2024 Vol.36(4)
Display Mode: |
2024, 36(4): 351-367.
doi: 10.21147/j.issn.1000-9604.2024.04.01
Abstract:
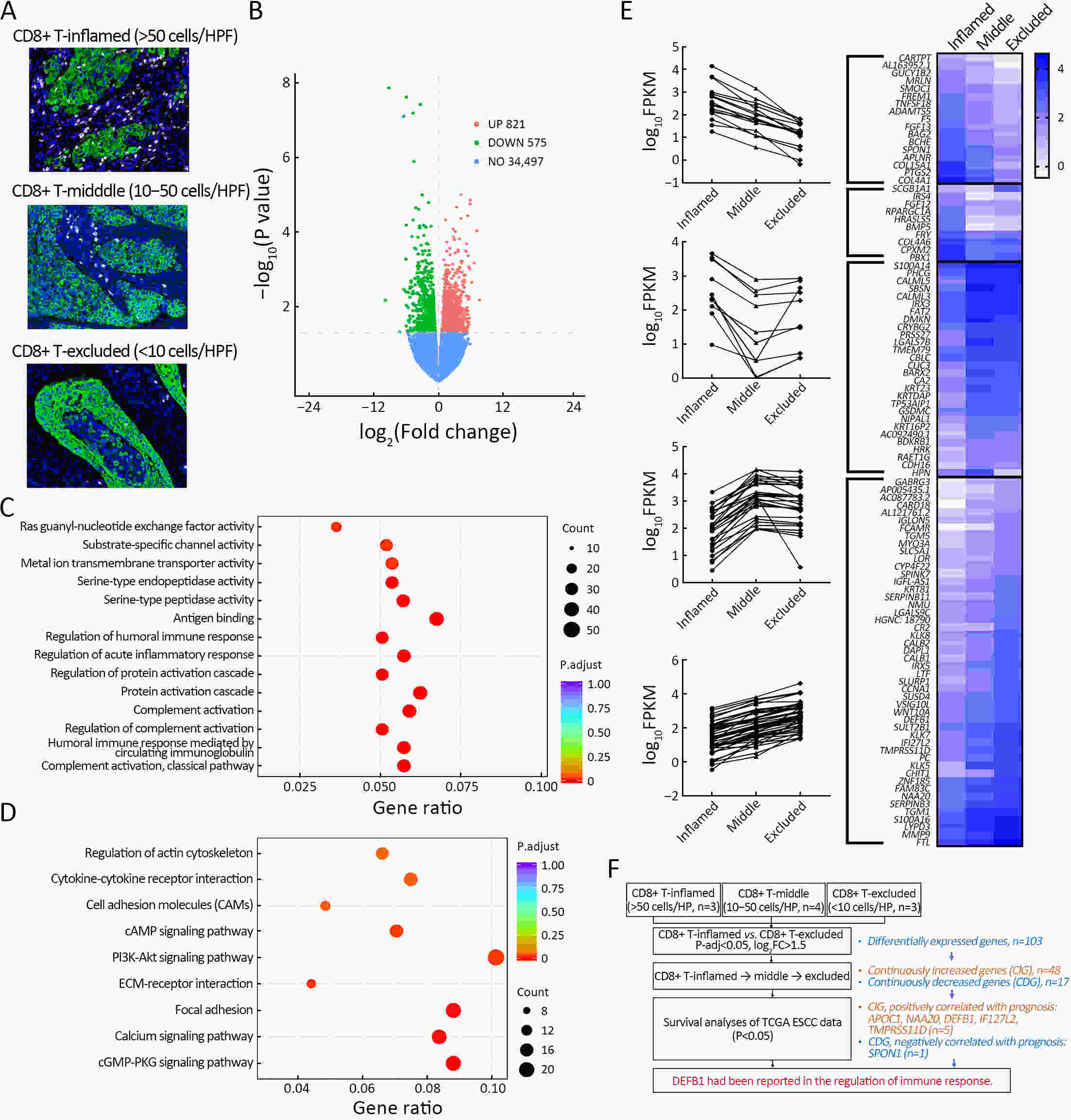
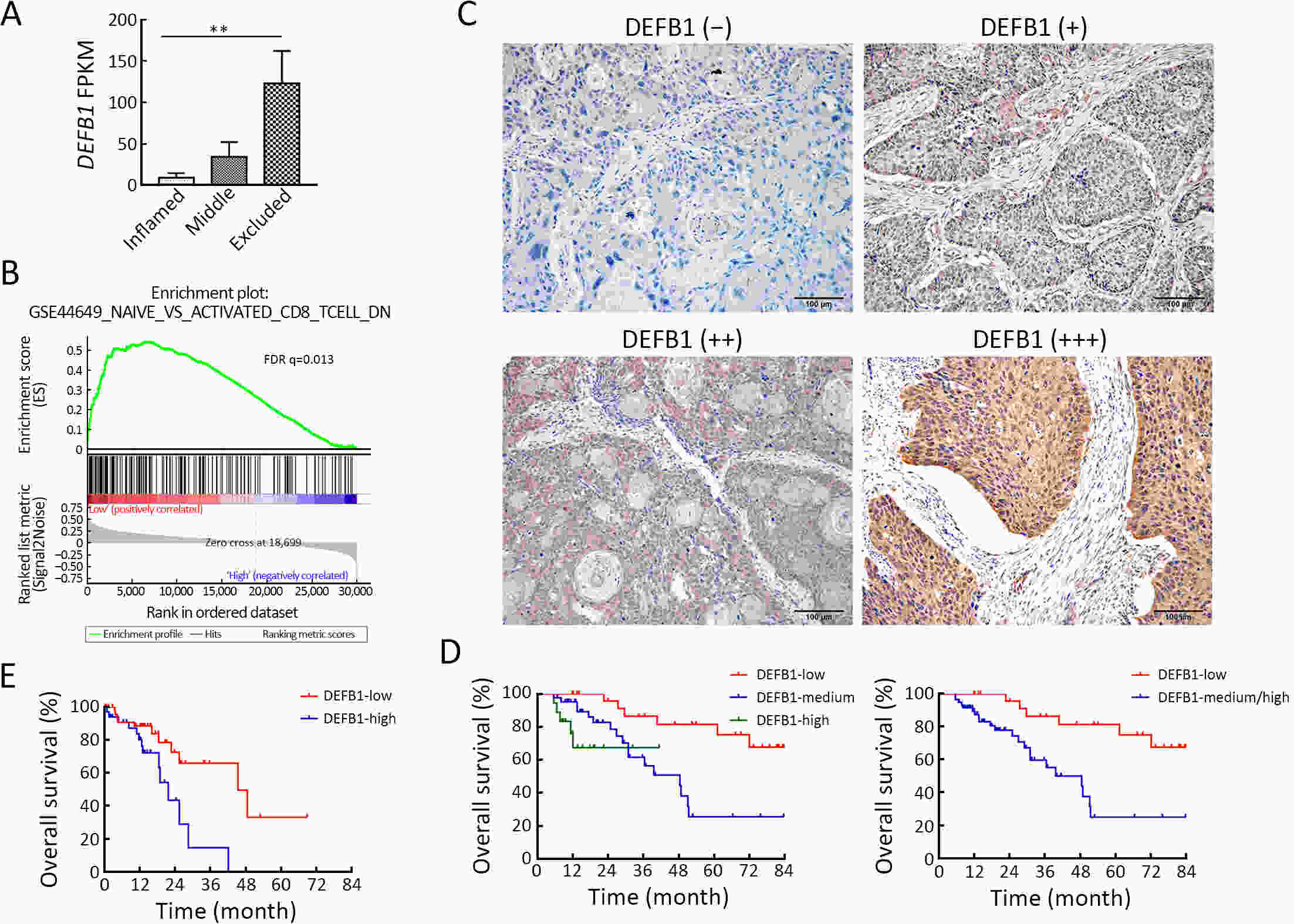
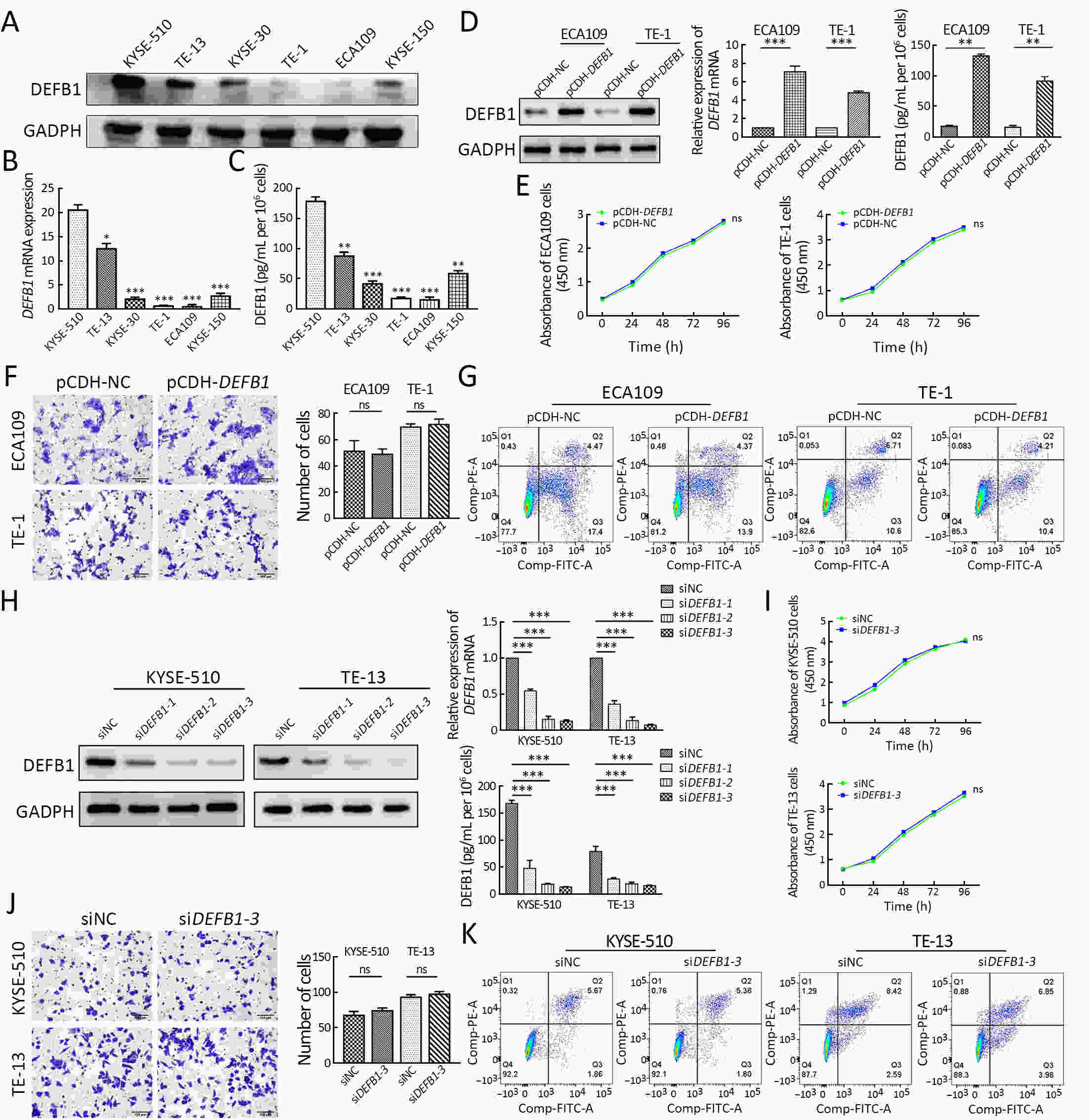
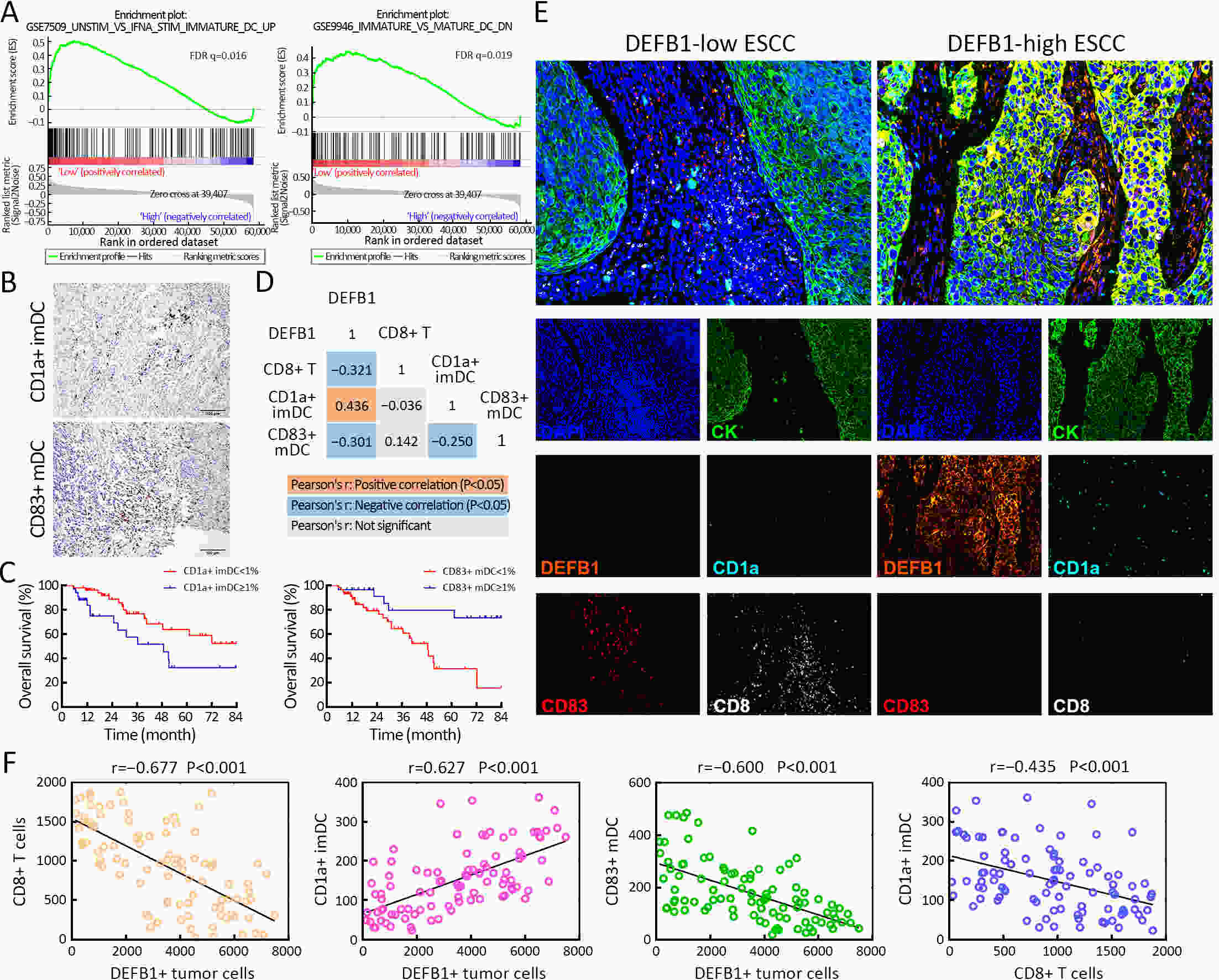
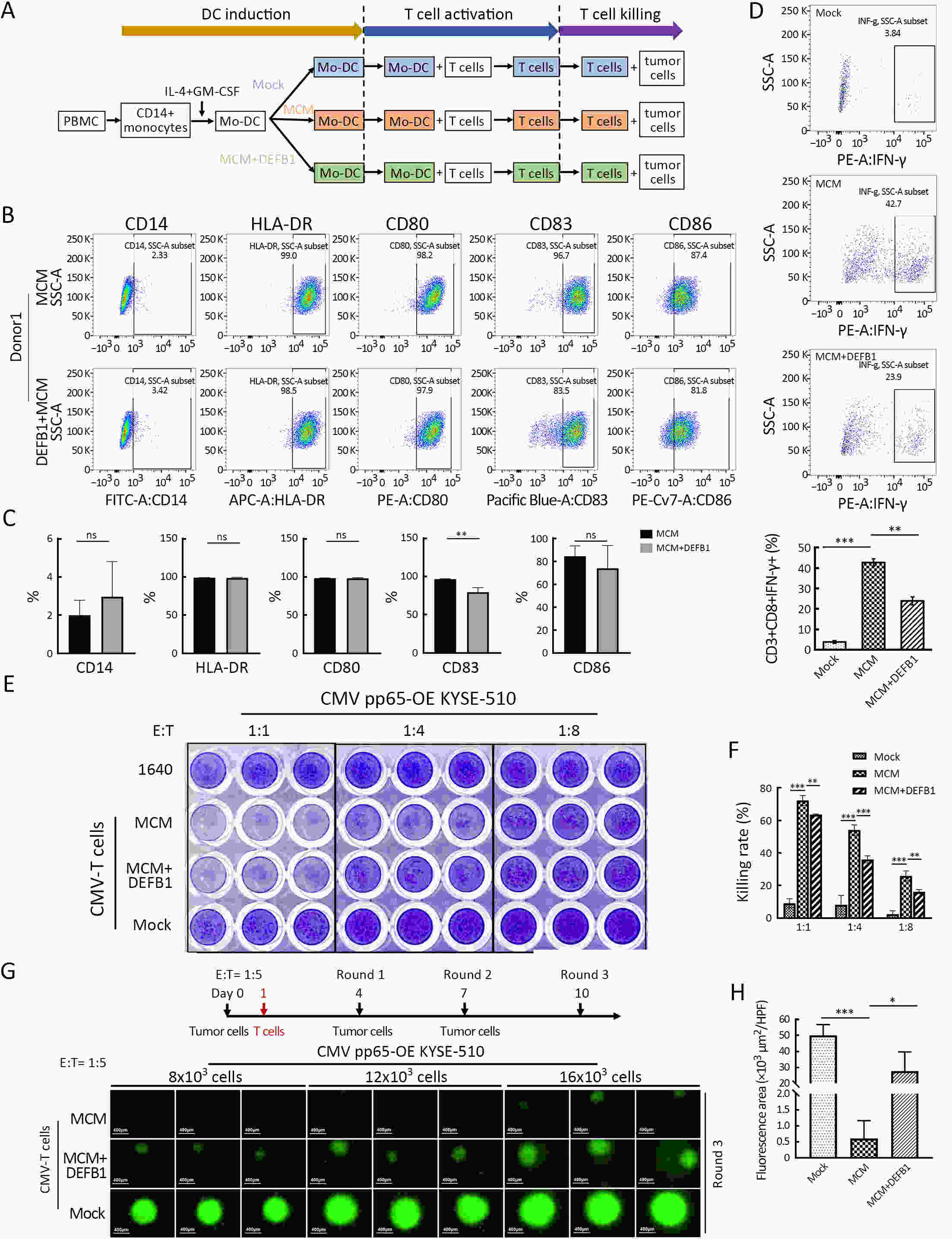
ObjectiveCD8+ T cells are the key effector cells in the anti-tumor immune response. The mechanism underlying the infiltration of CD8+ T cells in esophageal squamous cell carcinoma (ESCC) has not been clearly elucidated. MethodsFresh ESCC tissues were collected and grouped according to the infiltration density of CD8+ T cells. After the transcriptome sequencing on these samples and the combined analyses with The Cancer Genome Atlas (TCGA) ESCC data, a secreted protein DEFB1 was selected to explore its potential role in the infiltration of CD8+ T cells. Bioinformatics analyses, histological verification and in vitro experiments were then performed. ResultsDEFB1 was highly expressed in ESCC, and the high expression of DEFB1 was an independent risk factor for overall survival. Since the up-regulation or down-regulation of DEFB1 did not affect the proliferation, migration and apoptosis of ESCC cells, we speculated that the oncogenic effect of DEFB1 was achieved by regulating microenvironmental characteristics. Bioinformatics analyses suggested that DEFB1 might play a major role in the inflammatory response and anti-tumor immune response, and correlate to the infiltration of immature dendritic cell (imDC) in ESCC. Histological analyses further confirmed that there were less CD8+ T cells infiltrated, less CD83+ mature DC (mDC) infiltrated and more CD1a+ imDC infiltrated in those ESCC samples with high expression of DEFB1. After the treatment with recombinant DEFB1 protein, the maturation of DC was hindered significantly, followed by the impairment of the killing effects of T cells in both 2D and 3D culture in vitro. ConclusionsTumor-derived DEFB1 can inhibit the maturation of DC and weaken the function of CD8+ T cells, accounting for the immune tolerance in ESCC. The role of DEFB1 in ESCC deserves further exploration.
