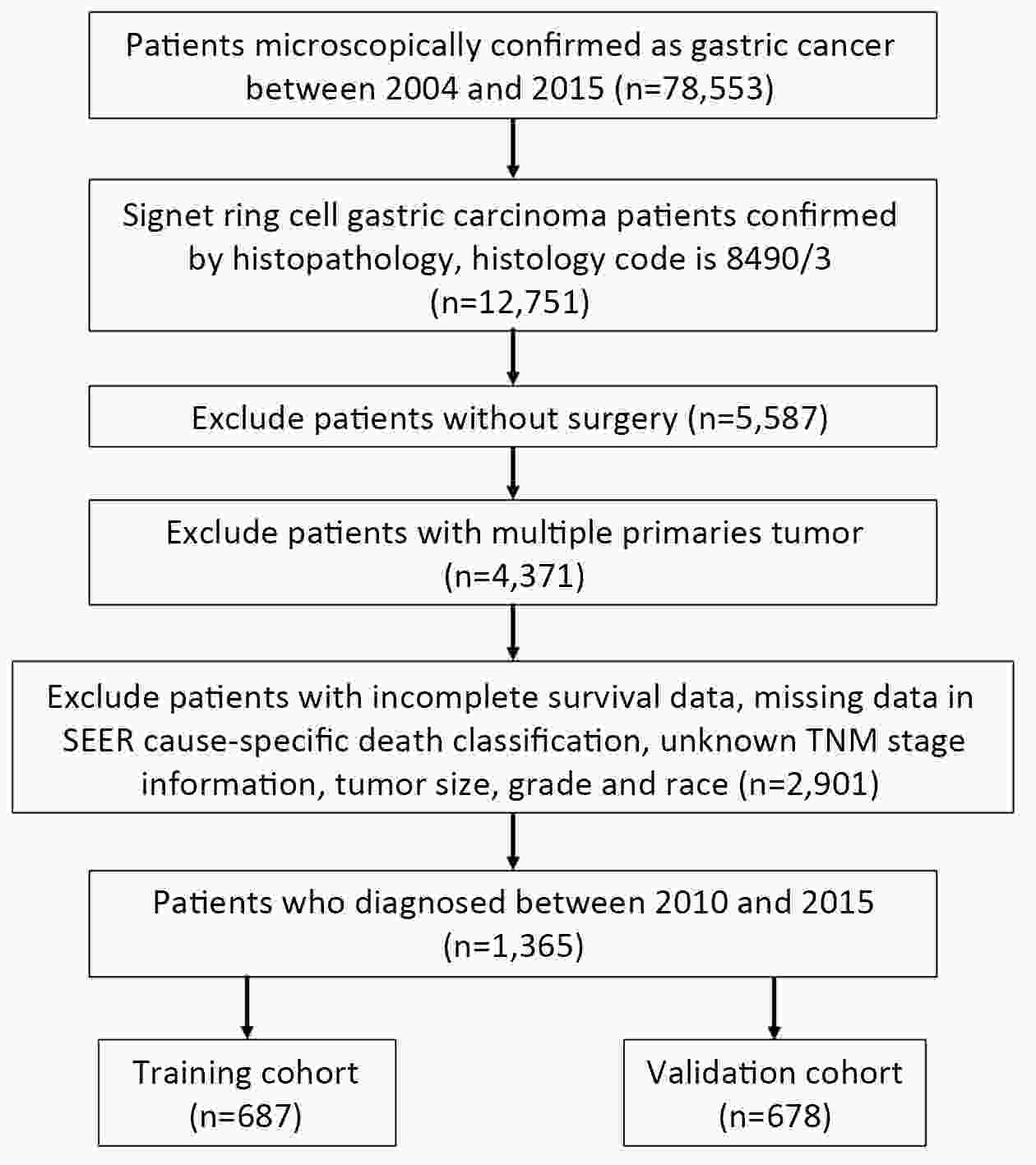
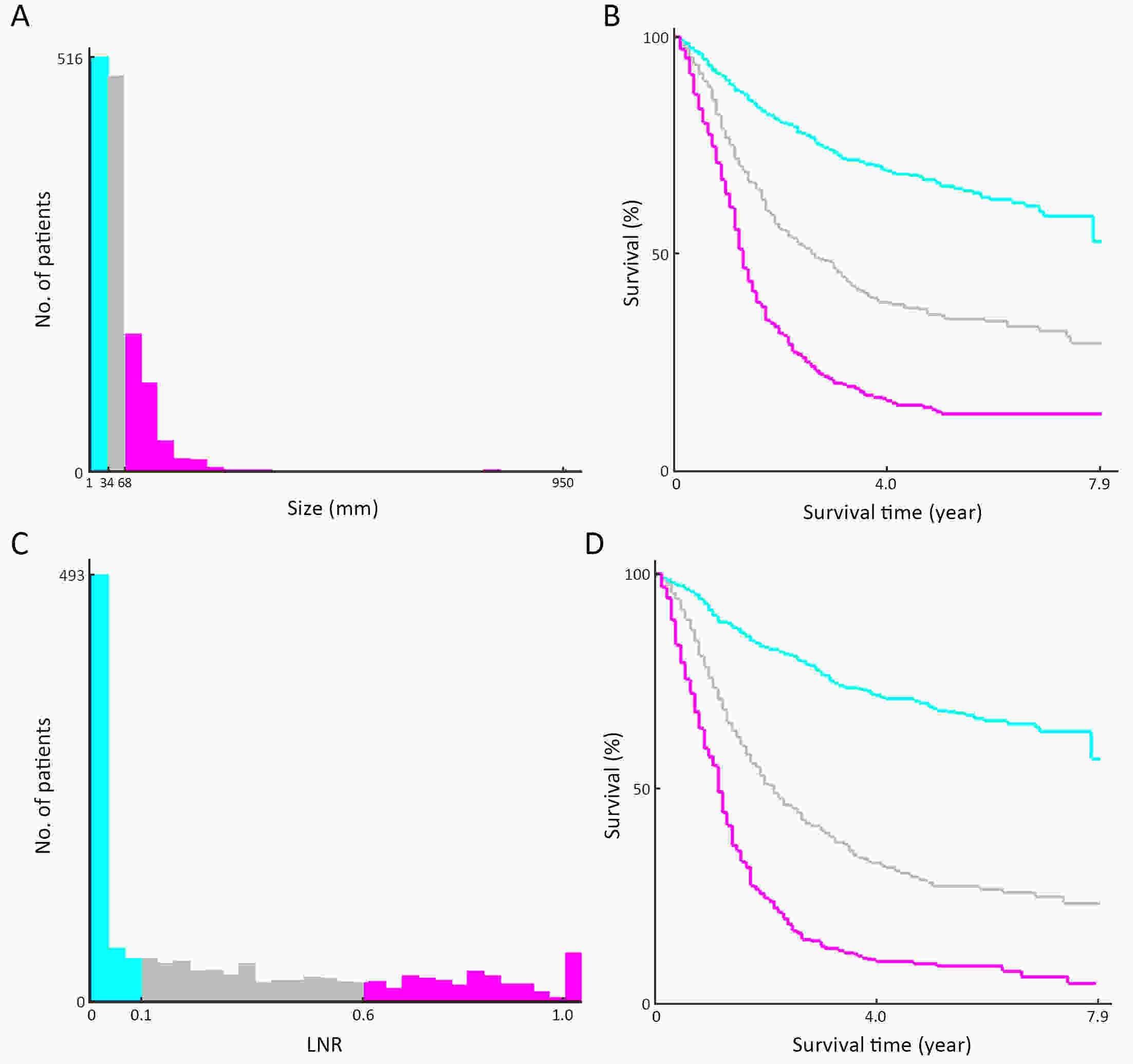
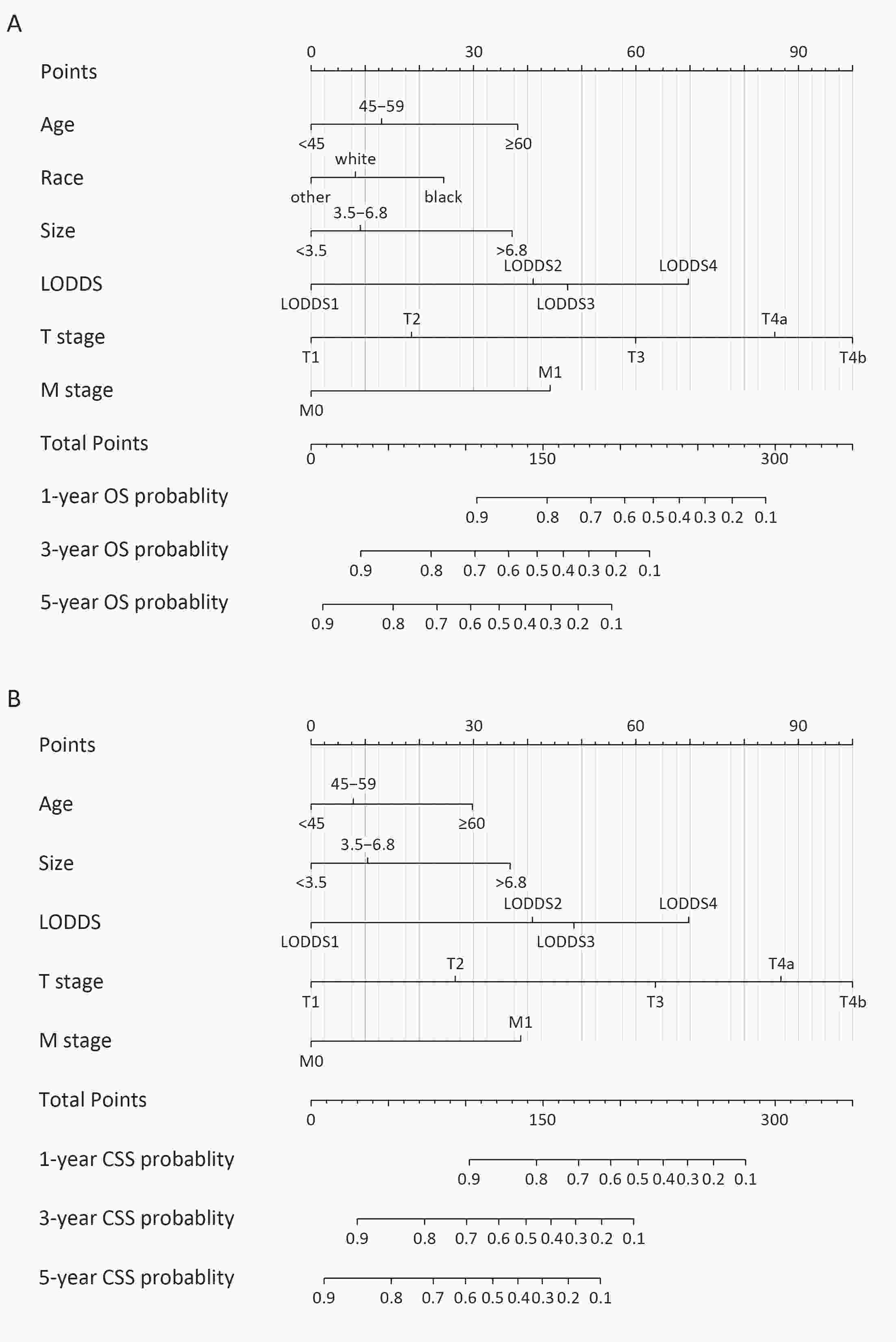
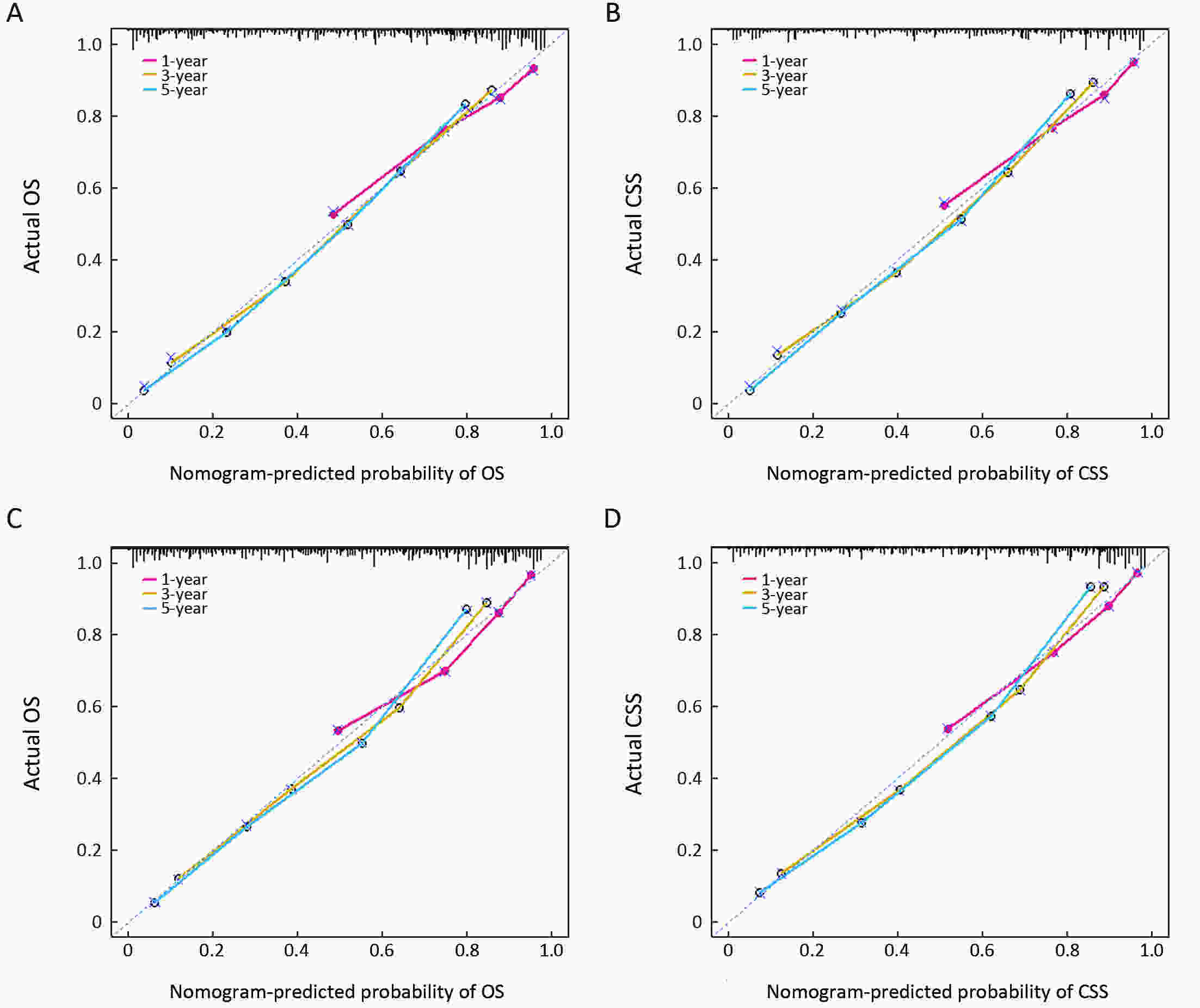
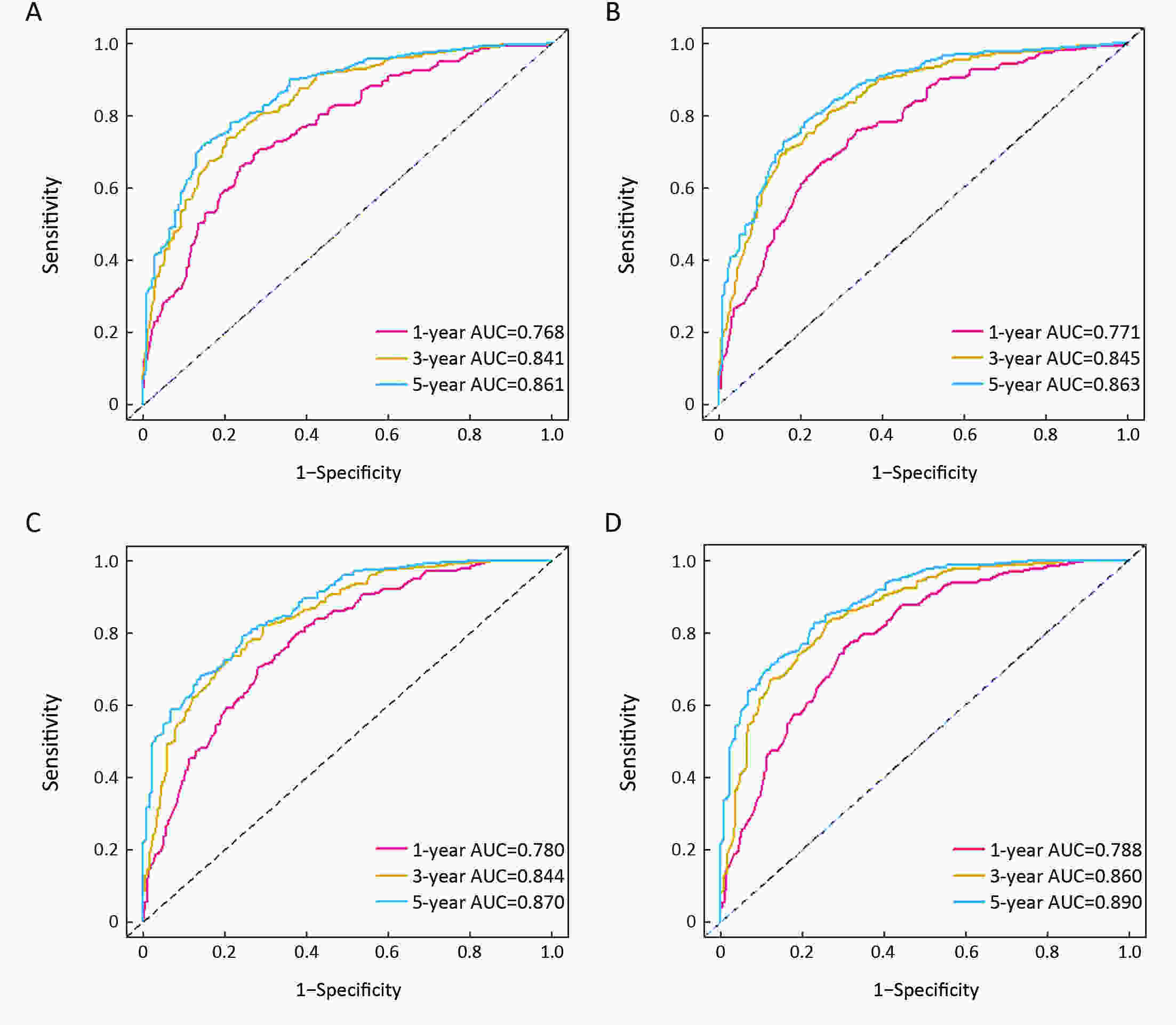
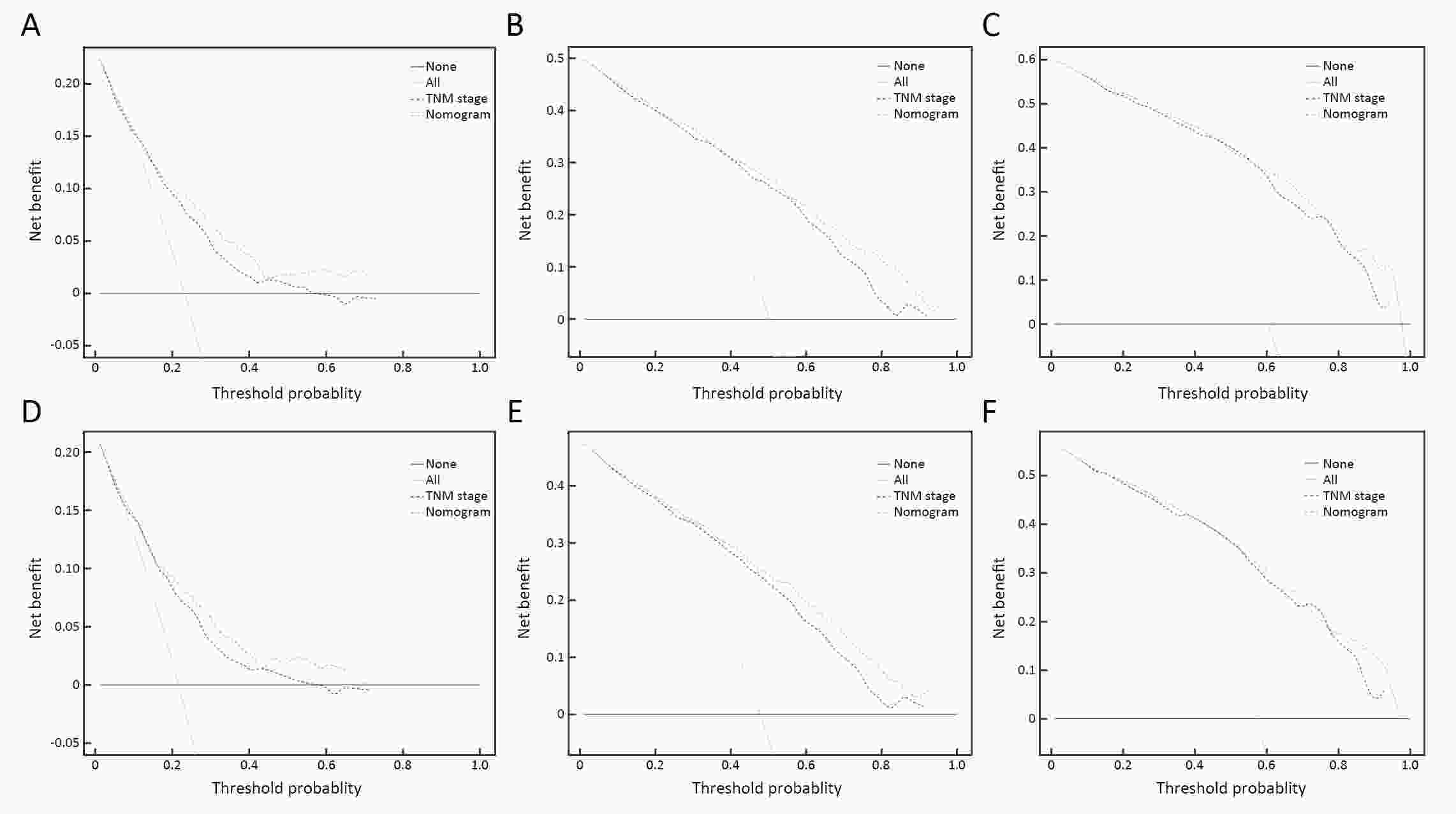
ObjectiveOur aims were to establish novel nomogram models, which directly targeted patients with signet ring cell carcinoma (SRC), for individualized prediction of overall survival (OS) rate and cancer-specific survival (CSS). MethodsWe selected 1,365 SRC patients diagnosed from 2010 to 2015 from