2024, 36(4): 368-377.
doi: 10.21147/j.issn.1000-9604.2024.04.02
Abstract:
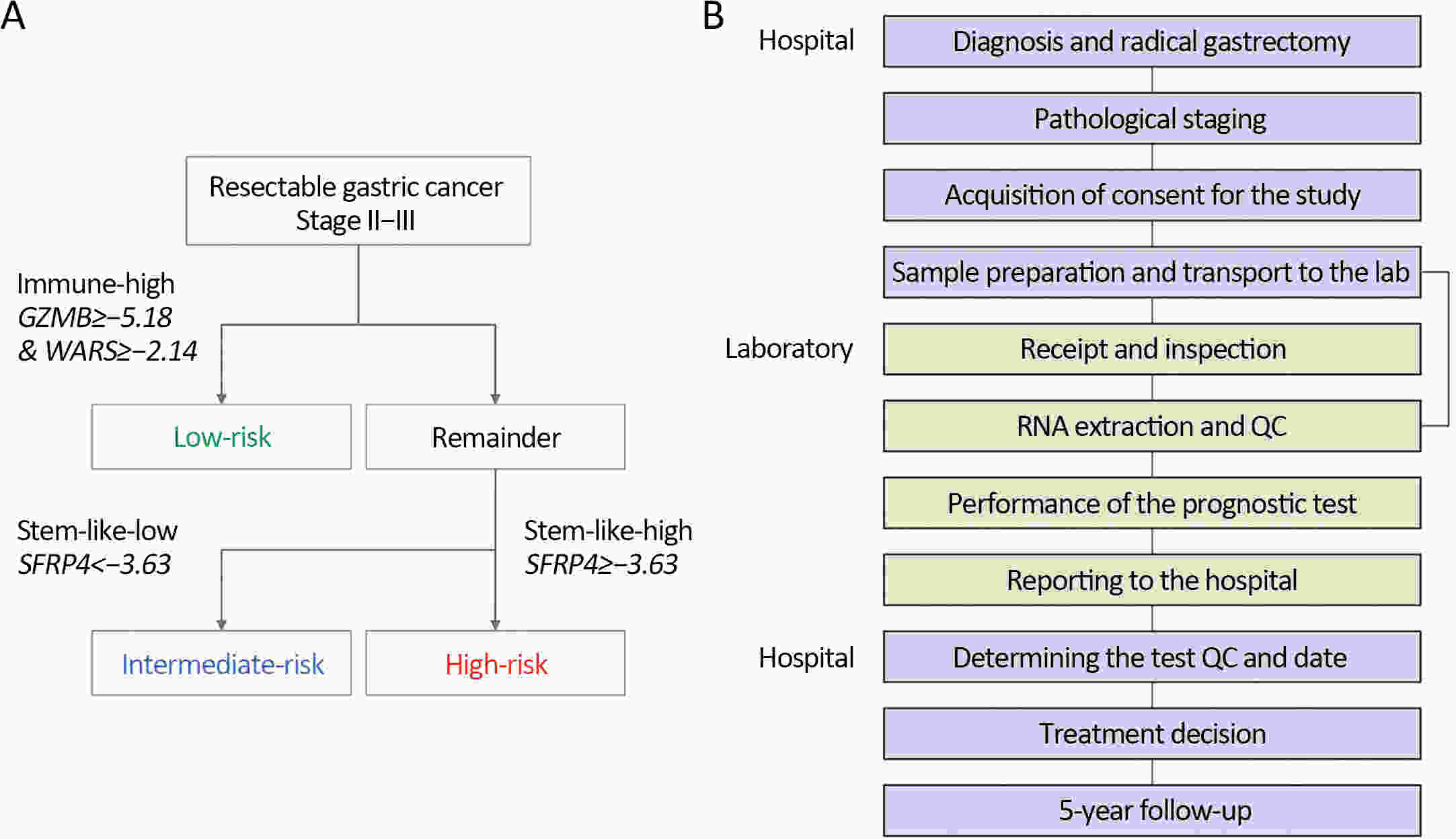
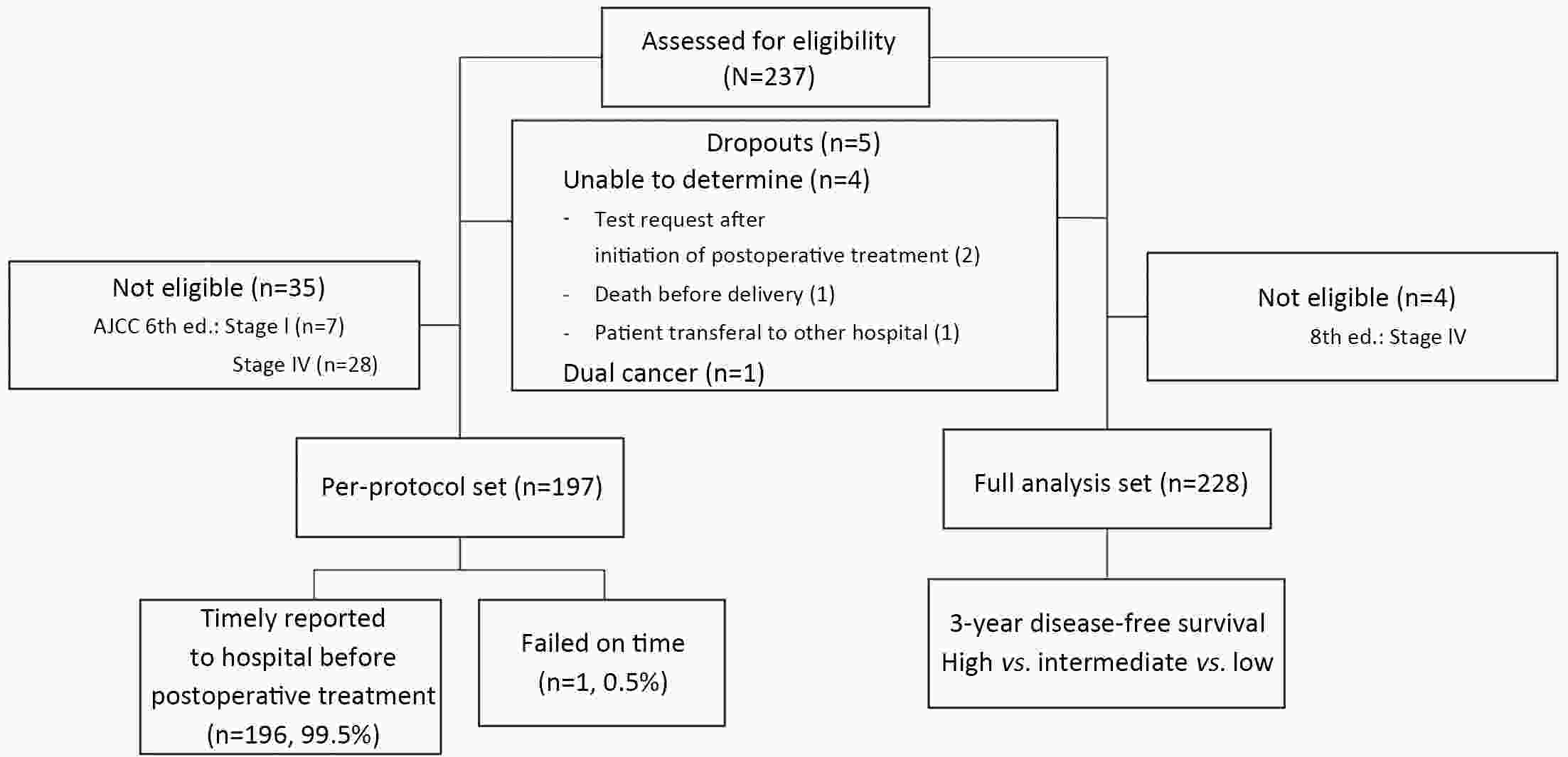
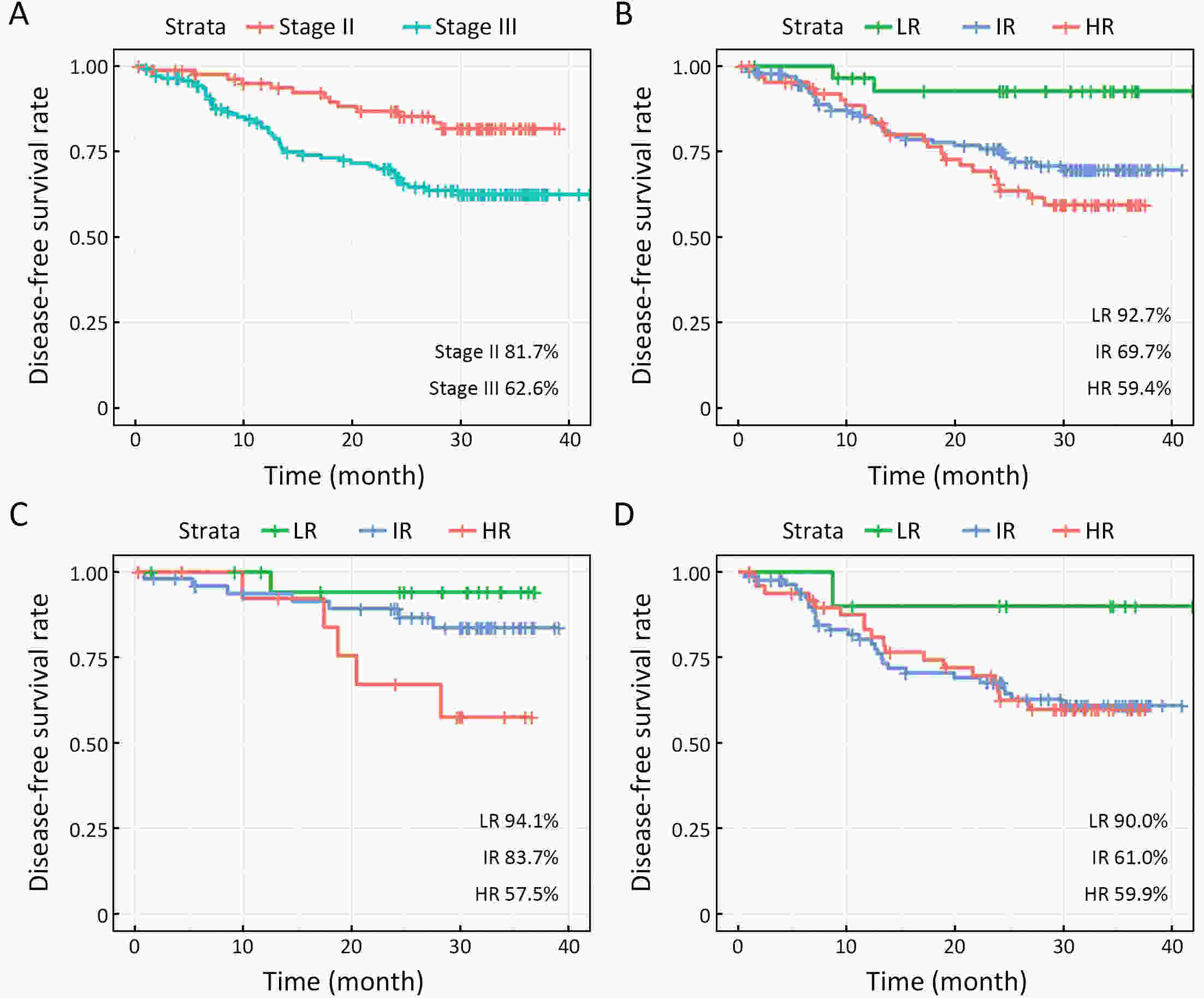
ObjectivePrecision medicine approaches emphasize the importance of reliable prognostic tools for guiding individualized therapy decisions. In this study, we evaluated the clinical feasibility of the single patient classifier (SPC) test, a new clinical-grade prognostic assay, in stage II−III gastric cancer patients. MethodsA prospective multicenter study was conducted, involving 237 patients who underwent gastrectomy between September 2019 and August 2020 across nine hospitals. The SPC test was employed to stratify patients into risk groups, and its feasibility and performance were evaluated. The primary endpoint was the proportion of the cases in which the test results were timely delivered before selecting postoperative treatment. Furthermore, 3-year disease-free survivals of risk groups were analyzed. ResultsThe SPC test met the primary endpoint criteria. The 99.5% of SPC tests were timely delivered to hospitals before the postoperative treatment started. In a clinical setting, the median time from the specimen transfer to laboratory to the result delivery to hospital was 4 d. Furthermore, 3-year disease-free survivals were significantly different between risk groups classified with SPC tests. ConclusionsThis study highlights the SPC test’s feasibility in offering crucial information timely delivered for making informed decisions regarding postoperative treatment strategies. It also provides evidence to support the implementation of a future prospective clinical trial aimed at evaluating the clinical utility of the SPC test in guiding personalized treatment decisions for gastric cancer patients.