Surveillance, Epidemiology and End Results (SEER) database, and then randomly partitioned them into a training cohort and a validation cohort. Independent predicted indicators, which were identified by using univariate testing and multivariate analyses, were used to construct our prognostic nomogram models. Three methods, Harrell concordance index (C-index), receiver operating characteristics (ROC) curve and calibration curve, were used to assess the ability of discrimination and predictive accuracy. Integrated discrimination improvement (IDI), net reclassification improvement (NRI) and decision curve analysis (DCA) were used to assess clinical utility of our nomogram models. ResultsSix independent predicted indicators, age, race, log odds of positive lymph nodes (LODDS), T stage, M stage and tumor size, were associated with OS rate. Nevertheless, only five independent predicted indicators were associated with CSS except race. The developed nomograms based on those independent predicted factors showed reliable discrimination. C-index of our nomogram for OS and CSS was 0.760 and 0.763, which were higher than American Joint Committee on Cancer (AJCC) 8th edition tumor-node-metastasis (TNM) staging system (0.734 and 0.741, respectively). C-index of validation cohort for OS was 0.757 and for CSS was 0.773. The calibration curves also performed good consistency. IDI, NRI and DCA showed the nomograms for both OS and CSS had a comparable clinical utility than the TNM staging system. ConclusionsThe novel nomogram models based on LODDS provided satisfying predictive ability of SRC both in OS and CSS than AJCC 8th edition TNM staging system alone.
2020, 32(6): 794-803.
doi: 10.21147/j.issn.1000-9604.2020.06.12
Abstract:
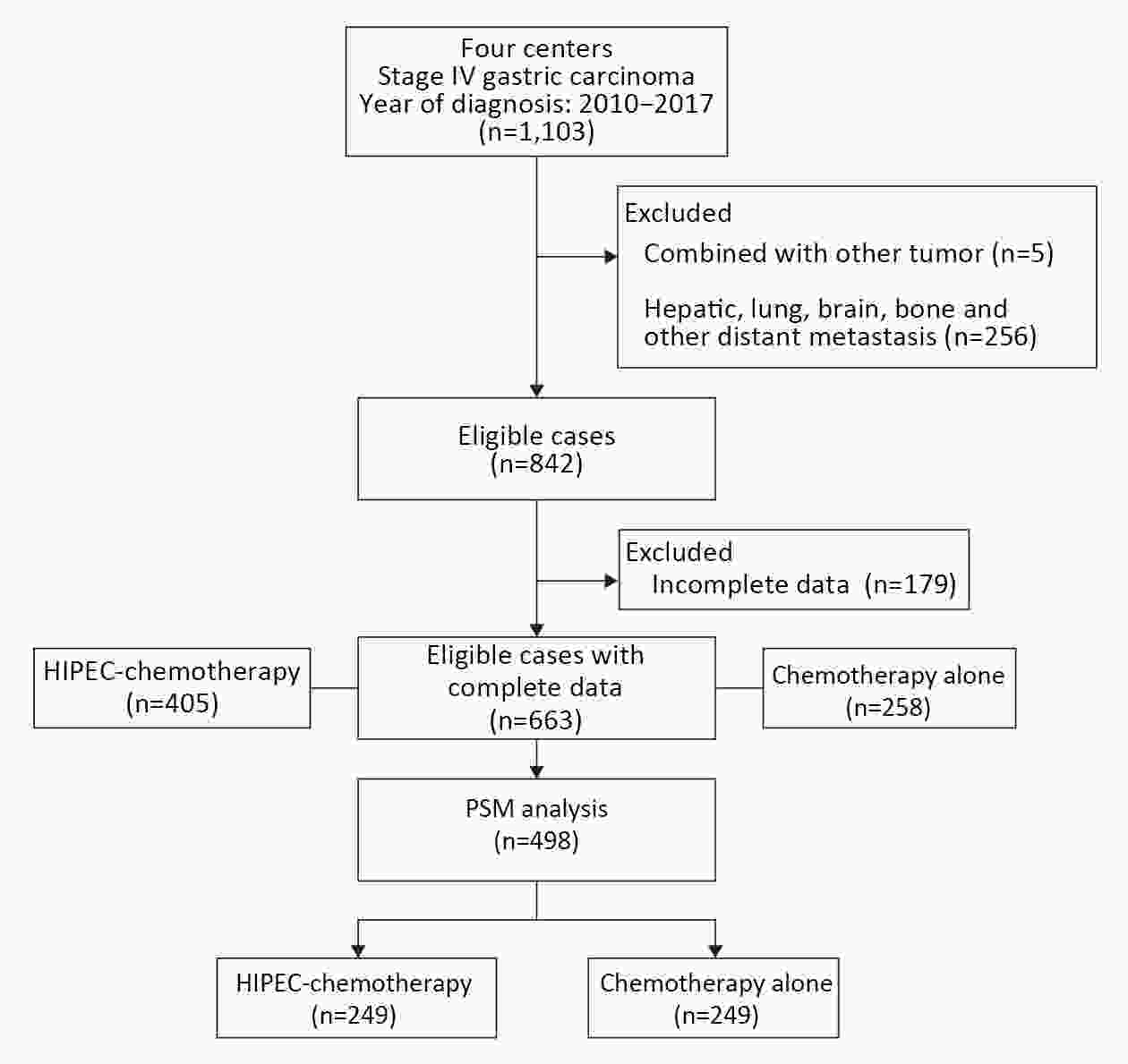
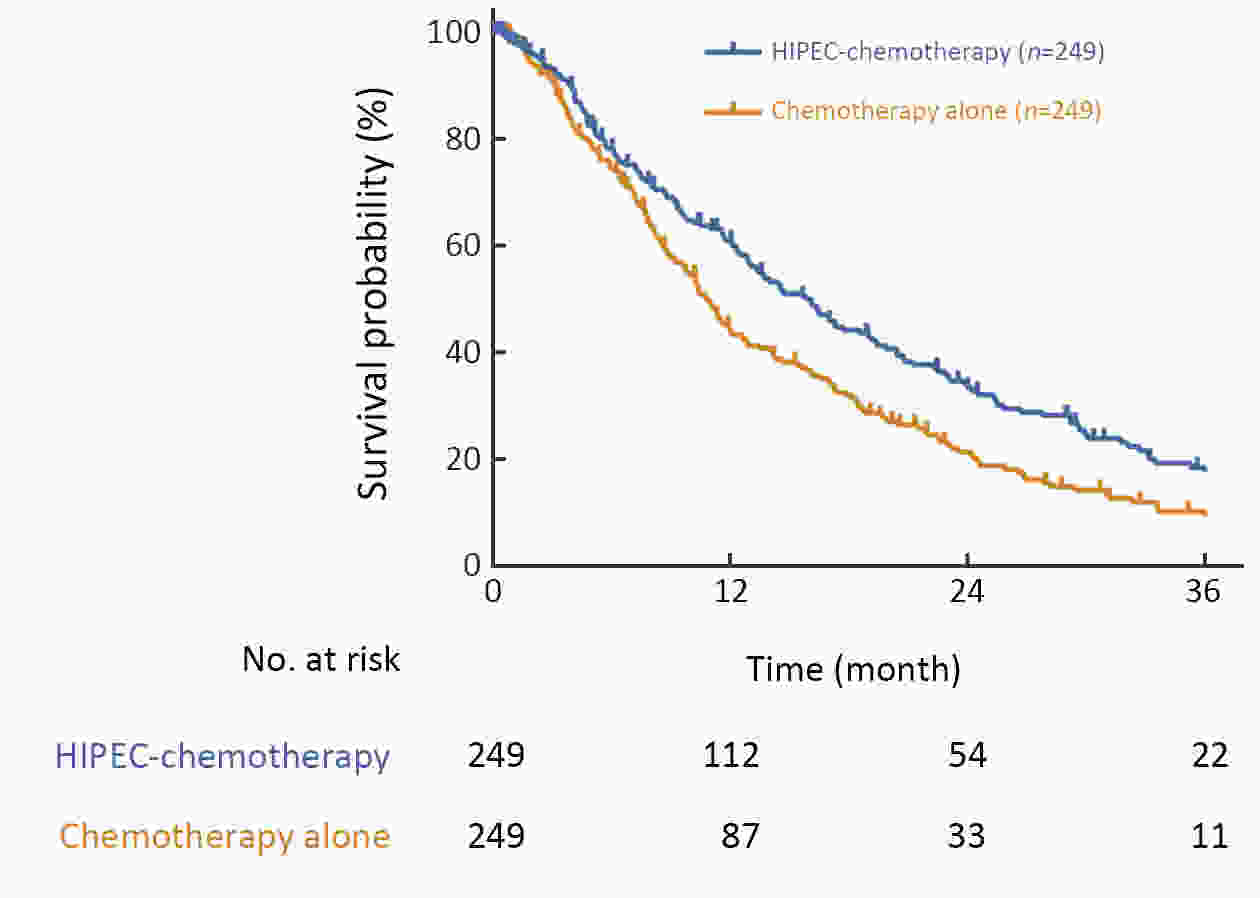
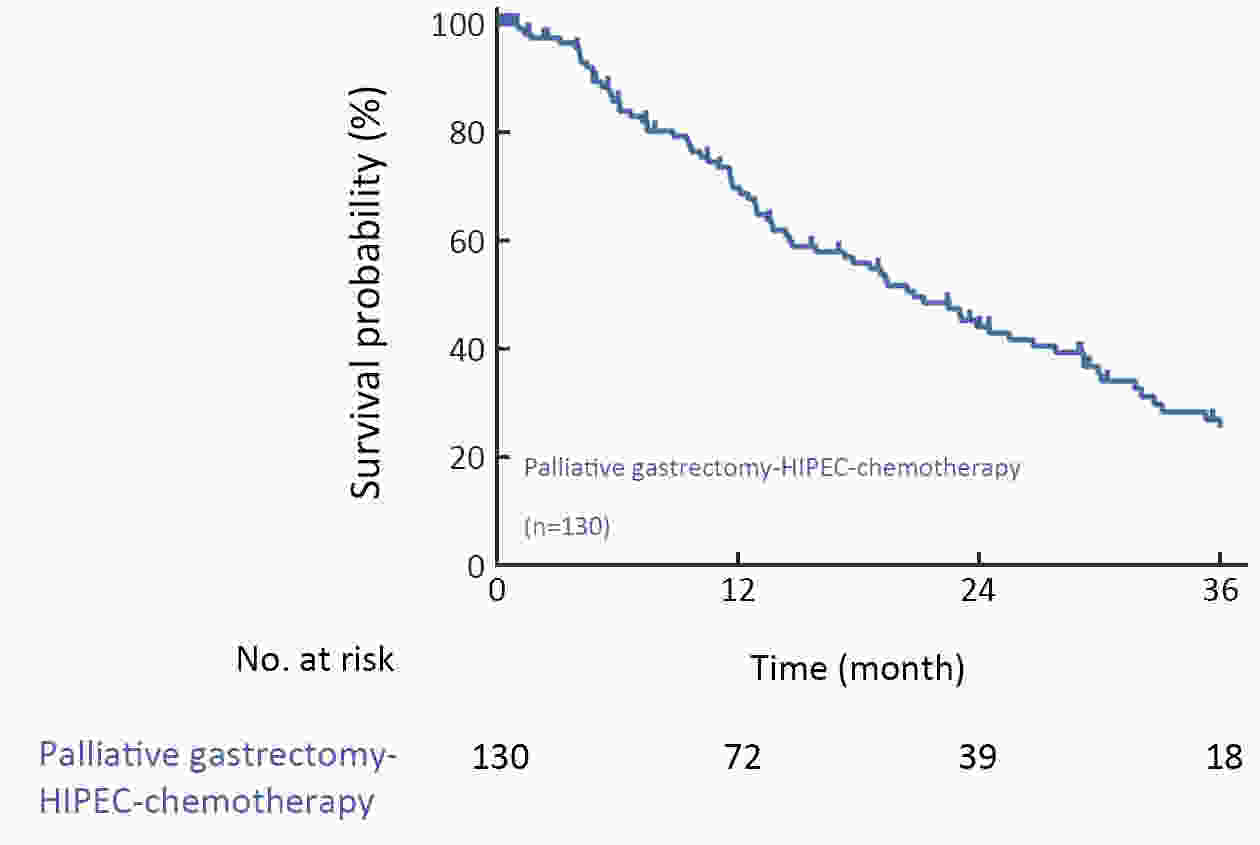
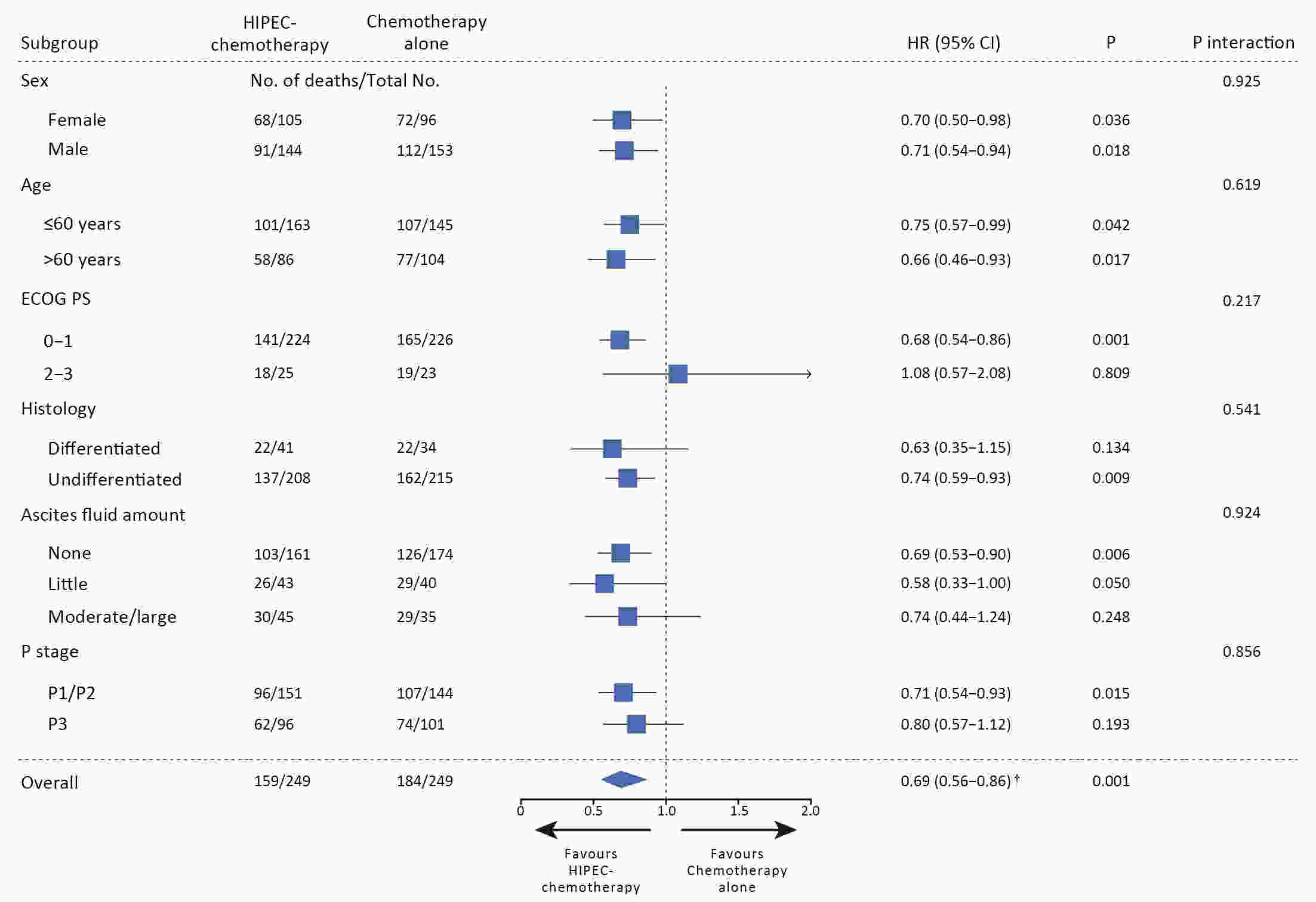
ObjectiveSystemic chemotherapy has limited efficacy in the treatment of peritoneal metastasis (PM) in gastric cancer (GC). Hyperthermic intraperitoneal chemotherapy (HIPEC) combined with complete cytoreductive surgery (CRS) has shown promising outcomes but remains controversial. The present study aimed to evaluate the safety and efficacy of HIPEC without CRS in GC patients with PM. MethodsThis retrospective propensity