2024, 36(4): 378-397.
doi: 10.21147/j.issn.1000-9604.2024.04.03
Abstract:
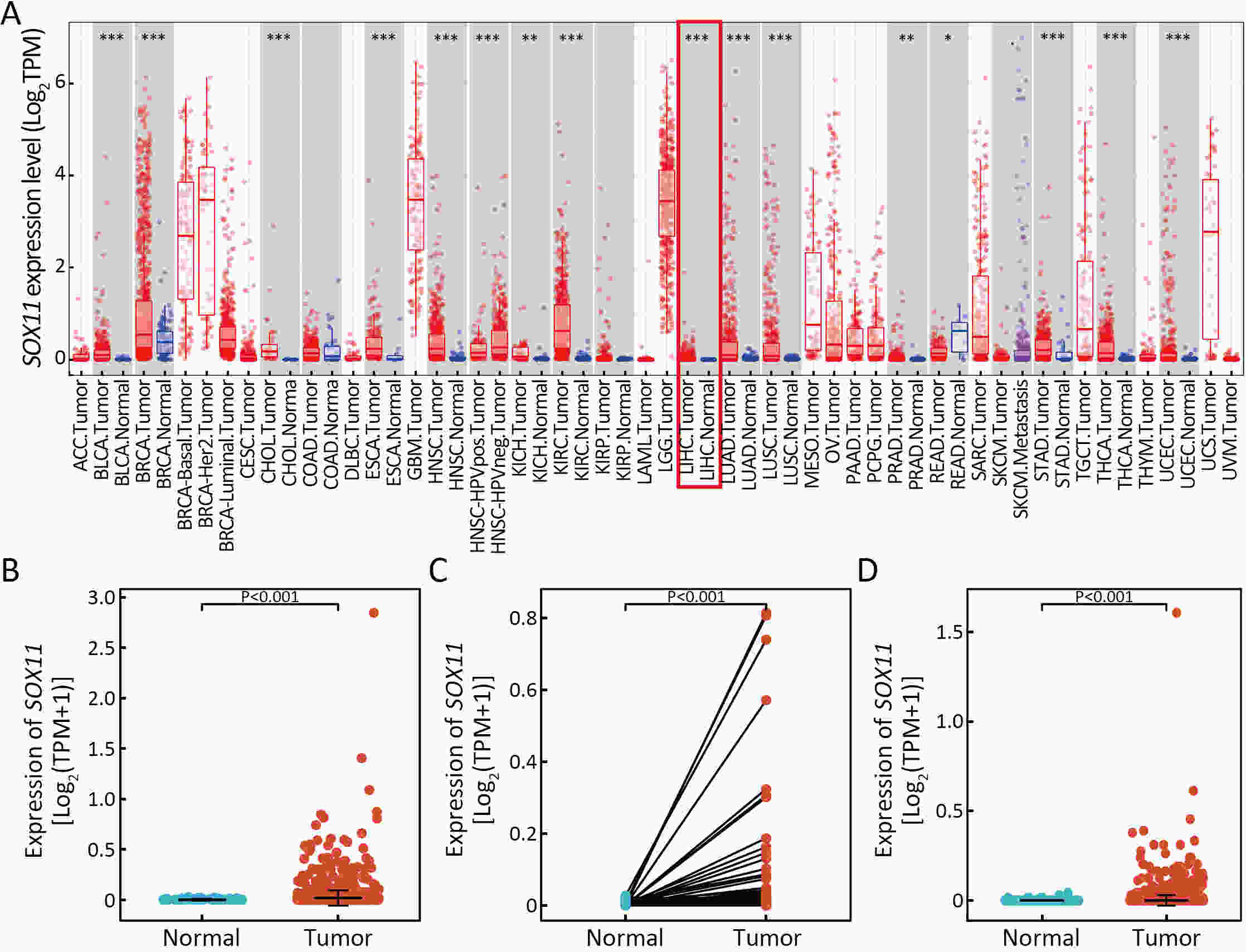
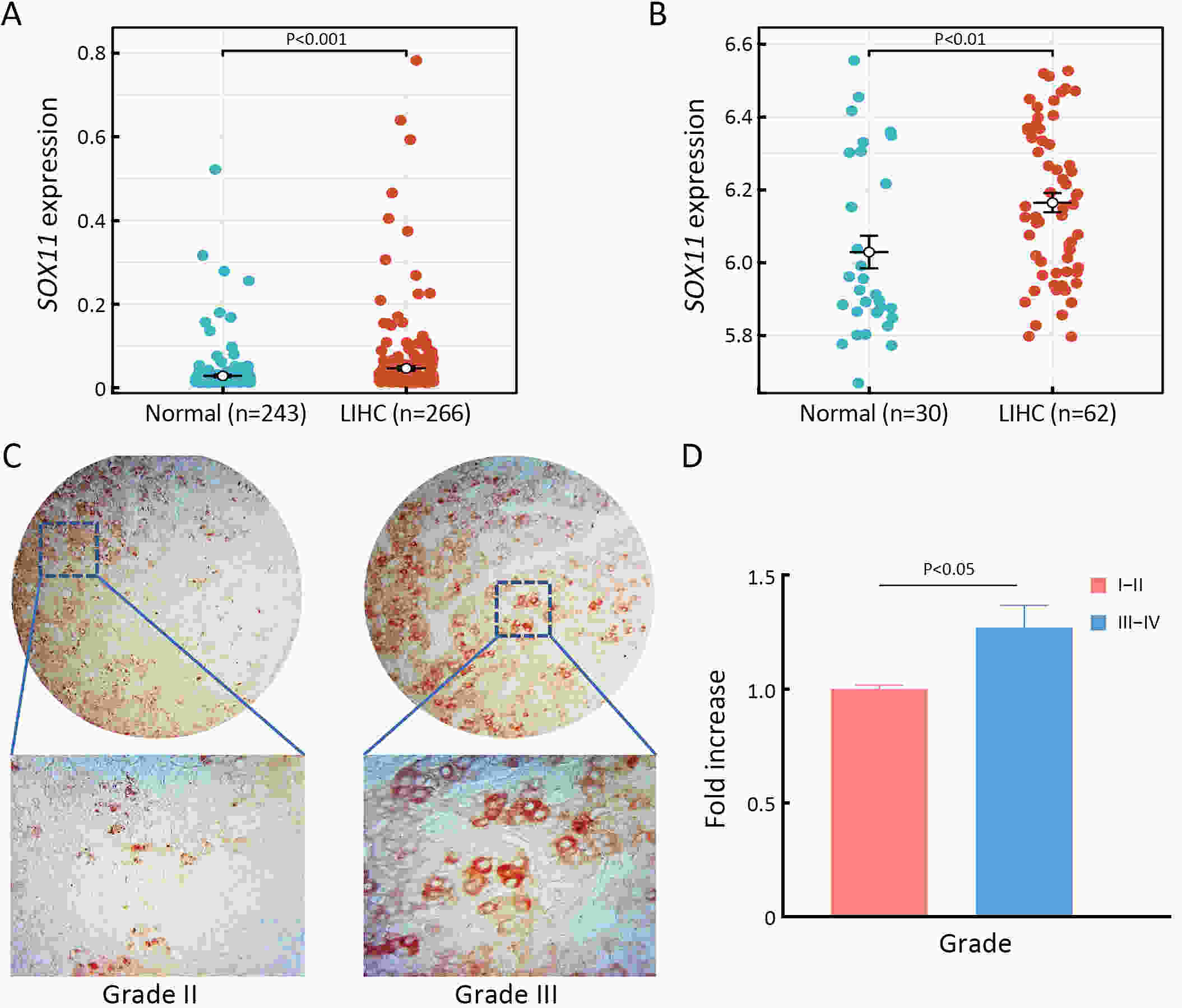
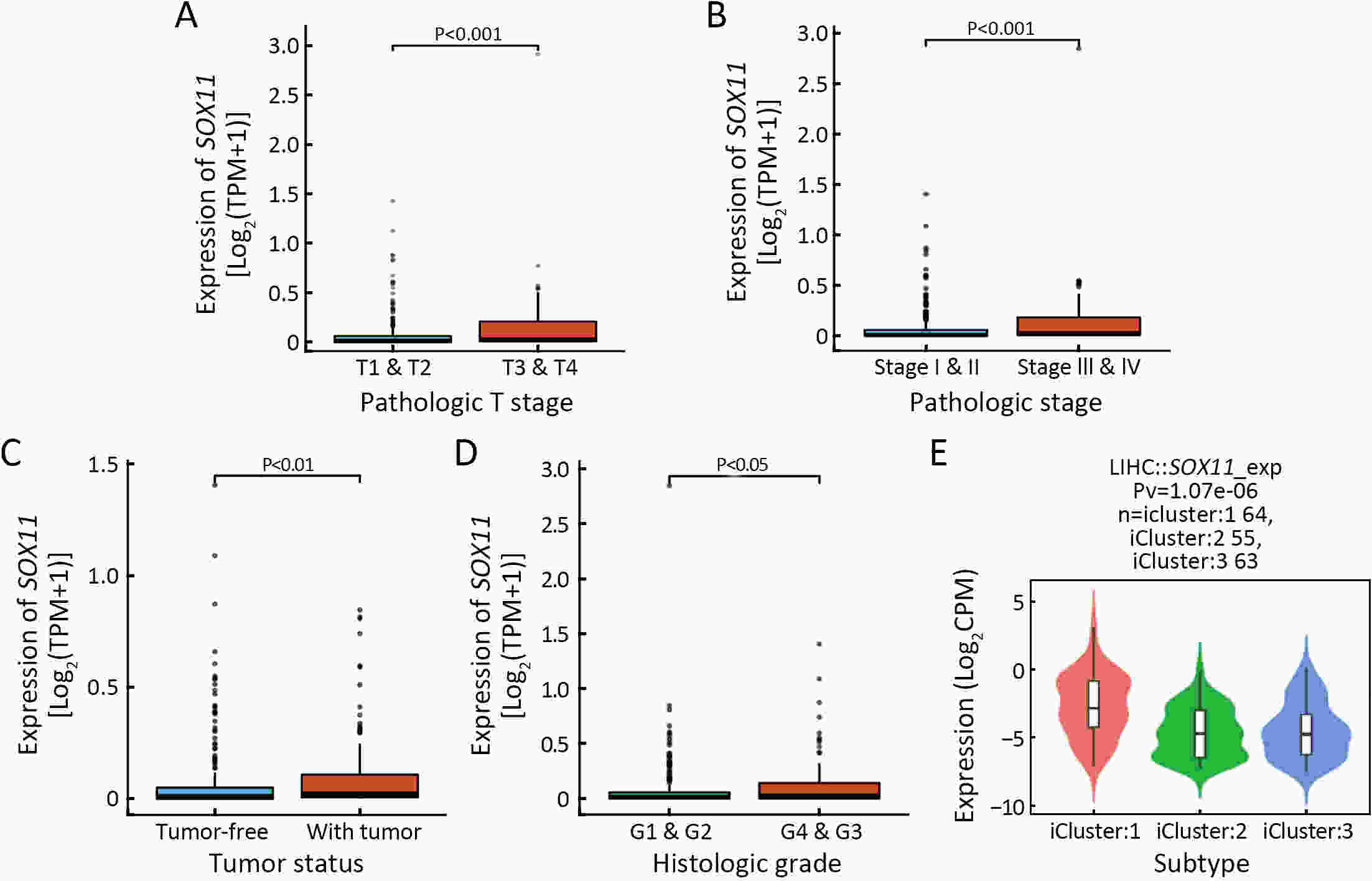
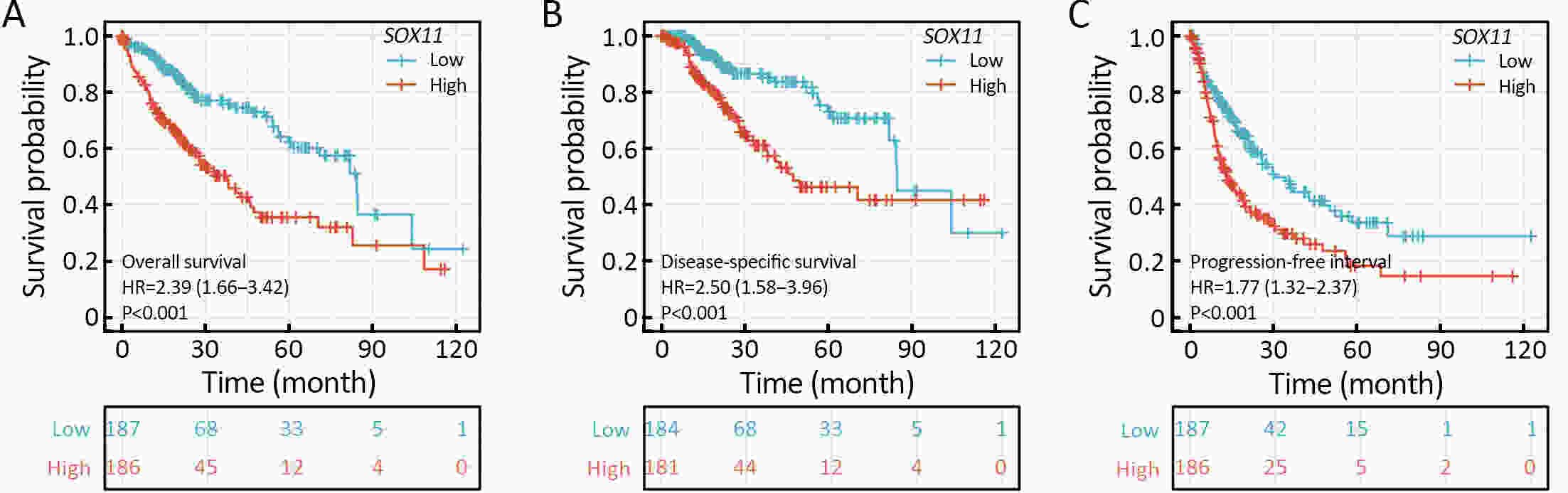
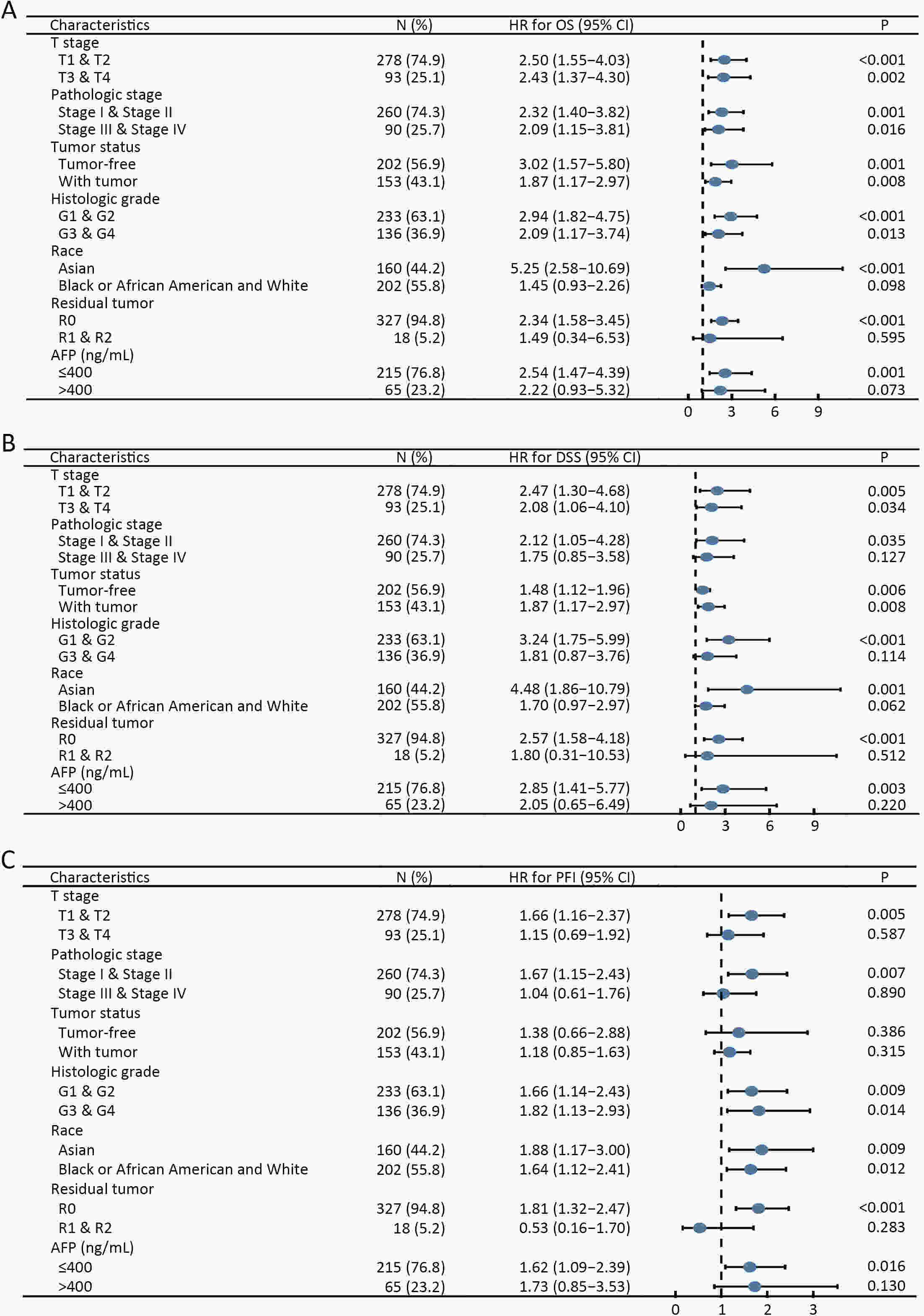
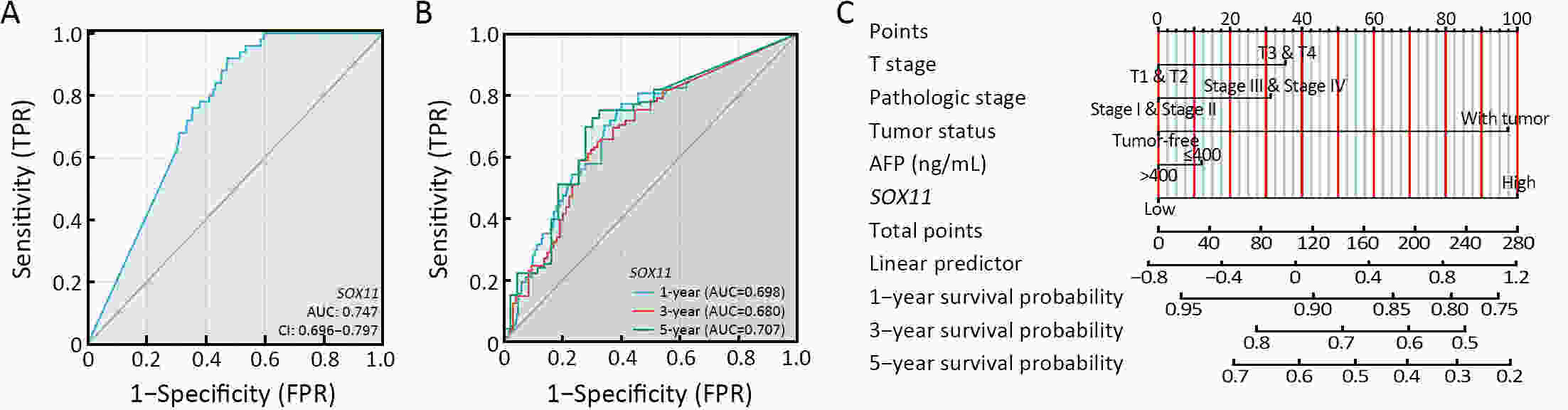
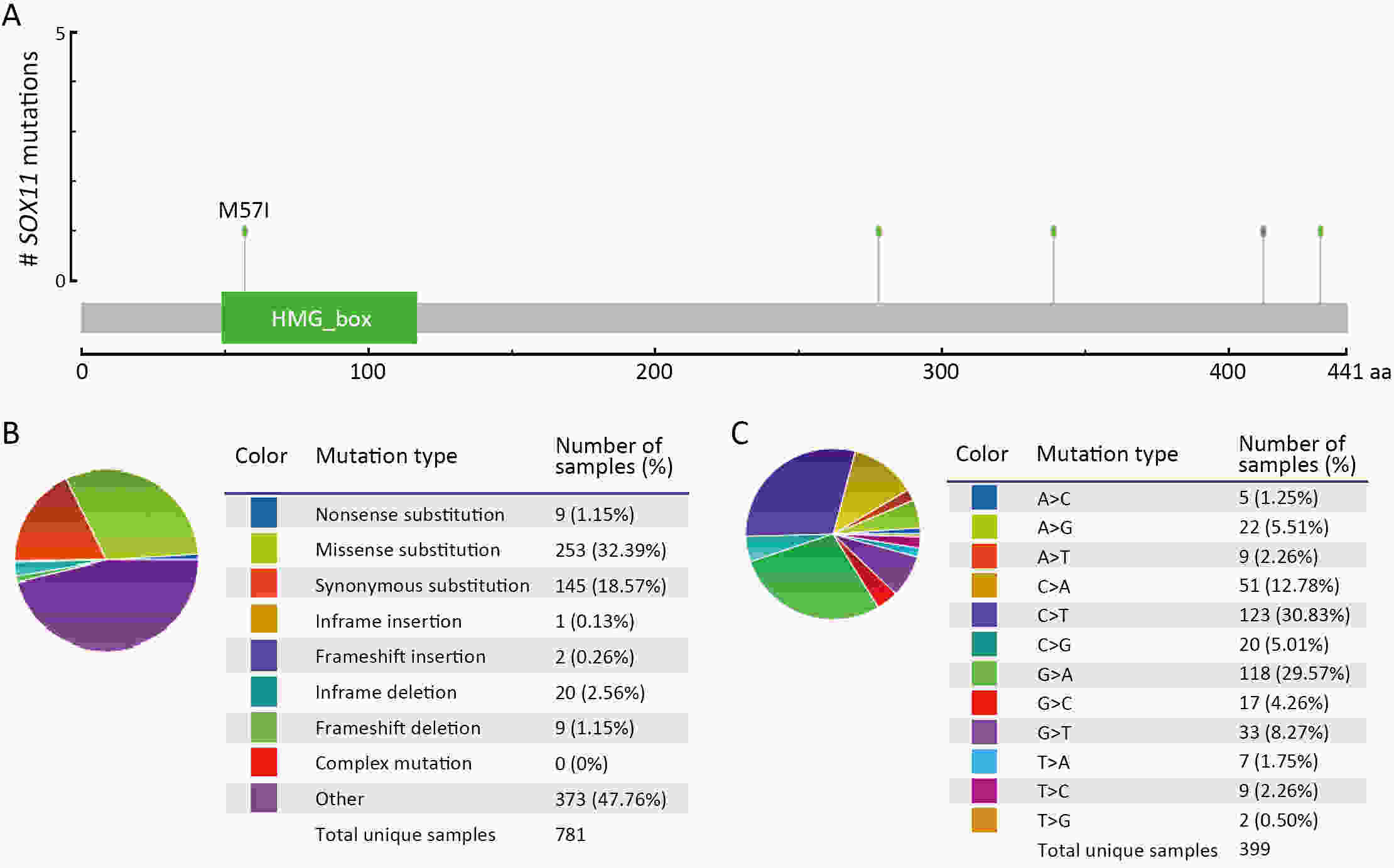
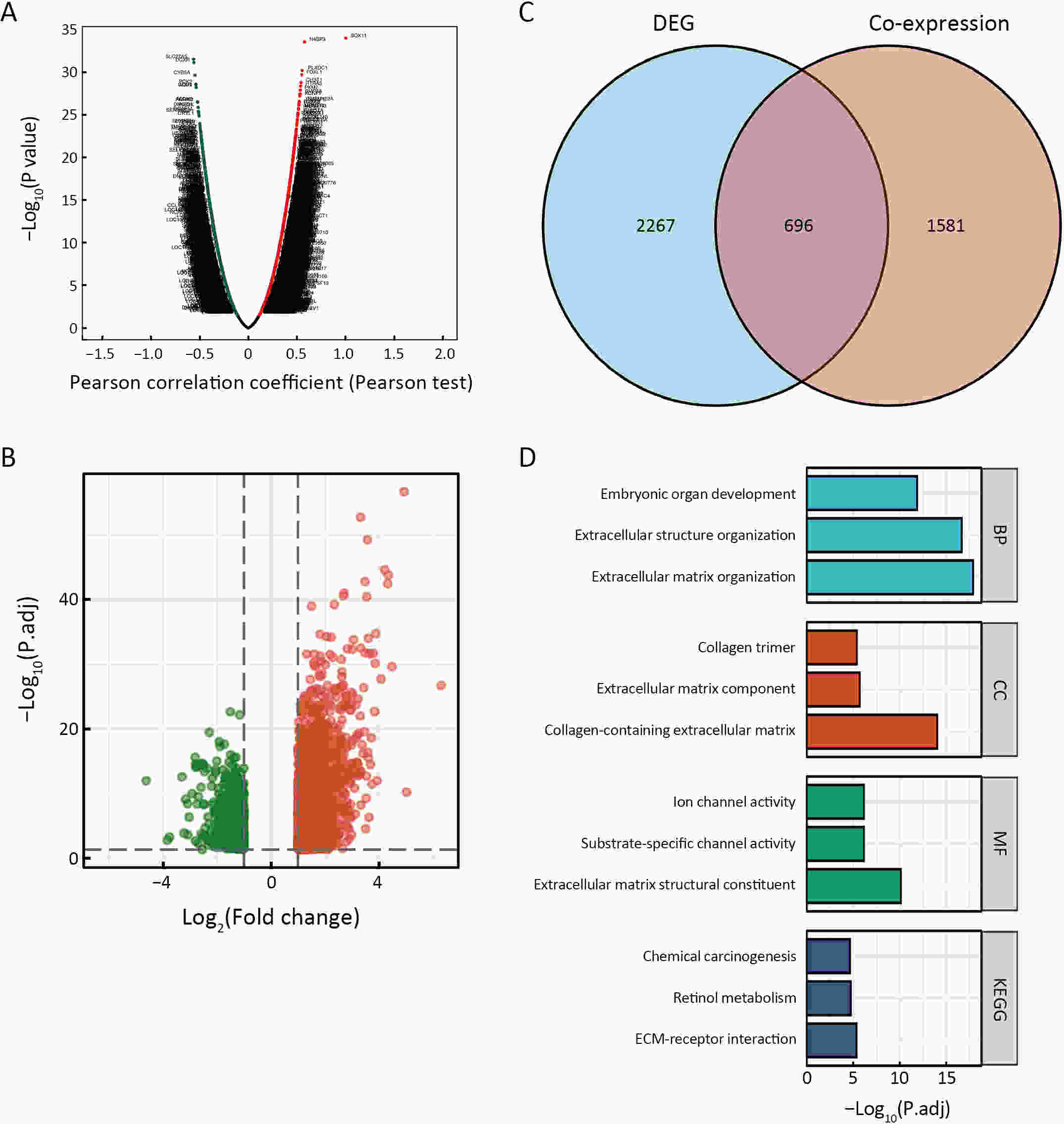
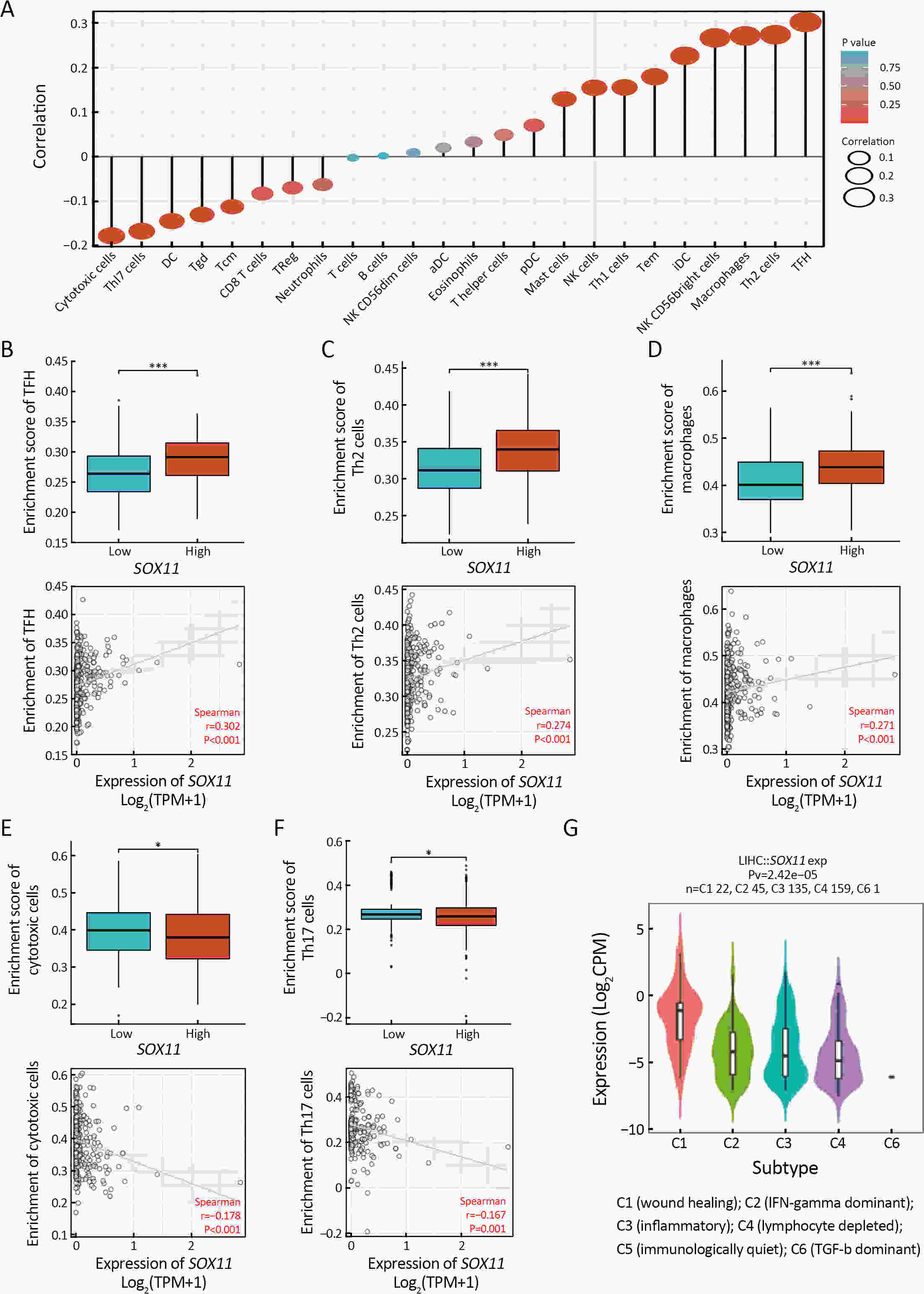
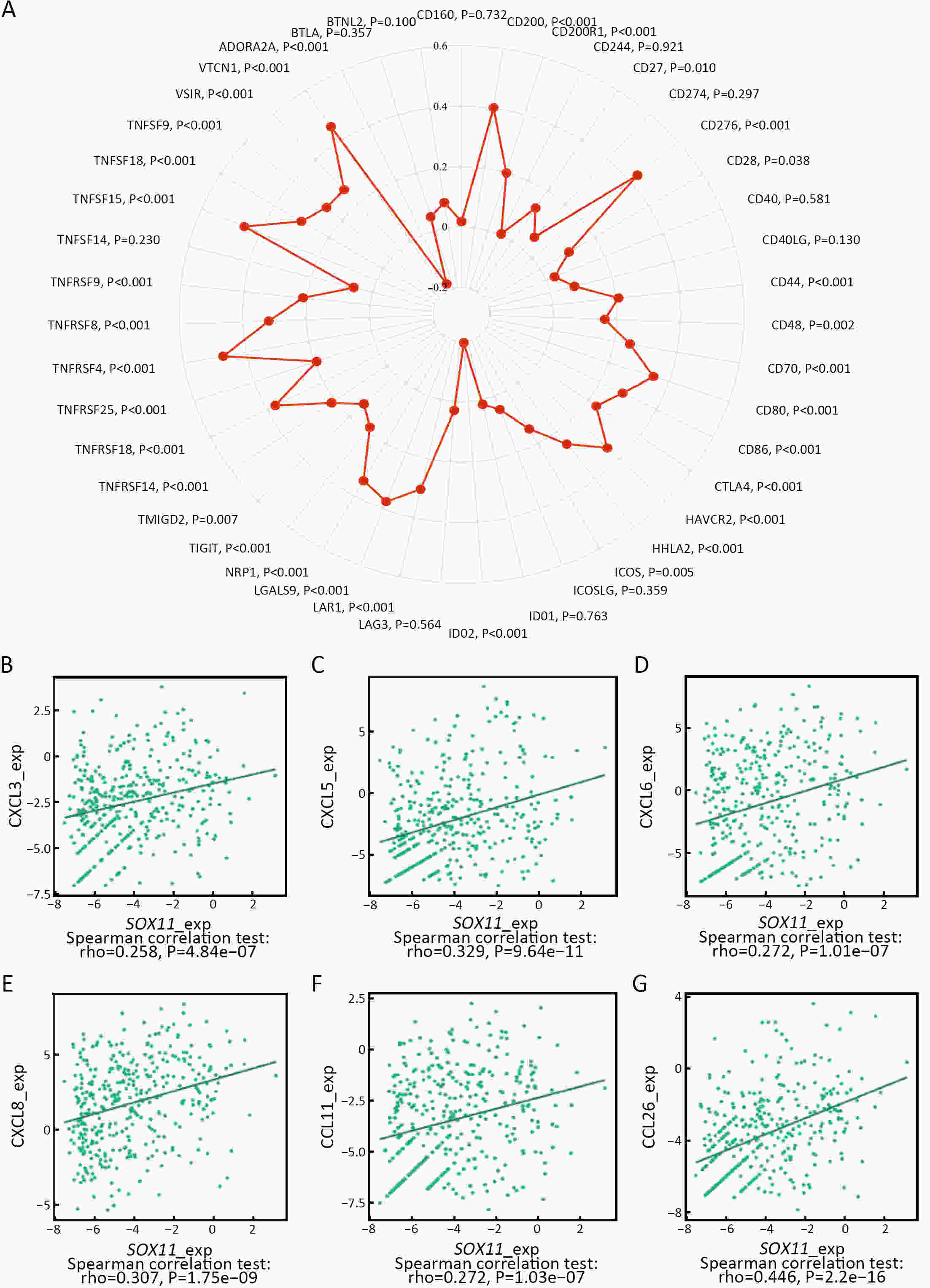
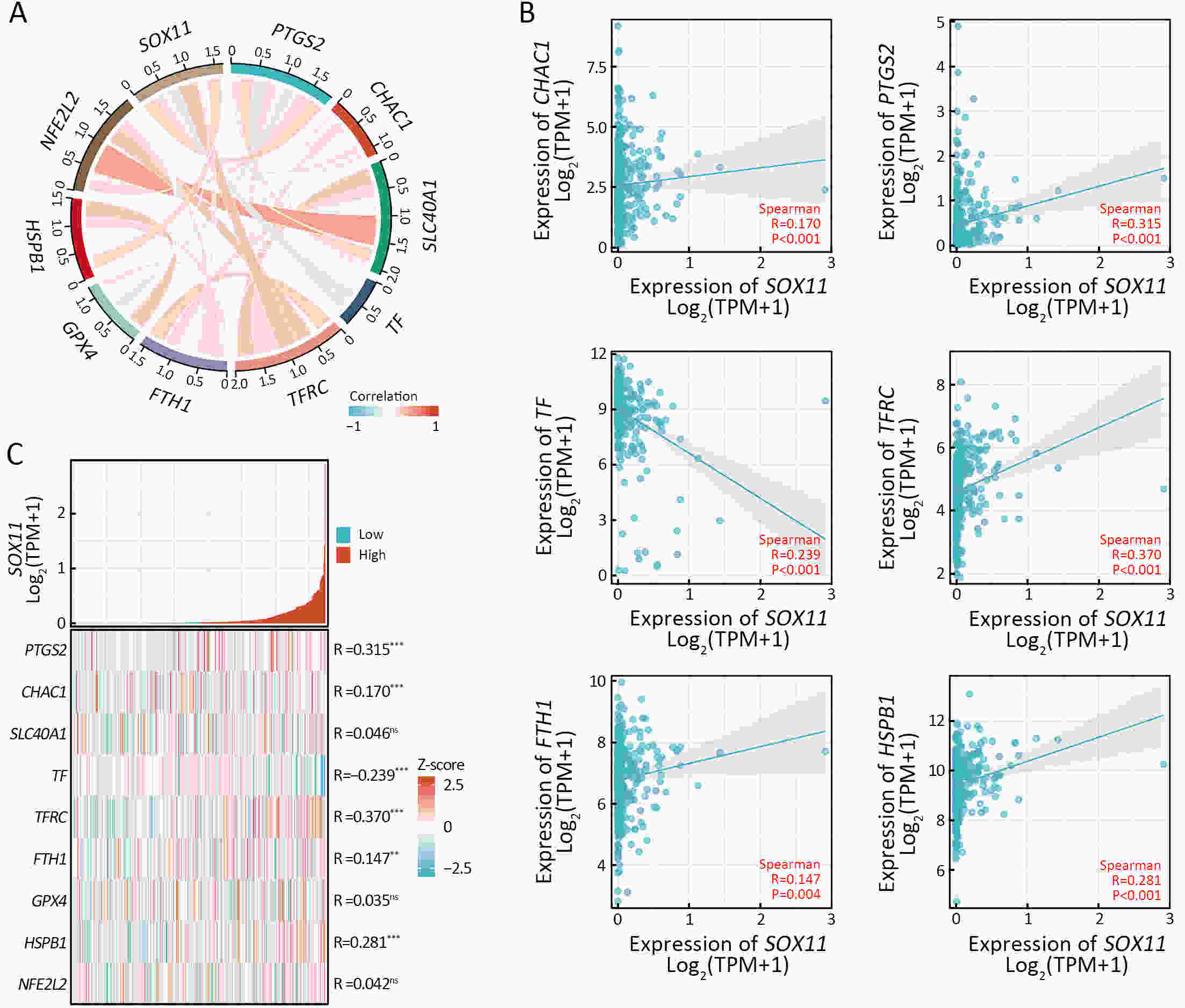
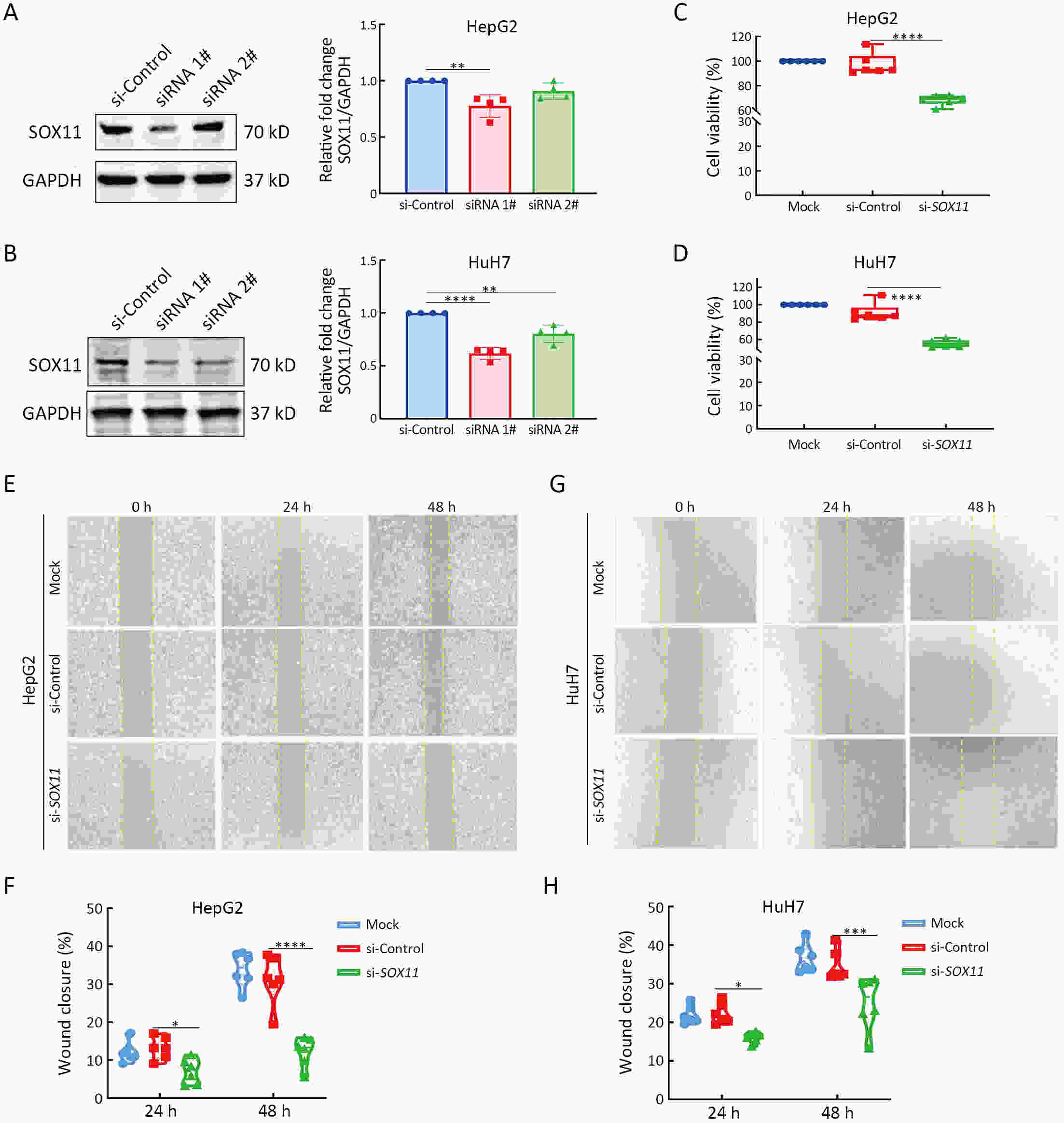
ObjectiveSOX11 is expressed in numerous malignancies, including hepatocellular carcinomas (HCC), but its oncogenic function has not been elucidated. Here, we performed a comprehensive bioinformatics analysis of the Liver Hepatocellular Carcinoma (LIHC) dataset to investigate the function of SOX11 in tumorgenesis. MethodsSOX11 expression data from The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) were validated by immunohistochemistry (IHC). Co-expression, differential expression, and functional analyses utilized TCGA-LIHC, Timer 2.0, Metascape, GTEx, and LinkedOmics databases. Associations with immune infiltration, ferroptosis, and