score-matched multicenter cohort study included GC patients with PM treated with either chemotherapy alone (Cx group) or with HIPEC combined with chemotherapy (HIPEC-Cx group) in four Chinese high-volume gastric medical centers between 2010 and 2017. The primary outcomes were median survival time (MST) and 3-year overall survival (OS). Propensity score matching was performed to compensate for controlling potential confounding effects and selection bias. ResultsOf 663 eligible patients, 498 were matched. The MST in the Cx and HIPEC-Cx groups was 10.8 and 15.9 months, respectively [hazard ratio (HR)=0.71, 95% confidence interval (95% CI), 0.58−0.88; P=0.002]. The 3-year OS rate was 10.1% (95% CI, 5.4%−14.8%) and 18.4% (95% CI, 12.3%−24.5%) in the Cx and HIPEC-Cx groups, respectively (P=0.017). The complication rates were comparable. The time to first flatus and length of hospital stay for patients undergoing HIPEC combined with chemotherapy was longer than that of chemotherapy alone (4.6±2.4 d vs. 2.7±1.8 d, P<0.001; 14.2±5.8 d vs. 11.4±7.7 d, P<0.001), respectively. The median follow-up period was 33.2 months. ConclusionsCompared with standard systemic chemotherapy, HIPEC combined with chemotherapy revealed a statistically significant survival benefit for GC patients with PM, without compromising patient safety.