immune checkpoint genes were assessed. Genetic changes were explored via CBioPortal. Logistic regression, receiver operating characteristic curve (ROC), Kaplan-Meier analysis, and nomogram modeling evaluated associations with HCC clinicopathological features. SOX11’s impact on proliferation and migration was studied in HepG2 and HuH7 cell lines. ResultsSOX11 was significantly elevated in HCC tumors compared to controls. SOX11-associated genes exhibited differential expression in pathways involving extracellular membrane ion channels. Significant associations were found between SOX11 levels, immune infiltration, ferroptosis, and immune checkpoint genes in HCC tissue. SOX11 levels correlated with HCC stage, histologic grade, and tumor status, and independently predicted overall and disease-specific survival. SOX11 expression effectively distinguished between tumor and normal liver tissue. Spearman correlations highlighted a significant relationship between SOX11 and ferroptosis-associated genes. Decreased SOX11 levels in HepG2 and HuH7 cells resulted in reduced proliferation and migration. ConclusionsSOX11 was found to represent a promising biomarker within HCC diagnosis and prognosis together with being a possible drug-target.
2024, 36(4): 398-409.
doi: 10.21147/j.issn.1000-9604.2024.04.04
Abstract:
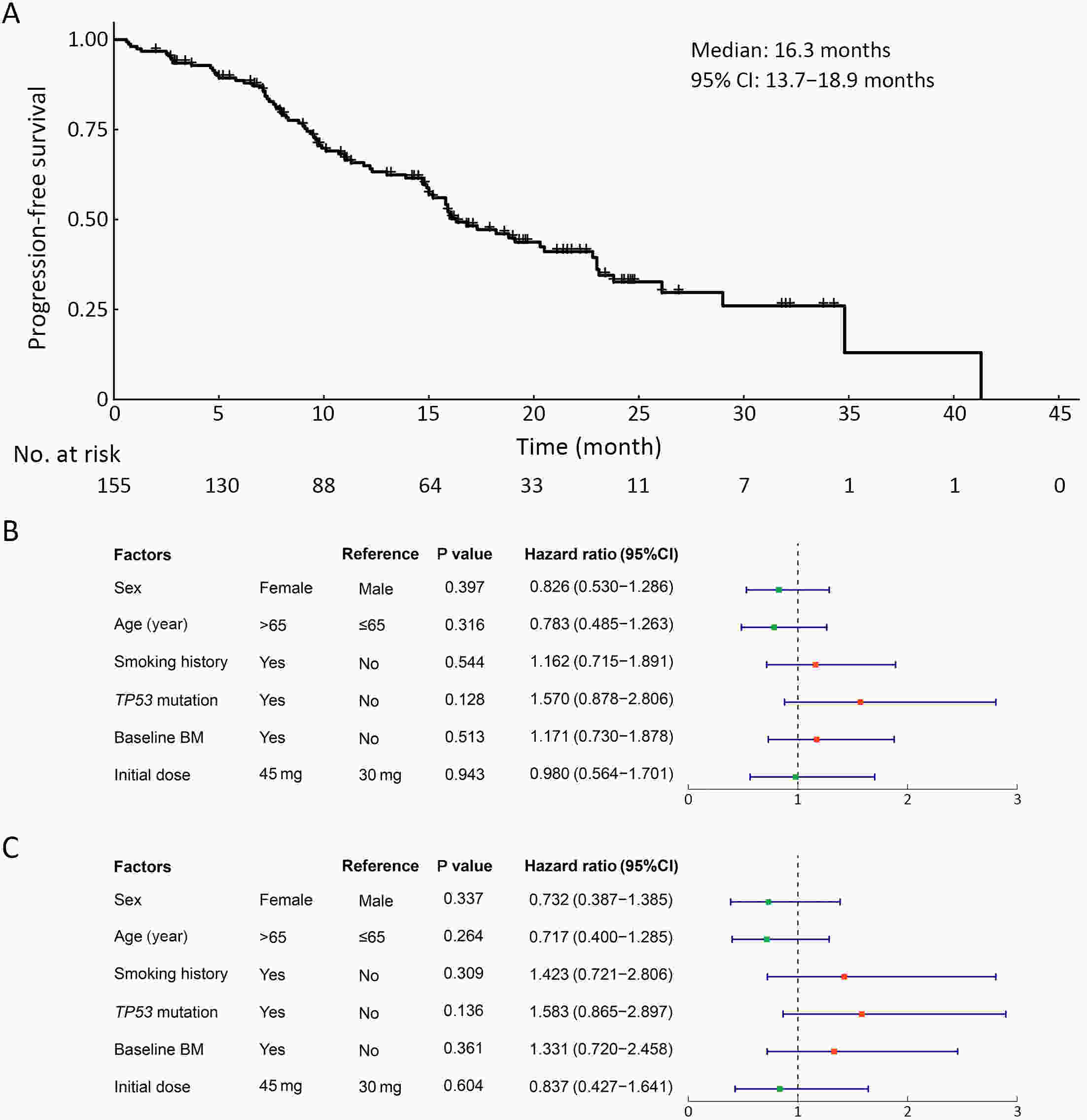
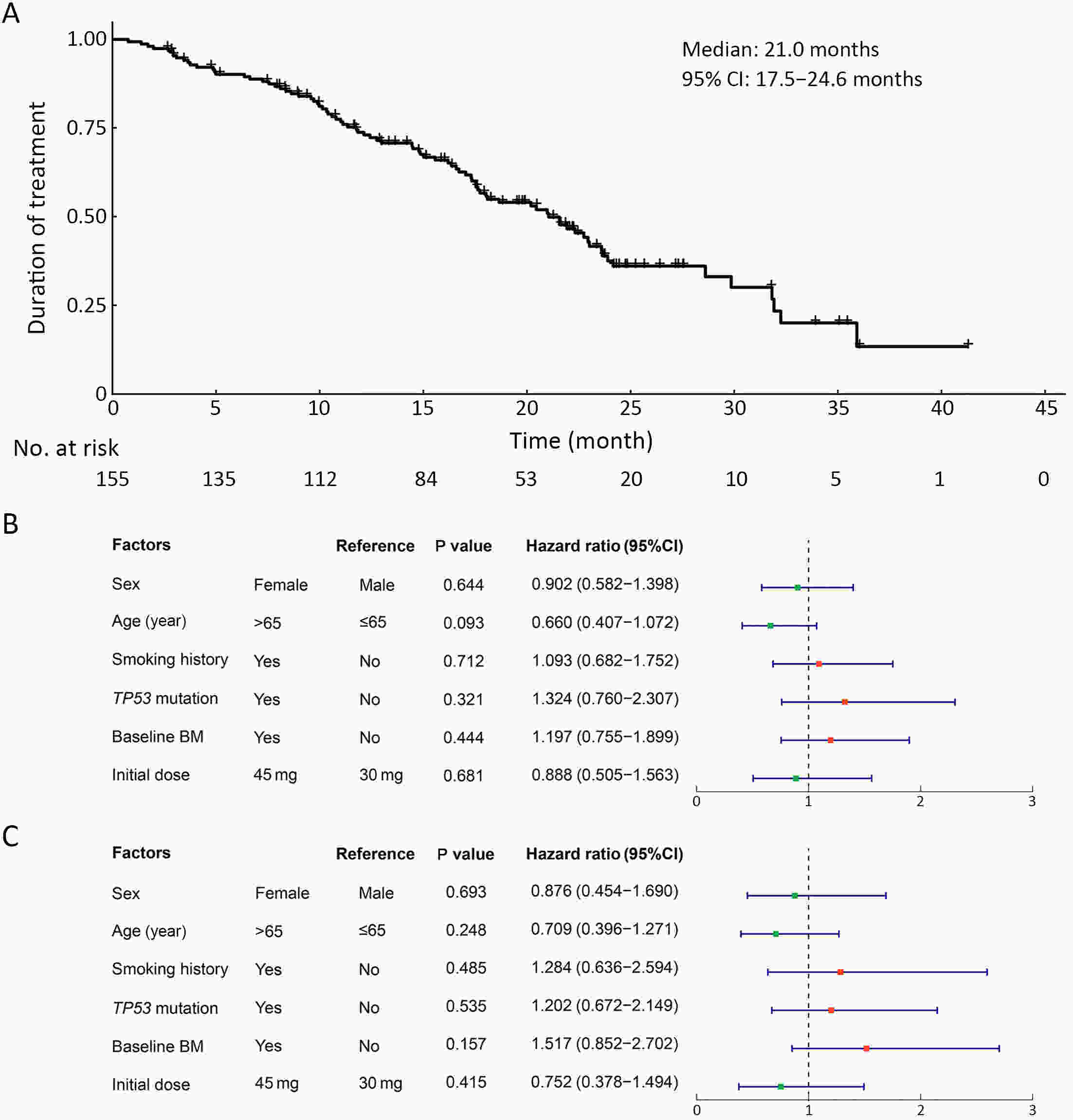
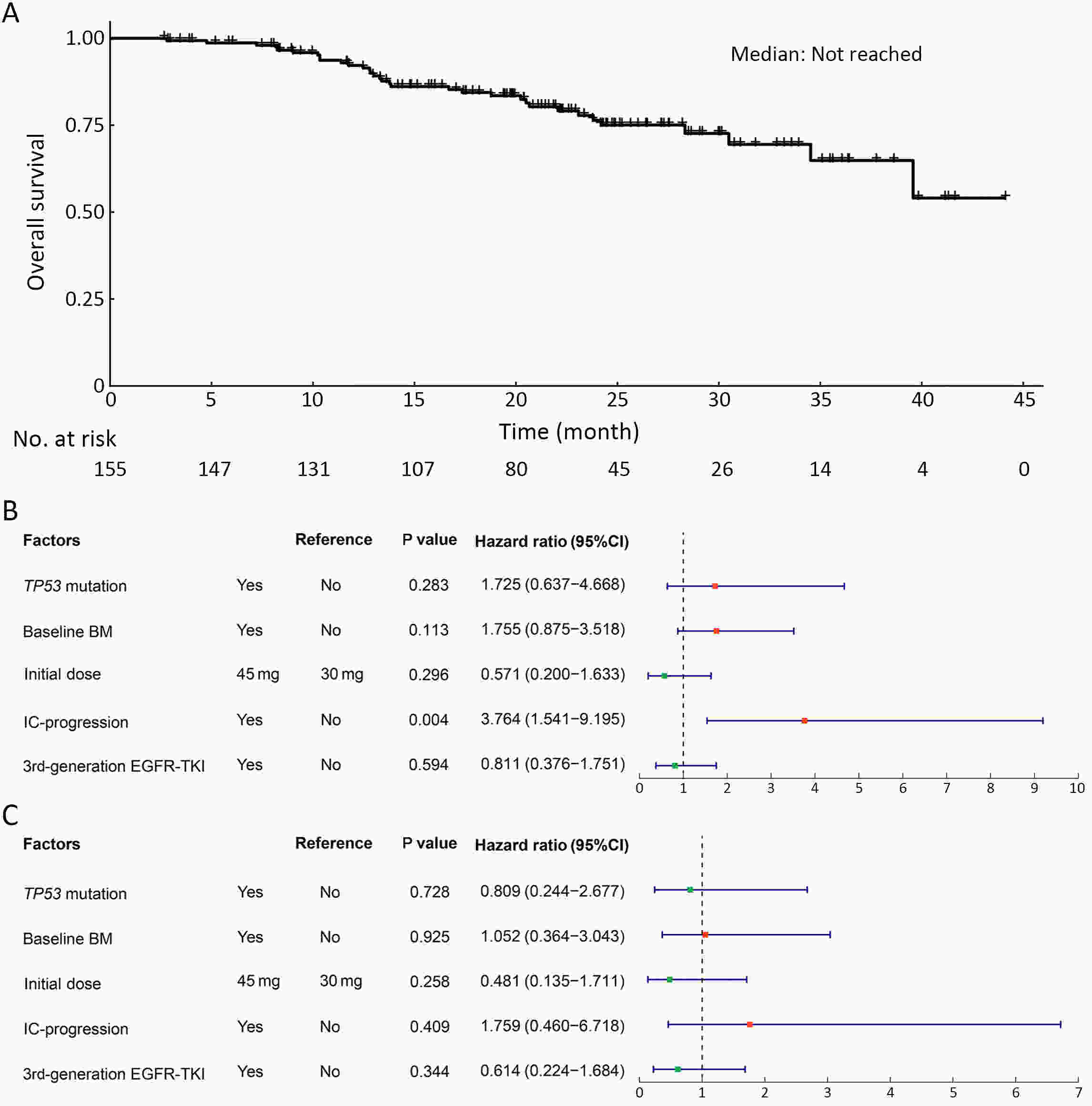
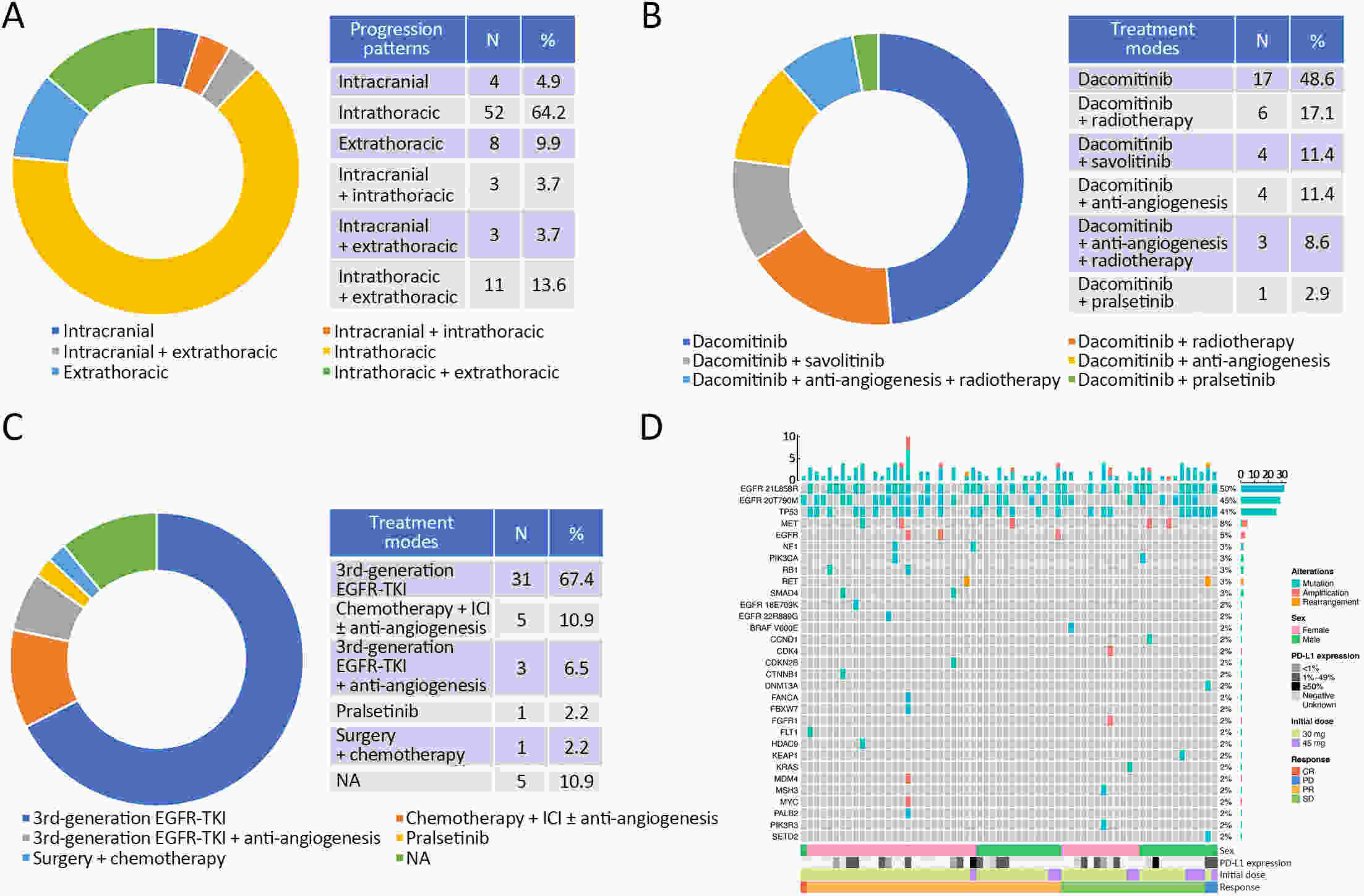
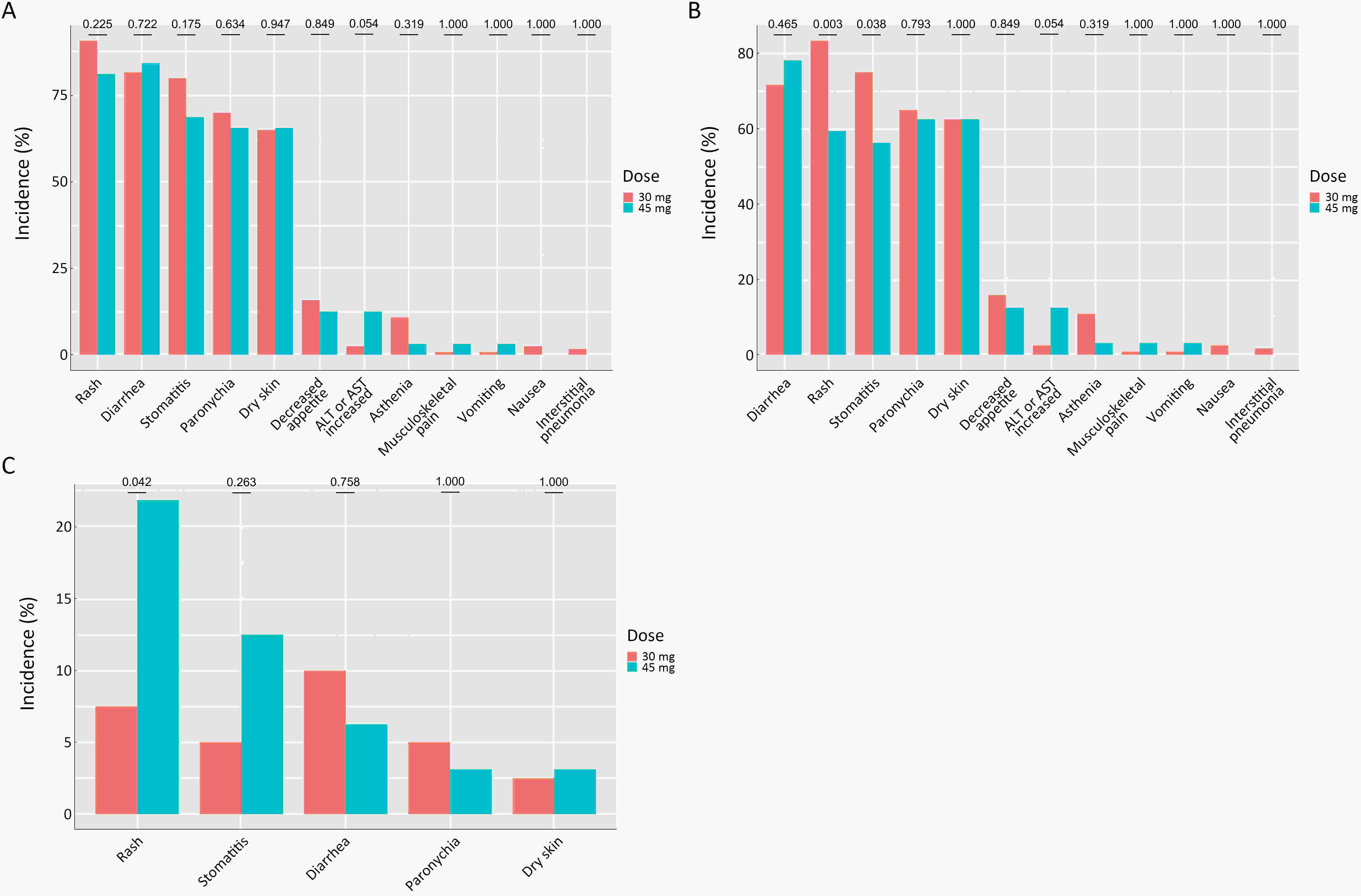
ObjectiveTo provide real-world evidence for the application of first-line dacomitinib treatment for epidermal growth factor receptor (EGFR) 21L858R mutant non-small cell lung cancer (NSCLC) patients in China and to explore the factors influencing the efficacy and safety. MethodsA longitudinal, consecutive case-series, multicenter study with mixed prospective and retrospective data was conducted. The primary endpoint was progression-free survival (PFS), and the secondary endpoints included duration of treatment (DOT), overall survival (OS), objective response rate (ORR), disease control rate (DCR) and safety. ResultsA total of 155 EGFR 21L858R mutant patients treated with first-line dacomitinib were included. The median follow-up time for these patients was 20.4 months. Among 134 patients with evaluable lesions, the ORR was 70.9% and the DCR was 96.3%. The median PFS was 16.3 [95% confidence interval (95% CI), 13.7−18.9] months. Multivariate Cox regression analysis suggested that the baseline brain metastasis (BM) status [with vs. without BM: hazard ratio (HR), 1.331; 95% CI, 0.720−2.458; P=0.361] and initial doses (45 mg vs. 30 mg: HR, 0.837; 95% CI, 0.427−1.641; P=0.604) did not significantly affect the median PFS. The median DOT was 21.0 (95% CI, 17.5−24.6) months and the median OS was not reached. Genetic tests were performed in 64 patients after progression, among whom 29 (45.3%) patients developed the EGFR 20T790M mutation. In addition, among the 46 patients who discontinued dacomitinib treatment after progression, 31 (67.4%) patients received subsequent third-generation EGFR-tyrosine kinase inhibitors. The most common grade 3−4 adverse events were rash (10.4%), diarrhea (9.1%), stomatitis (7.1%) and paronychia (4.5%). The incidence of grade 3−4 rash was significantly higher in the 45 mg group than that in the 30 mg group (21.9% vs. 7.5%, P=0.042). ConclusionsFirst-line dacomitinib treatment demonstrated promising efficacy and tolerable adverse events among EGFR 21L858R mutant NSCLC patients in China.
2024, 36(4): 410-420.