2020, 32(6): 804-814.
doi: 10.21147/j.issn.1000-9604.2020.06.08
Abstract:
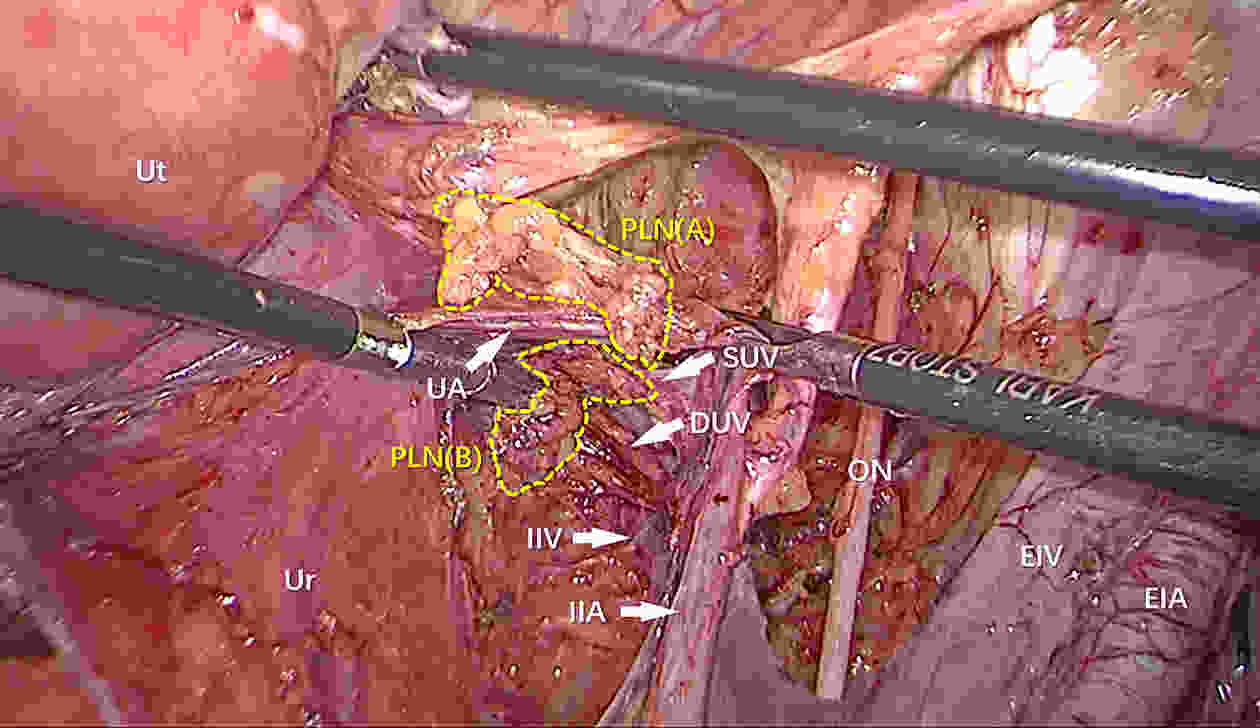
ObjectiveTo investigate the clinical significance of separate lateral parametrial lymph node dissection (LPLND) in improving parametrial lymph node (PLN) and its metastasis detection rate during radical hysterectomy for early-stage cervical cancer. MethodsFrom July 2007 to August 2017, 2,695 patients with cervical cancer in stage IB1−IIA2 underwent radical hysterectomy were included. Of these patients, 368 underwent separate dissection of PLNs using the LPLND method, and 2,327 patients underwent conventional radical hysterectomy (CRH). We compared the surgical parameters, PLN detection rate and PLN metastasis rate between the two groups. ResultsCompared with CRH group, the rate of laparoscopic surgery was higher (60.3% vs. 15.9%, P<0.001), and the blood transfusion rate was lower (19.0% vs. 29.0%, P<0.001) in the LPLND group. PLNs were detected in 356 cases (96.7%) in the LPLND group, and 270 cases (11.6%) in the CRH group (P<0.001), respectively. The number of PLNs detected in the LPLND group was higher than that in the CRH group (median 3 vs. 1, P<0.001). The PLN metastases were detected in 25 cases (6.8%) in the LPLND group, and 18 cases (0.8%) in the CRH group (P<0.001), respectively. In multivariable analysis, LPLND is an independent factor not only for PLN detection [odds ratio (OR)=228.999, 95% confidence interval (95% CI): 124.661−420.664; P<0.001], but also for PLN metastasis identification (OR=10.867, 95% CI: 5.381−21.946; P<0.001). ConclusionsLPLND is feasible and safe. The surgical method significantly improves the detection rate of PLN and avoids omission of PLN metastasis during radical hysterectomy for early-stage cervical cancer.

 Abstract
Abstract FullText HTML
FullText HTML PDF 405KB
PDF 405KB