doi: 10.21147/j.issn.1000-9604.2024.04.05
Abstract:
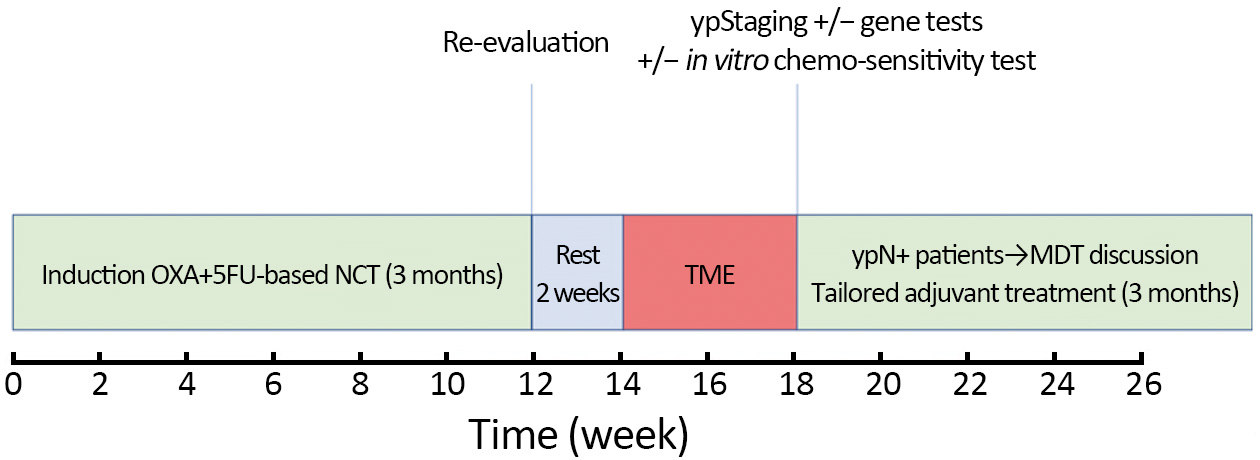
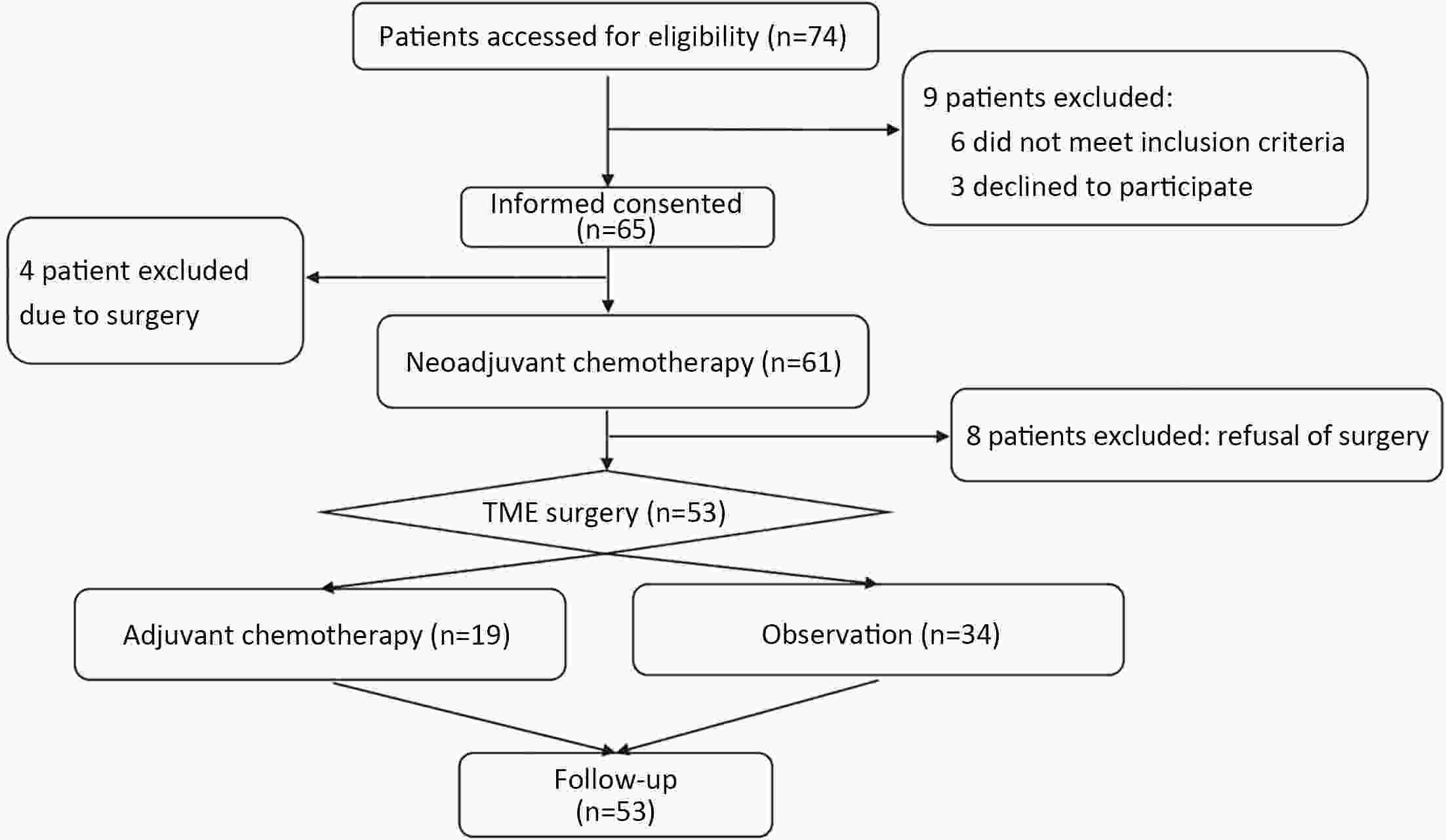
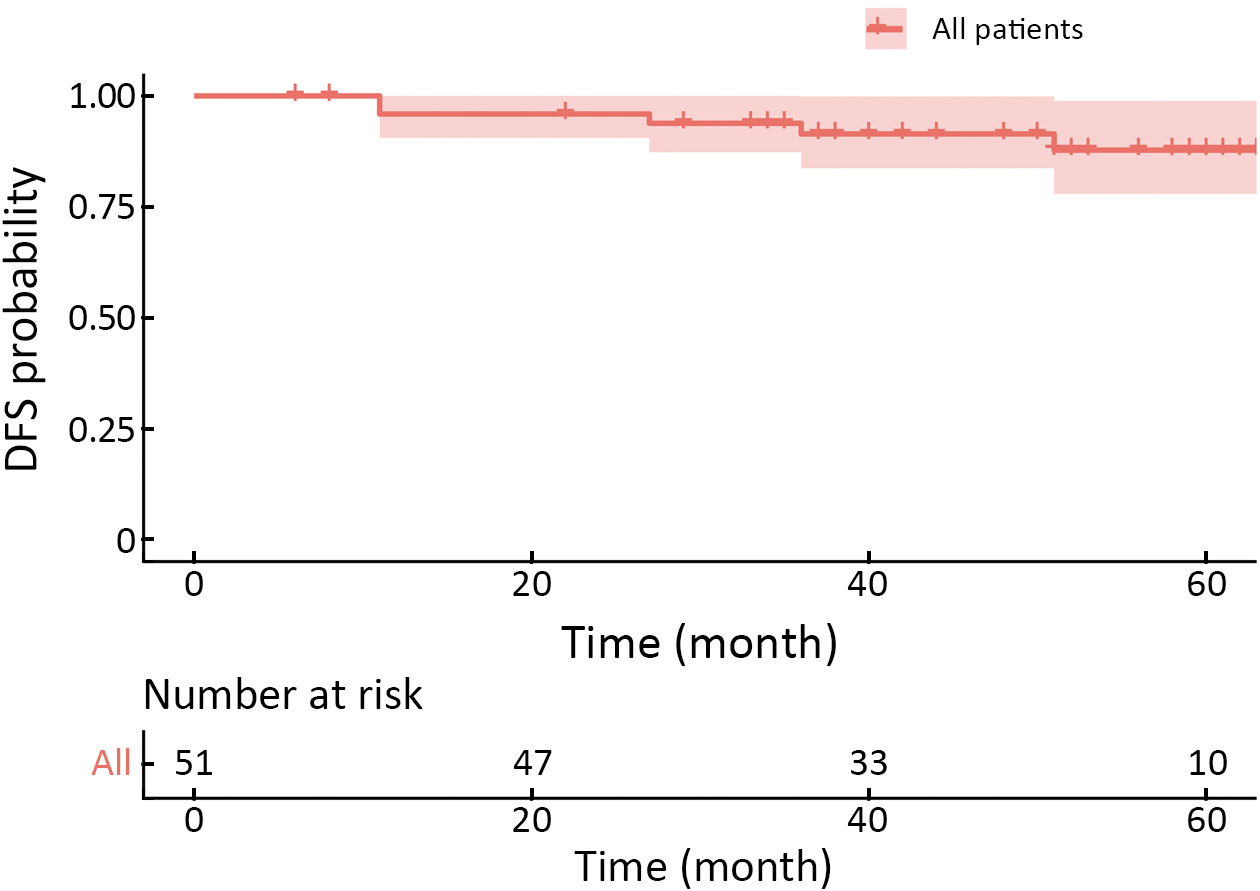
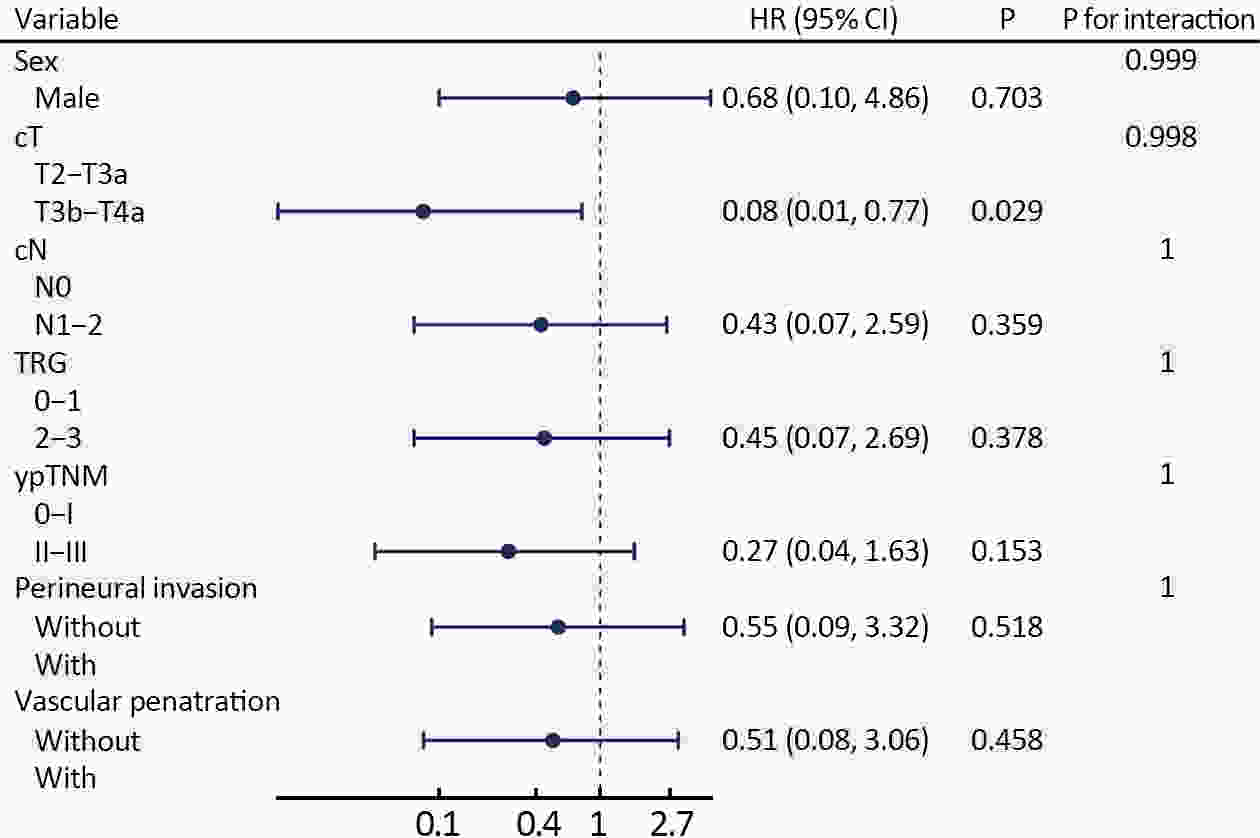
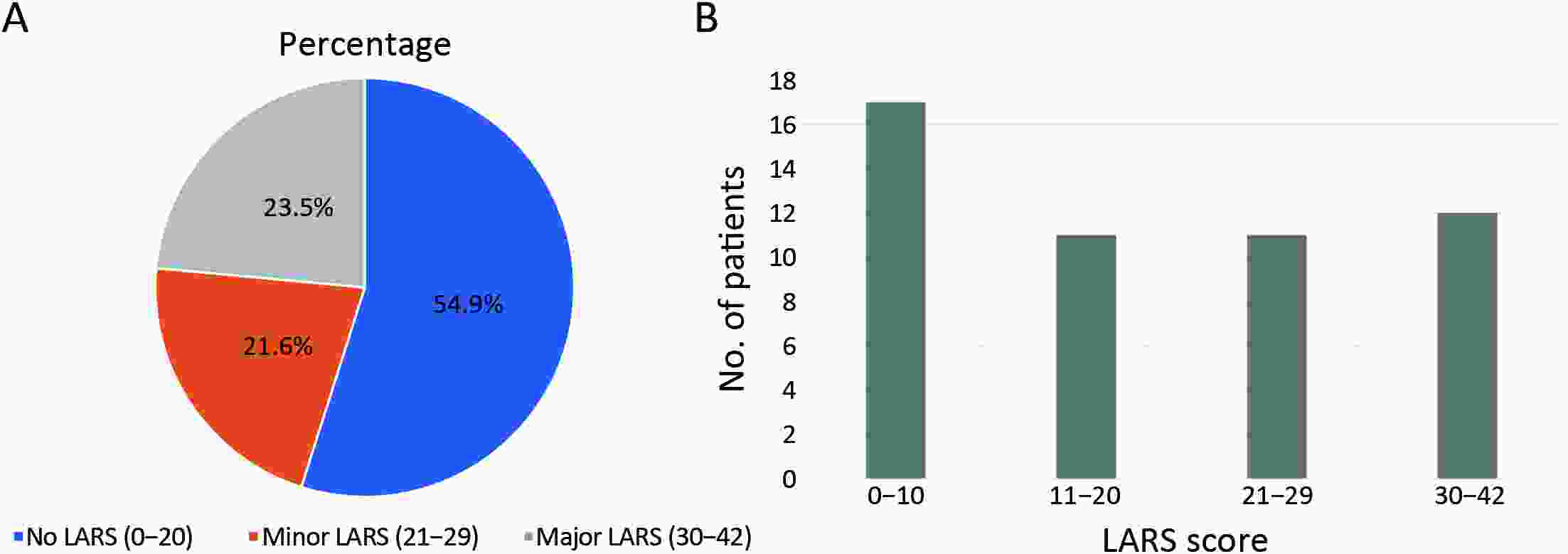
ObjectiveTo evaluate the safety and efficacy of neoadjuvant chemotherapy (NCT) in mid-low locally advanced rectal cancer with negative mesorectal fascia (MRF). MethodsThis prospective, single-arm phase II trial was designed and conducted at Peking University Cancer Hospital. The patients who provided consent received 3 months of NCT (capecitabine and oxaliplatin, CapOX) followed by total mesorectal excision (TME). The primary endpoint was the rate of pathological complete response (pCR). ResultsFrom January 2019 through December 2021, a total of 53 patients were enrolled, 7.5% of whom experienced grade 3−4 adverse events during NCT. The pCR rate was 17.0% for the entire cohort, and the overall rate of postoperative complications was 37.7% (1.9% of grade IIIa patients). The 3-year disease-free survival rate was 91.4%, and 23.5% (12/51) of the patients suffered from major low anterior resection syndrome (LARS). Postoperative complications were independently associated with major LARS. ConclusionsFor patients with mid-low rectal cancer with negative MRF, 3 months of NCT were found to yield a favorable tumor response with acceptable toxicity. With fair long-term survival, the NCT regimen could be associated with low rates of perioperative complications as well as acceptable anal function.
2024, 36(4): 421-441.
doi: 10.21147/j.issn.1000-9604.2024.04.06
Abstract:
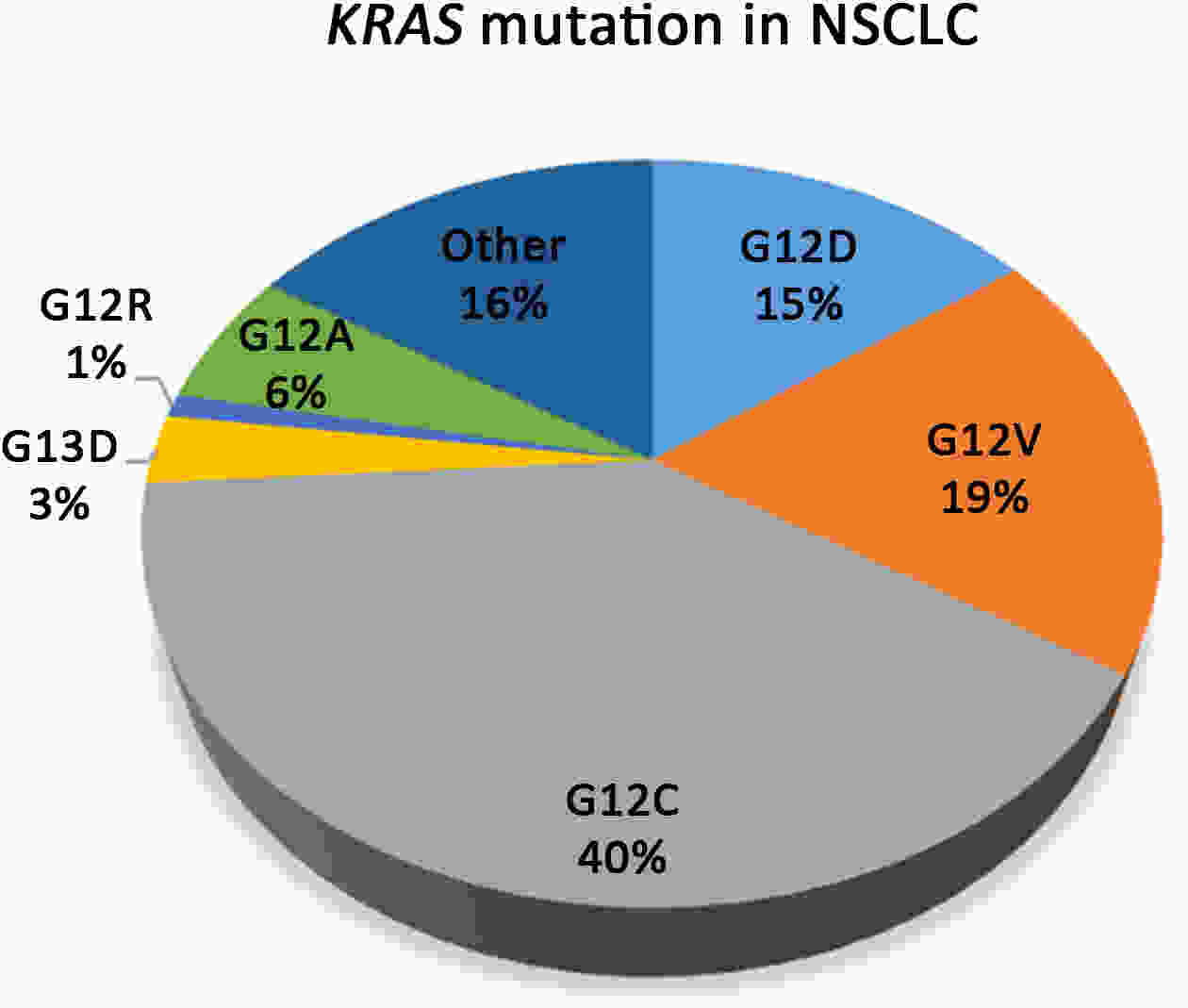
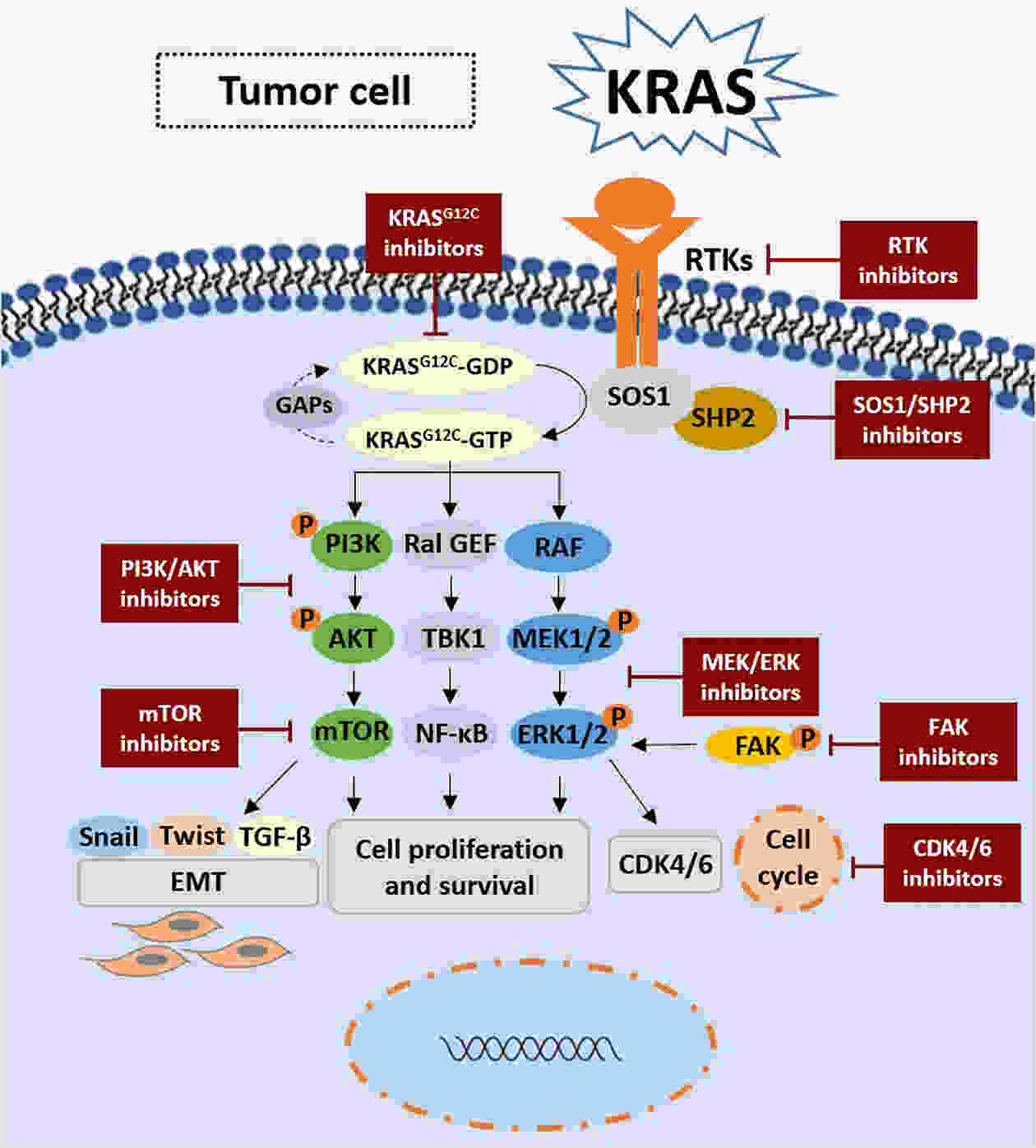
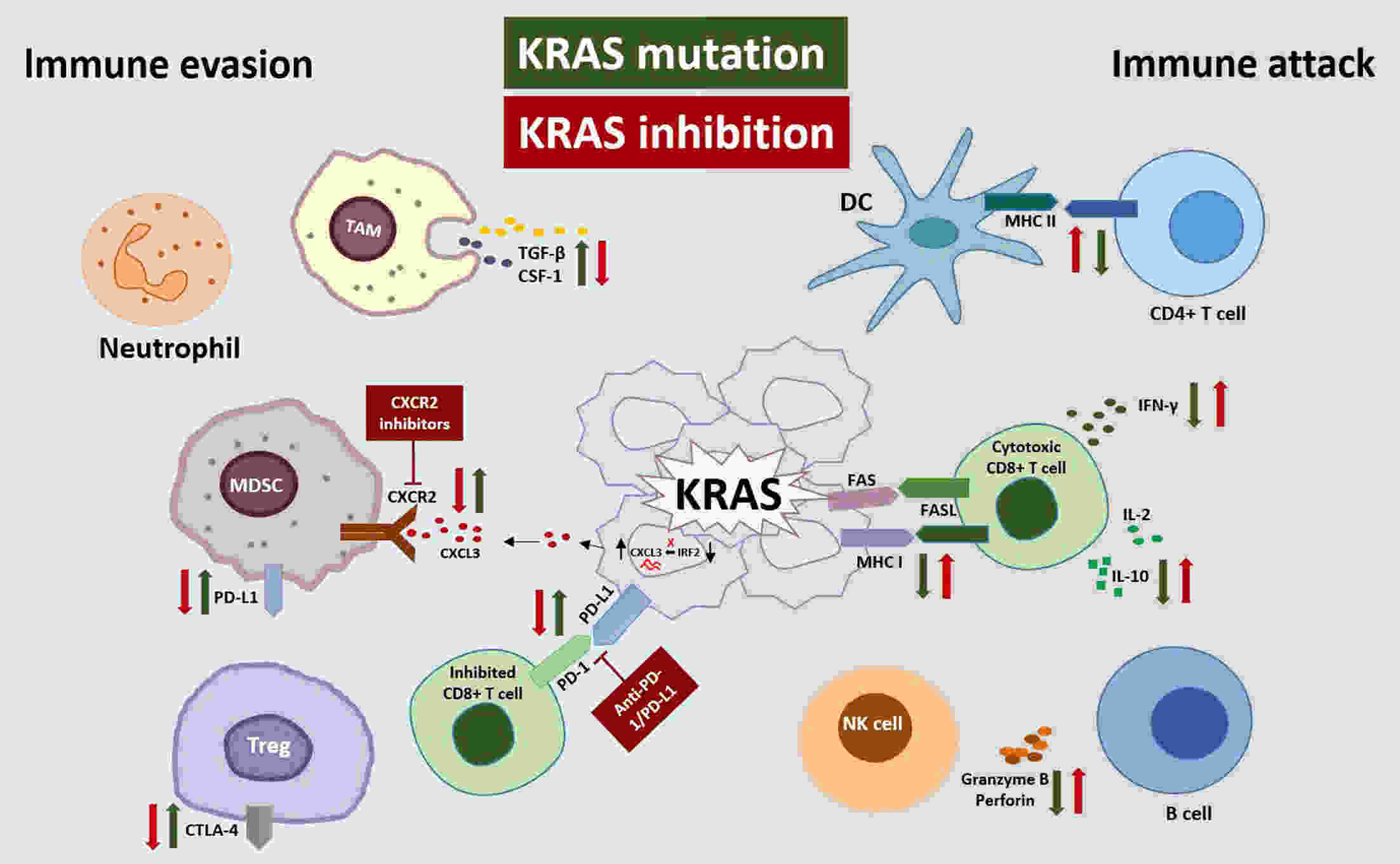
Kirsten rat sarcoma viral oncogene homolog (KRAS) is the most frequently mutated oncogene, occurring in various tumor types. Despite extensive efforts over the past 40 years to develop inhibitors targeting KRAS mutations, resistance to these inhibitors has eventually emerged. A more precise understanding of KRAS mutations and the mechanism of resistance development is essential for creating novel inhibitors that target specifically KRAS mutations and can delay or overcome resistance. Immunotherapy has developed rapidly in recent years, and in-depth dissection of the tumor immune microenvironment has led researchers to shift their focus to patients with KRAS mutations, finding that immune factors play an essential role in KRAS-mutant (KRAS-Mut) tumor therapy and targeted drug resistance. Breakthroughs and transitions from targeted therapy to immunotherapy have provided new hope for treating refractory patients. Here, we reviewed KRAS mutation-targeted treatment strategies and resistance issues, focusing on our in-depth exploration of the specific immune status of patients with KRAS mutations and the impact of body immunity following KRAS inhibition. We aimed to guide innovative approaches combining RAS inhibition with immunotherapy, review advances in preclinical and clinical stages, and discuss challenges and future directions.
Kirsten rat sarcoma viral oncogene homolog (KRAS) is the most frequently mutated oncogene, occurring in various tumor types. Despite extensive efforts over the past 40 years to develop inhibitors targeting KRAS mutations, resistance to these inhibitors has eventually emerged. A more precise understanding of KRAS mutations and the mechanism of resistance development is essential for creating novel inhibitors that target specifically KRAS mutations and can delay or overcome resistance. Immunotherapy has developed rapidly in recent years, and in-depth dissection of the tumor immune microenvironment has led researchers to shift their focus to patients with KRAS mutations, finding that immune factors play an essential role in KRAS-mutant (KRAS-Mut) tumor therapy and targeted drug resistance. Breakthroughs and transitions from targeted therapy to immunotherapy have provided new hope for treating refractory patients. Here, we reviewed KRAS mutation-targeted treatment strategies and resistance issues, focusing on our in-depth exploration of the specific immune status of patients with KRAS mutations and the impact of body immunity following KRAS inhibition. We aimed to guide innovative approaches combining RAS inhibition with immunotherapy, review advances in preclinical and clinical stages, and discuss challenges and future directions.
2024, 36(4): 442-454.
doi: 10.21147/j.issn.1000-9604.2024.04.07
Abstract:
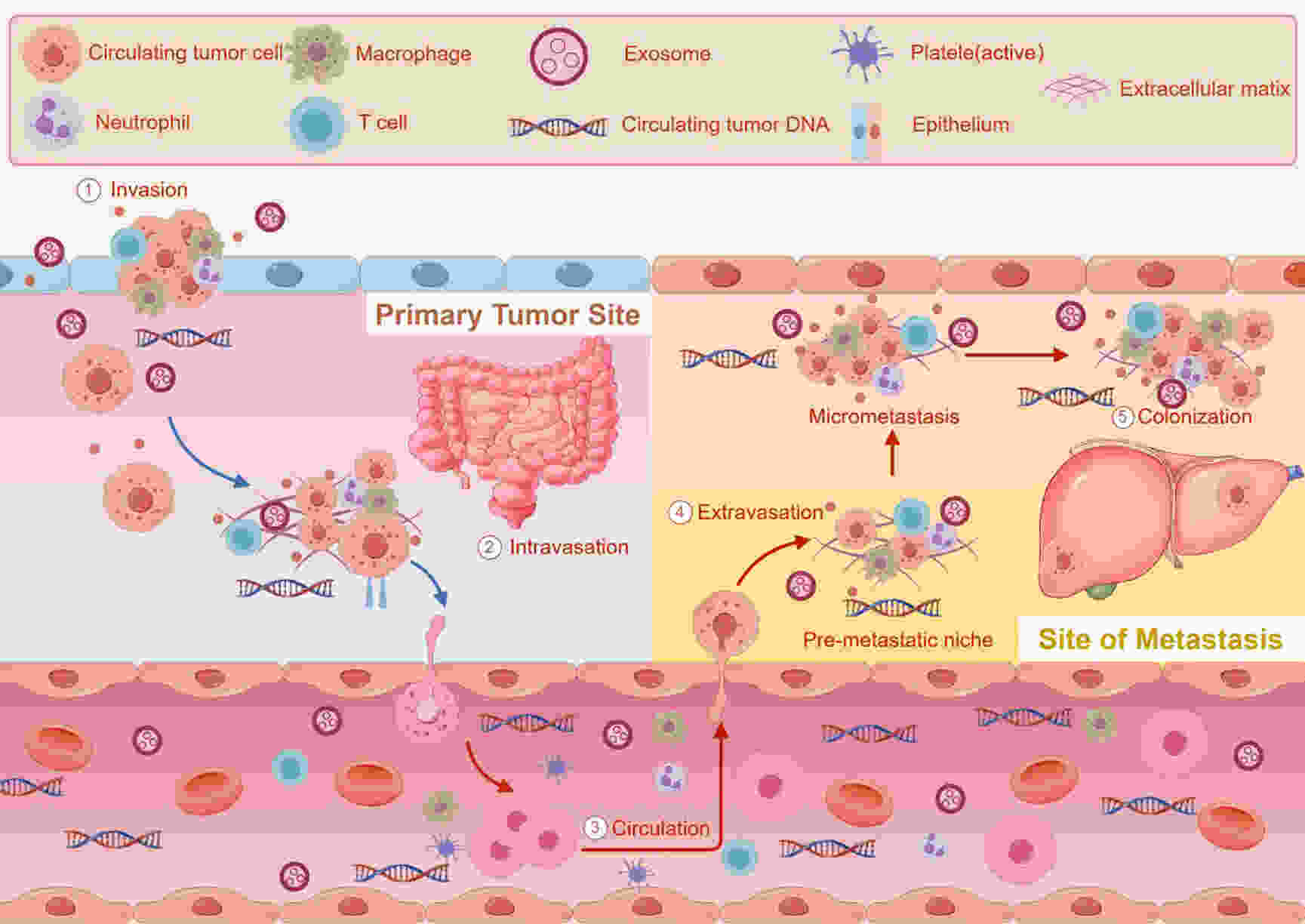
Although there has been significant advancement in the identification and management of colorectal cancer (CRC) in recent years, there is still room for improvement in the current standard treatment regimen. One area of concern is the lack of reliable tumor markers to predict treatment efficacy and guide tailored care. Due to its dynamic, effective, and non-invasive benefits over tissue biopsy, the detection of minimal or molecular residual lesions (MRD) based on circulating tumor DNA (ctDNA) is beneficial to the clinical development of drugs for patients with CRC after radical treatment, as well as for continuous monitoring of tumor recurrence and malignancy molecular gene evolution. The detection of ctDNA can currently be used to guide individual postoperative auxiliary treatment decisions (upgrade or downgrade treatment) in CRC, stratify the risk of clinical recurrence more precisely, and predict the risk of recurrence in advance of imaging examination, according to a large number of observational or prospective clinical studies. With increasing clarity comes the possibility of selecting a regimen of treatment based on postoperative ctDNA, which also improves the accuracy of clinical recurrence risk assessment for CRC. Therefore, it is anticipated that the identification of ctDNA would alter the current framework for dealing with CRC and lead to individualized, stratified precision therapy; however, additional confirmation will require subsequent high-quality, prospective, large-scale randomized controlled studies. This article will provide an overview of the definition and clinical significance of MRD, the primary indications and technological challenges for MRD detection, along with the advancement in clinical research about ctDNA detection following radical resection of the CRC.
Although there has been significant advancement in the identification and management of colorectal cancer (CRC) in recent years, there is still room for improvement in the current standard treatment regimen. One area of concern is the lack of reliable tumor markers to predict treatment efficacy and guide tailored care. Due to its dynamic, effective, and non-invasive benefits over tissue biopsy, the detection of minimal or molecular residual lesions (MRD) based on circulating tumor DNA (ctDNA) is beneficial to the clinical development of drugs for patients with CRC after radical treatment, as well as for continuous monitoring of tumor recurrence and malignancy molecular gene evolution. The detection of ctDNA can currently be used to guide individual postoperative auxiliary treatment decisions (upgrade or downgrade treatment) in CRC, stratify the risk of clinical recurrence more precisely, and predict the risk of recurrence in advance of imaging examination, according to a large number of observational or prospective clinical studies. With increasing clarity comes the possibility of selecting a regimen of treatment based on postoperative ctDNA, which also improves the accuracy of clinical recurrence risk assessment for CRC. Therefore, it is anticipated that the identification of ctDNA would alter the current framework for dealing with CRC and lead to individualized, stratified precision therapy; however, additional confirmation will require subsequent high-quality, prospective, large-scale randomized controlled studies. This article will provide an overview of the definition and clinical significance of MRD, the primary indications and technological challenges for MRD detection, along with the advancement in clinical research about ctDNA detection following radical resection of the CRC.

 Abstract
Abstract FullText HTML
FullText HTML PDF 10129KB
PDF 10129KB